I'm have been diagnosed with REM-related sleep apnea (RDI:14.3) in March and was prescribed with a CPAP (DreamStation CPAP Auto with A-Flex).
I have not done a CPAP titration to determine the pressure setting of my CPAP but instead determined the setting by a series of trial and error and my subjective experience.
Although my sleep quality improved markedly with the CPAP (I feel nausea the next day if I don't use the CPAP) and I yawn a lot less often throughout the day, I'm not sure if my REM-related sleep apnea is completely treated as I feel tired and unenergetic compared to my peers (which I sometimes get made fun of for yawning and looking unenthusiastic). I also still wake up to urine at night (which I was told is a symptom of sleep apnea). However, there had been two days since I started treatment when I feel completely refreshed and energised despite having only used the CPAP for 5 hours both times, and for one of those days, my AHI according to my CPAP was 0.
My CPAP's AHI ranges from 0.8-2 every night I use. My ENT consultant told me that so long the CPAP's AHI is below 5, then my sleep apnea is treated to that of a normal person. However, I'm not sure if the data from CPAP alone is sufficient to say my REM-related sleep apnea is treated. Since REM sleep occupies the shortest duration of one's sleep cycle, with the majority being non-REM sleep. Therefore, could it be possible that the period when I don't get sleep apnea during non-rem sleep will skew the CPAP's overall AHI to a number below 5 despite I continue to have notable episodes of apnea/hypopnea during REM sleep. I believe this concept is reinforced by my sleep study's data which showed I have an RDI of 1.8 (REM RDI: 14.3 and non-REM RDI of 1.1). But please correct me if I'm wrong.
If what I speculate is true, should I look for a private hospital to conduct a CPAP titration in my area to determine an objective and ideal pressure settings? Or should I seek another service? I have already talked to my GP briefly about the situation but he is not very familiar with OSA and he said it is unlikely a referral to a publicly funded sleep clinic will be successful as my Epworth Sleepiness Scale is in the normal range (despite having mentioned I can't sleep in public setting due to anxiety following two concussions).
The reason I think my pressure setting could be a problem was because I've experienced nights when I feel like the pressure isn't high enough which woke me up and made me gasp for air with a shrivel across my body or made me remove the mask to sleep. Alternatively, if I change the pressure to a higher setting, then my central apnea episode increases and I get very painful stomach bloating that wakes me up early.
Thank you very much for taking the time to read. Really appreciate any advice/inputs.
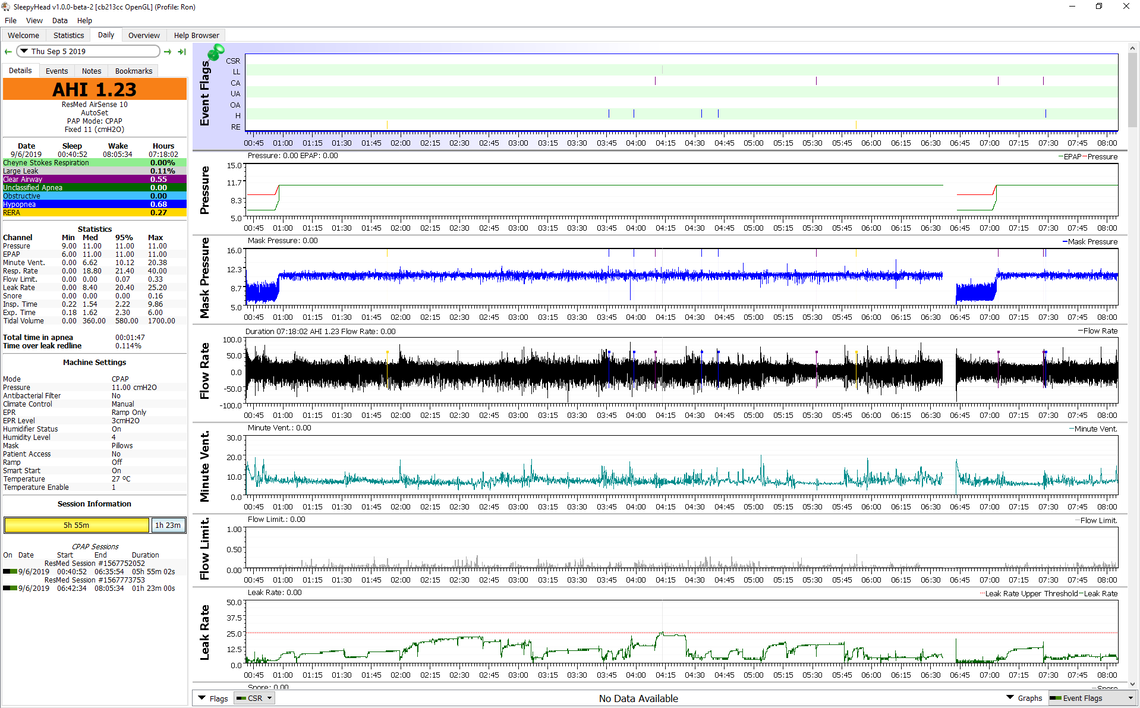
My suggestion would be to download SleepyHead and look at your detailed data which should all be captured on the SD card in your machine. Further development of SleepyHead has been shut down, but the current download should work fine with your machine. You need a PC or a Mac and a SD card reader to use SleepyHead.
SleepyHead will let you see every event during the night, when it happened, and at what pressure it happened at. This is very useful in determining if your pressure settings are optimized for you. If you want to post a screen shot here of a typical daily report I and others can comment. With an Auto CPAP you are essentially doing a titration test every night. The machine has no way of telling whether your are in REM sleep or not, but I suspect that is not the issue.
Here is an example of what a Daily Report looks like in SleepyHead. There are many other variable tracked, but I find these to be the more important/useful ones.
"I have not done a CPAP titration to determine the pressure setting of my CPAP but instead determined the setting by a series of trial and error and my subjective experience."
An Auto CPAP helps you to find your pressure and titration really isn't needed with an auto unit. If they tell you otherwise, they're just trying to make money. For instance, when I first got my ResMed Air Sense 10 Autoset, I think I set the initial pressure to like 5.3 starting pressure, 6 minimum and 12 maximum. Over a period of 1-2 weeks, I noticed that my max pressure never went above 8.9 and varied usually between 7 and 9. So that told me that my maximum pressure setting should be 9. I have also awaken for a bathroom trip sometime and saw that my pressure was exactly 8.9 on a consistent basis.
Over the past couple of months, I have since progressed with the settings. That told me that my maximum pressure setting should be 9 at the most. I examined my Sleepyhead events and confirmed it over the days and weeks. So 9 was my maximum pressure. Then I had to figure out what my starting pressure and minimum pressure (the pressure that it kicks up to once you actually drift off to sleep) should be. 5.3 at first seemed okay as a starting pressure, but after a day or two, it felt suffocating. I kept upping the pressure. Now I have it at 6 starting pressure and 6.4 minimum pressure with the option to go up to the max of 9 for the worst events. EPR setting is at 3. My starting pressure begins after 5 minutes.
The result? I typically have 5.3AHI and 18.1RDI without the machine. With the machine and the above settings, I'm up to 6 hours 10 minutes per night on average with 0.96AHI. When I first started out, I was yanking the mask off every 1-2 hours. The other readings are typically in the 0.X range and not even at a 1. I have massive sleep debt and I do feel better some days (more energy)...but I'm 37 and have had trouble sleeping since I was probably 12 or 13. So I have a lot to catch up to.
I either have REM-related sleep apnea or UARS based on my 18 RDI.
I have also found various research online that suggests that when you start getting used to the machine and catch up a little bit on getting used to the mask and air pressure itself, sometimes your actual apneas/hypopneas will decrease because you're more rested. When you're exhausted back to back, the apneas are known to get worse.