I copied my previous response to you on EPR below. I won't repeat that part again. What is new is your question about leaving EPR on full time. The problem with EPR is that it reduces your exhale pressure. Apnea can occur on inhale or exhale or the transition from one to the other. If for example you have a set pressure of 8 cm and an EPR of 3 then all night long the pressure will cycle from 8 cm to 5 cm on each inhale and exhale. If you are susceptable to apnea event on the transition or during exhale your effective treatment pressure is only 5 cm. But, you are having to endure a pressure of 8 cm on inhale. You may get almost the same benefit in apnea prevention by running a fixed 5 cm pressure.
The short story is that if you want to know what your effective treatment pressure is, then you have to subtract the EPR value from the set pressure. And if a set pressure of 8 cm and EPR of 3 works for you and feels comfortable then leave it that way. It indicates you really only need 5 cm, but that does not matter much. What works for you works for you.
" EPR stands for Expiratory Pressure Relief. It causes a reduction in the mask pressure when you breath out compared to when you breath in. The number is an approximate pressure reduction in cm of water pressure, often just called cm. Let me give an example:
If your therapy pressure is set at 8 cm, and you have EPR set at 3 cm and is turned on, then you will get 8 cm of pressure when you breath in. And you will get 5 cm (8 less 3) when you breath out. Now if you have a set pressure of 4 cm and and EPR of three, the EPR tries to reduce pressure to 1 cm on exhale. However, the machine is designed to never let pressure go below 4 cm. So in that situation the EPR does nothing. You will get 4 cm on inhale and exhale.
So if you set it up with the ramp in auto, a start pressure at 8 cm, and EPR at 3 for ramp only, it will go through this sequence. When you are still awake it will give you 8 cm on inhale, 5 cm on exhale. Most find that very comfortable. Then when you go to sleep, it will stop reducing the pressure on exhale. Most do not notice this change when they are asleep.
There is nothing magic about setting the ramp start pressure at 8 cm. If you find that too high, then try a ramp start pressure of 7 cm. Then it will do 7 cm on inhale, 4 cm on exhale, and then ramp up to a constant 8 cm when you go to sleep. The problem with setting the ramp start at 4 cm is that most people will find that too low, and feel like they are suffocating. I personally have a ramp start at 9 cm. I find that very comfortable, but everyone is different. Most with experience prefer a high pressure. A higher inhale pressure makes it easier to breathe.
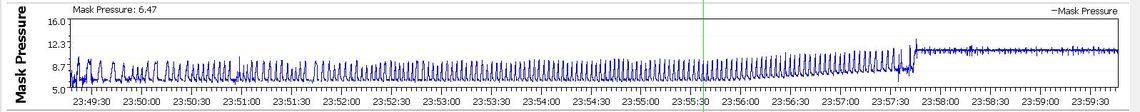
Here is an example of how my machine works, as shown with SleepyHead. This is with an auto ramp, a ramp start of 9 cm, EPR at 3 cm, for ramp only, and a therapy pressure of a fixed 11 cm. You can see how mask pressure cycles between 9 cm and 6 cm for each inhale and exhale. Then when breathing becomes regular and it detects I am asleep (about where the green line is) the pressure ramps up from 9 cm to 11 cm, and then finally stops the reduction on exhale.
You asked whether 8 cm was a high pressure. My opinion is that it is a quite low pressure. Your machine has a maximum of 20 cm. Some machines go up to 25 cm. So if you think 8 cm is a lot, consider that some are using three times that amount."
Hope that helps some.
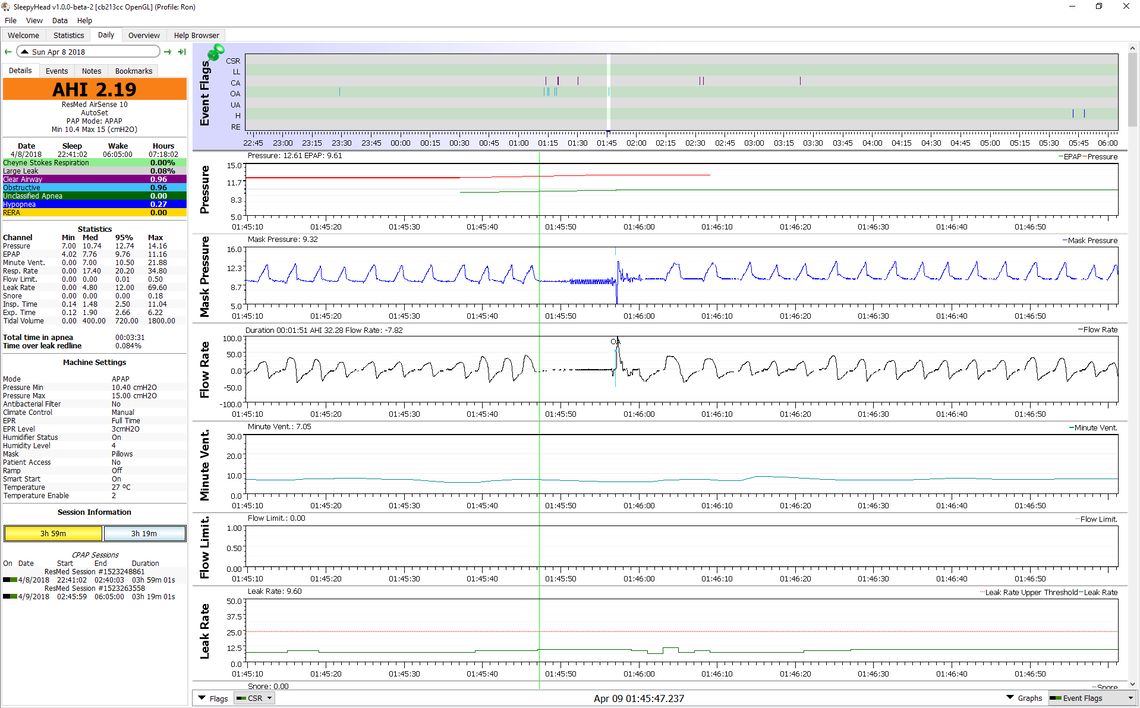
Here is perhaps a better way to explain it. This is one of my SleepyHead reports from about a year ago when I had EPR set at 3 cm Full Time. My pressure was in Auto with a minimum of 10.4 cm and a maximum of 15 cm. The apnea event flagged as obstructive (OA) occurs when the inhale pressure was hitting about 12 cm on each breath. Then when the apnea event starts where the green cursor line is, the pressure is at about 9.4 cm. Flow stops, and then about 4 seconds later the machine starts to try to cycle the pressure and flow up and down to test if there is an obstruction. When there is the pressure goes up and down. Then it finally gets flagged as an OA. the point is that even though my pressure is going up to 12 cm, the obstructive event started at the lower 9.4 pressure. That is due to the EPR reducing pressure on exhale.
And another way to think about it is if you were prescribed an 8 cm pressure that was likely determined in the lab with no EPR on. So when you go home and start to use EPR then you are not getting the same pressure that was determined to be effective in the lab.
CPAP and Auto CPAP are considered to be single constant pressure machines, though auto will algorithmically alter that pressure. Point here is you are only dealing with one pressure. EPR is intended to be a comfort setting by ResMed and the Medical community. It subtracts 1, 2, or 3cmw from your pressure "for comfort". I'll get back to this later. Titration on CPAP is based on having only one pressure and as such inhale = exhale or IPAP = EPAP
BiLevel machines operate totally without EPR but with a different pressure for inhale and exhale called IPAP and EPAP. The difference between these pressures is called Pressure Support or PS. Titration protocols call for increasing the EPAP pressure to resolve obstructive events. This is identical to raising the pressure on a CPAP. IPAP pressure is also increased to match the increase in EPAP pressure generally keeping the PS the same.
Now the question is why have 2 different pressures?
Officially CPAPs do not number 2 above. Unofficially by manipulating EPR and Pressure settings they can, up to the limit of 3cmw available with EPR. This is also why if someone just throws EPR on they can get a significant increase in obstructive events (because they just effectively lowered their pressure settings.) So, in general, you add 1 cmw to your pressure for every 1 cmw of EPR that you add to maintain the same level of effective therapy.
Realize that Increasing EPR and Increasing Pressure can make (not in everyone) Central Apneas considerably worse. Sierra is one of those very "lucky" individuals. (Note the sarcasm)
The trouble therapeutically with ramps is that your machine is not treating you with fully therapeutic pressures until the ramp completes. Most of the long term users do not use ramps. Using EPR during the Ramp is a comfort thing, as is the ramp itself, making it easier for you to fall asleep. Because there is pressure during the ramp you are getting some therapeutic effect.
I agree with most of this. EPR and PS on a ResMed is essentially the same thing, except EPR on an APAP is limited to 3 cm. I have to disagree with the ramp comment. ResMed and I think DreamStation machines have an Auto Ramp. The Auto Ramp is smart enough to end when you go to sleep. When you are awake you are highly unlikely to have an apnea event. For that reason using EPR during Auto Ramp is not an apnea risk. The bottom line is that you can use EPR during AutoRamp for comfort, with essentially zero risk of an apnea event.
This issue got thoroughly discussed over a year ago in this thread.