Hi everyone, I've seen a lot of questions come and go over my time on this forum and a lot of people asking good questions though ultimately they are best left to be answered by medical professionals. So I went and compiled the top 5 questions I've found and made a video with a sleep doctor discussing them and their answers.
https://www.youtube.com/watch?v=akY4XmgPtL0
Hope this Helps get some good info to you all!
Just need some help with my events. I have a Airsense 10 Cpap machine. I have been on it for about 3 months. I still get high 20's on events daily. I was diagnosed at 33 AHI. I have talked to my PCP who prescribed my machine about making some adjustments and he told me that my machine is and auto machine and that it should take care of itself. I have done some research and seems most setups need adjusting from time to time. Any guidance would be helpful. Thanks for your time.
I don't think you are going to get a response from the OP on this. I suspect this thread was started to get hits on a YouTube channel.
My first question would be what is your breakdown of AHI events into CA, OA, and Hypopnea?
I was also diagnosed at an AHI of 33, but now I average 0.8 for AHI. To get they I initially adjusted the machine in Auto mode, and finally switched to fixed pressure mode once I knew what pressure worked best for me.
Im having to help several people with this at the moment. Im formulating a guide with some of the sleep therapists im working with so feel free to send me a email and i can get you in touch for some guidance. Chris@medisource.tech
Those numbers would suggest the APAP is not set up as well as potentially could. Just based on those numbers alone, about the only possible quick fix may be to increase the EPR to 3 cm full time, if it is not set that way already. That MAY reduce the hypopnea. The other big issue is the high number of Clear Airway or Central Apnea events. Unfortunately since the airway is already open, more pressure does not help to reduce CA events. In fact especially with new users of the APAP, the pressure may even be making the CA frequency worse. But, without seeing more detail, I would not suggest just reducing pressure. What are your min and max pressures set at?
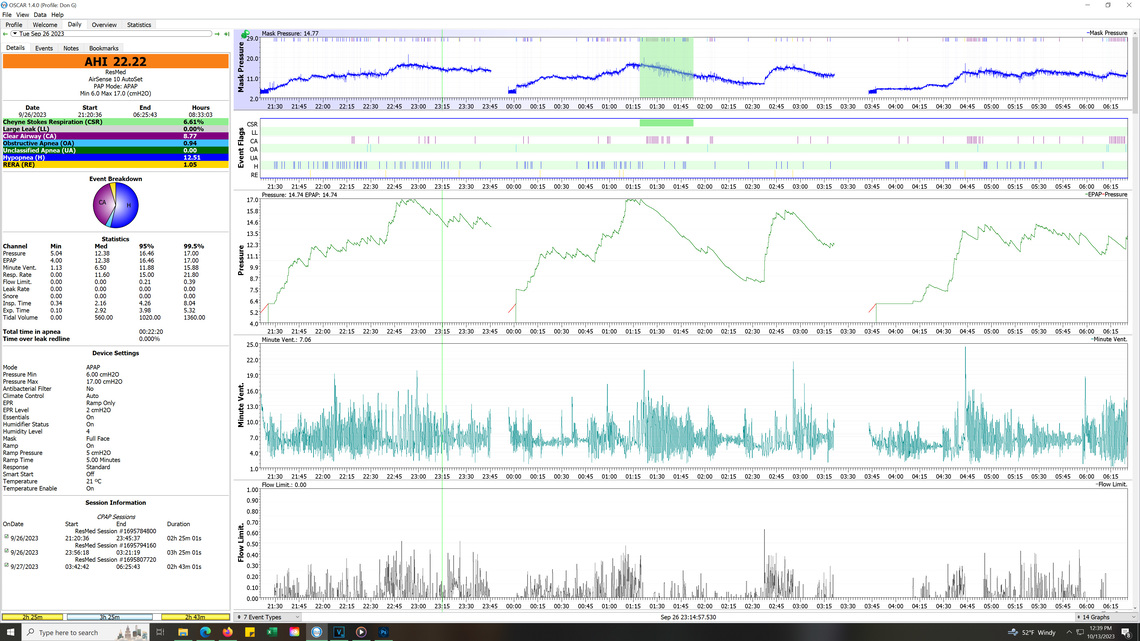
This said the best way the I could possibly help would be if you could download your data on the SD card to the OSCAR program, and then you could post your detailed daily report here. First you need a SD card in your machine. Some clinics unfortunately remove them. A 4 to 32 GB card is enough if there is none. Then you need a card reader and a PC or Mac to run the OSCAR software.
This software flags all the events you are having, when they are happening, and what the pressures are throughout the night. With your issues the first think to look for would be when the CA events are happening and what the pressure is at the time.
Post back if you need any help getting OSCAR working for you, and when you do post the daily report here. Save it as an image file, left click on it, and then drag it into an open post.
For some reason these posts with the OSCAR graphs did not show up until today. This site is quirky and seems to delay posts with graphics in them especially for new users.
I am having trouble seeing all the detail and if there is any way you can increase the width of the left hand window it would be helpful to read the numbers. You may also want to increase the height of the individual graphs by clicking and dragging on the dividers. The important ones are the Event Flags which I pin to the top position. Then Mask Pressure, Flow Rate, Pressure, Minute Ventilation, and Flow Limitations are the most important. If you click on the title of each you drag the graphs up to get these to display. It is OK if the rest slip down to the bottom and don't display.
In any case, what I am seeing is that most of your AHI is hypopnea, and next is central apnea events, with zero or near zero obstructive apnea events. First, assuming you are in Colorado, what elevation are you at? Denver? It is nearly a mile above sea level, and the altitude can aggravate the central apnea issue. And, more pressure can make central apnea worse, not better. EPR can help reduce hypopnea in some cases. I see you have EPR turned on only during the ramp. Here are some suggested changes you could try. I would try one at a time to see what impact each has. If things improve, keep it, and move on to the next change.
When you have tried these, then check back in. You may need an ASV machine instead of an APAP. It can deal with the CA events better, if they continue to be a problem, especially if you are at a high elevation. Another alternative is that a drug used for elevation sickness is sometimes used to reduce CA events if you are at a high elevation. You of course would need a doctor prescription to try it. But, try the changes above to see if they help first.
Your data suggests that you have Complex Sleep Apnea. Here is a link to a detailed article about the condition. Near the bottom of the article it mentions the off label use of acetazolamide which is the drug for altitude sickness.
I do live at 5,300 feet in altitude. Thanks so much for your help. I will adjust as you describe.
Now that I see the data better, it seems most of the CA events are happening at higher pressures. You may want to make your first max pressure reduction down to 14 cm max, and then do 1 cm at a time to get to the ideal pressure sooner. And to help a little bit to avoid OA events you may want to make these changes.
This will get your pressure up a little quicker and potentially avoid some of the early OA events.
It also appears that flow limitations are driving your pressure up. Putting the EPR to full time at 3 cm could help reduce them.
For what it is worth I had similar issues and when I finally got the max pressure about right, I had it at 11 cm. And, then at that point I found I got the best results by switching from the APAP mode to a fixed pressure CPAP mode, with the pressure set at 11. Leave that to the end, after you get into the correct pressure range.
Oh, and when you post a graphic, it helps to open a new full width window by using the orange Write a Reply button in the bottom left of the screen. Another quirk of this site is that it keeps making each response window narrower and narrower!
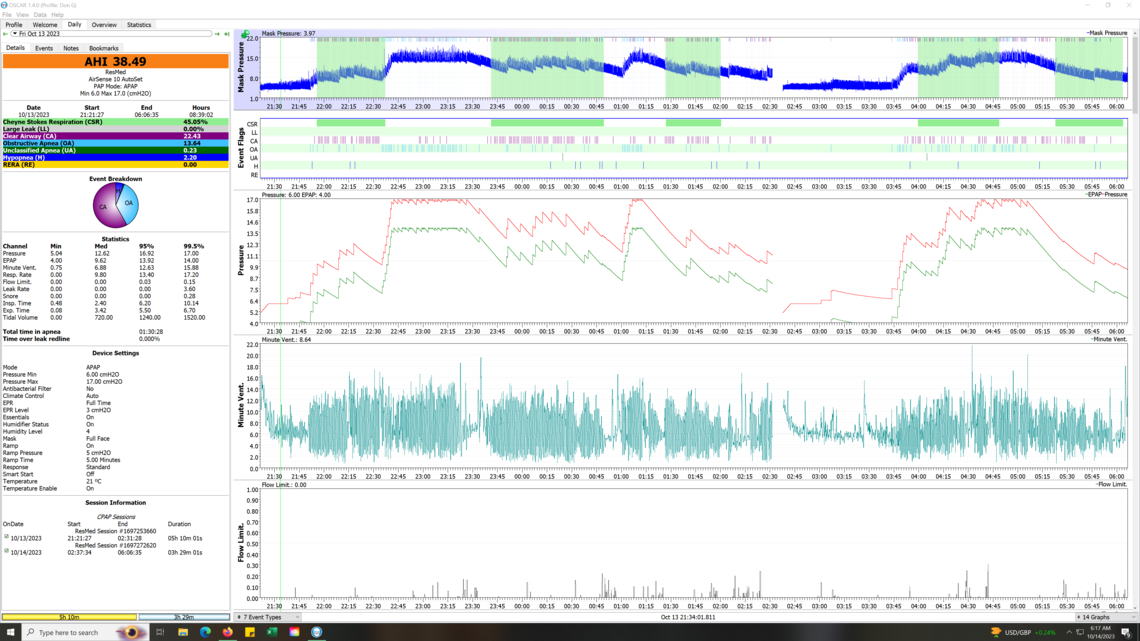
Thanks, here is night one of the first change. Looks like I will go back and try your latest settings suggestion.
Yes, you did not respond well to the full time 3 cm EPR, other than hypopnea seems significantly reduced. For sure go back to having it on ramp only. You may want to revisit it later at a lower level than 3 cm. The concerning part is how much OA you are getting with pressure at the max of 17 cm. It is also concerning that the CA events seem to be happening at a lower pressure. I would go back to ramp only EPR for a couple of nights with max pressure the same at 17 cm to see if the OA events come back down.
Okay thanks, didn't want to interrupt your weekend. Have a good weekend.
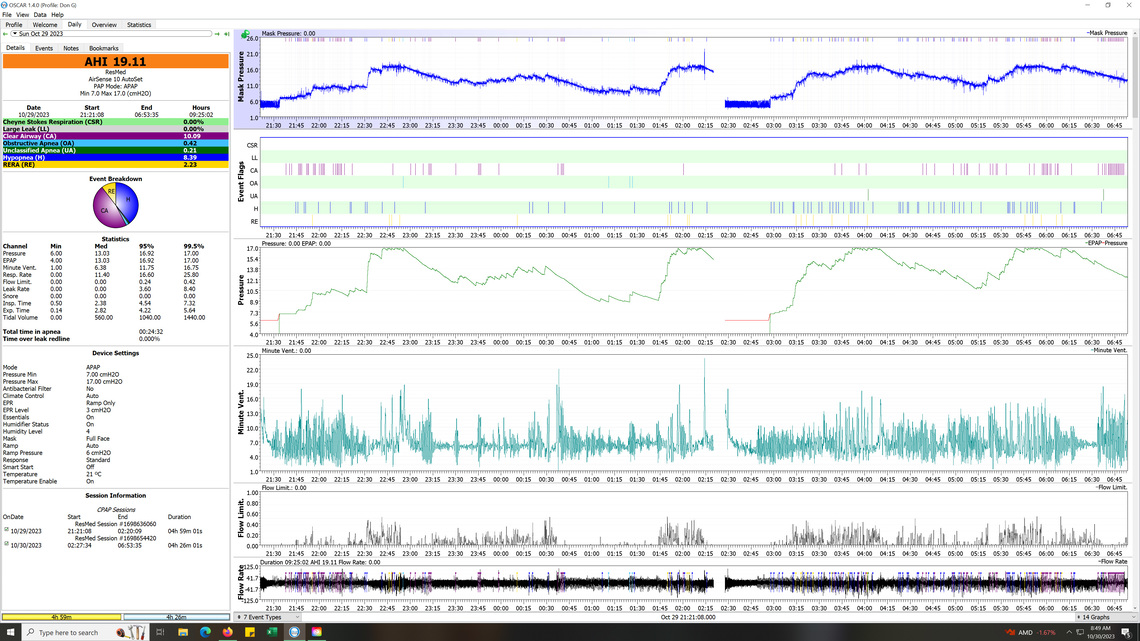
There are some areas to explore, but this is looking more and more like a situation that needs an ASV instead of a APAP. I exchanged a number of posts with an individual who lived in Canada at 500 feet but vacationed at Lake Chapala in Mexico at 5,500 feet. I recall him having similar issues. I think we found some settings that worked to some degree but it required two different setups for the two different elevations. He was on a BiPAP so the terminology is slightly different. You can find the posts at this link if you want to explore them.
https://myapnea.org/members/lakechapala/posts
In the end he got an ASV and brought AHI down to very low levels. So, while I would not give up on your APAP just yet, but an ASV may be the final best solution. See this information on the ResMed version of one. They are not cheap and are in the $5,000 range.
An ASV looks at your breathing pattern and adjusts pressure on a breath by breath basis to essentially force you to take a breath even when you do not initiate it.
Went for a week on the old settings. Had events ranging from 10.5 to 38.8 here is the report from last night.
I would be interested in seeing a zoomed in detail shot of the mask pressure, Flow Rate, and Minute Ventilation in a couple of the areas where you are having a high frequency of CA events. This may help understand what is causing the CA events. Here is an example from my data of what you might see.
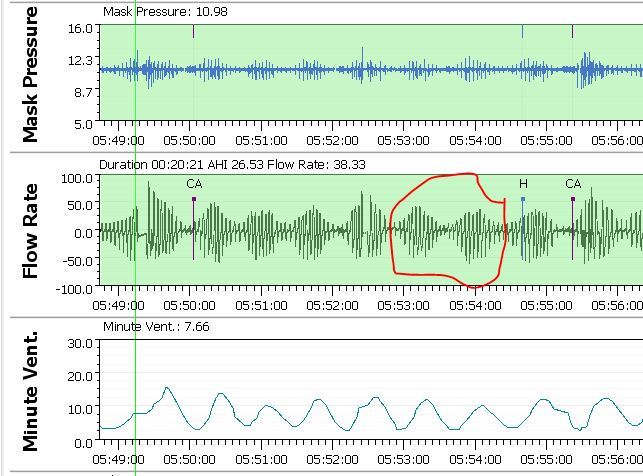
Hope this file is helpful.
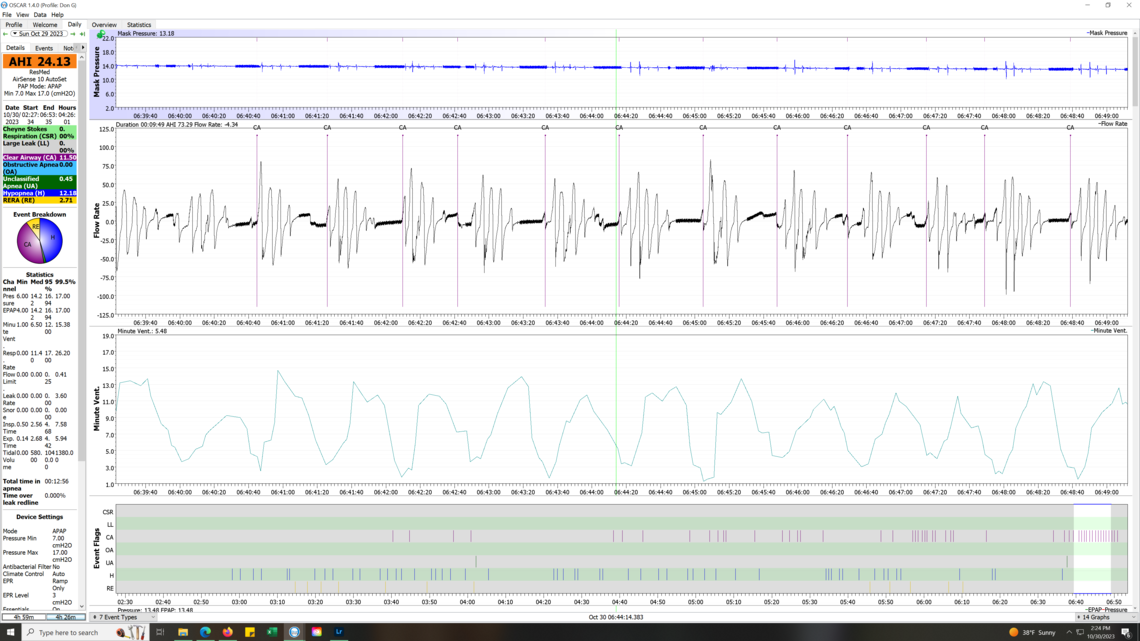
Although your machine has not flagged it as Cheyne-Stokes respiration (CSR), I am pretty sure that it is. CSR is a period of increased depth of breathing followed by decreasing depth of breathing, followed by a period of apnea with the airway open (CA). The reason that it repeats over and over is that the CO2 intensity signal is not getting back to the control system quickly enough. High CO2 causes you to breath more deeply, while low CO2 causes you to breath less deeply, and even stop breathing (CA). Your breathing rate gets out of sync with what it needed. You are breathing more and more deeply when CO2 has already recovered, but the control system does not know it. The control is essentially unstable. It never catches up like a dog chasing their tail.
While what is happening is fairly obvious, the root cause is not. In the worst case it could be a sign of heart failure, or a neurological issue. It can also be caused simply by the APAP machine pressure, but I am not so sure that is your case. In your previous post I see the multiple CA events even when your pressure is quite low and under 10 cm. Your could experiment with lower pressures or even fixed pressures in the CPAP mode, but I can't say I would be all that optimistic about it working. Because of your altitude the issue is likely aggravated by the elevation effect. The test of this would be to see if this still happens at an altitude closer to sea level. Another option would be to get a sleep apnea test where the pressure is not increased by the machine to see how frequent the CA events are.
Probably the first thing you should do is be seen by a cardiologist. Be sure to take the printouts of your overall results and some printouts of the expanded examples of your CSR. Potential solutions could be the prescription of the elevation sickness drug I mentioned earlier, or an ASV machine. Something needs to be done, as the AHI is currently way too high to leave things as they are now.
Here is a link that looks worth reading about CSR causes and treatment.
https://nchmd.org/health-library/diseases-and-conditions/con-20166460/
Altitude is likely causing your issues to be worse than average. I live at about 2,000 feet and CA's are my most significant contributor to AHI. I also have CSR flagged from time to time. When I vacation at sea level my AHI almost always goes down. I have not traveled to an area at 5,000 feet and I am sure my issues would get much worse at that elevation.
Thinking about this a little longer I would suggest these steps as the best approach.
Thank you. I have reached out to a new Sleep Doc and they are going to do a new complete sleep study to see what is going on. I do have Myasthenia Gravis, recently diagnosed so that may be part of the issue. I will update and we progress through this issue.
I am not familiar with that condition. The condition or medication used to treat it, may be a factor in CSR. It is worth investigating.
One thing to be aware of is that some sleep doctors/technicians may want to use a BiPap for treatment. It is very similar to an APAP like you have but it can up to 25 cm in pressure and the "pressure support" can go up to 10 cm. Pressure support is using more pressure on inhale than on exhale and is essentially the same thing as EPR except EPR is limited to 3 cm, and pressure support can be as much as 10 cm. Based on your use of EPR having benefit for hypopnea but aggravating CA events this device is unlikely to be successful for you. However, if you are involved in the DME system in the US, it may be a hoop you have to jump through to get an ASV, which is much more likely to work for you. Just make sure you get a free trial before buying a BiPap as it is not likely to work. I recall that the DME system may require you to fail on use of a BiPap before they are allowed to supply an ASV.
I did a little more checking into the impact of elevation on CSR or PB (periodic breathing). From what I saw, it seems healthy non apnea sufferers can tolerate up to 9,000 feet of elevation without suffering from CSR. However, those with other issues can be impacted at elevations as low as 4,500 feet. You (and I) may be in that category. If you are seeing specialists in Denver, they should be familiar with the altitude issue.
On the sleep test, be aware there are two steps to an in lab sleep test. First they test you with no pressure to see the type and frequency of apneas you are having. Next they do a step test (titration) where they keep increasing pressure in steps to see the impact on the apneas. This step test would be useful in determining if pressure is a factor causing your central apneas and CSR.
Thank you so much for the great info. It will be helpful. i am going to Anshutz Medical Center for the study. They are known for treating MG issues like mine along with the sleep stuff. Hopefully we can move forward. Thanks again.
FYI MG really attacks the diaphragm and breathing and may be the issue.