i need to do this myself as my doctors don't wanna help me or give me CPAP because my symptoms and RDI is to low, i bought a device myself.
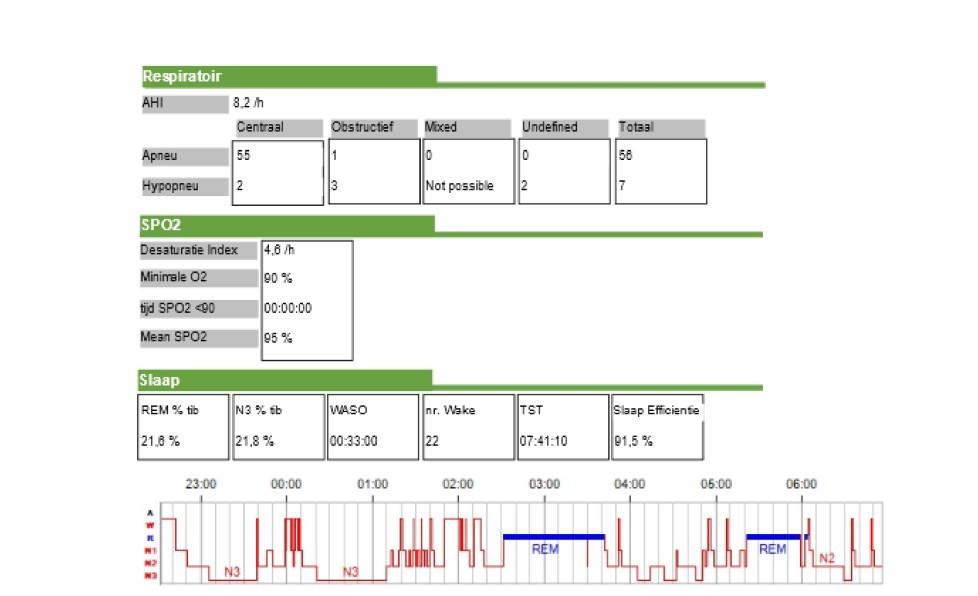
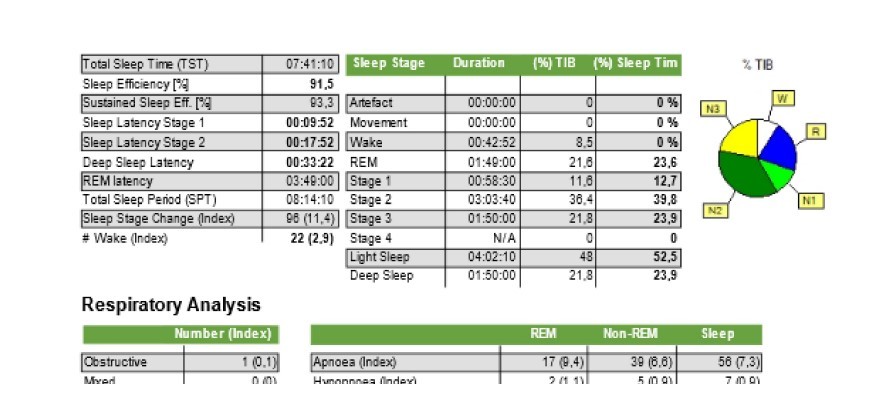
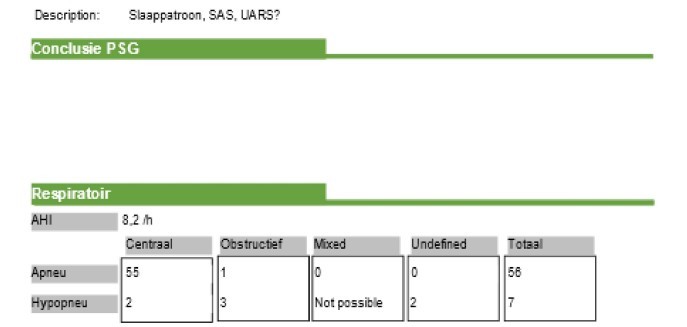
But what are the correct settings for a Resmed Airsense 10 Autoset for someone with mild (RDI 8.2) Central Sleep Apnea? it's only central, tho there were 0 RERA events during the sleep study which i find weird.
i know how to set it to clinical mode, and EPR should be set to 3 so i exhale just fine but what about the rest?
The general idea is to keep the pressure as low as possible while still maintaining a low obstructive apnea index. If the pressure is too high it can actually create central apnea events especially when you are a new used of CPAP. EPR at 3 is ok to start, but once things settle out you may want to try it with it lower or off. Each person is a bit different but I have found that EPR can reduce hypopnea. In others it can increase OA events with the same pressure settings.
I would suggest you start with a pressure of 8 cm max and 5 cm min. This will give you some idea if this is enough and you can go from there. It is best to wait 1-2 weeks between significant pressure changes. I like to set the Ramp on Auto, and with the pressure settings suggested, set the Ramp Start Pressure at 7 cm. Another convenience is to set the start stop to auto so the machine starts when you start breathing and stops automatically when you take the mask off.
Do you have OSCAR. It is essential to keep track of things while adjusting the machine, and also over the longer term to measure progress. It requires a PC or Mac and a SD card reader. Check your machine to ensure there is a SD card installed or it will not capture any detailed data. Some suppliers take them out.
If you have any questions, just ask,
due to problems with DHL i finally got the machine. i set it up and added the settings you gave me, also registered at myair and placed an SD card in the machine. Is it ok if i use start pressure of 4 cm for one or two days? it's the lowest number the machine gives me.
is it true that AHI will likely increase for 1 or 2 weeks because my body/brain needs to get adjusted with the CPAP machine?
oh yeah i put the machine on 'autoset' instead of 'cpap', is that fine?
Yes, it is fine to try the minimum at 4 cm. However since there is some flow resistance in the hose and mask, you may find that a little restricting when you inhale deeply. It can lead to a suffocating feeling. It can do that during the night too if it decides you need no pressure, and going down to 4 cm may wake you up. Especially with the EPR on, more pressure is easier to breathe with than low pressure.
Yes, there is something called treatment emergent central apnea. I found it lasted longer than 1-2 weeks and was more like 8 weeks.
Autoset if fine to start with. Once you find a good pressure it may give more predictable results with a fixed CPAP pressure. The machine can tell the difference between a central apnea event and an obstructive one. It raises pressure in response to the obstructive one, and makes no change in response to the central ones. However I don't believe it is smart enough to distinguish between a hypopnea that is central in nature compared to a obstructive apnea, and I believe it raises pressure on all hypopnea events. That can lead to more central apnea events. If you fix the pressure then you can stop that response. But, to know what pressure to fix it at, you need to run it in auto for a while and look at how it behaves over the pressure range it goes to.
Yes, it is fine to try the minimum at 4 cm. However since there is some flow resistance in the hose and mask, you may find that a little restricting when you inhale deeply. It can lead to a suffocating feeling. It can do that during the night too if it decides you need no pressure, and going down to 4 cm may wake you up. Especially with the EPR on, more pressure is easier to breathe with than low pressure.
i didn't think about that at all, so i should up it to 6 cm instead of 4 cm? what about the max?
Thank you, i will use OSCAR for the advanced data but i probably won't understand what i will see. For me the most important thing is if the AHI goes down or not, but i am willing to post the statistics after a good week of using the device (which will probably take some time to get used to).
I hope it fixes my fragmented sleep, in 8 hours i had about 23 brief awake moments and WASO was about 33 min.
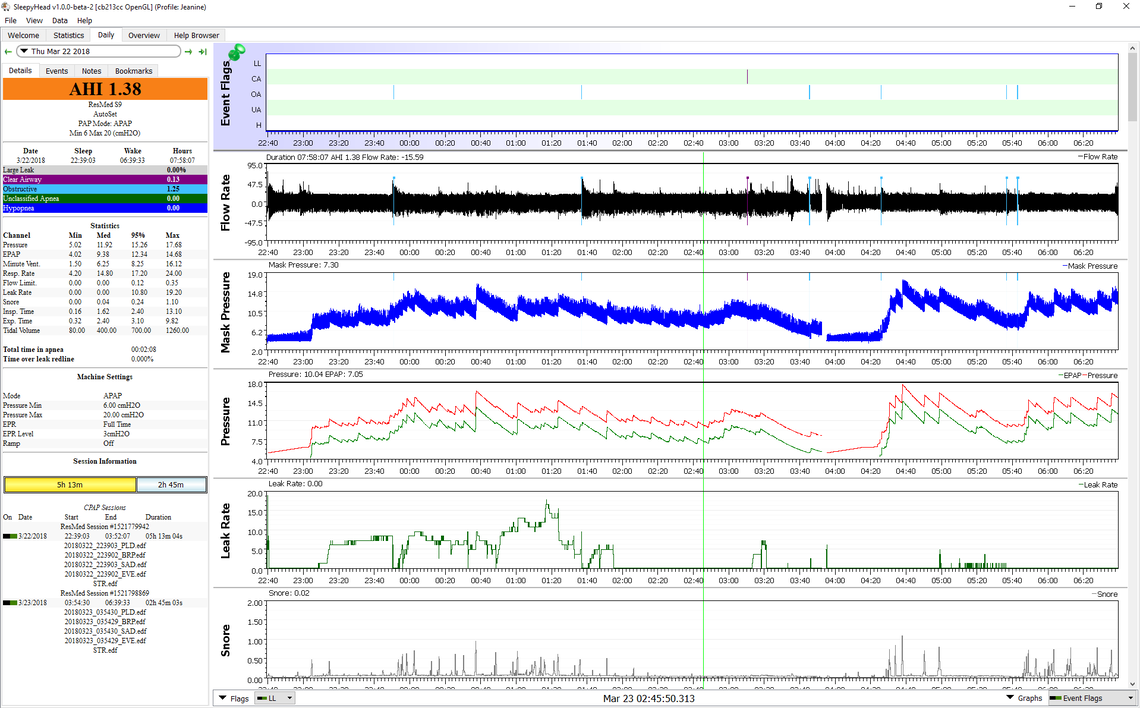
OSCAR is not all that hard to understand. It reveals the detail behind the numbers. See this example of the important graphs that it produces. You can see when the various types of events occurred. For example at 3:10 there is a CA. central apnea event, flagged with magenta. It happened with pressure about 14.5 cm. Note that the cpap does not increase pressure in response to a CA. A little later at 4:30 or so there is an obstructive apnea event, blue, that does result in an increase in pressure. Pressure was very low, too low, and that likely caused the event. There is a rapid response with an increase in pressure, but it is too late. Pressure at that time was set at a minimum of 6 cm and 20 max, which was where the sleep clinic set it. The minimum pressure for her was way too low, and the maximum was too high. A bit later she has another couple of events around 5:40 when the machine has ramped the pressure back down again. She currently uses a min and max pressure very close together in the 14.5 cm range to avoid this from happening. She was diagnosed at about 73 for AHI, and needs a much higher pressure than you will. In any case that is what you can do with OSCAR. It is essential in my opinion if you want to adjust your own pressures. Otherwise you are just shooting in the dark. You can post your results here for input if you are not understanding what they are showing. No need for all the reports that OSCAR can do. The main one is this Daily report. It has the important stuff. With a PC use F12 to capture the screenshot. Then just drag it with File Explorer to an open message here. Start with a fresh full width window, not like this one will be with a response to another post.
Unless it is just CA on initial treatment. The air sense isn't suitable for Central sleep apnea. Also in the sleep test, how much 02 desaturation. There are home spo2 overnight recording. Cms50 etc. You may need ST or better still, ASV.
what do you mean with 'initial treatment'? English isn't my main language.
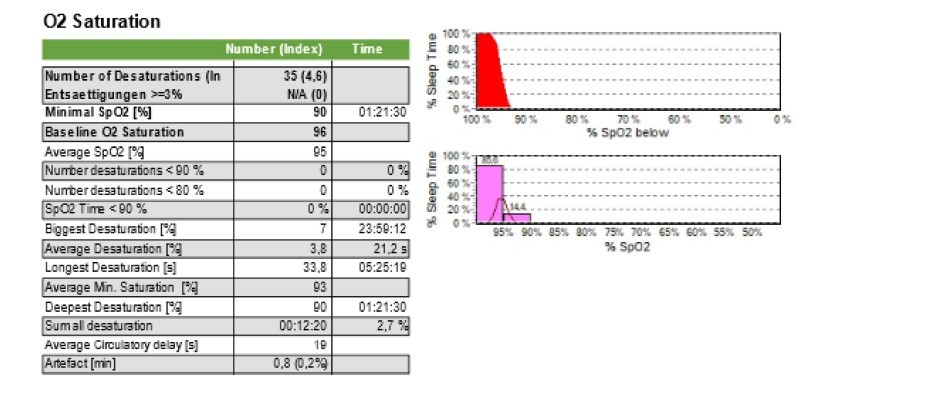
Desat index was 4,6/h min O2 was 90% mean SPO2 was 95%
it was a PSG, not a simple at home test.
It would appear that most of your apnea events are central. In this case a CPAP is not going to work. A central event is when you stop breathing while the airway is open. Increasing air pressure does not help with central events because the airway is already open.
what about the Resmed AirCurve 10 Vauto? is that good for central?
This is bilevel machine which has more pressure and a higher differential between inhale and exhale pressure. They typically do not work much better than a standard APAP for central apnea. The best machine for central apnea is the AirCurve 10 ASV. It follows your breath to breath breathing and steps in to assist when you do not breathe normally. See this link. https://document.resmed.com/documents/products/machine/aircurve-series/product-guide/1017631_aircurve10-asv-prod-guide_amer_eng.pdf
as RERA events were 0 i think that UARS was never measured during the study and judging by some aspects of my face (underbite and a slight deviated septum)i suspect that the central apnea events are caused by UARS for some reason (if that is medically possible).
During a short CPAP trial (lowenstein prisma smart) i managed to get a AHI of only 3 once as that was the only time i could sleep for like 2 hours). If all my events (AHI 7.2) were central then a CPAP cant lower those events.
for some reason my images aren't uploaded, does this work?
https://ibb.co/0CNnjgC https://ibb.co/RBNgb1N https://ibb.co/PMQDW1d https://ibb.co/nPxRK9p
What I meant by initial. When people start in CPAP, it is not unusual to have pressure induced CA. This normally resolves over time. The CPAP could be increasing your CA. You don't have obstructive apnea to treat. 5 all night, <one per hour.
I think this is why your doctor didn't do anything.
awake/arousal 2.3 times per hour... that's ok, you are sleeping through most CA.
av o2 95% ....that's ok.
Av desat 93% ...that's ok.
longest apnea 33.8, seconds, lowest desat 90% ..that's ok too.
No desat under 90%, ..goal is to be 90% and over.
Resmed titration guidelines S. If CPAP doesn't get good O2, next they switch to spontaneous bilevel, then ST and then ASV for CA, to get good O2 "For SpO2 < 90% with all respiratory events eliminated: • Increase IPAP by ≥ 1 cm H20 every ≥15 min until ≥ 90% SpO2 is reached• Follow sleep lab protocols for adding O2 Observe patient and document final settings, including IPAP/EPAP pressures and TiControl settings if altered from default"
You are always 90% and over, average O2 95% , average minimum 93% and wake/arouse 2.3 times an hour. For you I would ask your doctor, I think that treatment is optional, or un-needed.
but isn't 2.3 awake/arousel per hour bad? that messes up your sleep cycle big time right? my doctor still refuses to treat me with cpap or anything else. so what about UARS? i go from deep/rem sleep to light sleep more then the average person.
the answer to the question i am looking for for years is if my fatigue symptoms are caused by bad sleep or that it's mentally. nobody can give me that answer and it's killing me inside.
The basic purpose of a CPAP is to treat obstructive apnea and to a lesser degree hypopnea. If you don't have any, then it cannot do much, and as suggested can initiate more central apnea.
thanks.
what about UARS? does CPAP help against that?
Yes, CPAP can help with UARS. ResMed makes an AirSense For Her machine that acts faster to raise pressure to address it. But, it still just uses pressure, and more pressure can increase the frequency of central events. I believe the AirSense 11 AutoSet has the For Her mode built into it as an option. In the AirSense 10 model you need to buy the For Her version.
Sorry to ask again but wake/arouse is 2.3 times but my sleep is very fragmented right? like going from deep sleep to light sleep a lot of times? i want to ask my neurologist this but he is on vacation. How do you know i sleep through most CA?
btw did you hear about UARS? isnt it possible i have that?
What you need to do is look at your OSCAR daily reports. RERA events, Hypopnea, and Flow Limitations can be indications of UARS. Setting your EPR to full time at 3 cm may help reduce them.
i still can't sleep with the device! i am wide awake. Pressure is set at 6 but ramp is set at 5. i don't find the mask uncomfortable but it's the air and the focus on my breathing.
but i still would like to know why Bil thinks my sleep is 'fine' cause it looks very fragmented to me doesn't it? with fragmented i mean going from deep/rem to light/awake.
my doctor wants to put me on antidepressants but i really dont want that
I really can't see anything useful from your sleep reports, other than central apnea is the main issue detected. Without seeing your OSCAR reports which are much more useful than the sleep study information I can't really help you.
One thing to keep in mind is that a CPAP is not a "sleep machine". It cannot make you sleep when you don't want to sleep. In fact it can irritate you if you are not comfortable using it, and make it harder to sleep. Really all it can do is open the airway if it is closing (obstructive apnea), but you do not seem to suffer from that. If the airway is partly closing it can help with airflow by reducing pressure on exhale compared to inhale (EPR).
What the machine can do is report all the events which occur while it is on, along with what the pressure was at, etc. This can be helpful in diagnosing what is going on. But an OSCAR report is needed to do that...
You slept 7 1/2 hours in a lab, hooked up to a machine with wires everywhere. I don't see any trouble with your sleeping. Some people don't even get enough sleep to get a result
For the ca you could go talk to the doctor and see if there's any medications that you are on that is suppressing your breathing. Opiates are well known for this.
Google sleep hygiene CBT if you have bedtime issues
If you want to continue with a machine. I would get a secondhand S9 ASV. You should get that very cheap on Facebook or Craigslist. I definitely wouldn't use a CPAP mode machine, it can't help your ca and may in fact make it worse
The only other thing is plm, did they put wires on your leg.
Then maybe its not my sleep but maybe mentally tired...... not sure how i can feel the difference. I wasnt tested for plm but i dont have the urge to move my arms or legs at night tho
If it were me, I'd check with the lab/doctor on the number of arousals you had an hour. Regardless of whether they were CA, OA, RERA, URAS or PLMD. The lab should be able to count the arousals for any reason, on the sleep study. Your O2 levels have been fine and you don't need treatment for that part.
If you are arousing a lot. An ASV mode would treat all except PLMD and the CA excludes CPAP mode. I would get a low hour S/H resmed S9 ASV. The algorithm is very similar to the 10/11, if not the same. This would be a low-cost way to see if it helps your daytime feeling. If you aren't arousing, then it won't help and getting use to mask therapy, will disturb your sleep. It will have an overall negative effect on your sleep and daytime feeling.
If you are still using CPAP, I would stop. It is the wrong treatment for CA and can even make them worse. Have you downloaded OSCAR and looked at your past sleep history on CPAP?
for some reason my sleep study doesn't mention arousels at all.... but please keep in mind that i'm using the device because i suspect UARS, and not that my symptoms are caused by CSA.
about 2 years ago i could use a lowenstein prisma smart max CPAP device for a short time, and i remember that just once i had a AHI of 2 for the duration of 3 hours (thats how long i slept with it). if i really have central sleep apnea then there's no way that AHI would decrease
i tried to sleep with the device for a few days now but i get 0 hours of sleep, last night i tried a sleeping pill my doctor gave me but still 0 result.
I use a white noise device that goes off automatically after 1 hour, since i had to go to work early i removed it after trying it for 2 hours.
The report said i had an AHI of 4.7: both OSA and CSA and 'total AI. but how can i have these events while i was still awake?
how do people even sleep with it? i read that a lot of people with mild sleep apnea never get used to it.
I did not take to wearing a CPAP well at all. I recall thinking that I would get up and throw the whole thing out the window. but fortunately I did not. Getting the settings right, along with finding a mask you can "make friends with" goes a long way to improving comfort. What mask are you using?
If you can post a screenshot of a typical night with OSCAR I may be able to help you with the device settings to gain some more comfort.
Another thing that some people do is move their machine and wear it during the day while watching TV or while on the computer. A big part of it is getting comfortable with the machine, and realizing that you are not going to suffocate or anything bad. A screenshot will be helpful even if you do not sleep. It will show where all the settings are at, and I may be able to offer some suggestions for improvement.