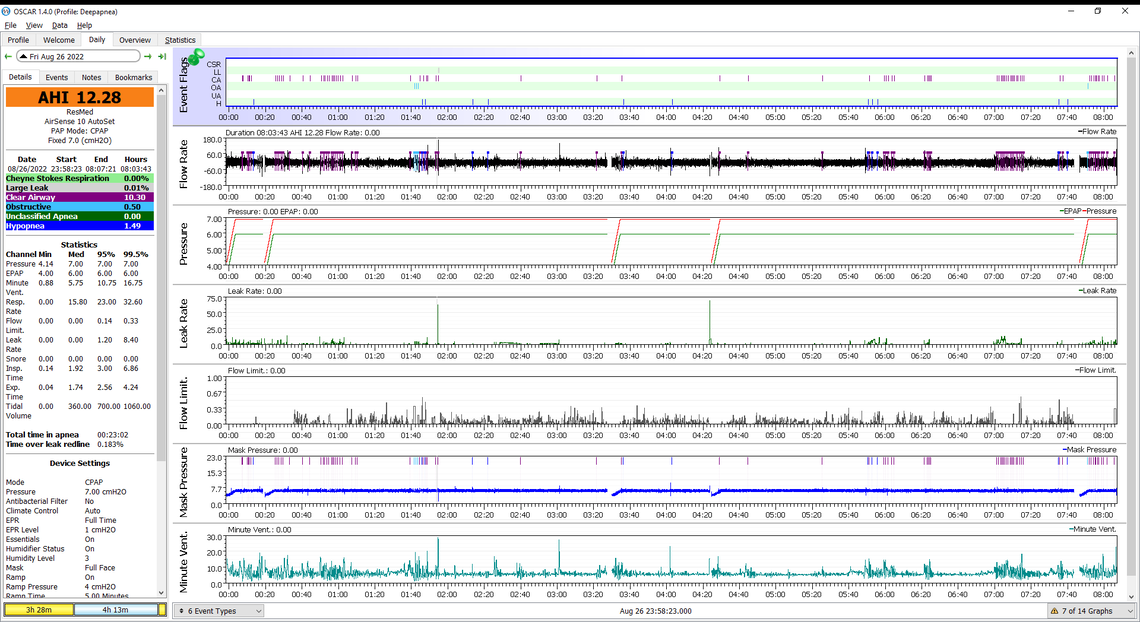
Using AirSense 10 for 4 months now (pressure at 7 cmH2O) but my AHI is always between 10 and 15, unless I drink the equivalent of 4-5 pints of beer alcohol, which brings the AHI down to 3-5. The OSCAR software tells me that 80% of my apneas are clear airway (CA) and less than 10% obstructive. Looking at the time course of AHI over night, there is typically a sharp rise shortly after falling asleep. I am also using a device that tells me the sleep pattern. When my AHI is between 10 and 15, I normally have only 2-3% of deep, non-REM sleep, which explains my dizziness, headache next day. Any suggestions?
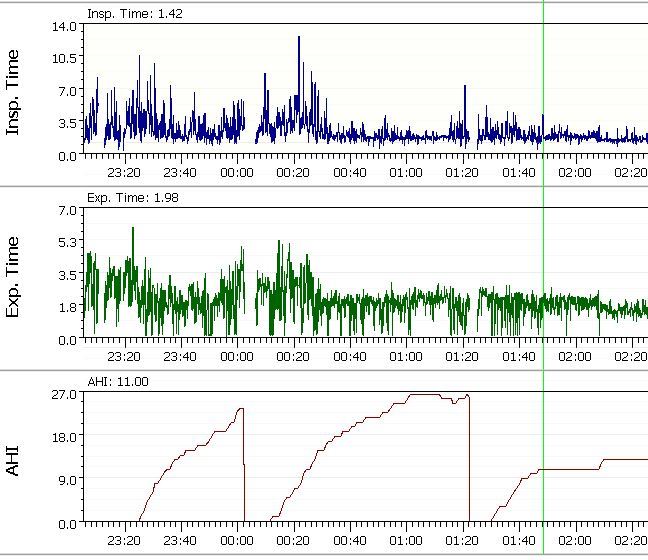
The image shows the rise of AHI after sleep-onset.
The problem with alcohol is that it can relax you and help you in the early sleep but as it wears off you tend to wake up and everything gets worse after that. It would be much better if you could post a Daily Screenshot with this type off format in the example below, and I could give you my comments. Central apnea is difficult but there are some things one can do to control it.
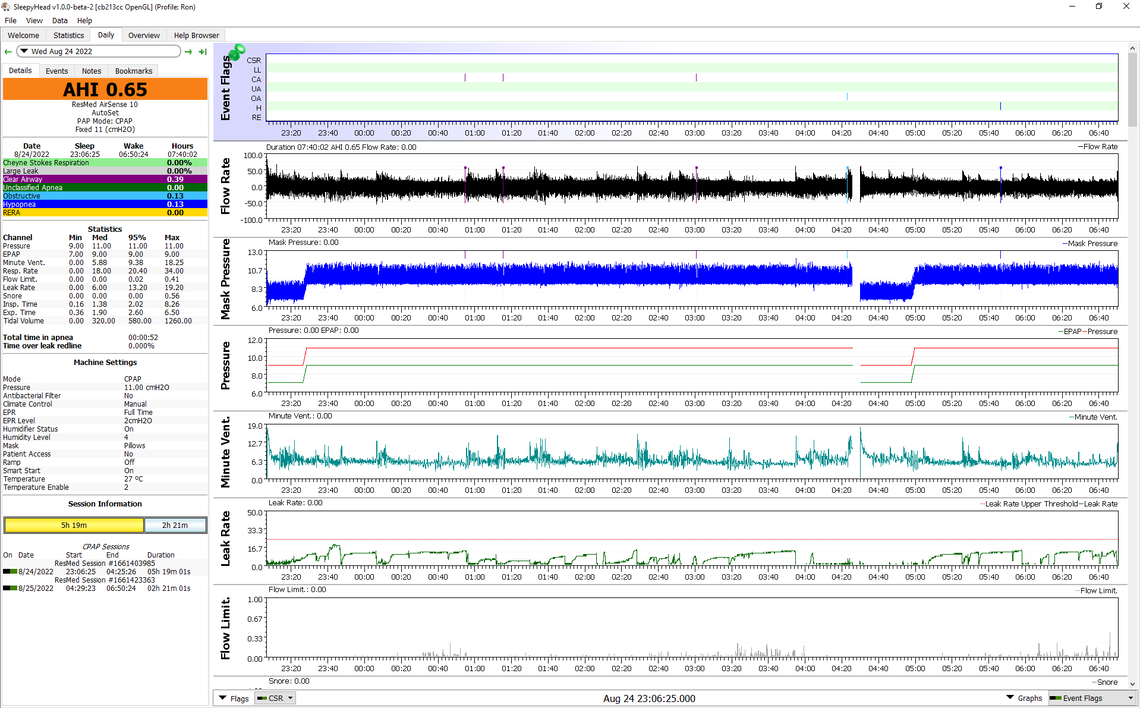
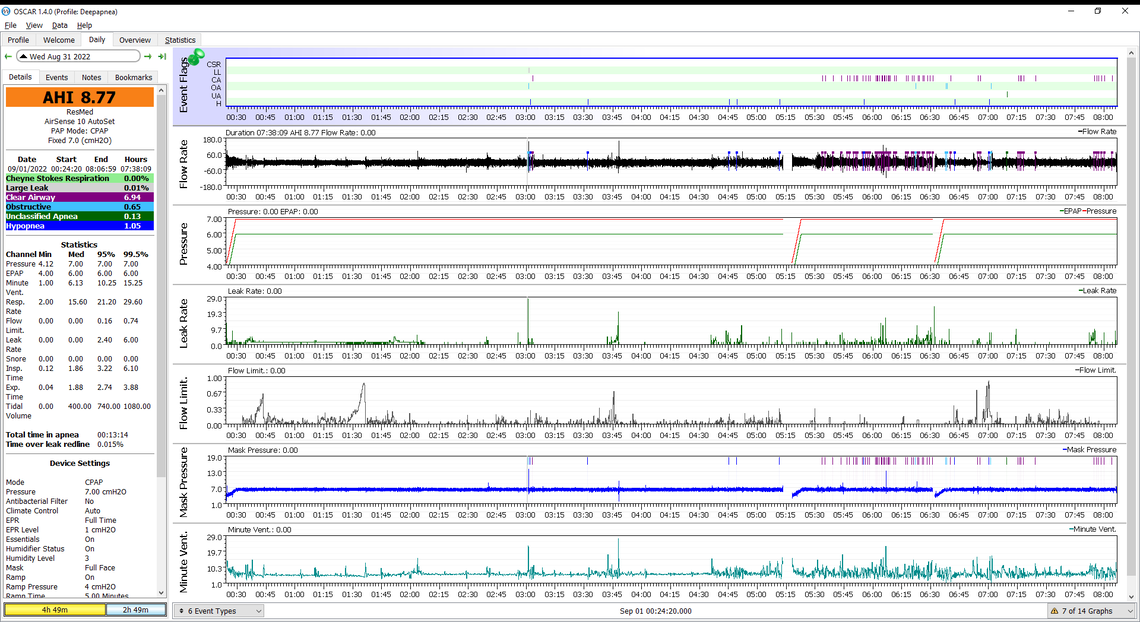
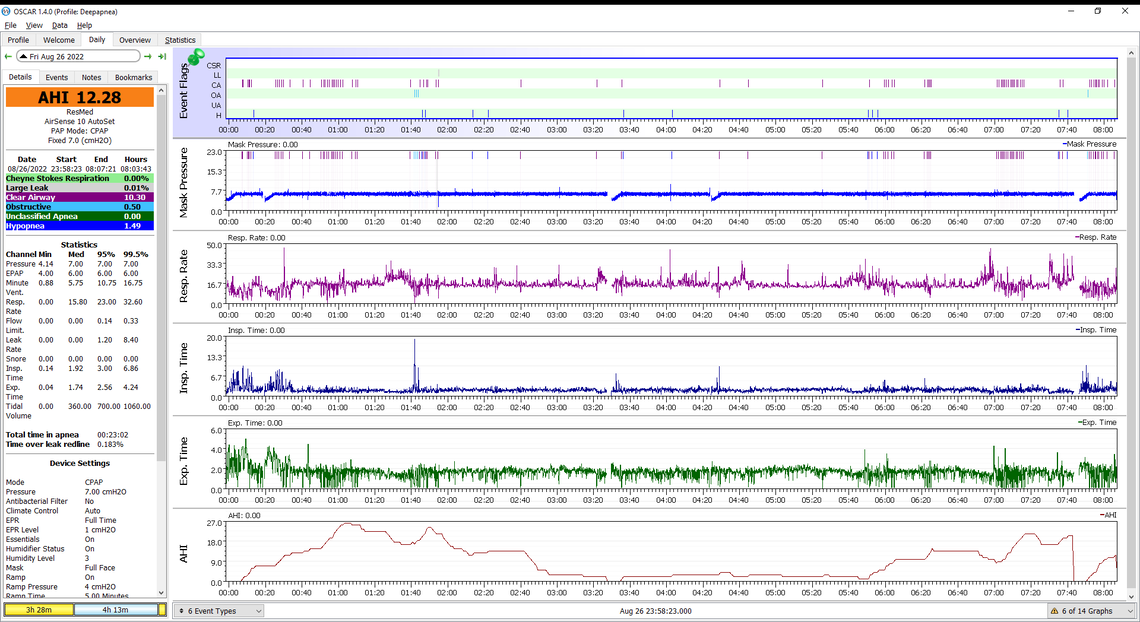
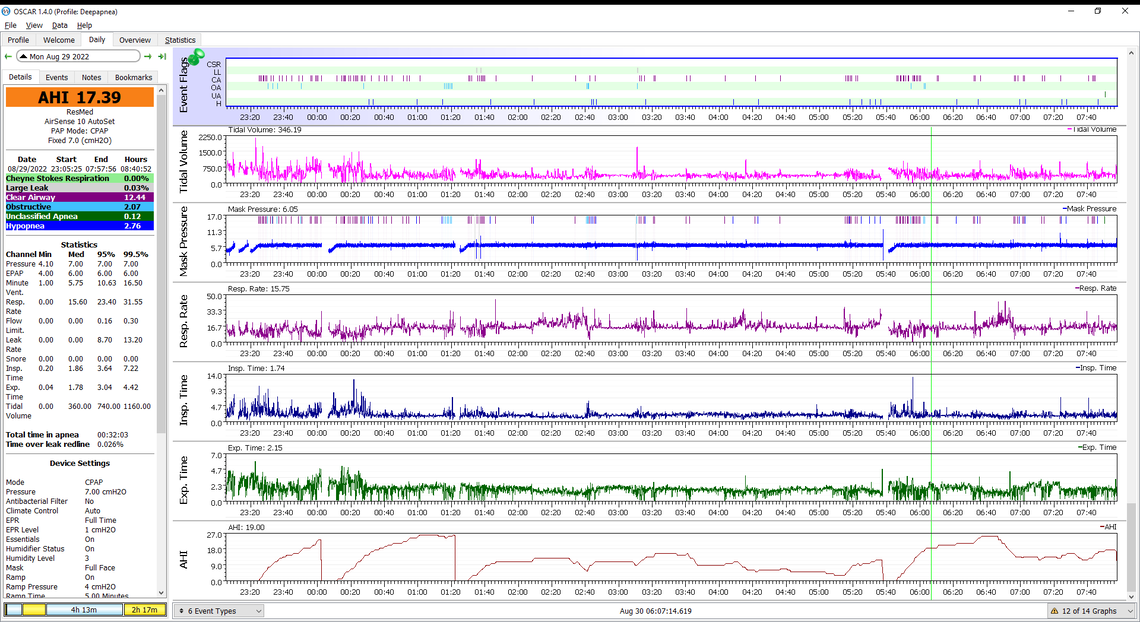
Thanks for your reply, Sierra. I appreciate your comments. Below I have 2 typical daily sreenshots (each divided in 2 parts). One from last night, with 4 pints of beer prior to sleep. AHI flat but rises sharply towards the end of night. The other is a night without alcohol. Typical AHI pattern is stron AHI rise after sleep-onset and also a rise towards the end of night.
For sure the central apnea frequency is an issue of concern. When you were diagnosed what was the breakdown of events in the sleep study? What was the total AHI, and of that how much was CA, OA, and H? The issue is that CPAP treatment pressure can cause the CA event frequency to increase. Here are links to a couple of articles about Central Apnea and Complex apnea (both obstructive and central). You should get yourself up to speed on what it is all about. You then should see your sleep doctor and/or regular doctor. I would print out those Daily reports where there are the high frequency of CA events to show them.
There are a lot of potential causes including medications, heart conditions, living at a high altitude, etc and you should get to the bottom of it. High frequency CA events and CSR can be an indication of underlying health conditions. I noticed in that article on Complex apnea that some get benefit from sleep medications, which may be why you are getting some relief from alcohol. It probably would be much better to go the prescribed medication route rather than alcohol though. I have had central apnea issues and I take a beta blocker drug called bisoprolol. I got the dose reduced and I think it has helped me some.
I would be interested in seeing a zoomed in shot of an area where there are a high frequency of centrals. Just left click repeatedly in that area to zoom in. The arrow keys can fine tune the zoom.
Hi, Sierra, many thanks for your comments and the links.
I could share a password-protected zip file of the entire dataset (165 MB) via tranfernow.net or similar platform that does not require registration. The data set does not seem to include my identity. If you agree, I could send you a link to the file (if this is allowed here) and the password.
I seem to be seeing some interesting patterns in the data.
The big rises in AHI seem to appear right after sleep onset and towards the end of the night. The overview daily screenshot below shows my 3 travels to the toilet and right after that, when I go back to sleep, the AHI rise is clearly seen.
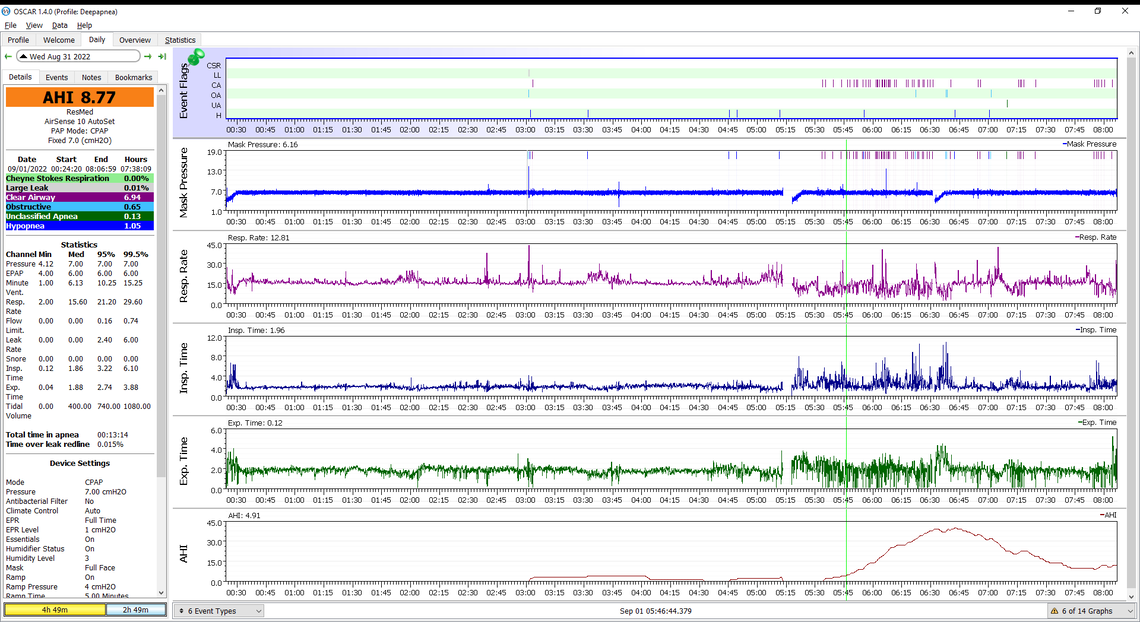
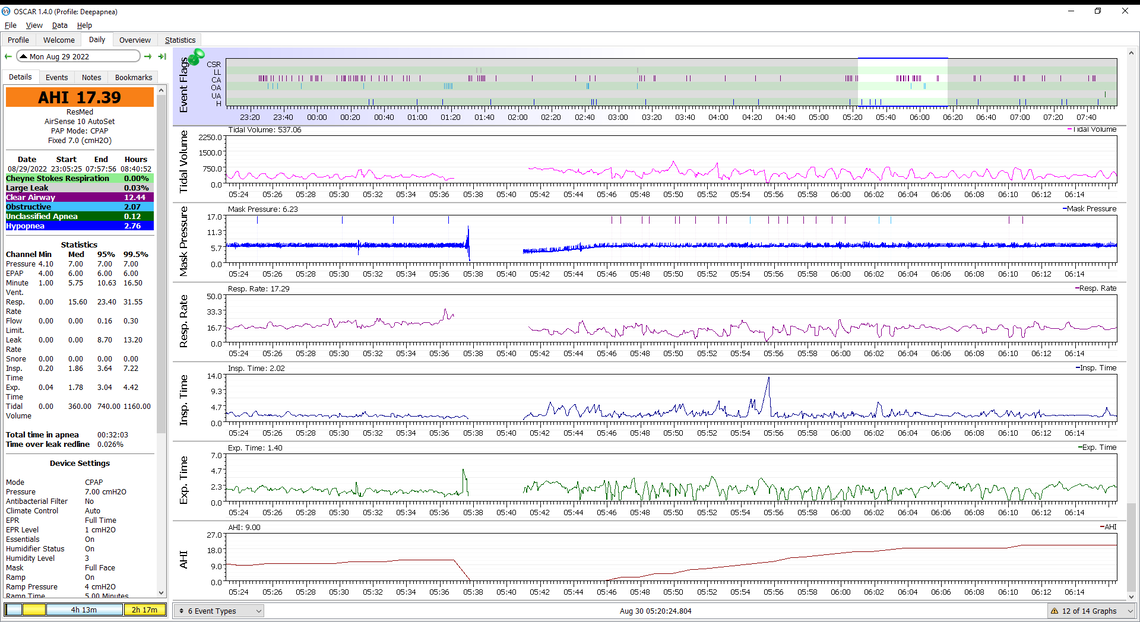
The other screenshot shows the last big rise of AHI around 6pm after my visit to the toilet. What is interesting there is that right after the end of the 5 min ramp period set in the CPAP machine, the expiration rate frequently drops to zero. This pattern seems to be repeating across the entire data set. Maybe I should remove the ramp setting entirely. Also, my expiration rate always is lower then the inhalation rate. Is this normal?
Initially, a polygraph at home put me at an AHI of 37, the first night in the sleep lab came up with AHI=25, after that, 2 nights in the lab were used to determine a pressure of 9 for me. Apparently, at this stage, we talked about 1/3 of apneas being central. When I went back to the lab after wearing CPAP for about 6 weeks, the pressure settimg was reduced to 7 recognizing that central appneas were predominant. Since then I have played a little with the pressure; it is set to 7 now.
I have done a 36h ECG which found nothing except that my heart rate at night is around 50, that is why drugs that further reduce the heart rate are not conisdered at the moment. I will have a head MRI in 2 weeks looking if there are any blood flow issues in the brain. Thyroid is normal so are static ECG and heart ultra sound inspection. Currently I am wearing a 24h blood pressure monitor.
My current hypothesis is that I may have a too low arousal threshold as mentioned in the paper: Breathing Re-Education and Phenotypes of Sleep Apnea: A Review J. of Clinical Medicine P. McKeown et al. 2021
Here is an example of the zoomed in detail that would be helpful to look at. This is from a night where I had quick successive CA events. What you can see on the very left is that my breathing indicated by flow rate was reasonably regular. Minute Ventilation is a measure of how much air is being moved in and out. It was somewhat regular. But then at 6:36 there is a flow disruption. I may have woke up, or had a very brief obstructive event, but whatever it was it started a repeating regular cycle of deeper and deeper breaths and then shallower and shallower, until at some point they were so shallow it gets flagged as a CA event. And, then that repeats causing even more events. In my case I believe this is being caused by my cardiovascular system being too sluggish. Bisoprolol slows the heart rate, and I think cutting the dose of that in half helped bring my heart rate up and increase response. This can also be caused by heart failure, and I hope that is not the case, for either of us! The body depends on CO2 in the blood to determine if the breathing rate is too slow or too fast. But if the response from decreasing breathing rate is too slow the control system can go unstable. It is somewhat like being on cruise control and encountering a hill. The vehicle slows, and the control system applies more gas. But if the application of the gas is too slow you can get to the top of the hill and then there is too much gas for the needed speed. Basic control system instability. The big question is what is the cause of the instability. Alcohol and drugs like Ambien can impact the control system and possibly dampen it to make it stable.
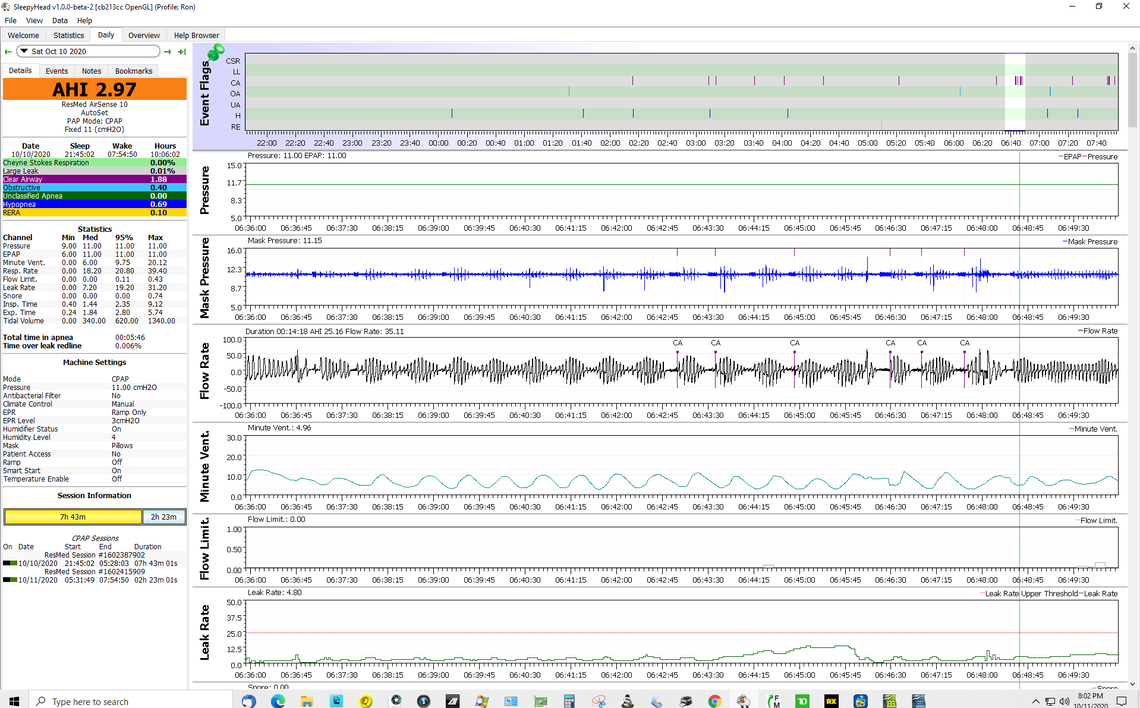
I find the flow rate and minute ventilation the most important graphs in trying to figure out what is going on. If you could post a screenshot similar in layout and level of detail (zoom) to mine it would be helpful. Your underlying issues may not be the same as mine, but that screenshot should be telling.
I am not sure about the arousal level being a problem. I suspect most central apnea has a control system stability issue that is at the root of it. Looking at minute ventilation is the easiest way to see how stable the control system is working for you. Ideally this graph should be a nice smooth flat line.
Thanks, Sierra. Below is the graph. On that night, my average heart rate was 56 and the average SPO2 96%.
My low resting hear rate at night without alcohol is typically 50-55 with alcohol (depending on dose) 60-70. Indeed, there could be another explanation for the odd behavior when I have alc.
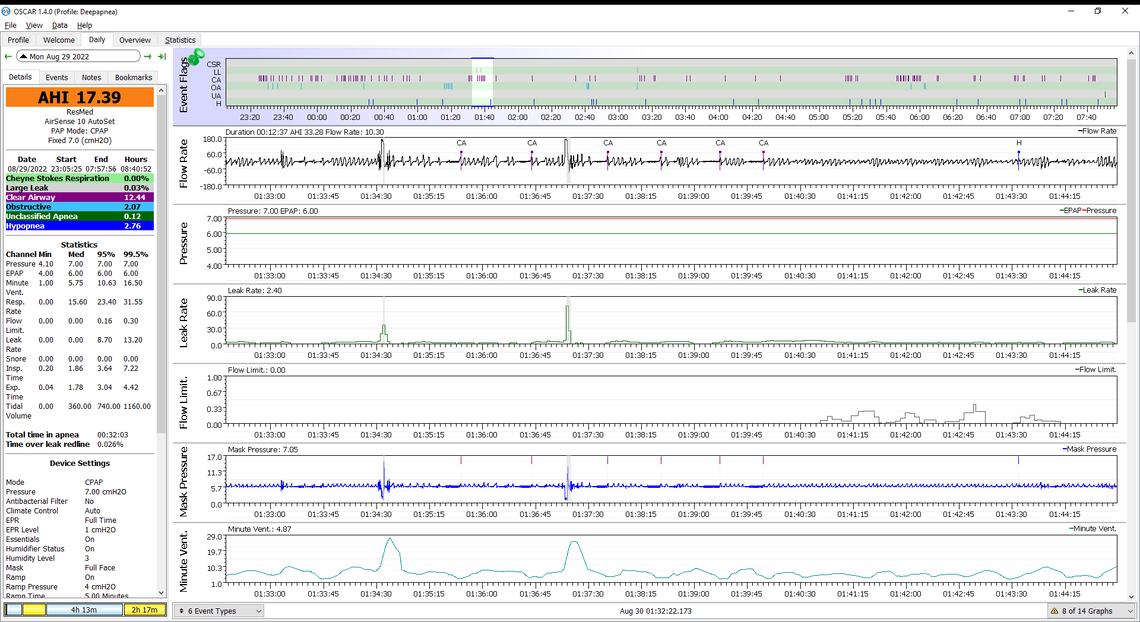
Here is another detailed graph around a CA clutter later that night.
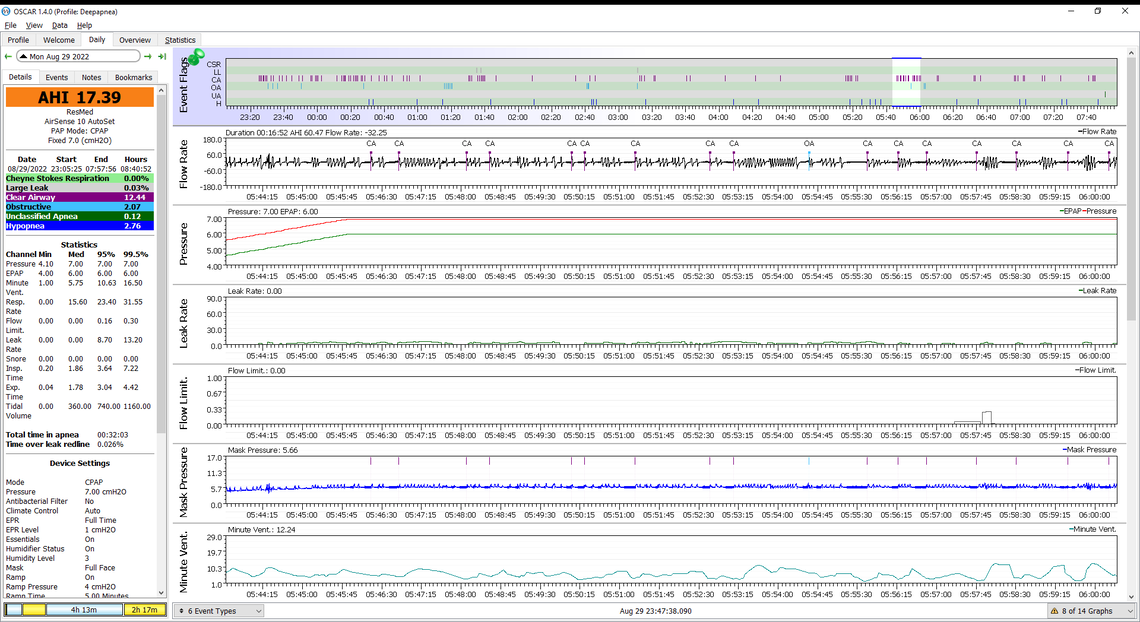
That is interesting and very different from the CA patterns I experience. Now I am not so sure it is a control system problem. That said part of it may be, as those last 4 events on the second graph do have some similarities to mine and indicate a control system issue. As far as CPAP options about all I can see is further reductions down to 6 and possibly 5 cm. The hope would be that it would reduce CA without causing much of an increase in OA events. Beyond that, I think you are best to find a good sleep apnea specialist, and show them what you are getting for results. A central apnea frequency like you have is not really acceptable, and you need to get to the bottom of it. Acetazolamide which is prescribed for altitude sickness and is off label for central apnea treatment, has worked in some cases. You should ask about it when seeing a specialist. See this article:
The role of acetazolamide in sleep apnea at sea level: a systematic review and meta-analysis
Another kind of last resort option may be to investigate use of an Adaptive Servo Ventilation machine instead of a CPAP, They go beyond just using pressure to keep the airway open, and adjust inhale and exhale pressure on a breath by breath basis to maintain regular breathing. ResMed makes one called the AirCurve 10 ASV which looks very similar to your A10 machine, but operates in a much more sophisticated way. It essentially forces you to breath regularly. Phillips also make one that some claim is better. I have not done much research on them, as I have managed to solve my issues with just the regular A10 machine by using a fixed pressure of 11 cm, and adjusting my beta blocker med.