I have been on CPAP treatment for Sleep Apnea for about one year and the results have been dramatic: the AHI's went down from about 40+ per hour to about 0.50 avg, with no OA’s, mostly brief hypopneas and occasional RERAS. The results have improved even more after my doctor has recently increased the mask pressure to 12-16 H2O, with an option to increase it to 14-16 if needed. I believe my sleep it is not yet optimal , though, as l still experience some sweating and back aches at wake up, albeit not regularly and i wonder if further increasing the mask pressure would help to further reduce hypopneas and RERAS and, generally, improve my sleep. In fact, contrary to what I expected given the severity of my disorder, I never felt subjectively any changes or improvement in my sleep quality after starting treatment, none of those …AHA ! feelings of relief many people report after their sleep dramatically improves by undergoing treatment. The only tangible difference is that I no longer need to wake up several times to relief the bladder. A big relief, but perhaps I still have some way to go, even though at 79 I cannot expect the same quality of sleep as when I was younger. I know that, in the end only a doctor can make recommendations on this, but I was wondering if there are people who have noticed reduced hypoapneas or RERAs after increasing the pressure.
Thanks
Ittiandro
Apap machines are a wonderful mode of treatment as they can be set in a range of 4 cm to 20 cm and anything in between. You are correct in saying the doctor is the only one who can prescribe the pressure setting. I was in Sleep medicine for nearly 25 years and patient support was my forte. I can tell you this, your AHI is not the only factor to look at. An AHI is a index of all your apnea activity so if your index went from 40 to 0.5 I’m certain your hypopneas are treated also. Your oxygen level is also very important. If that is coming up to normal and your leak is acceptable and it sounds , from what you stated ,your AHI is down and your compliance is good, then your on a good path. Your not waking as often which is probably indicative of getting through your REM stages. All seems like a perfect remediation with only a suggestion and that is to let you pressure range end at 20. It won’t reach it if you don’t need it but on the other hand if you set the max too low it can’t go above that pressure.
Not everyone feels the WOW! You should however see improvements in small ways, no snoring, wake up much less tired, less naps or none at lol, and if for some reason you could not use the mask for a couple of days I’m sure you would notice a difference from the nights you do sleep with it. All in all it sounds like you’re very happy with your progress. Kudos and keep up the good work.
I was diagnosed with an AHI of 37 and with CPAP it has been reduced to under 3 or so. I never had any big AhHa moment. My wife likes that I don't snore any longer. Based on your success with EPR I decided to try it again along with my fixed pressure. After trying a few different combinations I am now using the same fixed pressure of 11 cm but now with a full time EPR of 2 cm. It is working very well to reduce my reported AHI. I had gone over 600 days with the same setting of 11 cm with no EPR and averaged over that time an AHI of 2.1. With the new settings and an EPR of 2 I have averaged an AHI of 0.74 after 19 days. The hypopnea has been reduced to close to zero. While it is nice to see the lower numbers I really do not notice anything different about my sleep. No AhHa moment from the lower numbers.
My thoughts are with the OSCAR reports that you have posted that there is no further opportunity for improvement with more pressure on your CPAP. You could have the maximum pressure increased to 20 and see what the machine does. However, what I would be worried about is that the higher pressure would cause more discomfort and than it would provide benefit. My overall strategy is to keep the pressure as low as possible while still giving good AHI results. Higher pressure can also cause CA events to increase.
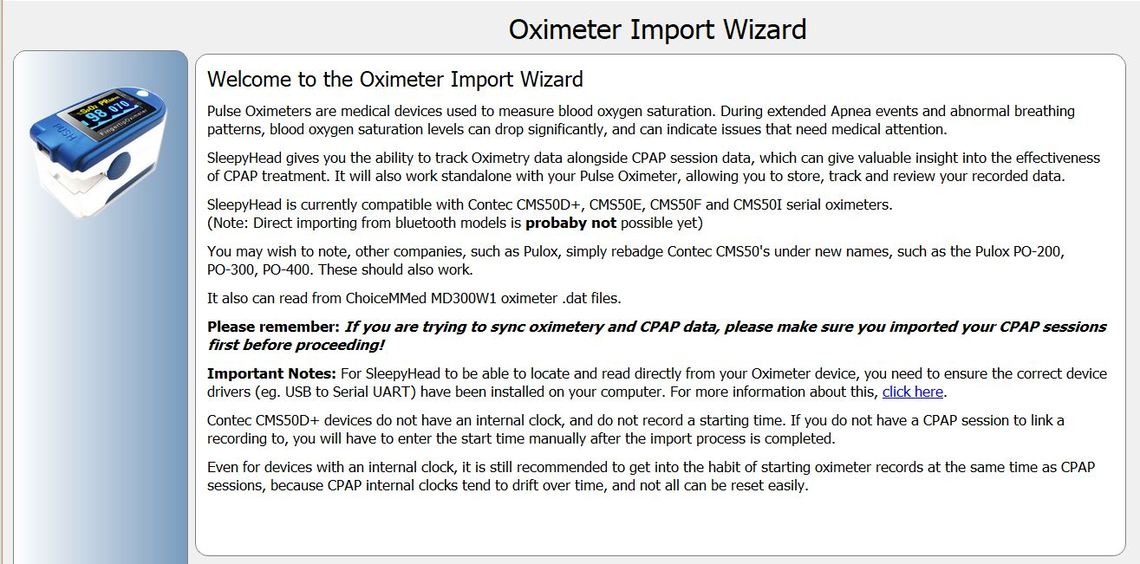
Some people use an oximeter to monitor their oxygen levels during the night. If it is a compatible machine the results can be imported into the OSCAR program like you can import your CPAP data. I still use SleepyHead but I assume OSCAR is similar. Here is a screenshot of what the Oximeter introduction screen looks like. You should look at the similar screen in OSCAR if you are going to buy an Oximeter to ensure it is going to be compatible with OSCAR. I have no experience with them, but it might give you some idea as to whether or not your oxygen levels are going low at night despite having good AHI results. On the advice of a doctor there are fittings you can buy for you CPAP tubing that allow you to use supplemental oxygen with your CPAP. You would need their advice as to whether or not you would benefit, and how much oxygen should be used.
Hi Sierra, Started cpap therapy three months ago with a mixed bag of results, using Resmed AirSense 10 autoset and nasal mask.
AHI numbers are typically under 10, with umbers ranging from 15 to 24 15% of the time. Minimum start pressure is 6.8, max is 8.2 with no ramp time. At times, I blow raspberries, which my pulmonologist suggested might be due to max pressure being too high.
With covid and in lieu of an overnight sleep study, my pulmonologist recommended I turn on the EPR function, as well as experiment a bit with max pressure settings. I’ve read some of your posts and must admit, have difficulty understanding hoe EPR works, but hoping you could provide a bit more insight as to how I might use EPR.
Thanks a lot for the information you provide - it’s very helpful.
Can you provide more detail on what the components are of your AHI? How much is OA (obstructive apnea), CA (clear airway or central apnea), and H (Hypopnea)?
There are some ways to get a little more detail out of the AirSense 10 machine by setting it to provide a more advanced sleep report. Post if you want to know how.
If I am reading this right you have your minimum pressure set at 6.8 cm and maximum at 8.2? If so, that is not very high, and your main problem may be that the maximum is too low.
EPR is normally considered a comfort setting, and in most cases it can cause AHI to go up instead of down. That said Ittiandro has had some success with it, and so have I. Would need more detail to determine if you would benefit or not. For sure AHI's of 10 to 24 are not that good. Normal guidelines are to get AHI under 5.
Thanks so much for your reply, really appreciate you getting back to me.
My min pressure was at 6.2, not 6.8, and I have a ramp time of 5 mins. Max pressure of 8.2 and using nasal mask.
I use the MyAir app, but don’t have a reader for the Airsense sd card. Just purchased from amazon but wouldn’t be able to provide you detailed data. Ok to get that info to you as soon as available?
When I’ve tried to increase my pressure, it’s seems like I blow more raspberries. Will try to up my pressure tonight, but any idea about how I might stop the raspberries?
Is there a site that has more info on OA (obstructive apnea), CA (clear airway or central apnea), and H (Hypopnea) in layman’s terms? Have no idea how these events impact my AHI number.
Yes, saw how improved both your and Ittiandro ‘s results have been. Certainly would like to give if a try.
8.2 is not a very high pressure. You talk about making raspberries. I take it that means you are blowing air out your mouth? If so, that is one issue with using a nasal mask. People that can keep their mouth closed are OK with it. Those that can't have a problem. One solution is to use a mask that covers your mouth as well as your nose. Another solution is to tape your mouth shut. I have to admit that I do that.
If you have a SD card reader and PC or Mac you can look at the detailed data with OSCAR. It can be downloaded from this OSCAR link.
Here is a link to a basic introduction to Apnea. In simple terms OA or Obstructive Apnea is when the airway simply collapses and prevents air flow. It is the most common and easiest to treat with a CPAP. The CPAP just uses air pressure to open up the airway. CA or Central Apnea is when the brain for reasons that are not totally understood simply does not tell you to take a breath. The airway is not collapsed and more air pressure does not help as it is already open. H or Hypopnea is when the airway is restricted but not obstructed. They are all added together to get the AHI.
Hope that helps some. If you have more questions, just ask...
Thanks a lot for all your help. Hoping to have sd card reader by tomorrow - should have a report in a few days, if you wouldn’t mind taking a look.
Think I’ll try to up my pressure a bit to see how I respond.
And yes, the raspberries I was talking about was just a blowing out of my mouth. Happens some nights, not others.
Thanks again for all your help! Really appreciate you taking the time to help!
Some users report being able to hold their tongue at the top of their mouth and up against the top teeth to prevent air leakage out of their mouth. I can do it, but sustaining through the night is a problem for me. So, I just tape my mouth. Here is a link to a video on it.
Thanks a lot - will definitely give that a try.
I was able to draw my data from the Resmed sd card. Think you could take a look and let me know what you think? This is over the last 30 days. Just upped my pressure to 9 two nights ago. Thanks again for all your help.
AHI 10.24 Obstructive Index 0.70 Hypopnea Index 2.41 Clear Airway Index 6.74 RERA Index 0.06 % of time in Cheyne Stokes Respiration 8.22% Average Leak Rate 4.14 95% Leak Rate 22.80 % of time above Leak Rate threshold 3.88% Average Pressure 7.44 Min Pressure 6.20 Max Pressure 9.00 95% Pressure 8.18 Average EPAP 6.37 Min EPAP 4.40 Max EPAP 7.20
It would be best to post a Daily Report screenshot of this night. Don't post more than one screen shot or it can get hung up in the spam filter here. Assuming you have a PC with the Daily report full screen just press the F12 key and keep an eye on the bottom right corner of the screen. It will display where the screenshot has been saved on your computer. Then with File Explorer find that file, left click on it and drag it to an open post here. It should upload. It is best if you start a new thread of your own, and use a full width window, not the reduced width ones like this is when your respond to a post.
I can comment better when I see it. On a quick look at your data your biggest issue seems to be clear airway events, and Cheyne Stokes Respiration. In general that condition does not respond well to increased pressure.
Trying to attach a screenshot, and post to original thread, but posts don't seem to be going through - sorry about that . I've got the text of my daily data - hope this helps. Had a total of 66 clear airway events, which seems pretty high.
AHI 10.74
ResMed AirSense 10 AutoSet PAP Mode: APAP Min 6.4 Max 9.0 (cmH2O)
Date Start End Hours 5/10/2021 21:51:02 05:29:12 07:38:10
Cheyne Stokes Respiration 14.41%
Large Leak 0.02%
Clear Airway 8.64
Obstructive 0.92
Unclassified Apnea 0.00
Hypopnea 1.18
RERA 0.00
Channel Min Med 95% Max
Pressure 6.40 7.96 8.90 9.00
EPAP 4.40 5.96 6.90 7.00
Minute Vent. 0.00 6.25 10.75 14.75
Resp. Rate 0.00 13.80 17.20 24.40
Flow Limit. 0.00 0.00 0.03 0.22
Leak Rate 0.00 0.00 9.60 18.00
Snore 0.00 0.00 0.00 0.00
Insp. Time 0.48 2.16 3.40 5.22
Exp. Time 0.06 1.98 2.72 5.04
Tidal Volume 0.00 440.00 780.00 1160.00
Total time in apnea 00:23:19
Time over leak redline 0.022%
Machine Settings
Mode APAP
Pressure Min 6.40 cmH2O
Pressure Max 9.00 cmH2O
Antibacterial Filter No
Climate Control Auto
EPR Full Time
EPR Level 2 cmH2O
Essentials On
Humidifier Status On
Humidity Level 4
Mask Nasal
Ramp On
Ramp Pressure 6.40 cmH2O
Ramp Time 10.00 Minutes
Smart Start Off
Temperature 27 ºC
Temperature Enable 1
Trying to attach a screenshot twice, but post didn't seem to go through. I've got the text of my daily data - hope this helps and sorry not able to post screenshot. Had a total of 66 clear airway events, which seems pretty high.
AHI 10.74
ResMed AirSense 10 AutoSet PAP Mode: APAP Min 6.4 Max 9.0 (cmH2O)
Date Start End Hours 5/10/2021 21:51:02 05:29:12 07:38:10
Cheyne Stokes Respiration 14.41%
Large Leak 0.02%
Clear Airway 8.64
Obstructive 0.92
Unclassified Apnea 0.00
Hypopnea 1.18
RERA 0.00
Channel Min Med 95% Max
Pressure 6.40 7.96 8.90 9.00
EPAP 4.40 5.96 6.90 7.00
Minute Vent. 0.00 6.25 10.75 14.75
Resp. Rate 0.00 13.80 17.20 24.40
Flow Limit. 0.00 0.00 0.03 0.22
Leak Rate 0.00 0.00 9.60 18.00
Snore 0.00 0.00 0.00 0.00
Insp. Time 0.48 2.16 3.40 5.22
Exp. Time 0.06 1.98 2.72 5.04
Tidal Volume 0.00 440.00 780.00 1160.00
Total time in apnea 00:23:19
Time over leak redline 0.022%
Machine Settings
Mode APAP
Pressure Min 6.40 cmH2O
Pressure Max 9.00 cmH2O
Antibacterial Filter No
Climate Control Auto
EPR Full Time
EPR Level 2 cmH2O
Essentials On
Humidifier Status On
Humidity Level 4
Mask Nasal
Ramp On
Ramp Pressure 6.40 cmH2O
Ramp Time 10.00 Minutes
Smart Start Off
Temperature 27 ºC
Temperature Enable 1
You appear to be getting central apnea due to the increased pressure. This may be a more serious condition than can be treated with a APAP machine. If you want to try a simple change, and are comfortable with adjusting your machine, I would make the following changes:
This would be a test to see if it can reduce your CA events. If it helps there may some other improvements that can be made.
You should be able to capture a screenshot by just pressing the F12 key. The file should be saved in a directory location like this:
C:/Users/(Your Name)/Documents/OSCARData/Screenshots
The key information is the events bar and the Pressure graph
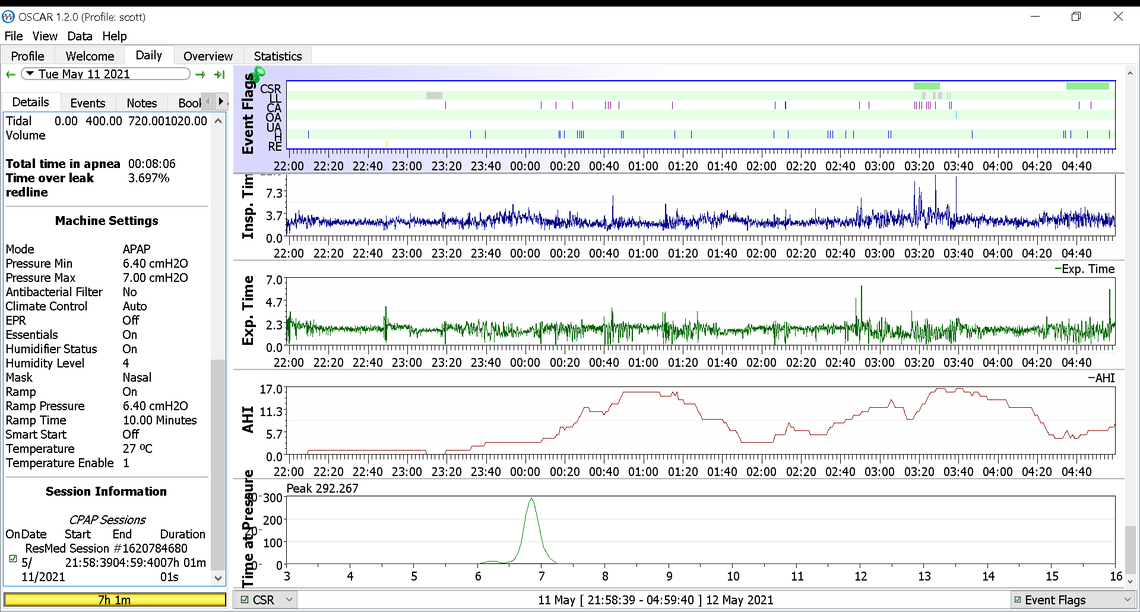
The good news is that CA events went down and OA events did not go up. The hypopnea events are still high but they are less severe than CA or OA events. My suggestion for machine settings would be to lower the pressure some more to see if the CA events can be reduced even more without increasing OA significantly. My suggestion would be a minimum of 5 cm and maximum of 6 cm to see what that does. You will also have to lower your Ramp Start pressure to 5 cm as it cannot be higher than your minimum pressure. If this helps with CA events and OA are still good, then they next step would be to turn the EPR back on again. But, leave that until you see what simply reducing pressure does. It is best to just make one change at a time so you know what to attribute the outcomes to.
Do you live in an area of higher elevation like Denver? That can contribute to central apnea. Some medications can also cause central apnea, as well as some heart conditions. Here is a Mayo Clinic link where you can do a bit of research.
I can't thank you enough! You're response and advice are greatly appreciated! I feel like I've got a bit of control over using my cpap, and with some continued tweaks my numbers will lower to under 5.
I'll try lowering ramp to 5 and max pressure to 6 to see how that works. I'm in New Jersey so elevation isn't an issue. I am taking medication for hypothyroidism - 100mcg of Levoxyl daily. Read that thyroid issues might impact sleep apnea, but not sure if that applies to individuals that are being treated.
Thanks again for all your help!
I hope you are doing ok with your machine setup. The next steps I would consider would be to turn your EPR back on with it set at 2. If that works OK then another thing to consider once you know what pressure controls OA events but does not cause excessive CA events is to switch the machine to CPAP mode and then just set a single fixed pressure. That is how I run mine.
If CA and Cheyne Stokes respiration events keep happening then you really should see a doctor about it to be sure there are no underlying conditions and in particular heart issues that are causing it.
There is a limit to what a standard APAP machine can do when central apnea is an issue. Some sleep clinic will try to sell you a BiPAP machine instead of an APAP, but usually they do not work any better. They can provide more pressure but pressure is not what you need. The specialized machine made to deal with central apnea is called Adaptive Servo-Ventilation or ASV. Before they are prescribed there are some heart function tests that need to be done to ensure they are suitable for your condition. Here is a link that talks about it.
Pros and Cons of Adaptive Servo Ventilation
They are expensive, but for some that is about the only way to deal with the high CA events.
Thanks so much for checking up! I appreciate you taking the time to help me!
These are my numbers for the last few nights:
5/11 Ramp: 6.4
Fixed: 7
Mode: APAP
AHI: 8.12
CSR: 8.4
CA: 3.85
Obs: .14
Hyp: 4.13
RERA: .14
5/12 RAMP: 5cm
Fixed: 6cm
Mode: CPAP
AHI: 10.53
CSR: 10.07
CA: 6.78
Obs: .29
Hyp: 3.46
RERA: 0
5/13 Ramp: 5.6
Fixed: 6.6
Mode: CPAP
AHI: 10.58
CSR: 5.69
CA: 7.33
Obs: .36
Hyp: 2.89
RERA: .12
5/14
Ramp: 6
Fixed: 7
Mode: CPAP
AHI: 14.59
CSR: 18.32
CA: 8.87
Obs: .45
Hyp: 4.96
RERA:.15
I had 3 beers last night, and my numbers went up. But typically on nights where I'll have a glass or two of wine/beer, and my AHI is 5 or under. Weird, I know.
Over the last 104 days, I've had CSR events under 6.0, 58 times, and 0.0, 39 times. Spoke with my pulmonologist after a month of therapy, and my CSR and CA events were quite high. She wanted to wait another 6 weeks before doing an in-clinic sleep study. Within that period, my AHI numbers improved significantly. It's only been over the last two weeks that my numbers have gone up quite a bit. I'm noticing I'm sleeping on my back more, but don't know if that would impact CSR or CA events.
I'm 49 yrs old, BMI of 24.4, have regular physicals. Started doing some reading on CSR events and got a bit nervous. Was able to schedule an appt with my pulmonologist Monday, so hope will be able to get some better direction. Thanks again for all your help! Can't tell you how much I appreciate it!
You may also want to consult a cardiologist about the CSR. From the numbers you post, it does not look like you are going to resolve the CSR and CA event frequency with just lower pressure. You may also want to discuss the use of an ASV instead of a CPAP if cleared to do so by the cardiologist. This document discusses the screening process to consider the use of an ASV.
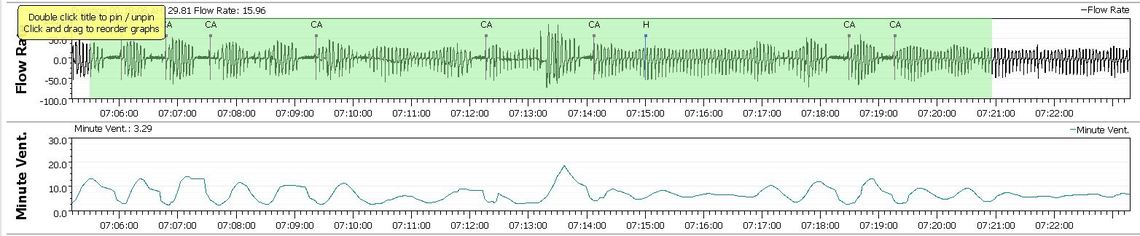
You may have figured it out but if you click repeatedly on a green area highlighting CSR you can bring up the expanded detail on your breathing response to compare it to what you see in this document. My long term CSR is 0.02%, so I see it occasionally but not very often. Here is an example of what I see when I zoom in. Minute Ventilation cycling is another indicator of CSR. In the worst cases you can get a CA event between every CSR cycle. That racks up CA events pretty rapidly...