I think I have the AHI concept correct:
The AHI (Apnea Hypopnea Index)score is measured and produced by most CPAP machines. AHI comes from the machine sensing apneas and hypopneas occurring per hour during a sleep session. A score of 5 and under is considered okay. The machine senses that breathing has stopped and if the stoppage lasts for enough seconds (I think 10) it is recorded as either CA (central apnea), OA (obstructive apnea), UA (unidentified apnea, or H (hypopnea). If my score is 5 or under a green smiley face will appear under Sleep Report on my ResMed AirSense. Over 5 and a red frown face appears.
To see the AHI numerical score I must remove the SD card from the CPAP machine, insert it into my laptop, launch the program OSCAR, and import data from the SD card. Daily reports will then be available for AHI scores and a large amount of other data concerning sleep sessions like machine settings, date, hours of sleep, air leaks, and number of apnea events.
Some feel AHI scores can be off due to the machine's falsely identifying apneas. My high AHI scores occur when a cluster of apneas are recorded during a 30-minute to hour period of large mask leaking. This happens when I roll from side to back during sleep. This action knocks the mask off its seal, therapy is not being delivered. How apneas can be registered when the mask has no seal, is something I do not understand. I eventually wake, adjust the mask, and therapy resumes. I feel that the large leak periods of lost mask seal skew the AHI. I would rather see an AHI of only the time I'm getting therapy, excluding the time spent with the mask seal lost.
Some may think my cluster of apneas that produce a >5 AHI score likely comes from my chin going towards my chest which causes restricted air flow, resulting in OAs. I think it is the mask losing its seal that causes these clusters to appear which can be 75 OAs registered in less than an hour. That's over 1 apnea per minute! Not breathing 10+ seconds out of every minute does not sound like an accurate sensing, but maybe it is possible.
Are there any opinions of the AHI being skewed by large leaks?
Leaks over the leak rate redline of 24 L/min show as grayed out areas in OSCAR. During leaks this high the machine cannot reliably distinguish between central apnea events and obstructive apnea events. For this reason ResMed (if that is what you have) suspends the classification of events, but I believe still reports them as Unclassified apnea events, UAs. Because it does not know if the event is obstructive which indicates the need for more pressure, or central where more pressure is inappropriate, the machine takes no action on pressure, and just holds it where it is. So, in some cases if the pressure is not high enough, more events can occur, and when the large leak ends pressure may be too low and a series of events can occur. What affect does this have on AHI? I am not that sure. My wife suffers from significant leaks and I am not sure it hurts her AHI.
The other thing to check when when a large leak occurs is how well the machine holds pressure. If you have a ResMed which displays Mask Pressure in OSCAR, that is a good indication of whether or not you are losing pressure. If you have a DreamStation machine I don't believe it reports Mask Pressure, so that check is not possible.
If you post an OSCAR daily report with your high event issues I can comment. But, the first thing that comes to mind when there is a quick succession of OA events is a positional problem, like a kinked neck. If this is a problem some gain amazing relief by wearing a soft cervical collar. This was the case with another poster here that I worked with. He started using a soft cervical collar and brought his AHI down to very good levels. See this thread. It is a long one, but the poster stuck with it and got good results.
I think I have been fretting over high AHI scores needlessly for years due to my often Large Leak cluster of events. It has always been a wonder as to why many times I may feel better with a 7.30 AHI than a 2.75 AHI and a frustration that for 18 years I could never get an AHI below 1.75 yet I see other's OSCAR reports showing frequent < 1.00 and even 0.00 scores. I am concluding that if you Large Leak for more than a few seconds your AHI is not accurate. Take out the OAs, CAs, and UAs of a Large Leak cluster then calculate the AHI for a more accurate score especially if the events are within a tight cluster of an event every minute (AHI 60.00) which seems like more suffocation, not apneas. Why average in a short time period of AHI 60.00 with hours of AHI < 2.00? Does this not skew the AHI?
The possibility that my AirSense 10 is false flagging of events during a Large Leak gray area is part of my issue with a possibly skewed AHI. I can have 20 events within a 20-minute cluster within a gray area. The large amount of compacted events raises the AHI giving a false indication of the quality of therapy over a total sleep session. In other words, pull out the Large Leak time and its cluster of events from X hours of sleep and the AHI score will drop dramatically. Why be concerned over a 7.00+ AHI when it was a 20-30 minute cluster of events within a Large Leak gray area that caused the score? The AHI would be < 1.00 with the cluster excluded. Even if the events are accurate, they skew AHI's meaning toward the overall sleep session with over 90% of the sleep time in an AHI of <.50.
If a cluster of events is seen on a report even though over a gray Large Leak area the interpretation includes, "positional," and "chin tucking." The advice will be to use a low pillow and a soft cervical collar and may give suggestions on how not to roll to the back during sleep. Some CPAP users strap their chins, tape their mouths, collar their necks, and put nostril-opening spring strips to their noses when another mask could be all that is needed to get AHI down by reducing Large Leaks.
I don't expect perfection from anyone or a machine, but I would like those concerned with CPAP therapy to take a closer look at apnea clusters within Large Leak gray areas and give more consideration to the possibility that these event clusters may not be caused only by sleeping positions that restrict airflow. They could be false flagged events due to a Large Leak. How can the machine flag events and measure airflow limitation if the air pressure is lost in the mask by air freely flowing out its perimeter? Does the rate of 75 events an hour make sense inside a Large Leak gray area? Could not the cluster of events be eliminated by fixing the leak problem as opposed to wearing a soft collar, mouth tape, or a chin strap? I do understand that it is jaw-dropping that may cause the Large Leak, but is it worth disturbing sleep with a collar if one or two event clusters in a gray Large Leak area are showing nonexistent events? Would not a mask that functions with a jaw drop be better advice than a collar or at least give it as an alternative try before a collar?
I am not of the opinion that large leaks have a significant effect on AHI. Unless the leak is really large, like the mask fallen right off or away from the face, the machine can still maintain pressure with a high leakage rate. My wife has large leak issues but I have never seen them that bad that mask pressure is not maintained. If you have a ResMed machine it will display mask pressure and you can check to see if it drops off by using OSCAR.
What does change on a ResMed when you have a large leak is the identification of the type of apnea event. During a large leak (greater than 24 L/min) the machine cannot distinguish between OA and CA events, so it calls them UA events, or unidentified apnea. Because it cannot distinguish the type it simply holds the pressure, because increasing pressure in response to a CA event would be inappropriate. So the worst thing that can happen is that you need more pressure and don't get it because of the leak issue. Then what may happen when the leak stops you get a few OA events right after the large leak ends.
I also think positional issues and large leaks are quite unrelated issues. You cannot eliminate apnea events related to position by stopping large leaks.
Some claim fixing large leaks will clear up AHI events. When large leaks occur everything goes up on my OSCAR report including mask pressure. Mask pressure does not drop off, it goes up but I don't think therapy is being delivered. I feel the whole system is compromised during large leakage including its ability to report events accurately. My leaks are out the sides of a full face mask. They wake me sometimes due to air rushing out of the periphery of the mask. This would be better described as a blow out.
Thank you for posting that OSCAR report.
I think it may be one from a nasal mask and I see single-pressure mode. I use APAP mode 9 to 19 cm. It is strange for me to see a straight pressure line, very little flow limitations, and even mask pressure. My reports are a varying mess of pressure changes, flow limitation spikes, and a range from 0.50 to 7.00 AHI. It has been suggested I record a video of my sleeping to see what goes on in my restless nights. My theory is that when I roll from side to back and then to the other side the mask loses its seal then regains it as I move again. When this happens all graphs spike and numerous apnea events are registered during the leak time.
Pain causes me to move a lot in my sleep. Once in a while, I realize I have slept in one position (left side) for about six hours. On these rare occasions, my OSCAR graphs are smooth with a low AHI, and I feel much better than usual. I have been doing better with the Evora FF to control leaks. Maybe my next mask, the F40 will be even better keeping a seal on my bearded, moving face. It has been a long 17 years of severe apnea with not very effective APAP therapy.
If you want to post an OSCAR report from a typical or bad night I can comment. My wife's setup has been adjusted many time over the 8 years she has been using it.
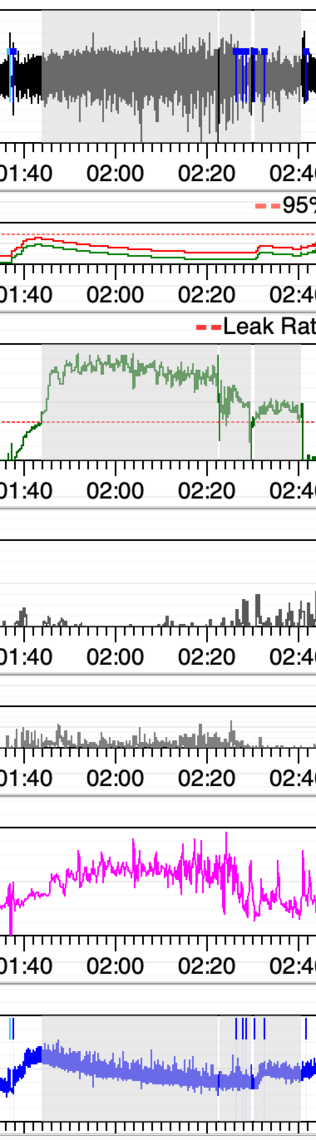
This is an example of what I call a blow out. An OA triggers a pressure increase which may cause me to move. I move, and the mask loses its seal. Mask pressure goes up and first then down as the seal is lost. All graphs on OSCAR shoot up. I theorize therapy has been lost during this LL session, and the flagged Hyponeas are false so AHI is skewed.
It would be much better to look at a full screenshot with all the settings on the left etc. However from what I can see of this, the leak has had no effect on your mask pressure and should have no effect on your AHI.
I will post the whole screen. It is not the leak that affects AHI, my theory is that during the long leak period, the Hypopneas flagged within the leak event are not correct and it is those events that raise the AHI. If the mask is in such a high state of leaking, how can it be registering genuine hypopneas?
Thanks for taking a look.
I think it is the flow limitations that are driving your pressure up. You appear to have your EPR set at 2 cm. You may gain some reduction in hypopnia and flow limitations by increasing that to 3 cm. I get a very significant reduction in my hypopnea with 3 cm of EPR.
The detail is missing, but I kind of think those hypopnea events are sneaking in when the leakage drops below the leak rate redline for brief periods of time. When the leakage is higher they are probably being suppressed.
A BiPAP machine like the ResMed AirCurve 10 VAuto may be of benefit to you. EPR is limited to 3 cm on the AirSense 10, but the similar pressure support on the BiPAP can be set as high as 10 cm. And max pressure will go up to 25 on a BiPAP. You are pretty much at the limit of 20 that the APAP can do. But, normally they will not prescribe a BiPAP until you can't stay under the 5.0 for AHI. At least on this night you are doing it.
I see what you mean. The pressure and flow limitations follow a similar path. Thanks. I have the machine on EPR 3 now. I will increase my Min. pressure to try to get flow limitation down. Is that not a tactic to reduce FL? I rarely go over 5.0 AHI so I may be out of luck on getting BPAP covered by insurance. There is a possibility that my FLs are not treatable by any PAP machine. My airways are chronically clogged. I have FLs awake or asleep. I will mention an AirCurve next doc visit. Sierra wrote: "I kind of think those hypopnea events are sneaking in when the leakage drops below the leak rate redline for brief periods of time."
A brief leakage drop below the leak rate redline lasted 14 seconds. 2 minutes and 30 seconds later, a hypopnea was flagged. In 1 minute 20 seconds, another hypopnea was flagged. In 30 seconds another hypopnea is flagged. The breath shapes near the H flaggings look the same as many breath shapes with no flags.
By "sneaking in," do you think these hypopneas could be false flags? My point about this issue is that I think AHIs may be inaccurate due to false flagging of events that I especially notice within gray areas. I have seen it demonstrated on video how machines or OSCAR can miss flagging events. I am saying events get flagged that did not exist, and I think the hypopneas I describe above are examples. I theorize that when the leak rate goes high enough the system malfunctions because it takes a good steady mask seal to produce a more accurate AHI. I am not concerned about my machine or OSCAR missing a few OA/CA/Hs. I think I may need to make the decision to stop fretting over AHIs of 2.00 - 5.00 and realize my air flow limitations...literally.
I wonder if the data that comes from CPAP machines have a published margin of error (+/-) for AHI. I also wonder if OSCAR has an accuracy margin of error.
Thank you for your attention, consideration, and lending of expertise. My doctor only checks compliance with usage requirements and refills the CPAP prescription annually. Not once in 17 years of CPAP therapy has my doctor, DME, or any medical staff looked at any report, asked how therapy is going, or offered advice. ejb
By "sneaking in" I mean that when the leakage rate is below the 24 L/min redline the machine can report events. For apnea events for sure, it stops trying to classify apnea events when the leakage rate exceeds 24 L/min. I am assuming the same may apply to hypopnea events. In other words they are not likely false, and are there during high leakage but are not being reported. Then when leakage drops below 24 then it starts reporting them again. One issue with high leakage is that when the rate goes over 24 the machine stops responding with more pressure to events. When the leakage returns to normal the pressure can be lower than it needs to be and events then occur as soon as leaks go below 24. There can be a burst of events right after a high leakage rate period.
Yes, EPR at 3 as well as a higher minimum pressure should help reduce flow limitations. I agree that your minimum pressure could be quite a bit higher. The 95% pressure is at 15.5, and if you were to switch over to fixed pressure CPAP mode that would be the first pressure to try. In auto you could try 12 or 13 for a minimum to see if that helps with flow limitations. If it does then it may not be so quick to increase pressure further.
Hope that helps some,
Sierra wrote: "For apnea events for sure, it stops trying to classify apnea events when the leakage rate exceeds 24 L/min. I am assuming the same may apply to hypopnea events. In other words they are not likely false, and are there during high leakage but are not being reported. "
OSCAR can show events with a code of H, CA, AU, or OA during gray, over the red line periods that exceed 24/L min. Would those not be false events (with classification) due to the machine not functioning properly during the over 24 L/min. perioid? I will research more to see if waveforms and/or lack of them match the event classifications shown in over red line sessions.
If the machine has lost its ability to function due to an over the red line 24 L/min. limit, how can the Hs, OAs, AUs, and CAs, flagged during that time be accurate? This is the basis of my theory that AHI is skewed by Large Leaks. During a Large Leak over 24 L/min limit, events are being counted in with the rest of the events of the sleep period. These flagged false events can produce an incorrect AHI, possibly way off the true AHI.
I suspect I have AHIs that if corrected for false events would be up to 50%+ less than the index shown.
What I am not sure about is how the machine treats hypopnea during large leaks. It does have the ability to classify apnea events as unidentified apnea or UA. I have seen those. They are apnea events, but the machine just cannot determine what type they are, obstructive or central.
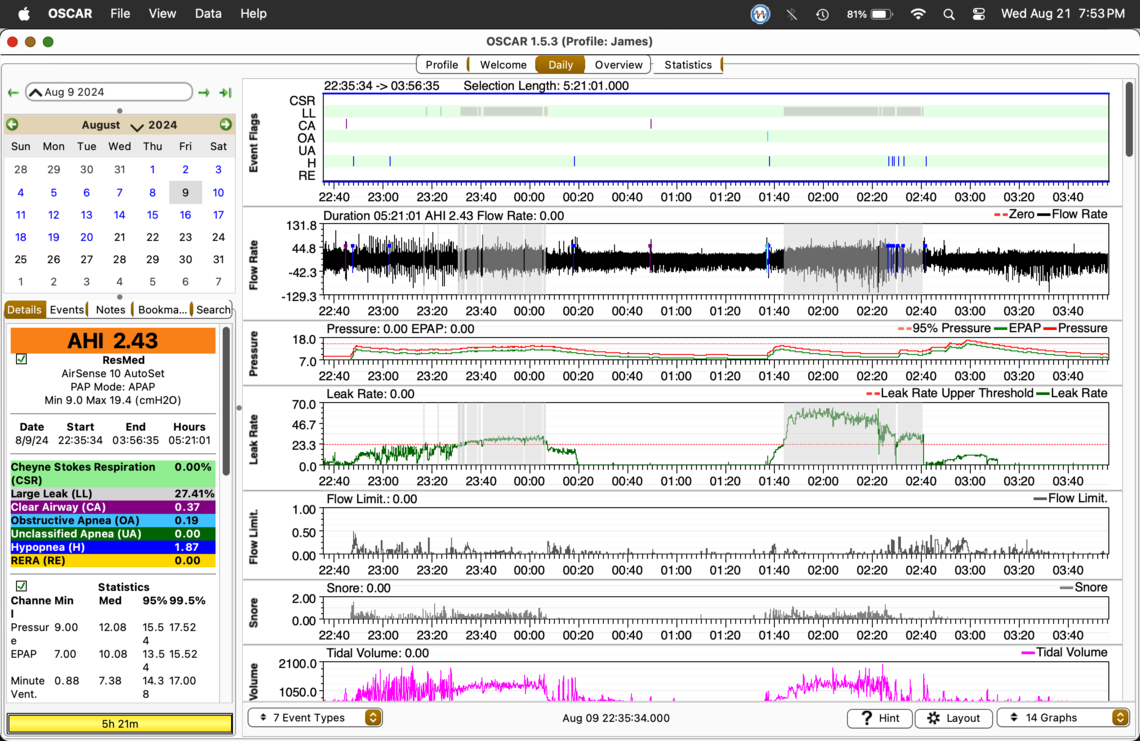
My wife had a bad night for leaks a couple of nights ago and even got the red unhappy face on the sleep report. That takes a lot to bring that up. Here is what it looked like. As you can see AHI was still very good, and no events flagged during or after the largest leak period.
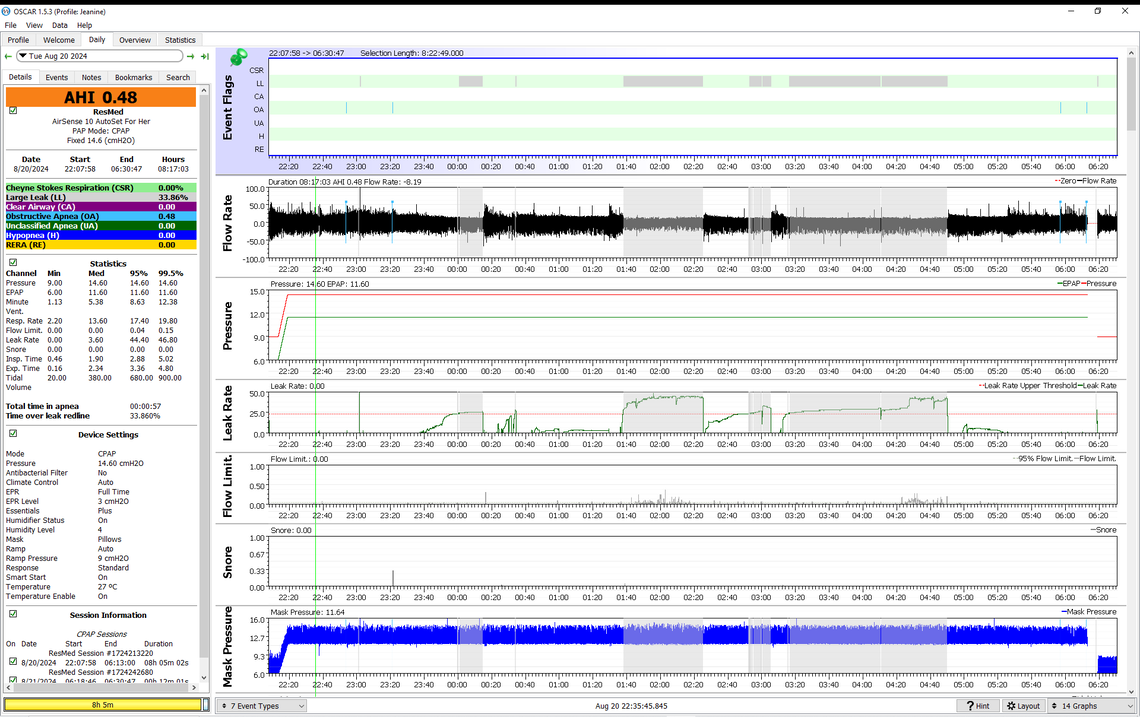
And the other thing you can do if you think the machine is not reporting events properly is zoom in and look for apnea events where there is no flow. I did that for this large leak period and only found one potential apnea event and zoomed further in on it. See this graphic. The event starts where the green vertical cursor line is and continue on for near 10 seconds. After 4 second the machine starts to oscillate the flow to test for the apnea type. You can see that as the high frequency cycle in the mask pressure, starting at 4 seconds. However it does not flag it as an apnea event. I would have expected to see it flagged as a UA. I'm thinking it ended just short of the 10 second length required before it is classified as an apnea event.
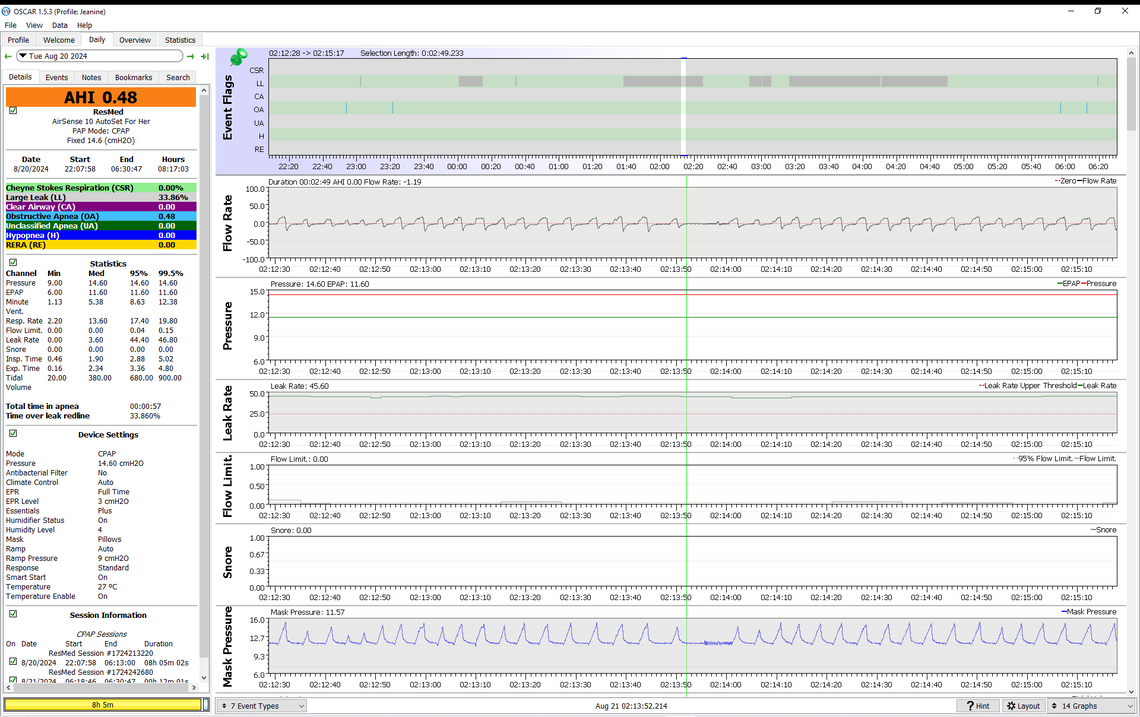
In any case you can see how to manually check for events during a high leak period manually and decide if there are missed events or not, Hypopnea is harder as I have trouble seeing what the machine classes as hypopnea. But, you could use a similar process to look for them. Find a hypopnea event that is flagged as such, zoom in and see what it looks like, and then search for that pattern during your high leak rate periods to manually look for them.
If you think your machine is not responding properly to events due to high leakage you can always switch to fixed pressure CPAP mode. That is how my and my wife's machines are set. Unless the leak is super huge, like the mask falling right away from the face, the pressure is maintained right through the high leak periods. The standard way of switching to a fixed pressure is to look at the statistics page and find your long term average of the 95% pressure and then just set the fixed pressure at that value.
Hope that helps some,
Thank you for the help. I will let go for now of my recent obsession with events flagged during Large Leaks. What I consider bizarre is how during LL sessions 70 OA events can register over 30 minutes. That is suffocation, and I don't think it is accurate.
If my machine is set to past 10 cm pressure no full face mask will stay sealed on me. I call it a blowout when a seal cannot be made. By week two on a new mask cushion, I have to cinch straps tighter and tighter to keep leaks down. It becomes painful.
Using APAP I have recurring themes of pressure up leaks up and leaks up pressure up. I tried straight CPAP @ 8 cm and had the worst AHI ever... 17.00 so back to APAP.
I raised my Min. pressure to 9.4 cm using my new F40 mask. Flow limitations went down but the rise in CAs caused an unusually high AHI yet I think therapy went better than usual. Two rested days in a row with my new F40 mask is very impressive. Leaks went up, AHI went up, but I felt more rested than I have in years. Finally, maybe a mask that somewhat works.
CPAP therapy has been very disappointing for me for over 17 years. I see a doctor once a year. Nothing is checked or disgusted. It was just last year my compliance was verified. For 14 years I complied with therapy even though it never made me feel any better. I am sure I am not alone. With time to get into the nit and grit of OSCAR reports over the past couple of years, I just may be on the verge of effective therapy. If it were not for online volunteers like you I would have no guidance...AT ALL.
Maybe someday CPAP machines and OSCAR will be at a higher AI level and be able to fine-tune therapy on the fly.
My next quest is to copy/paste my OSCAR Statistics to a spreadsheet and then produce line graphs from the data. The bar graphs of OSCAR Overview are too busy for me to track trends. It is a sort of "can't see the forest for the trees," effect I get from staring at those bar graphs.
Best of luck to you and your wife. ejb
Just another view..... be VERY careful about making any changes to your cpap pressure without reviewing that with your MD. It is real easy to set them too low or too high and create more problems. Talk to your MD before making any pressure changes.
My MD does not set cpap features nor does my DME. It is all up to me and advice I can get from forums like this which is a common state of many. Point is that my median pressures are skewed by a session of apneas that the machine cannot supply therapy to therefore the median and the high pressure are not the optimal setting. I must factor out the large amount of apneas that occur under high pressure to get a realistic figure for min./max. cm. and AHI. What good is an AHI of 10.0 when 97% of those apneas happened during an untreatable session of positional causation?
I have managed to get Large Leaks down to get a more accurate AHI on OSCAR reports. I, unfortunately, have to tighten straps to a quite uncomfortable level to prevent what I call blowouts that ruin therapy due to loss of mask pressure. I am now getting consistently lower AHIs.
I resolved the blowouts by easing up on the side straps, snugging up the top strap a bit more and, more importantly, lowering my machine pressure to 8 wish. This is because the mask face seal is supposed to work by closing in on itself(reverse acting) and I had too much mask pressure and too much strap tension. This seems counter-intuitive but it worked.