While reviewing my sleep reports in Sleepyhead, I notice that I nearly always have a big increase in central apneas in the hour before I wake. I believe that these may be responsible for me feeling in a fog until noon.
Has anyone else noticed this? Has anyone found the reason and what can be done to reduce these central apneas?
My all night AHI hovers around 5-7, but just before waking it can shoot up to 19, with nearly all central apneas.
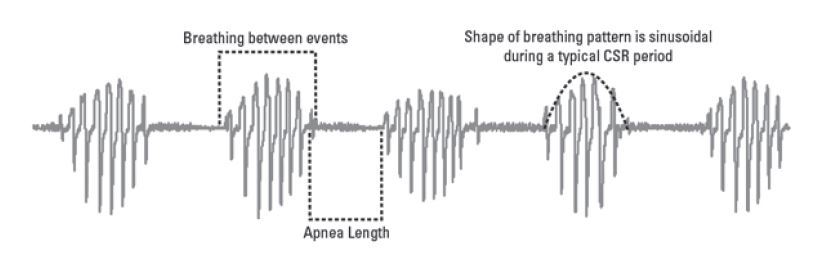
There are two things that I can think of to consider. One is that for whatever reason you have or are bordering on cheyne stokes breathing. Have you expanded your flow rate (use up arrow when cursor is over the area of interest, or keep left clicking) to see what it looks like around the events? You can recognize the cheyne stokes pattern by the rhythmically increasing and then decreasing flow rate with each breath. See this link for an example of what it looks like.
Recognizing it is easy. Figuring out the cause is much harder. The most frequent reported cause of central apnea is the use of opioids or similar sedatives. Heart disease unfortunately is another potential cause. Lower blood flow seems to negatively affect the breathing control system. That said I have it from time to time and I know I don't use opioids, and hope I don't have heart disease. I do use bisoprolol (beta blocker) for blood pressure control and I have blamed that, and even had my doctor cut my dose in half. I think the frequency of it went down, but not away.
There are some things that can be done with a BiPAP machine like the AirCurve 10 Auto. It involves the timing of pressure support on inhale. The more direct way is with a ventilator like the AirCurve ASV, but that would be for pretty serious cases of central apnea probably along with other heart or breathing conditions.
The other possibility is what some call sleep wake junk. That is when you keep waking up and going back to sleep. In that situation your body can simply forget to breath and that is flagged as an apnea. It can be recognized by a more garbage looking breathing pattern than the rhythmic breathing of Cheyne Stokes. Some would say that this sleep wake junk is not real apnea, but if you stop breathing, you stop breathing. One possible cause is trying to sleep too long. Most people only need from 7-8 hours per night. If you are sleeping much longer than that, you are likely going to be having wake up and go back to sleep issues toward the end of the night. Here is a video that is quite annoying to watch, but if you can endure it, the guy does give a few bits useful information as to what the various types of events look like.
Hope that helps some...
There's a bit more to recognising Cheyne-Stokes respiration than just the characteristic wax/wane pattern. While that is part of it, many other forms of central apnoea can have they same wax/wane patters as happens in Cheyne-Stokes. To be true Cheyne-Stokes it must also be accompanied by a low carbon dioxide levels. This is part of the mechanism of Cheyne-Stokes. It is a rise in your CO2 level, rather than a decrease in your O2 level, that tells you when to breathe, however, your body can only properly monitor your CO2 levels within a certain range. If it gets too high then you body can no longer see the very small increase and decrease which triggers your breathing mechanism, so it then switches to O2 drive meaning that it is your O2 levels that triggers your breathing response. The problem with this is that your body is much worse at monitoring its O2 levels than CO2, so your breathing is much less stable on O2 drive. If your CO2 levels go too low, as in Cheyne-Stokes, then your body just thinks "cool, I don't need to breathe" and so it stops. after a while of not breathing your CO2 will come up again and restart your breathing mechanism, which will send it too low again and repeat the cycle. This is what causes the wax/wane pattern of Cheyne-Stokes breathing. The difference is very important because to fix someone with elevated CO2 levels you need to help them breathe more, thus getting more O2 in and blowing more CO2 out and pushing CO2 levels down. If you do this to someone with Cheyne-Stokes breathing you will send their already low CO2 even lower and only make things worse.
Appropriate treatment for any form of respiratory failure is not really about which machine is used so much as it is about how it is set. Some different machines do have different settings available, but unless they are set in a manner appropriate to the condition of the patient, they will be useless.
Cheyne-Stokes is just one form of central apnoea and far less common than others. Each requires its own tailored response.
I hope that is useful for you.
This is an example of what my ResMed A10 flagged as Cheyne Stokes in July. It gets highlighted in green. My conclusion is that it is a breathing rate control system instability. This one started with an obstructive apnea, and the instability it caused was flagged as Cheyne Stokes. You can also see that the instability was there before that but not bad enough to get an apnea flag. Flow rate in the top graph, and mask pressure in the lower.
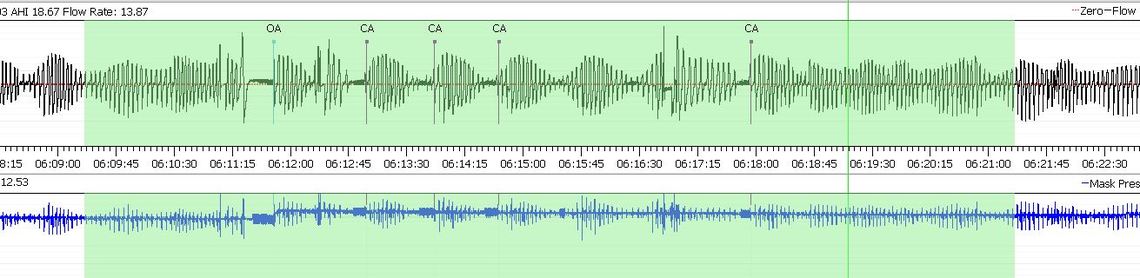
When a machine reports Cheyne-Stokes breathing it's just guessing. It really doesn't know. It is quite common to see some Cheyne-Stokes on a download but it is almost always not real Cheyne-Stokes. That looks like series of post-arousal events. Cheyne-Stokes doesn't start and stop that quickly.
Another example an hour or so before waking.
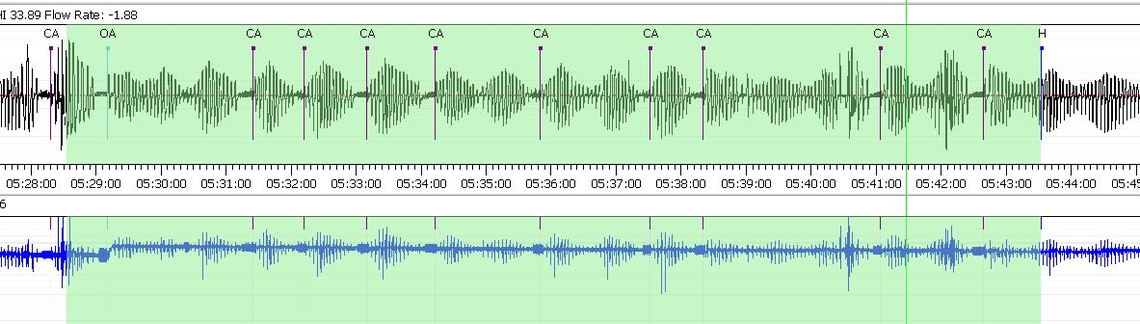
Sure looks like the example in the ResMed Clinician Manual to me. About the only difference is the length of the apnea period. Mine are around 10 seconds, so most, but not all get flagged as CA's.
There doesn't even need to be a total apnoea for it to be Cheyne-Stokes. I agree that the second sample has a fairly appropriate shape but, as I mentioned above, Cheyne-Stokes cannot be properly diagnosed without a CO2 level as well. When data from a machine reports Cheyne-Stokes it is really just an indication, not incontrovertible fact. It's a bit naughty of them to claim to be able to diagnose something which they really can't. All data from a download is best interpreted in the light of medical history, other downloaded data, recorded sleep studies etc.
Also, the ResMed Clinician's manual isn't exactly the best source for detailed technical info on scoring of sleep. There are international standards for how these things are assessed and it's a bit more complicated that the RedMed manual suggests.
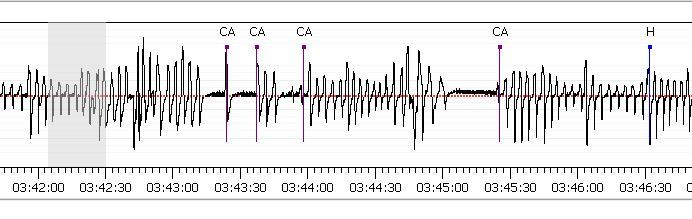
I should also have posted a clip of what I think Sleep-Wake-Junk looks like. See image below. This type of central apnea concerns me much less than the ryhthmic stuff. In this clip, I think I woke up due to mask leakage (grey area) and then the CA events were the result of going to sleep and waking up and simply not breathing.