I recently brought to my doctor's attention that there seems to be an inverse correlation between masks leaks and AHI events. More specifically, I took five days with the highest AHI's and five days with the lowest AHI's and I found out that in all five sample-days the lowest leaks ( under 20 l/m) invariably yielded higher or higher -than -my-average AHI's ( 3-7 AHI's) while, conversely, the occasional highest leaks ( 30-70 l/m ) yielded AHI's within my usual low average ( less than 1.5).
The doctor found my observation very pertinent ( he qualified it as "intelligent.."). In fact he evinced from the Resmed report that, no matter my low average AHI rate, often my air ways are still obstructed more than they should and gave me a prescription to increase the CPAP air pressure from 9-15 to 12-16. He said this would take care of the occasional slight head=aches and sweating at wake-up, caused by the AHI's.
He then went on to explain that the airway obstruction creates a pressure build-inside the mask and the machine reacts by automatically evacuating the excess pressure as a mask leak.
This explains the occasional high-leaks, but not the inverse correlation. In fact I would have thought that the airway obstruction should always yield a high-leak rate. He tried to explain this over the phone, but it was getting a bit technical and we were short of time. Can anybody comment on this?
Thanks
Ittiandro
First on the high leak rate correlating with lower AHI I would suggest one possible explanation is that on ResMed machines they suppress the reporting of apnea events when the leak rate is over the redline. So you may in fact be having them while the leak rate is high, but they are not being reported. I believe you are using OSCAR. If you go into a day where you have high leak rates you can scan across and see if there are any reported events during the grayed out periods of time where the leak rate is high. I suspect you will not find any flags for events. I reviewed several days of where I had high leak rates and could not find any. Here is an example.
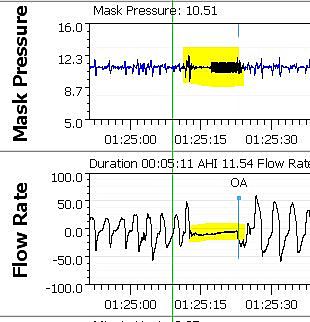
See the area I have zoomed in on. There is a CA event right before the high leak rate grayed out time, and two hypopnea events after, but nothing during the high leak time. This does not mean there are no events, it just means they are not being flagged. I further zoomed in on this period of time to see if I could find any events. See this further zoomed in screen shot and in particular where the green vertical cursor is located. That has all appearances of being an apnea event but was not reported.
If you go through a similar process of looking through your results during high leak times you may find something similar.
With respect to the thought that obstructive events causes mask pressure to build up and cause leaks, I have never seen that. If you look at the mask pressure trace in the screen shots I posted above there is no indication that mask pressure increases during a high leak event. Remember that your mask has a fairly large vent flow that is always venting air even when you are inhaling or exhaling or during apnea events. The fan in the machine increases and decreases in speed to maintain the mask pressure constant. There is always some fluctuation of pressure with each breath and during an apnea event this fluctuation may even decrease. There is no need for the mask to leak during an obstruction event as that is the purpose of the mask vent.
If you want to post a daily report of a typical night I could comment on the pressure issue. Ideally post one from before the pressure adjustment. Whether or not a pressure increase would be helpful depends on the types of events you are having and when during the night they occur. But if you post I would be happy to comment. When you have the screen displayed, assuming you have a PC, just press F12 and take note of where the screenshot is being saved. Then use file explorer to find the file, left click on it, and then drag it to an open post here. It will be copied into the post.
Hope that helps some,
Hi
thanks for your reply and your offer to review some of my Oscar reports. I don’t know how to attach them, though. I have no IMAGE files for them, only PDF documents. If you want, I can e-mail them to you. Or you can give me instructions.
In the meantime, I’d like to comment briefly on your reply, with a few questions, so that I can better understand how to read the reports .
It is fascinating, but a bit challenging as I am neither a doctor, nor a technician with biomedical background ( I can read much more easily… ancient Greek than matters pertaining to medical technology ..)
First off, I have compared both the Oscar and the ResMed reports . Indeed, that inverse correlation holds for both. You were right, there are no AHI’s in the report for the hourly time windows of the large leaks. Why so ? How reliable then are these reports if they miss some AHI’s? .
Let me say, though, that I find it difficult to understand why both Oscar and ResMed should exclude from the count the AHI’s occurring when the leaks are large. Why should these AHI’s be of a lesser value in the overall clinical appraisal of the report, to the point of ignoring them?
In fact, I find it a bit intriguing that my doctor would want to increase the pressure setting in spite of the very low AHI readings. I simply told him that occasionally I still wake up in a light sweat and a slight head ache. So he must have sniffed something else, in spite of the very low number of AHI’s. …
May be I misunderstood the explanation he gave me, which you yourself question, but my doctors’ explanation went at least some way to explain the correlation, rather than simply saying that both Resmed or Oscar have deliberately designed the reports to ignore AHI’s when the leaks are large. If so, the question is, again, why? Perhaps there is a scientific explanation....
Secondly, why do you say that in the 2nd report with large leaks that you zoomed on there must be some AHI’s that are not shown?
Thirdly, I assume that perhaps the duration of the AHI’s is more important than their number, but where is the duration of each AHI occurrence ( or the total duration) shown?
Lastly, in my reports which you will hopefully receive, the mask pressure graphic shows as “plots disabled “ Why ?
You may want to have a look at these issues. I’d really appreciate.
Thanks
Franco V.
Are you using a PC or Mac? Let me know and I will be able to help you more on how to post your OSCAR Daily Report here.
On the question as to why ResMed ignores the apnea events during high leak times, the reason I have read from ResMed is that that the leak interferes with their ability to distinguish what type of apnea event it is. They take the approach of not reporting them rather than reporting them wrong.
On the identification of events what ResMed does is speed the fan of the CPAP up and down quite rapidly to see how the pressure responds. If the airway is closed (OA - obstructive) the pressure goes up and down quite a bit in sync with the fan speed. If the airway is open (CA - clear airway or central apnea) then the pressure does not cycle up and down so much.
To zoom in on a event you just left click on the events bar near the event. Repeated clicking zooms in more and more. The other way is to use the up and down arrow keys.
Here is what a central event looks like. See the highlighted area. After 4 seconds of no flow the machine starts to cycle the fan speed. Notice the width of the mask pressure (blue) cycle.
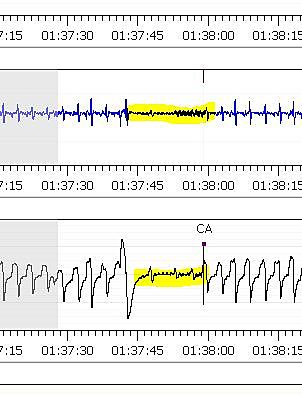
Now here is an obstructive event. Note that the blue mask pressure cycle is much more and paints a wider blue band.
That is what you are looking for.
If you look on the left of the OSCAR Daily report screen you will see four tabs named Details (default), Events, Notes, and Bookmarks. The Events tab will identify each event during the night and how long it lasts. Higher up if you go to the Overview tab instead of the Daily one you will see a graph of the Total Time in Apnea. It is somewhat useful as it adds up the time you are in apnea rather than the number of events.
In any case if you post what type of computer you are using I should be able to explain how to post your daily report screen.
Thanks I am on PC, Windows 10 32-bits. Here are some more points.
1.The term AHI is, from what I understand, an umbrella term including a variety of apnea events, like O.A, Hypoapnea, Central Apnea and others. To be able to identify them individually is essential, but if Resmed, to this purpose, removes the AHI’s from the report in case of large leaks, will these individual apnea modes be still traceable? If not, won’t the reports be unreliable, if they don’t show the correct number of AHI events?. It is a bit like deleting a folder from the computer: all the files it contains will also be gone.
I’d would think that OA has perhaps the greatest impact, but perhaps other apneas are just as important..
My AHI’s have drastically gone down, in the average, to well under 2 /day over one year. . Sometimes there is none and sometimes, very rarely, they spike to 6-8 in one night. Looking at my reports, I found that the OA’s represent about half of my AHI’s. and this raises a few questions.
Of course, if the AHI’s for the night are down to one or less, the OA component becomes insignificant. When, however, the AHI’s are six or eight and half of them are OA’s, I wonder if there isn’t a more serious impact on health.
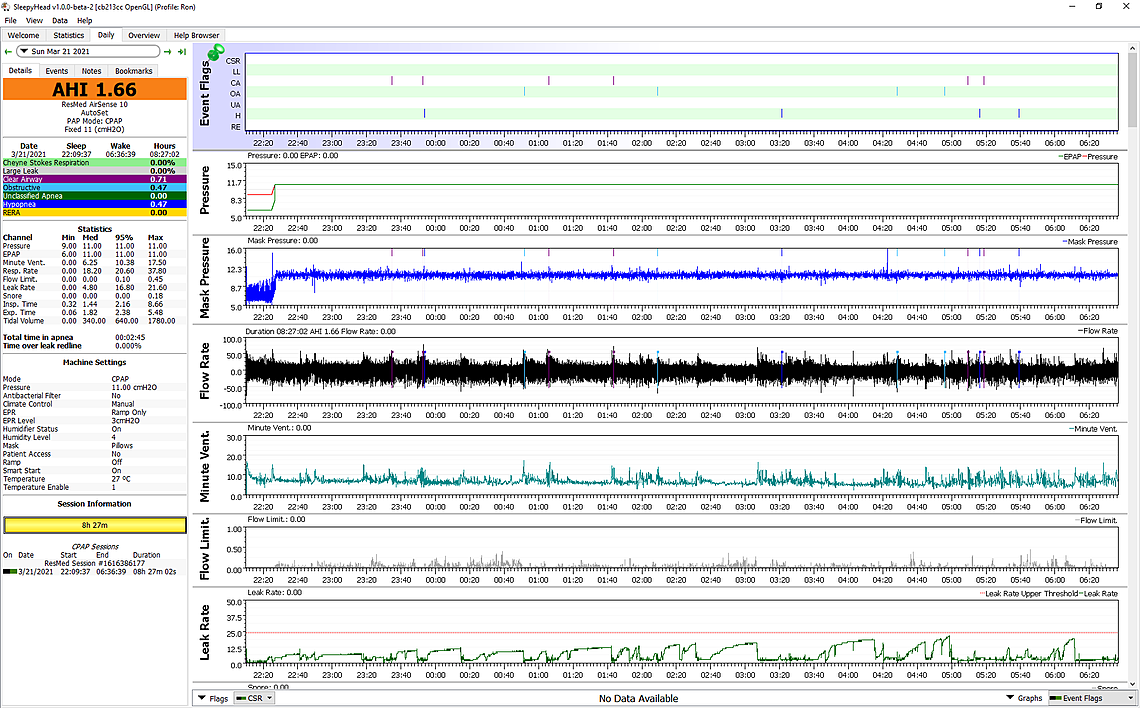
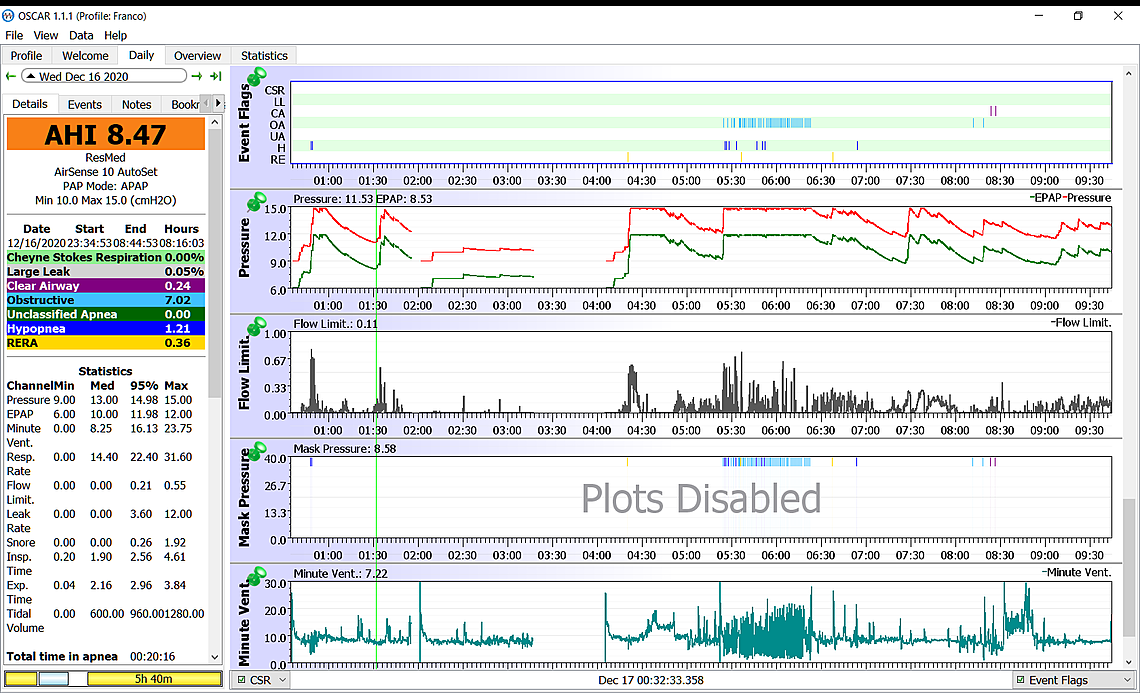
The report of 12/22 , which I will attach as soon as I know how to do it, shows for example 8.47 AHI’s, of which 7.02 ( practically 90%) are OA’s. Considering the TTIA for the night ( about 20:min), each OA had a duration of 2.85 min. A lot! . Of course, I didn’t stop breathing foe almost 3 min, or I’d be dead, but 20 min. of OA’s events shouldn’t perhaps be underestimated. This may be why my doctor has decided to increase the pressure.
3.I’d also like to have your take about the possible connection between sleep apnea and cardiac arrythmias. Can sleep apnea cause arrythmias?.
Two years ago, before being treated for Sleep Apnea, I had an episode of Afib, when I was about to begin my usual 6 km running session . I am 79 and it was the 1st time. The cardiologist put me on betablocker ( Metaprolol) as a precaution, but I had a 2nd episode a few days ago, with the pulse briefly shooting up to 160 bpm, with absolutely no discomfort, though.
I spoke to the doctor again. In the meantime my heart had gone back to normal, except that I have a lingering arrhythmia, with the pulse fluctuating between 90-110 bpm ( it usually is 60 bpm at rest ) , It doesn’t go away. I don’t even feel it and I can detect it only with the cardio watch, but it is still there.
If it it doesn’t go away, I’ll speak to my doctor again, but I wonder if arrythmias are an expected… byproduct of Sleep Apnea.
Thanks for your input, as usual
Ittiandro
Good that you are on a PC. That makes it much easier for me. First the process to include a Daily Report screen shot in a post here:
That is basically it. Don't drag more than one of these images into the post, or it may get hung up in the spam filter. Just pick a good one to look at, with more events -- a night of concern.
Will answer in more detail when you post your Daily Report, but a few quick comments:
AHI is basically the CA+OA+H events added up. There are RERA events which get flagged but not included. There are very occasionally Unidentified events (green colour I think), and I am not sure they get included or not.
My view is that OA and CA events are equal in severity. No airflow goes in or out of the lungs during the event. Hypopnea events are less severe as there is partial airflow in and out.
The main issues are OA and CA events. They are equal in severity but differ greatly in cause. More pressure can keep the airway open and reduce OA events. However more pressure does not help with CA events as the airway is already open. For reasons that can be complex the body just decides not to breathe. And again for complex reasons more pressure can actually increase the frequency of CA events. That is why I would like to see your Daily reports before commenting on the value of increasing pressure. When you have both CA and OA events the pressure can be a balancing act. Not too high and not too low...
Actually when the OA event lasts for 3 minutes you really do not get any oxygen for 3 minutes. If you zoom in on a OA or even CA event by left clicking to see the detailed flow for each breath you will see that airflow goes to ZERO. That is why apnea is a problem. If you were to use an oxygen monitor you would see oxygen saturation in the blood drop significantly during an event.
I am 71 and like you I have had issues with irregular heartbeat. Mainly for blood pressure issues, but also to deal with the heartrate I take bisoprolol. Is is very similar to metoprolol but lasts longer and is more uniform in effect. I became concerned that it was causing more CA events, as it slows the heartrate. I discussed with my doctor, and although I don't think he was real convinced I got him to reduce the amount in half. I think it may have helped reduce the frequency of CA events. Something to discuss with your heart doctor.
Do you ever get areas highlighted in green on your OSCAR report. Those are indications of Cheyne–Stokes respiration. It also can be associated with an irregular heartrate. It can also generate a whole series of CA events. Something to look for on your OSCAR daily reports.
Hope that helps some for now. Post a Daily report and we can go from there.
Thanks so much I think the most interesting reports to look at are those showing an unusual high number of AHI’s ( up to 8) and consisting of a majority of OA’s ( up to 90%) or a 50/50 mix of OA’s. and CA's. Given the TTIA and the relatively high number of OA’s and CA's making up the mix, I believe that in the long run there is less oxygen going into my system at night and this may have some effects, like arrhythmias or other .. I’ll send you the report as soon as I have sorted out the nuts and bolts of how and what to post. Getting there. Please bear with me…
The mask pressure has been increased by the technician ( 12-16) according to the doctor's prescription, effective tonight. I'll see. I hope it won't feel like snow blower into my throat. I had enough of snow and ..snowblowers here in Montreal.!. .
Thanks
Ittiandro
I would post the Daily screen only and for a start a day when AHI is higher and has a balance of OA and CA events. This is an example of what it should look like and which graphs to include. You can move the graphs up or down by left clicking on the title and dragging them up or down. Also if you click on the black triangle beside the date in the top left corner you can hide the calendar to save some space. Also under File, Preferences, Appearance, you should uncheck the box that says "Show event breakdown Pie Chart". It is redundant and takes up useful space on the left. Last if you press F10 you can hide the Navigation bar on the right to gain more screen space. I find the bar to be just in way, and not helpful.
When you have a mixture of OA and CA events it is sometimes called Complex Apnea. And, it is quite complex. Your body uses carbon dioxide in the bloodstream to regulate breathing. I'm sure I am over simplifying but when your overall blood circulation is low the regulation of breathing can be unstable. The depth of breathing can go too high, too low, too high, and so on. Between these cycles it can stop causing an central apnea event. Exactly how it happens is not fully understood, but a CPAP can also upset the carbon dioxide levels and aggravate the instability. The higher the pressure used, the worse the problem can be.
In any case post your Daily report and then I can comment better.
Here is one report. I was unable to include the leak rate graphic. I hope it won't matter. There is also a 2n one with a different mix that I'd like to send, but it won't go through on the same post.
Thanks
Ittiandro
First on the Mask Pressure Plots Disabled issue, you could try going to File, Preferences, and the Waveforms tab. There is a box to check to restore the defaults. That may be worth a try. I checked my SleepyHead and all boxes on the left are checked off. The second thing you could try is upgrading to the latest version of OSCAR which is 1.2.0. Make sure you download the version that matches your 32 bit Windows operating system. The latest version is at this link. Or, you could try clicking on Help in OSCAR and see if there is a Check for Updates option which may let you download it that way. On a quick search I saw some indication that your issue may be a bug in OSCAR, and the later version may fix it.
Comments on the daily report:
Those are my initial thoughts. If turning the Pressure Relief off works to reduce events, there is a more sophisticated way to disable it when you are sleeping but still have it active when you are going to sleep. Let me know if you are interested in that. Here is a Clinical Guide PDF for your machine to read if you want to understand what all the options are.
Hope that helps some. If you have questions just ask.
Here is the 2nd one
Thanks
Franco
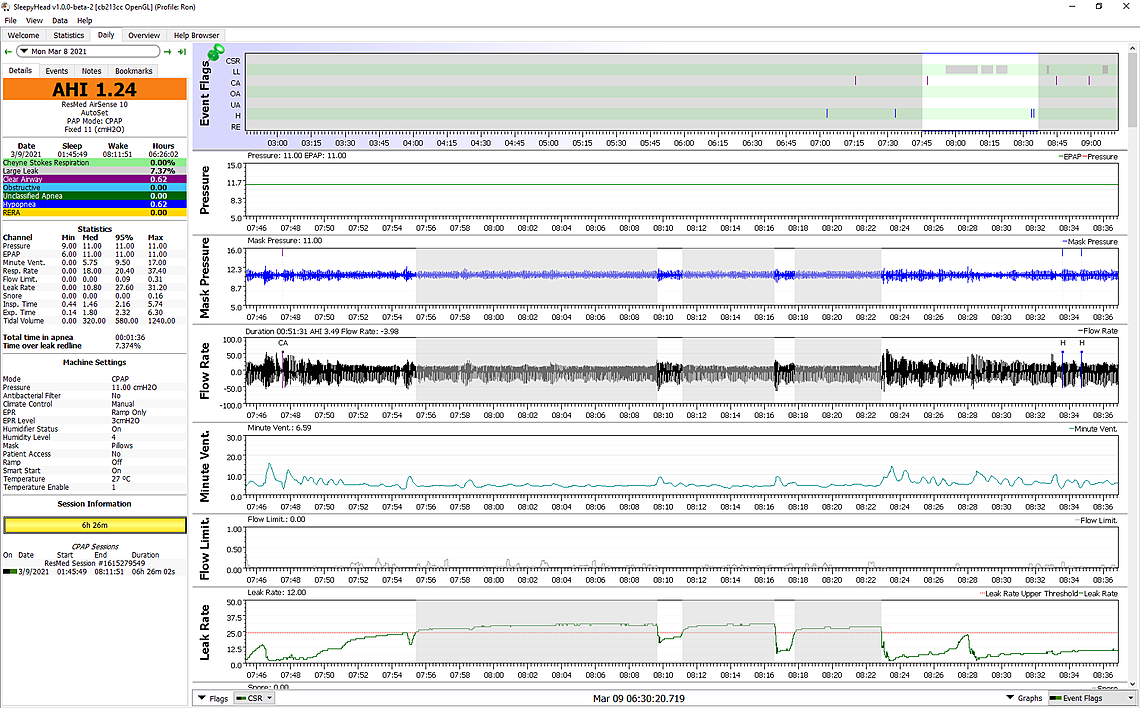
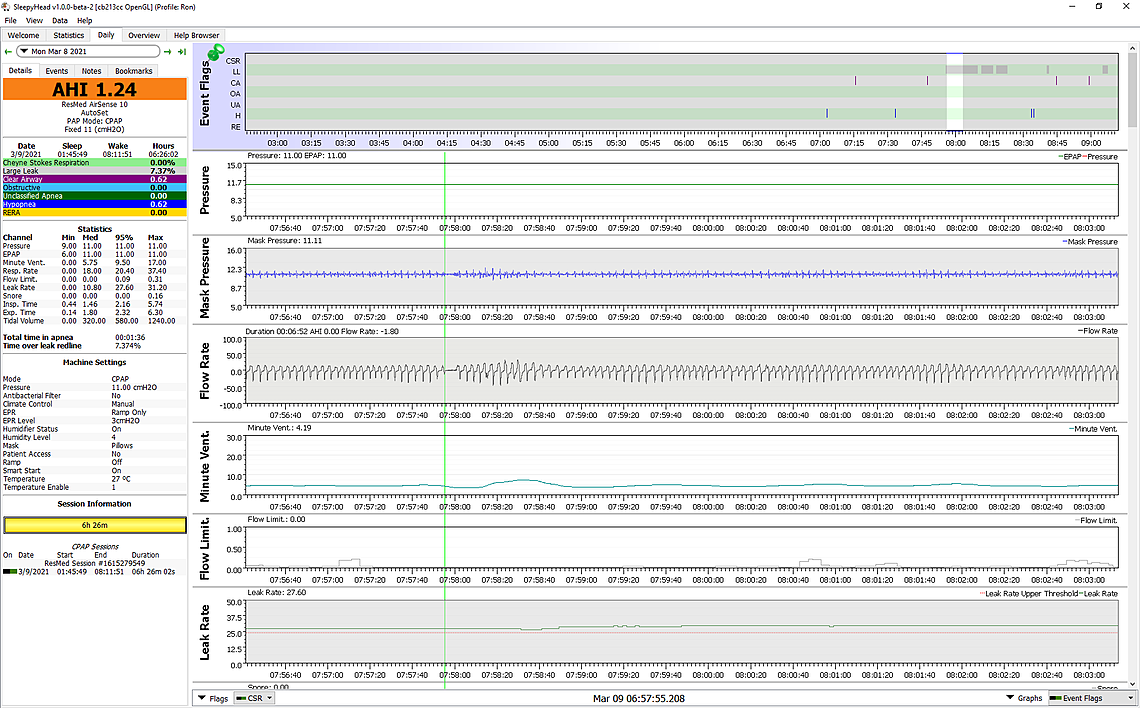
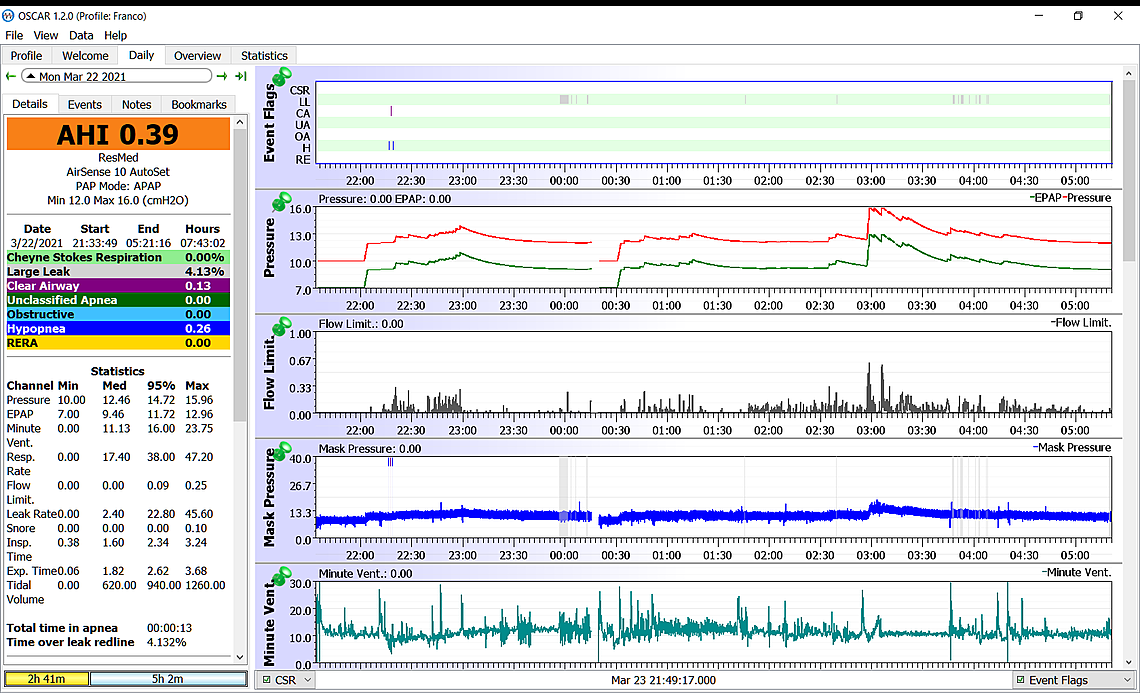
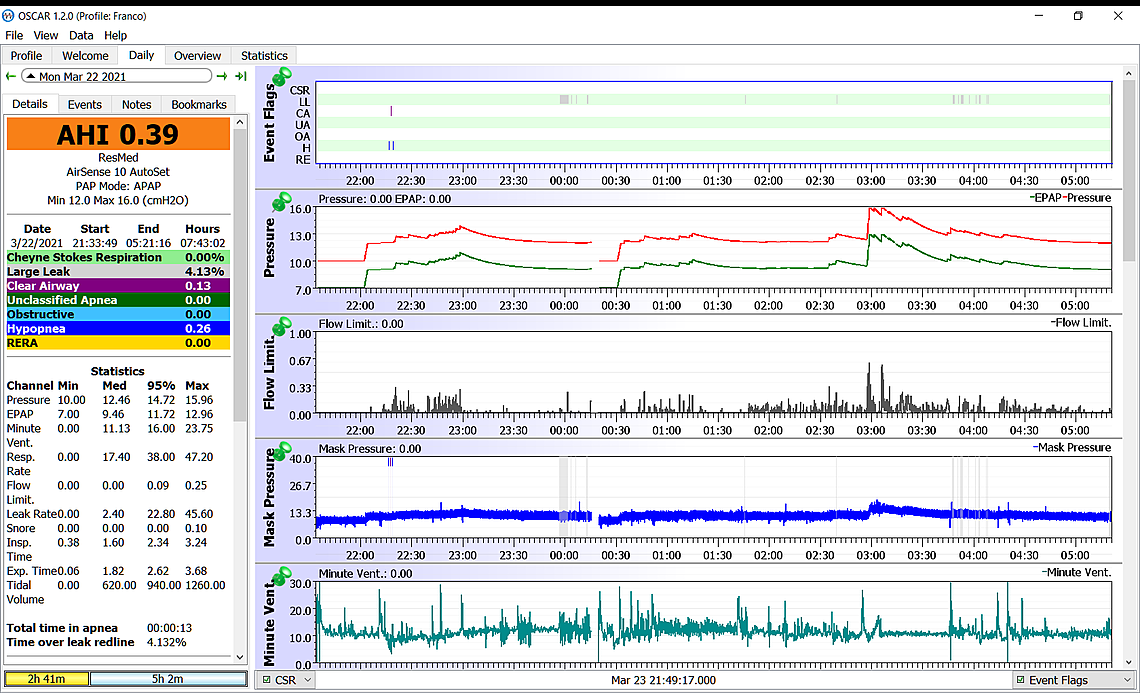
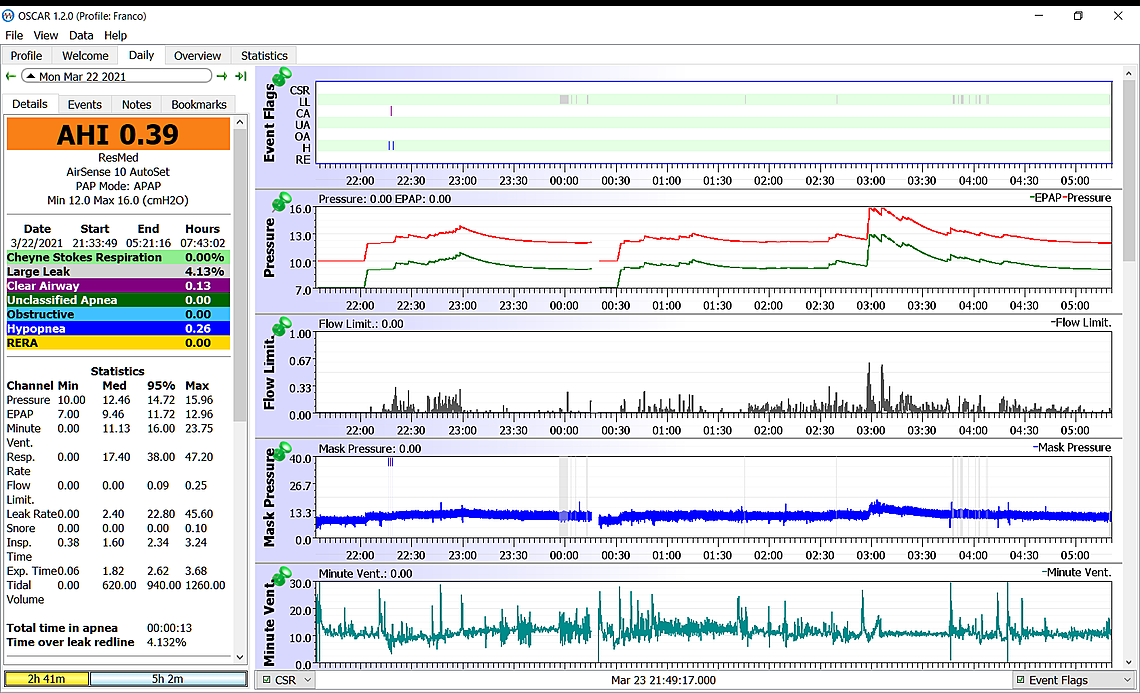
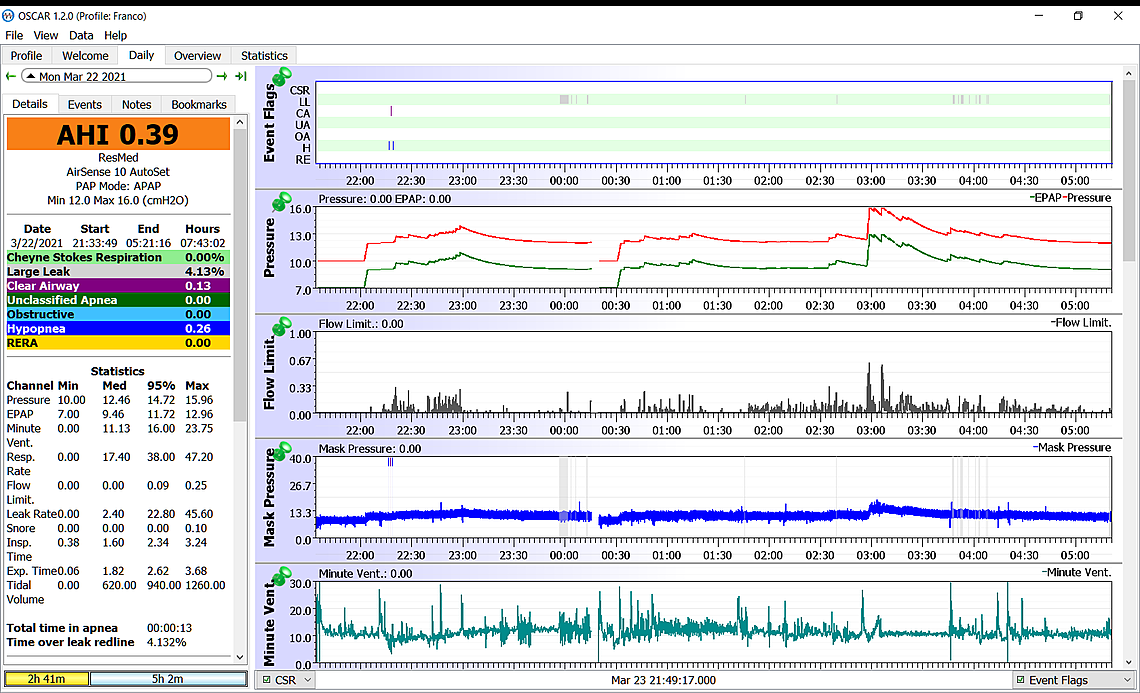
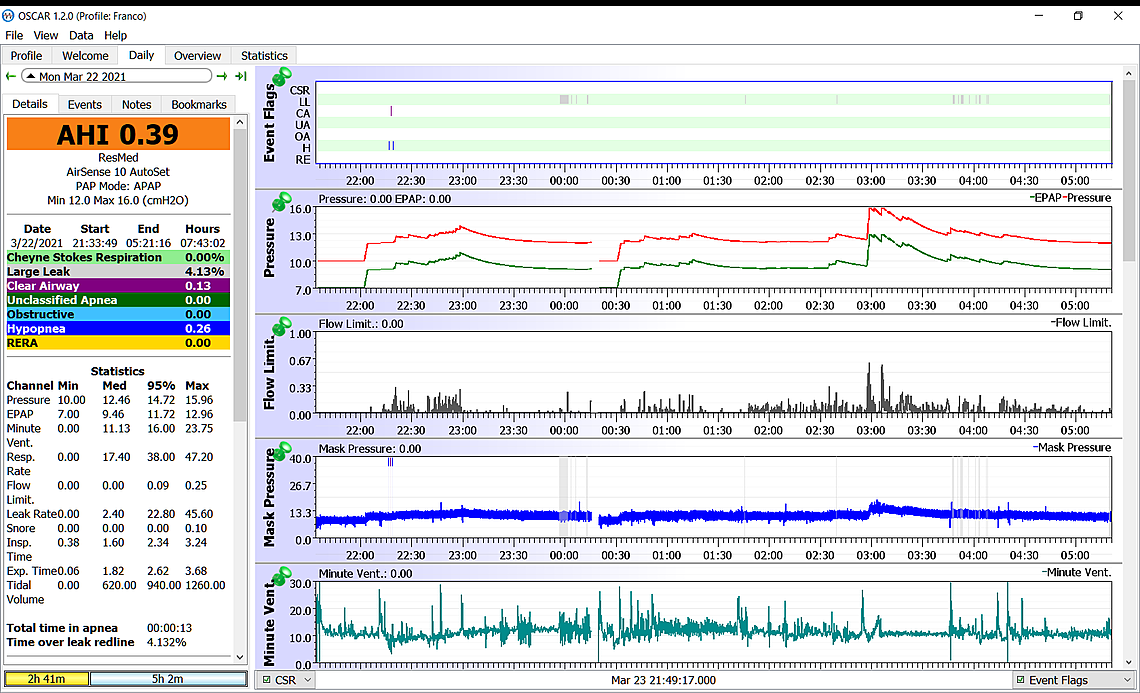
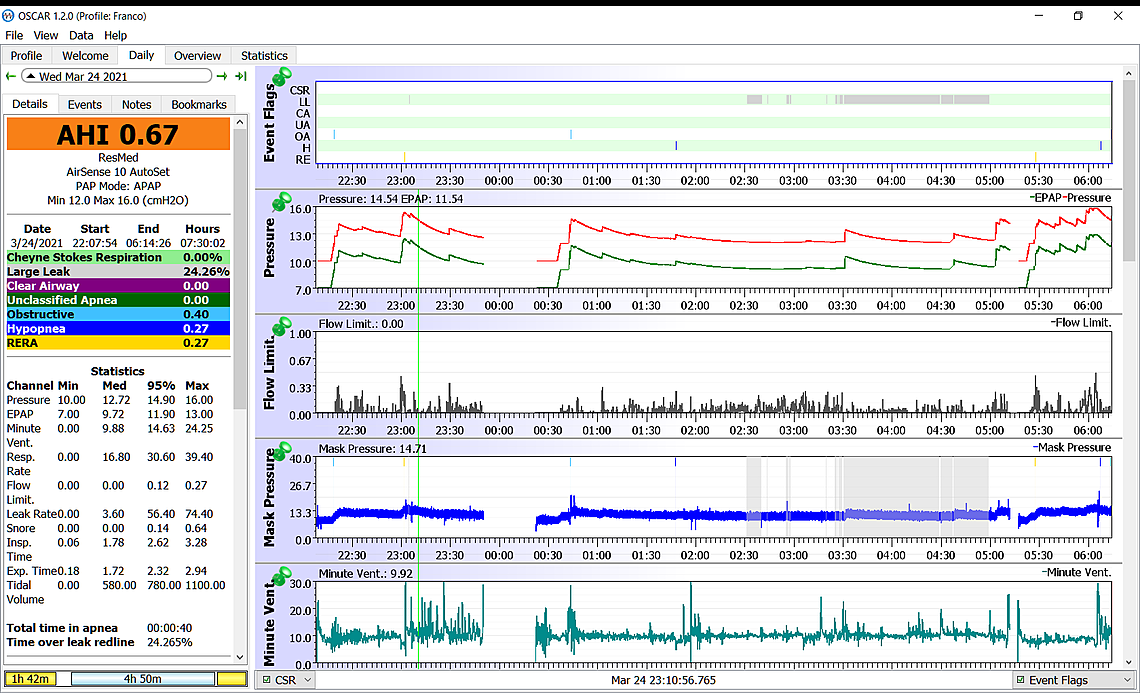
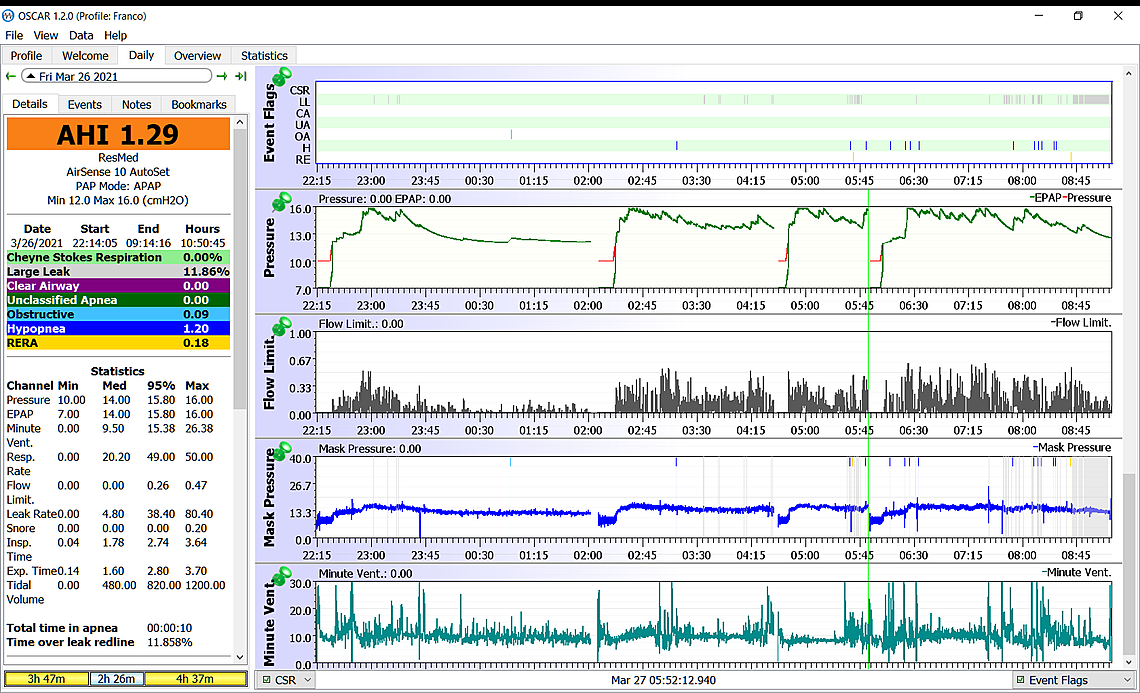
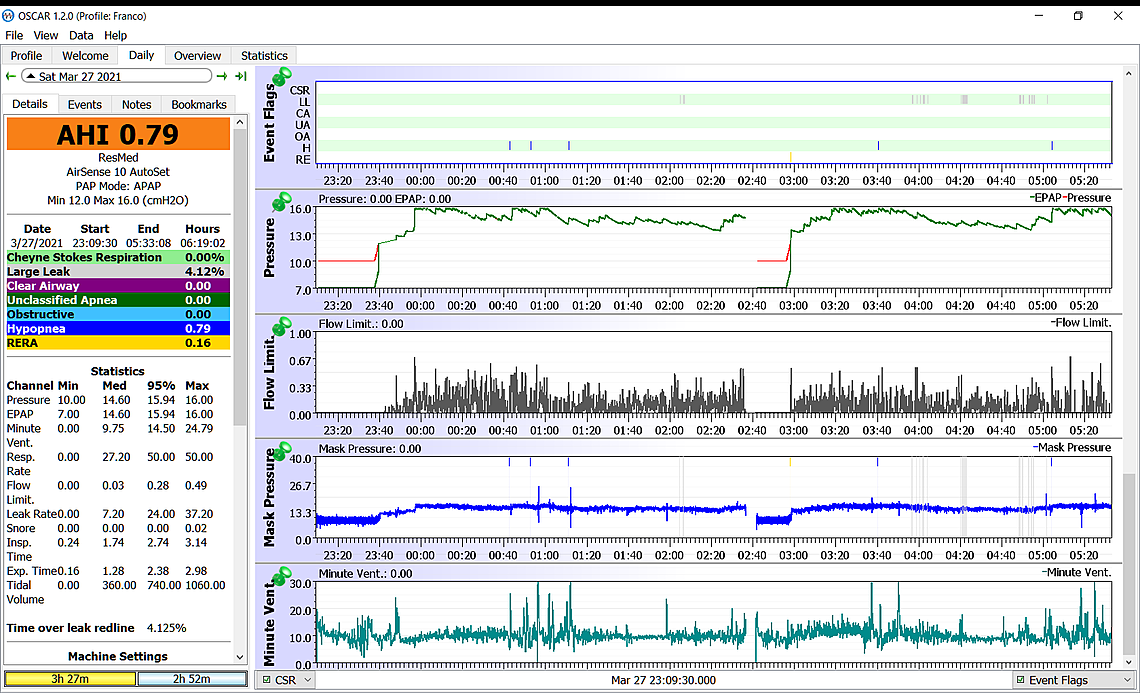
This Daily screen is also showing similar issues of many obstructive events when the inhale pressure is maxed out at 15 cm. The good news here is that it does not seem to be creating central apnea events. They are much more difficult to deal with.
This report does however show a period of Cheyne Stokes Respiration (CSR), which is the green highlighted area. You may want to zoom in on that area to see what the Flow rate graph looks like. Notice that the Minute Ventilation is also going up and down quite a bit. Ideally the Minute Ventilation should be a fairly smooth level line indicating your breathing rate is stable. I would be worth looking at your Statistics to see how often you are having CSR. It would be also worth discussing it with your heart doctor especially if it is happening frequently.
Again, I hope that helps. Any questions just ask.
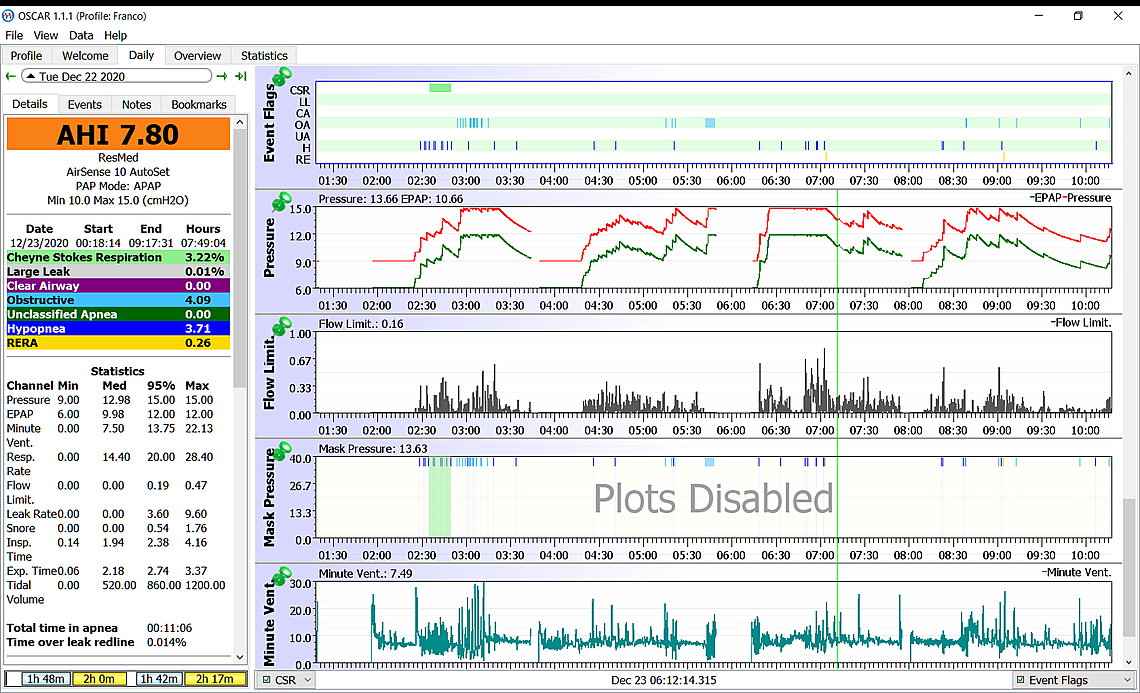
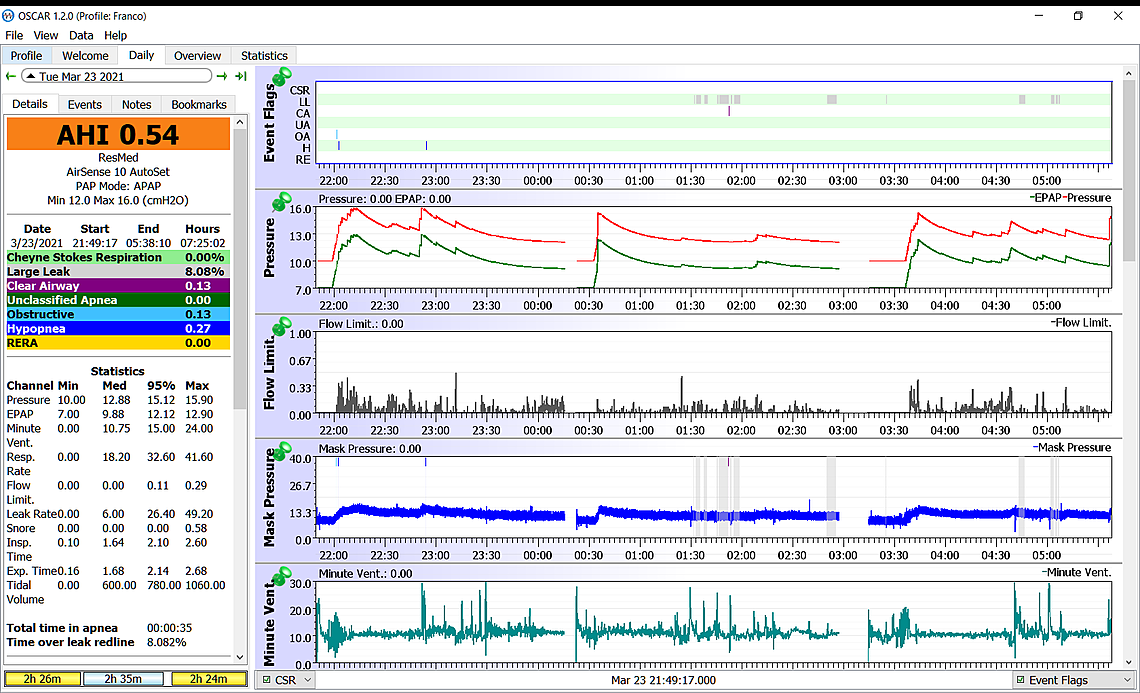
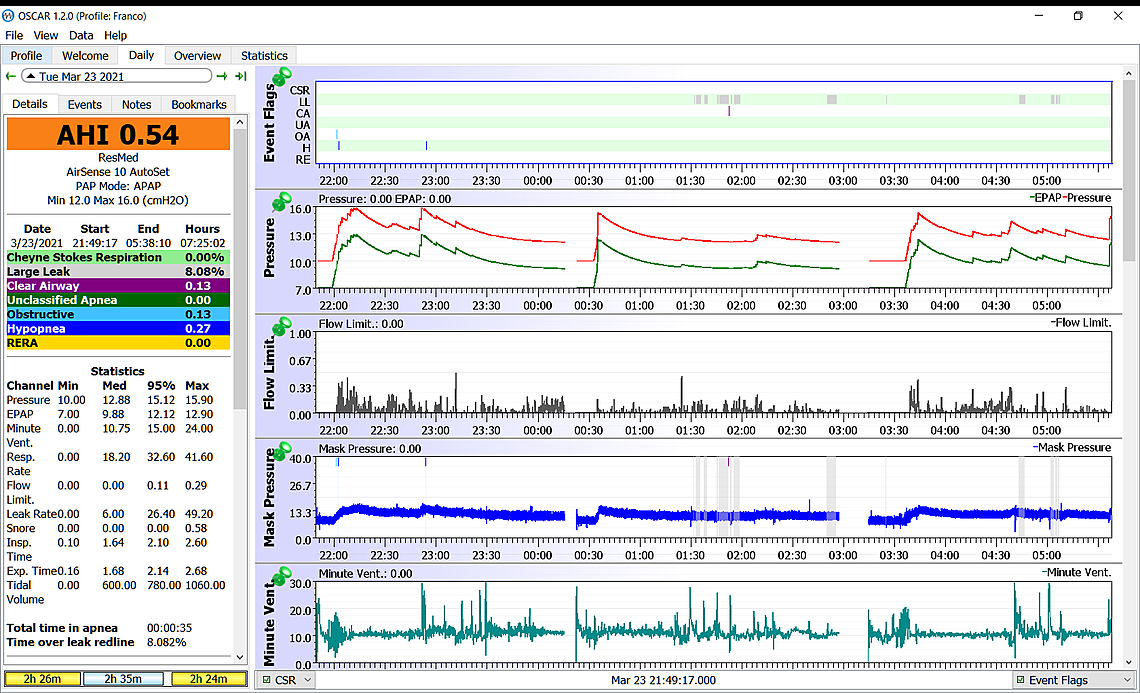
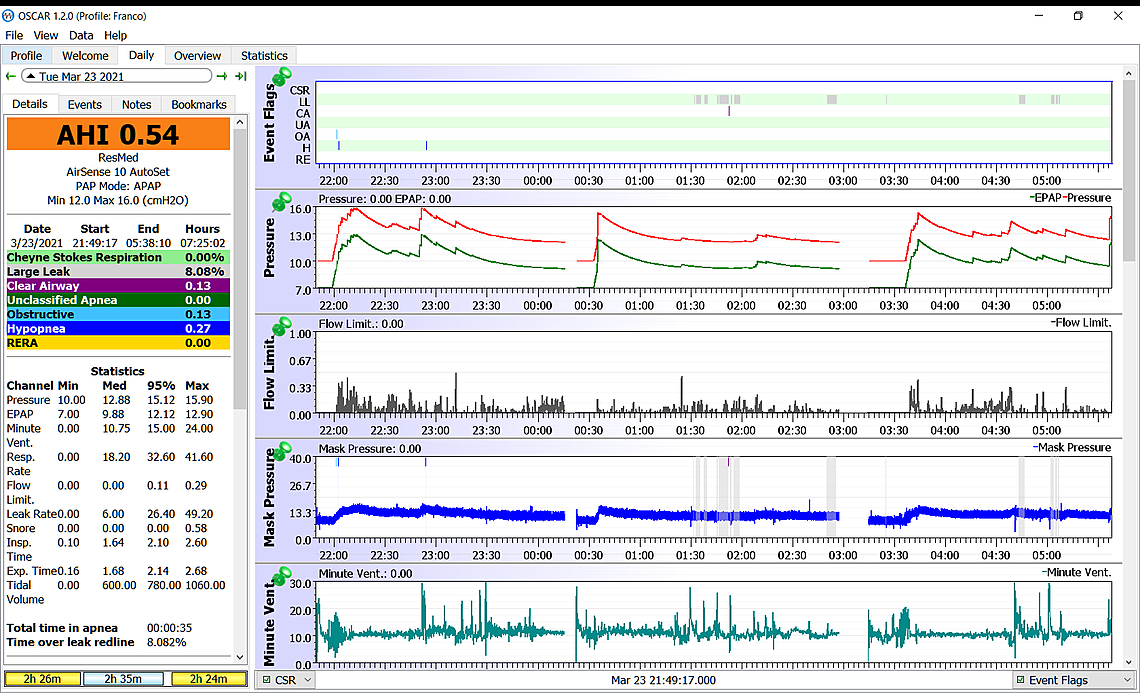
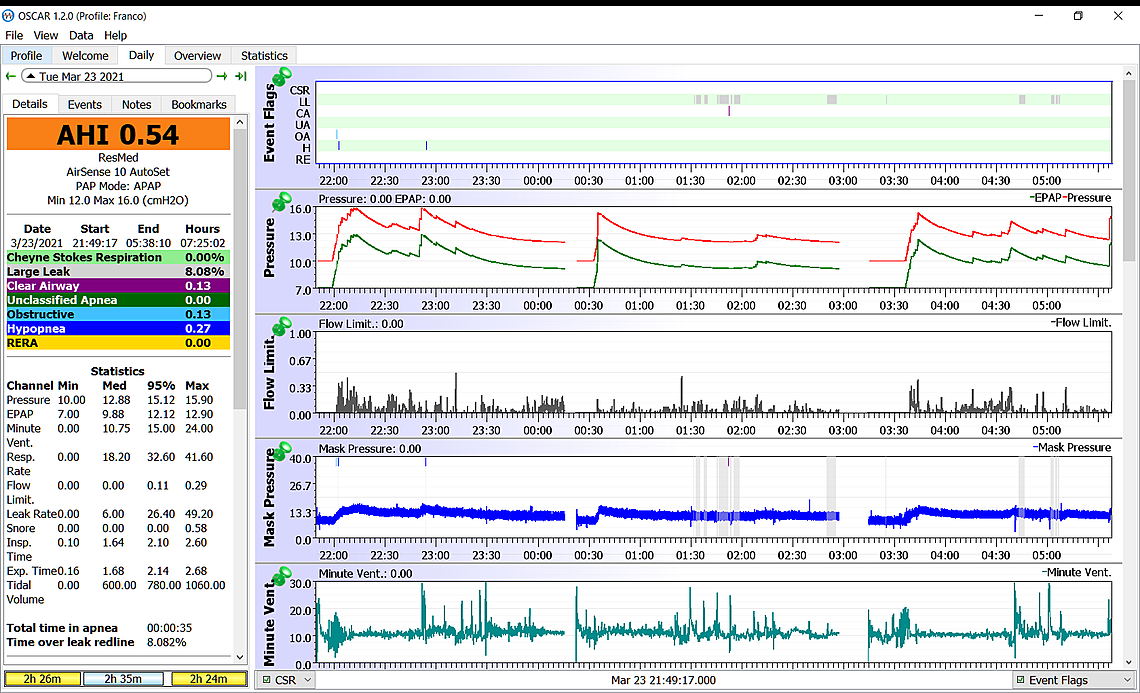
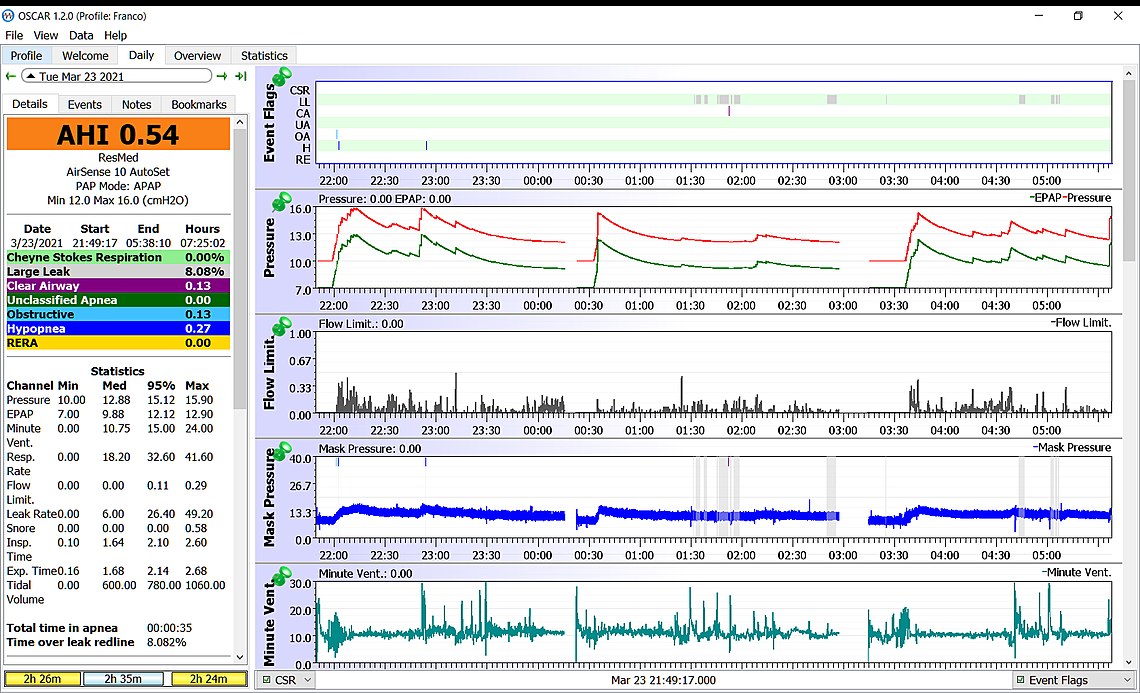
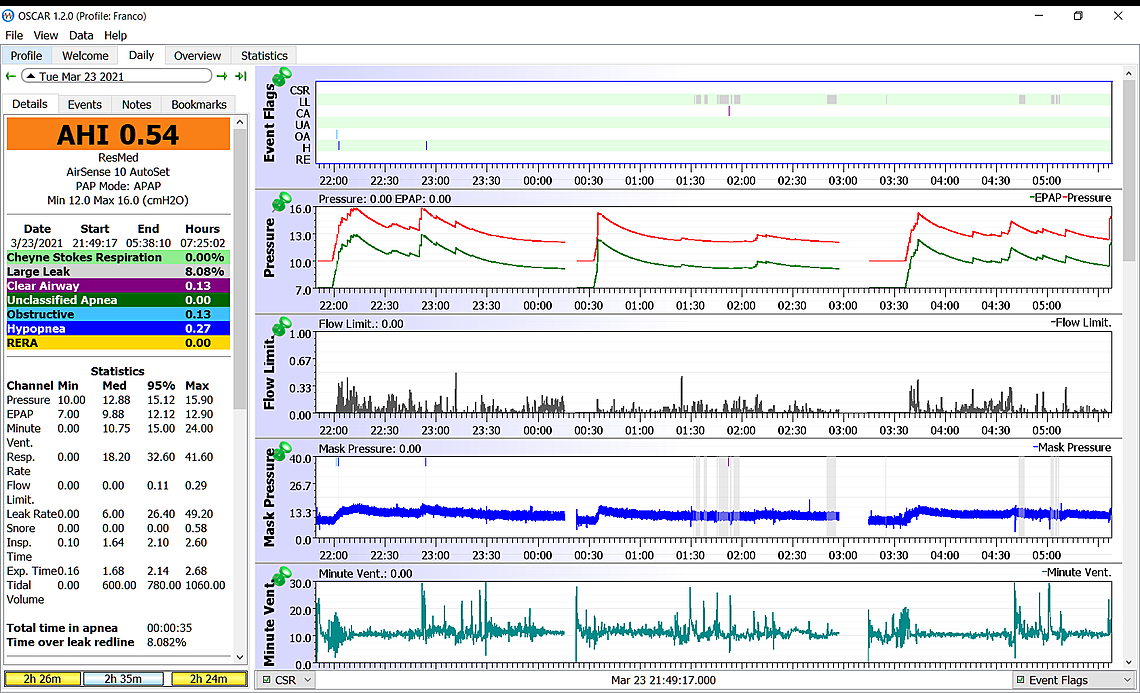
HI Thanks for your comments and explanations. I am sending a couple more daily reports after the pressure change to 12-16. Those I have previously sent are perhaps not as representative, because they are way off my average in terms of AHI. I sent them in case you see something standing out. It is the first time that my AHI’s keep under ONE for two consecutive days. May be it is a sign of improvement. Regarding the “pressure plots disabled”, I have now restored the setting to default as per your instructions. I have also upgraded to Oscar 1.2. I am unable to turn off the EPR, though. This option does not seem to be included in the Preferences, but I prefer not to play with this setting. I’ll just wait to see if there is any improvement after increasing the pressure. I have also checked the CSR issue. The Stats show an incidence of 0% over the last 30 days and 0.11% over the last 6 months. I don’t think I should worry. From what I begin to understand, there may be some interesting clues in the Flow rate, the Flow limit and the Minute Ventilation graphics, but all this is kind of nebulous for me at this stage, because the analysis of these parameters involves a good understanding of technical and physiological issues. It is really a fascinating issue, even more so that it is about my health and I hold dearly to it.
Here are the reports
Thanks
Franco
Hi Sierra HI Thanks for your comments and explanations. I am sending a couple more daily reports after the pressure change to 12-16. Those I have previously sent are perhaps not as representative, because they are way off my average in terms of AHI. I sent them in case you see something standing out. It is the first time that my AHI’s keep under ONE for two consecutive days. May be it is a sign of improvement. Regarding the “pressure plots disabled”, I have now restored the setting to default as per your instructions. I have also upgraded to Oscar 1.2. I am unable to turn off the EPR, though. This option does not seem to be included in the Preferences, but I prefer not to play with this setting. I’ll just wait to see if there is any improvement after increasing the pressure. I have also checked the CSR issue. The Stats show an incidence of 0% over the last 30 days and 0.11% over the last 6 months. I don’t think I should worry. From what I begin to understand, there may be some interesting clues in the Flow rate, the Flow limit and the Minute Ventilation graphics, but all this is kind of nebulous for me at this stage, because the analysis of these parameters involves a good understanding of technical and physiological issues. It is really a fascinating issue, even more so that it is about my health and I hold dearly to it.
Thanks
Here are the reports
Hello Sierra
HI Thanks for your comments and explanations. I am sending a couple more daily reports after the pressure change to 12-16. Those I have previously sent are perhaps not as representative, because they are way off my average in terms of AHI. I sent them in case you see something standing out.
It is the first time that my AHI’s keep under ONE for two consecutive days. May be it is a sign of improvement. Regarding the “pressure plots disabled”, I have now restored the setting to default as per your instructions. I have also upgraded to Oscar 1.2.
I am unable to turn off the EPR, though. This option does not seem to be included in the Preferences, but I prefer not to play with this setting. I’ll just wait to see if there is any improvement after increasing the pressure.
I have also checked the CSR issue. The Stats show an incidence of 0% over the last 30 days and 0.11% over the last 6 months. I don’t think I should worry. From what I begin to understand, there may be some interesting clues in the Flow rate, the Flow limit and the Minute Ventilation graphics, but all this is kind of nebulous for me at this stage, because the analysis of these parameters involves a good understanding of technical and physiological issues. It is really a fascinating issue, even more so that it is about my health and I hold dearly to it.
Here are the reports
Thanks again
Franco
HI Thanks for your comments and explanations. I am sending a couple more daily reports after the pressure change to 12-16. Those I have previously sent are perhaps not as representative, because they are way off my average in terms of AHI. I sent them in case you see something standing out. It is the first time that my AHI’s keep under ONE for two consecutive days. May be it is a sign of improvement. Regarding the “pressure plots disabled”, I have now restored the setting to default as per your instructions. I have also upgraded to Oscar 1.2. I am unable to turn off the EPR, though. This option does not seem to be included in the Preferences, but I prefer not to play with this setting. I’ll just wait to see if there is any improvement after increasing the pressure. I have also checked the CSR issue. The Stats show an incidence of 0% over the last 30 days and 0.11% over the last 6 months. I don’t think I should worry. From what I begin to understand, there may be some interesting clues in the Flow rate, the Flow limit and the Minute Ventilation graphics, but all this is kind of nebulous for me at this stage, because the analysis of these parameters involves a good understanding of technical and physiological issues. It is really a fascinating issue, even more so that it is about my health and I hold dearly to it.
Here are the reports
Thanks
Franco
HI Thanks for your comments and explanations. I am sending a couple more daily reports after the pressure change to 12-16. Those I have previously sent are perhaps not as representative, because they are way off my average in terms of AHI. I sent them in case you see something standing out. It is the first time that my AHI’s keep under ONE for two consecutive days. May be it is a sign of improvement. Regarding the “pressure plots disabled”, I have now restored the setting to default as per your instructions. I have also upgraded to Oscar 1.2. I am unable to turn off the EPR, though. This option does not seem to be included in the Preferences, but I prefer not to play with this setting. I’ll just wait to see if there is any improvement after increasing the pressure. I have also checked the CSR issue. The Stats show an incidence of 0% over the last 30 days and 0.11% over the last 6 months. I don’t think I should worry. From what I begin to understand, there may be some interesting clues in the Flow rate, the Flow limit and the Minute Ventilation graphics, but all this is kind of nebulous for me at this stage, because the analysis of these parameters involves a good understanding of technical and physiological issues. It is really a fascinating issue, even more so that it is about my health and I hold dearly to it.
Here are the reports
Thanks
Franco
HI Thanks for your comments and explanations. I am sending a couple more daily reports after the pressure change to 12-16. Those I have previously sent are perhaps not as representative, because they are way off my average in terms of AHI. I sent them in case you see something standing out. It is the first time that my AHI’s keep under ONE for two consecutive days. May be it is a sign of improvement. Regarding the “pressure plots disabled”, I have now restored the setting to default as per your instructions. I have also upgraded to Oscar 1.2. I am unable to turn off the EPR, though. This option does not seem to be included in the Preferences, but I prefer not to play with this setting. I’ll just wait to see if there is any improvement after increasing the pressure. I have also checked the CSR issue. The Stats show an incidence of 0% over the last 30 days and 0.11% over the last 6 months. I don’t think I should worry. From what I begin to understand, there may be some interesting clues in the Flow rate, the Flow limit and the Minute Ventilation graphics, but all this is kind of nebulous for me at this stage, because the analysis of these parameters involves a good understanding of technical and physiological issues. It is really a fascinating issue, even more so that it is about my health and I hold dearly to it.
Here are the reports. The 2nd one won't go through o. Thanksn the same post. I'll send it separately
Hi Sierra
I am sending a couple more daily reports after the pressure change to 12-16.
It is the first time that my AHI’s keep under ONE for three consecutive days. May be it is a sign of improvement.
I have now fixed the “plots disabled” issue as per your instructions.
I have also upgraded to Oscar 1.2.
Regarding the CSR issue, the Stats show an incidence of 0% over the last 30 days and 0.11% over the last 6 months. I don’t think I should worry.
From what I begin to understand, there may be some interesting clues in the Flow rate, the Flow limit and the Minute Ventilation graphics, but all this is kind of nebulous for me at this stage, because the analysis of these parameters involves a good understanding of technical and physiological issues.
It is really a fascinating issue, even more so that it is about my health and I hold dearly to it.
Here are the reports
I'll send a 2nd and last report on a separate post. I have been trying for two days, but
Thanks
Ittiandro
Sierra As per previous post, here here is the 2nd and last report after the pressure increase. Over three days of increased pressure , even though there still is a mix of OA and H's, the AHI's seem to have fallen consistently below 1
Thanks again
It looks like your posts got stuck in the spam filter here due to the repeated posts and the larger number of graphics. It is usually best to only post one graphic in a post and then wait until it gets displayed in the thread.
I see you have got your Mask Pressure back so that is good.
I also see that compared to your earlier graphs that the machine is now using the AutoRamp feature and starts your pressure out with 10 cm and holds it there until you go to sleep. It is good that it is set up that way.
The increased pressure seems to be limiting your obstructive events.
The only change I would suggest you make is to stop the EPR pressure reduction on exhale during sleep. This is not likely to improve your overall AHI as it is very good already in your most recent reports. But, what it should do is reduce the amount of pressure you need to get those good results. 16 cm of pressure is getting up there. The machine can only go up to 20 cm. A higher pressure can make it more difficult to get a comfortable sleep and more difficult to stop mask leaks. So in my opinion it is a worthy task to try to minimize the pressure needed to get good results. The very best way to do this is to set the EPR Type to Ramp Only. No other settings on the machine would need to be changed. It is very easy to do, and I could give you the steps needed to do it. Or, you could ask your provider to do it. If they are making changes to your machine remotely over the internet that would be easy too.
When this change is made what you should see is that during that initial part of the night were you can see the red inhale pressure is fixed at 10 cm and the exhale (green) is fixed at 7 cm they should stay the same. While you are awake it is reducing the exhale pressure for comfort. But, when this "ramp" period ends when you go to sleep the machine stops reducing the exhale pressure. You would then see the red and green trace go to the same pressure. Also you would see the blue Mask Pressure stop cycling so much with every breath. But, and it is an important "but" the pressure it goes to may be significantly lower. This is because of the increased exhale pressure. Overall it may reduce the maximum pressure the machine uses from 16 to 13-14 cm. This feature is described on page 10 and 16 in this Clinical Manual. It is a very good feature and is one of the big advantages of a ResMed machine compared to a DreamStation.
Other than using the EPR during sleep, I think your machine is well set up. If you go with the EPR on Ramp Only you may be able to reduce your maximum pressure setting back down to 14 cm or so. However, hold off on that until you see what EPR on Ramp Only does.
Hi Sierra Regarding the EPR change I am not too keen on changing the original settings prescribed by the doctor. However, if you tell me how to do it, I’ll try it just to see how it works. I can always reset it later.
Except for the very few 0 (zero) AHI’s I have got so far,( probably three or four in a year), my AHI’s are getting consistently lower and lower after the pressure change. Today, the 3rd day, the AHI's were 0.29, all of which being Hypoapneas . No OA’s or other
I also noticed a drastic change in the Minute Ventilation graphic: the waveform is considerably smoother when there are few or no OA’s. Conversely, the more the OA’s, the more does the Minute Ventilation wave pattern look like…. a seismograph during an earthquake and vice versa.
This can easily be seen by comparing my recent graphs with the older, high AHI’s ones, especially the one of Dec 16 which I had sent you. I seem to detect changes also on the Flow Limit graph , but I cannot put my hands on them. All in all, I am very satisfied with my therapy, if it continues like this.
If you have any comments, I always like to hear them..
Thanks
Ittiandro
Here are the steps to change the EPR to Ramp Only:
That is it. It sounds more complicated than it really is. That is the only change you need to make. The pressure does not have to be changed as the machine should automatically use less pressure. You should try it for a few nights to see what difference it makes to pressure. With Oscar you should see the pressure graph change so the red and green lines track over each other after the initial "ramp" at 10 cm ends. You should also see on the left section for Machine Settings show the EPR as Ramp Only.
Minute ventilation is disturbed by apnea events. It can also be disturbed by central apnea breathing issues like CSR. Sometimes you will see minute ventilation cycling before a central event occurs. It is a good overall measure that breathing is stable.
Any questions, just ask.
Are the Canadians back playing again? I was looking forward to the three games this week with Edmonton (where I am from), but they all got cancelled due to COVID...
Hi Sierra when I select the Ramp type option there is no option to select "Ramp only". I can only choose between different Ramp time settings( in minutes), or AUTO or OFF.
Thanks
Franco
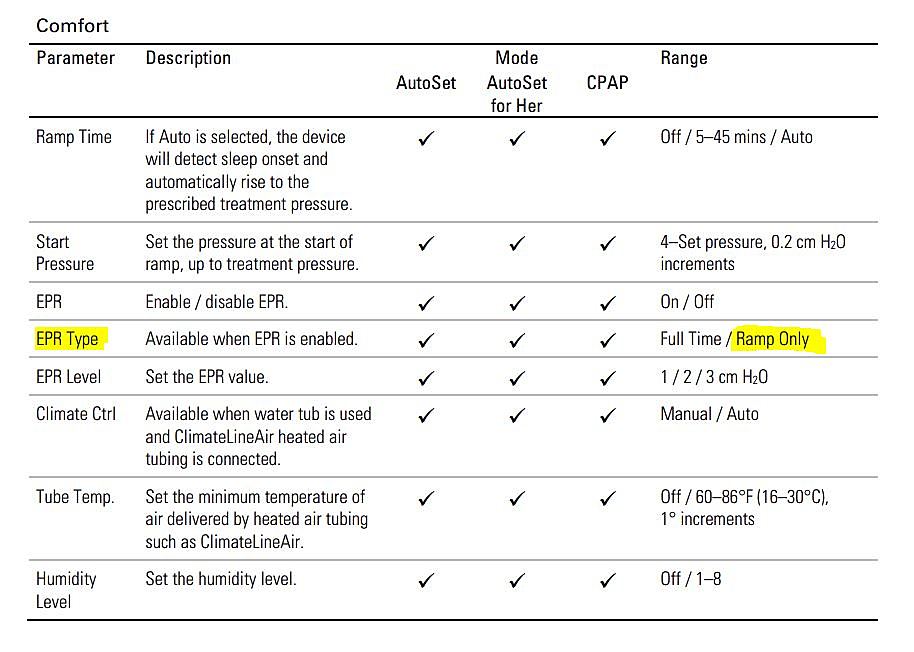
See page 16 of this manual. It shows the options under the Comfort section:
From what you are describing, I think you have selected the Ramp Time option instead of the EPR Type. From what I see of your Oscar reports you have Ramp Time set on Auto -- which is good. Go further down to EPR Type. There should only be two options Full Time (which is where your machine is) and Ramp Only. Choose Ramp Only.
From the Manual:
OK, thanks, I got it. I'll see how it works after tonight. Just a question, though. Given the fact that with the increased pressure my AHI's are so dramatically low, with practically no OA's and very few, short Hypoapneas, what perceived benefits should I expect from using the Ramp-only feature? Better, more refreshed?
Also, an unrelated, but important question: when I travel can I go without the machine for a couple of weeks or so? It is too cumbersome in the luggage. I believe there shouldn't be a problem, because I probably lived my whole life with SA and I never knew it..Perhaps you can comment on this. .
In fact, now that I think about it, when I was in my early twenties and I was traveling with friends In Italy, where I still lived at the time, one morning I found a doctor at bedside in my hotel room, when waking up ( better seeing a doctor, though, than... St Peter with the Hell's key in his hand...)
I never knew what really happened that night, but my friends told me that something was happening when asleep ( gasping for air?) and this is why they called the doctor.. Actually, I was feeling fine ( until I got the doctor's bill..). Now I think I understand..
Franco
If you want to read a bit more about the issue of using the EPR feature see the link below to an older thread. "sleeptech" was a regular participant here a few years ago. He works as a sleep technician setting up CPAP machines in Australia. I can't say I agree 100% with what he says is an issue, but for sure he is right on the fact it can raise the needed pressure to treat the apnea in most users. The feature is sold as a comfort option, but it has a price of needing more pressure. Not everyone responds the same, but you will find out fairly quickly how well it works for you.
https://myapnea.org/forum/not-understand-epr-setting/1#comment-5056
This may be more detail than you really want, but it may help you understand why EPR which is a pressure reduction on the exhale part of the breathing cycle, can cause apnea events. See this zoomed in Daily Report example of a OA event. This was very shortly after I started CPAP treatment (three years ago) and was not getting very good results. At the time my machine was set up with a Minimum Pressure of 10.4, and Maximum of 15 cm. EPR was set to Full Time and at 3 cm.
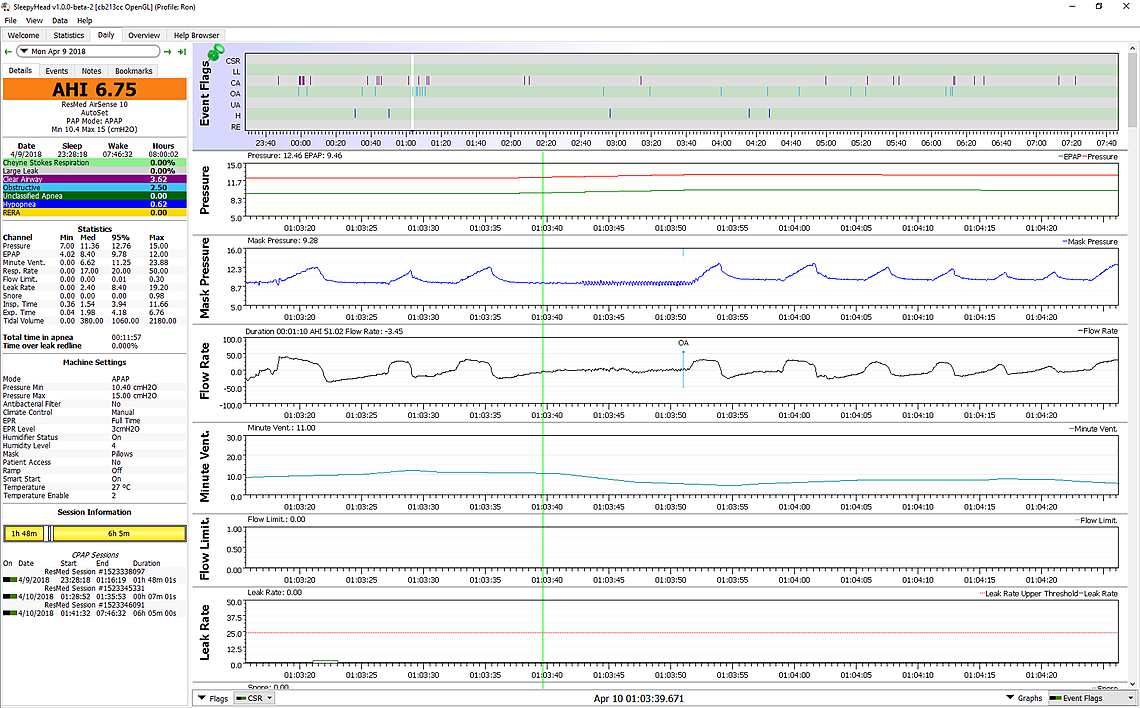
If you look carefully at this OA event it basically starts where the green vertical cursor line is just before 1:03:40 for time. The Flow rate should have gone above zero in into an inhale cycle at that point, but it does not. The pressure due to the EPR is at 9.5 cm, instead of the higher 12.5 that one would expect it to be at. That is the main learning point. The event which is a collapse of the airway started at the lower exhale pressure. The higher inhale pressure did not prevent it because that machine had not increased it at that point. In fact it did not increase the pressure until just after the machine flagged it as an OA event.
I hope this shows why the EPR feature can have negative impacts on how the CPAP controls apnea events. I now use a much lower fixed 11 cm of pressure and no EPR after the ramp ends and have much fewer events than when I was using EPR. If you have any questions, just ask.
I will start a new full width post because when you keep replying to post after post they get kind of narrow on the page! You said:
"Given the fact that with the increased pressure my AHI's are so dramatically low, with practically no OA's and very few, short Hypoapneas, what perceived benefits should I expect from using the Ramp-only feature? Better, more refreshed?"
I can't predict how refreshed you will feel, but what you quite likely will see is that the actual pressure used in auto over the night will go down. This should feel more comfortable, and make the mask less likely to leak. That also could make you feel more comfortable. I wouldn't expect your AHI or apnea events to get better or worse.
On the travel issue, before COVID, we travelled a lot. Airlines let you take a CPAP as an extra carry on piece of luggage with no charge. They will want you to take the CPAP out of the case, but other than that you should sail through security. Getting water for the humidifier can be an issue. For periods of up to two weeks we just use tap water. You probably have to use some extra vinegar to clean out the reservoir after you get back, but overall no harm done. If you look around the airport in the boarding lounge you may be surprised how many people have a CPAP. The advantage of the AirSense 10 is that it packs up quite small. It can accept 230 volts or 110, but you may need an adaptor to fit the wall socket depending on the country. We would not consider travelling without them. My wife and I both use a CPAP.
I am sending last night’s report, after the EPR setting change. The AHI’s have slightly increased, with Hypoapnea and RERA component, no OA’s. . Actually this time my sleep was a bit disturbed by frequent leaks throughout the night, with a persistent ( and bothering) hissing sound. Usually, I can fix this by readjusting the straps and the mask position which sometimes goes off center when I change side. Not this time. May be the silicon seal needs to be replaced. I don’t know if the EPR new setting has something to do with this. I’ll see how it goes tonight. Regarding traveling , I was wondering if it is safe to go without it. I wouldn't see why not, because I have traveled all my life without trhe CPAP, but may be with age my physiology has changed and it will affect me . Thanks
Franco
It may be worth trying it another night just to confirm, but from what I see you may be one of the few that do not benefit from having EPR off during sleep. It looks like the pressure is being driven up by the Flow Limitation rather than the obstructive events. The EPR may be helping to reduce the Flow Limitations and actually results in a lower pressure. If pressures do not come down on the second night, it would be best to go back to EPR Type of Full Time. That is the way it goes with CPAP treatment. It is always a bit of trial and error.
Hi Sierra With the EPR still off, last night was very smooth. The only thing I noticed was an unusual very low pulse at wake up. Usually it is 60 bpm because I take a betablocker following an isolated episode of atrial fibrillation almost three years ago, but this time It felt even lower. It was also skipping a beat, although very regularly. I don’t know if it is related to the EPR setting and the oxygenation pattern. I don’t worry, anyway. For one thing, I am not new to arrythmias. I had a very unusual one recently, with the pulse shooting up and down between 90-130 bpm, accasionally 150 bpm, for about a week, with absolutely no symptoms. I rushed to the emergency, but the ECG indicated a perfectly normal heart. The doctor said I shouldn’t worry about occasional arrythmias or tachycardias as long as I have no symptoms, like chest pains, fatigue or breathing difficulties. She said the cardio watch is not a medical instrument. It doesn’t show the complete wave pattern It only picks up the irregular beats and it averages them out in a way that can be misleading. You can have a look at the report
Thanks, as usual.
Well, even though the AHI is better the pressure is certainly not lower. I don't think you are gaining anything with the EPR set to Ramp Only. I think I would switch it back to Full Time. The 95% Flow Limitation number seems to have about doubled from when you had the EPR full time. It has gone up from about 0.12 to 0.28. Your OA events have gone to zero, but I think Flow Limitations are driving the pressure up.
If you ever have issues not being able to control the Flow Limitation issue, you may be a candidate for a BiLevel machine instead of the standard APAP. EPR on an APAP is limited to 3 cm differential between inhale and exhale pressure. A BiLevel can go much higher, and the maximum pressure can go up to 25 cm instead of the 20 cm limit on an APAP. But, for now I think you are doing fine with an APAP.
Yes, I might as well switch back to Full time as there isn't much of a perceived difference in having the EPR set at Ramp only. What I understand less, though is the Flow limitation issue and what it means to have the Flow limitation number doubled, along with the doubled pressure and the implications
Thanks
Franco
I agree. EPR seems to be helping you. First time I have seen it demonstrated to be a benefit. I learned something.
First to be clear, I am not a doctor, just a mechanical engineer. I know more about machines than bodies. ResMed does not say much about flow limitations but the machine certainly does respond to it in Auto mode by increasing pressure. I think it may be the first warning of an impending hypopnea event or even obstructive apnea event. My wife also uses a CPAP and her 95% Flow Limitation also seems to be up in the 0.28 range, like yours are with no EPR. My typical 95% Flow Limitation is 0.09. She also suffers from Snore more than I do. I was diagnosed at about 37 for API. She was diagnosed at more like 83. So perhaps it is an overall indication of sensitivity to apnea. I have found that I can reduce the flow limitation and snore for her with more pressure. However she dislikes the additional pressure and I cut it back. Her machine is set with a minimum of 13.6 cm and 14.4 cm Max, and no full time EPR.
But we are all kind of different. My wife almost always is under 1 for AHI. I am happy to be under 2. She gets no CA events, and for me after H events CA are the most common.
All considered, with your EPR on Full Time I think your machine is set up well. Allowing pressure to go above 16 cm may reduce your Flow Limitation numbers, but like my wife, possibly not your comfort level. Some clinics set the maximum pressure at the 20 cm default and let the machine do what it wants. It is an option, but you will deal with the potentially increased frequency of mask leaks. On the other hand I cannot let the machine keep increasing pressure as it causes lots of CA events. That is the main reason I switched my AirSense 10 from Auto to fixed pressure CPAP mode.
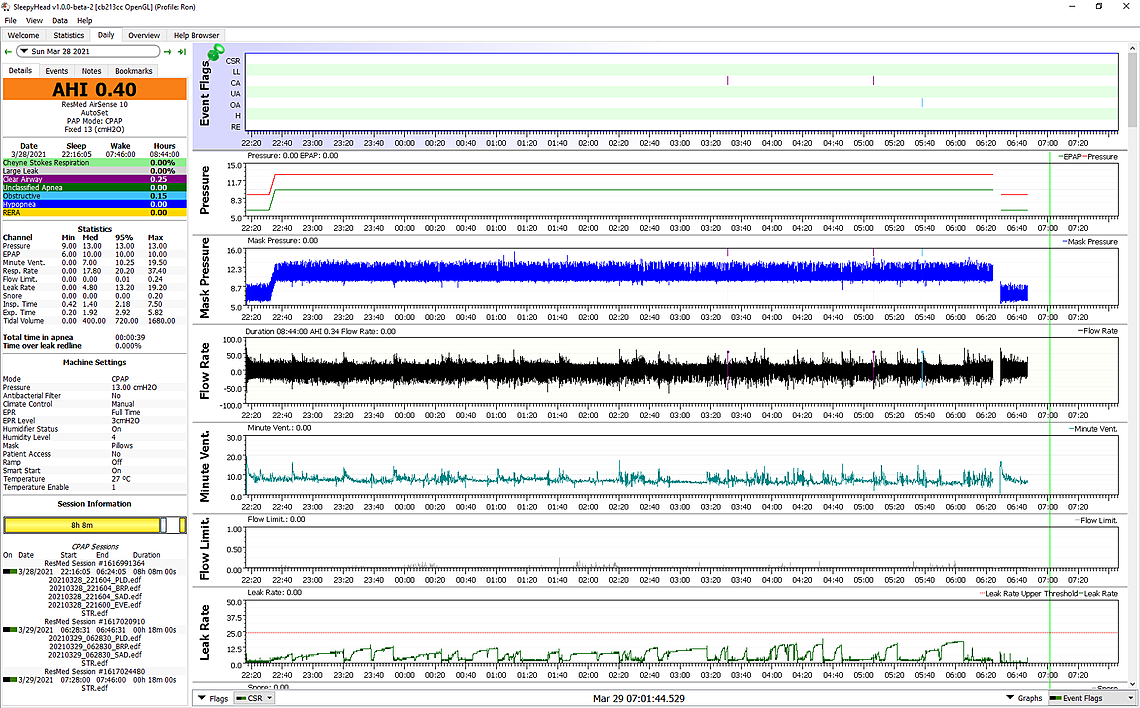
Franco, your good results using EPR motivated me to try it again for myself. I went through a very long trial and error process to end up with what I have been using for a couple of years now -- 11 cm fixed pressure in manual CPAP mode with EPR on Ramp Only. For last night I changed that to 13 cm (to compensate some for the EPR reduction) and turned EPR back to full time. I had intended to try this a long time ago but had never gotten around to it after I settled on the fixed pressure mode. Your results prompted me to try it.
In any case I got about the best results I have ever had with this change -- API of 0.4. 95% Flow Limitation was 0.01. Almost zero. This is one night only and may have been a fluke, but I will leave it there to see. My biggest issue has been hypopnea events and not so much OA events. For the night I got zero hypopnea events and one each of the CA and OA. Kind of amazing. Will have to see if it is repeatable. I did not notice the extra pressure during sleep and my leak rate was quite acceptable, although not zero.