I have been on a CPAP for 13 years. My "sleep professionals" deploy technology. They have never talked about sleep.
My first sleep study was in Oct 2019
Stage N3 0% Stage REM 20% AHI 25.3
Then a titration (mask fit) later in Oct 2019
Stage N3 0% Stage REM 9.6% AHI 2.6
So they fixed AHI way back then but I didn't notice about N3 and REM Watching a series on Brain Heath and the important stages are N3 and REM.
Over the years had 4 different masks, had trouble holding the seal, and occasionally get to 5 or below on AHI.
New sleep study Feb 18, 2024. I was congested so it might have been an invalid study Stage N3 0% Stage REM 0% AHI 65.1
At the end of the year I asked the sleep doctor how to increase REM. She didn't know how. Since I had lost weight she thought a new sleep study was needed and lowered the pressure. I might not need a CPAP at all she said.
I realize that the sleep study on 2/18/24 was probably corrupted because I was congested. But, but, I don't know how to work with this doctor to get good Stage 3 and REM sleep because this involves problem solving which I have not yet seen. There is a company that provides a FITCHECKER that I am going to use to get the best mask for me, but I don't know what to do about the quality of my sleep.
Question: Is it common to see State 3 at 0%? Is it common to see REM decrease during titration/mask fitting?
Comments and suggestions are welcome.
Welcome to the forum,
Some questions for you to clarify where you are at:
The breakdown of AHI is very important as a CPAP is most effective in reducing obstructive apnea events because they are caused by the airway closing down, and the pressure can open it. If they are mainly clear airway or central events then more pressure can make the event frequency increase instead of decrease.
Hi Sierra, Thanks for the reply.
I am using AirSense10 Respond
This the first time I have looked at the data. In the 2009 study _ Hypop 65, Obstruct 65, Central 10, Mixed 0, Apneas 75
AHi/Hour Hypo 25.3 Non-REM 25.7 Ren 23,5 (I am not sure about the Hypo score: it is a column with 3 numbers added up to get 25.3
This initial contact is very helpful because my "sleep doctor" never discussed these issues with me.
I am 81 years old, weigh 160 lbs. and the only prescription I have is for the CPAP. Lifestyle progress in last year got me off 4 prescriptions.
The 2/18/24 report is 7 pages with an introductory letter of 3 pages.
I was congested with drainage to my stomach. I think that that made the entire study invalid.
Here is my attempt to provide you the data. The table titled "Respiratory Events" The first row is "counts" and here are the columns for "Count" Cen. Apneas 16, Obs. Apneas 190, Mxd. Apneas 5, Hypop 9, Total Apneas 211, Apnea+Hypop 220, RERA 17, All Resp Events 237
The 2009 study was 2 pages long.
Final question. I am considering using the service of FitChecker for advice on the best mask fit. They are at maskfitar.com. I heard of them from a Dr. Talks series on sleep that ended recently.
I hope that I came close to providing what you were asking for. Sincerely Don
I am so happy to be able to discuss these issues.
I am using Resmed AirSense 10 Respond. My current mask is AirFit 30i which covers the mouth and extends to the underside of the nose
This is the first time I have looked at this data. Hypop 65 Obstr 65 Central 10 Mixed 0 Apneas 75 from 10/13/2009
Ces Apneas 16 Obs Apneas 190 Mxd Apneas 5 Hypop 9 Total Apneas 211 RERA 17 All Resp Events 237 from 2/18/24
Stage 3 0.0 REM 20.0 Study 10/13/2009 Stage 3 0.0 REM 9.6 Titration 10/20/2009
Stage 3 7.6 REM 28.1 Titration 3/9/2017
Stage 3 0.0 REM 0.0 Study 2/18/24
I noted in the original mail that I didn't think this study is valid because of chest obstruction. The primary doctor said that she reviewed the test results and said that they are valid. My hunch is that the purpose of the test is to set the stage for the next action, titration scheduled for May.
Final question. I think that the 0.0 scores for stage 3 and REM prove that the test is invalid.
Thank you Don
I have not heard of an AirSense model called Respond. Perhaps it is not North American? The common models are the AutoSet, AutoSet for Her, Elite, and CPAP. All but the CPAP model capture detailed data on the SD card. The first thing to check for is to see if there is a SD card in it. It will be in a slot on the left upper side that has a flexible cover that you have to pull back to get at the card.
You can click on this hot link to find OSCAR: OSCAR
It is free to download, but requires a SD card reader and a PC or Mac to run it. If there is a card in your machine it should have all your past data on it. If there is no card and it is a model that supports detailed data collection you will have to install a 4 to 43 GB card. They normally come from the factory with a 4 GB card.
I can't make a lot of sense of the test result numbers as they seem to be event counts and not in events per hour. Normally there is an events per hour number of each type of event which is added up to give a total AHI. Ideally one wants the AHI to be under 5. But this said you do seem to have a lot of obstructive events which means you should benefit from a CPAP machine.
There should be no need to get that Fitchecker for advice on mask fit. Your machine should have a display that has a happy face if leaks are ok, and a red unhappy face if leaks are too high. OSCAR provides a much better display of your leaks though. See an example of the OSCAR report below. There is a leak rate graph that shows the minute to minute leaks during the night. The gray areas highlight when leaks go over the "leak redline". You can see a couple of those events at 5:00 and 6:20.
There is also a detailed sleep report on your machine if it is set up properly. First lets start by figuring out if your machine has a SD card and if it supports OSCAR. Here is a link to a detailed manual on the AirSense 10 that may be of some help.
https://www.respshop.com/manuals/ResMed-AirSense-10-for%20her.pdf
Thank you again for the help. And thank you for this community. Here is an update.
I was really upset about sleep issues and the realization that my "sleep doctor" was just a technician with a CPAP tool.
When the sleep test came back with 0.0 for both Stage 3 and REM I freaked out. These are the two most important scores for cognitive decline.
As noted earlier, I thought that the sleep test was invalid because of congestion in the chest. I attempted to find out the meaning of these scores.
I realized that they don't pay attention BECAUSE there are two tests. The initial test and the titration, the second test is when they fit the mask.
They had a SUCCESSFUL initial test because it yielded a score of 60 AHI which justified the second test and the titration. They don't care about the details. They offered me a chance to come in and speak with the big cheese sleep doctor but I know she won't be of any help because a few years ago when I brought up the book "Why We Sleep" she freaked out. A challenge to her authority or something.
Looking for another sleep doctor so far has failed. I am looking for a doctor who works with lifestyle and supplements.
I have settled down from my high levels of concern and will go for titration study in May. They sure aren't in a hurry!
I have not downloaded OSCAR and begun looking at the data in my machine. I will do that in a couple of weeks when I have more time.
Again, thanks for the help.
An AHI score of 60 is very high and certainly needs treatment. The titration test is worthwhile doing, but is not totally necessary if the machine is going to be put in Auto and you are going to follow the results with OSCAR. In fact using OSCAR is better than a titration test as that is a one night stand, whereas you can look at every night with OSCAR.
Incredible! My machine was already in Auto which I verified because I now know how to check settings.
I had no idea that it was possible to work with my own data. The "professionals" were keeping OSCAR a secret.
I downloaded OSCAR and entered my profile. Under OSCAR Documents I see many that will help getting started and using OSCAR.
As noted in the original post, I think this 2024 sleep study is invalid but in 2009 the study found AHI at 25 which is high. In 2009 I was so sleep deprived that I would fall asleep while driving during the day. In any case, I do need some additional assist.
I do not have the time today to begin OSCAR and we are out of town next week, so it will be a couple of weeks until I respond on how it is going.
Once again, thanks for the help!
There is a RESMed SC card in my AirSense 10. I loaded it into my desktop and listed the files for each day.
As mentioned earlier, I will not fire up OSCAR because getting ready for a week long trip. Will do it then.
i
i
It is very good that the card is there. All the detailed data captured since the machine was first used should be on it - up to the capacity limit of the card, probably 4 GB.. You will be able to go back in time and look at all your data on a day by day and minute by minute basis. It may take a very long time for the data to be transferred to OSCAR the first time you do the data transfer. It my take hours but be patient and it should transfer. OSCAR assuming it is like the predecessor software, SleepyHead, is particular about handling the data. For some reason it may want to be loaded directly from the SD card rather than from a folder on your hard drive.
Hi Sierra,
It has been more than a month and I finally loaded OSCAR today. I loaded it directly from the card. OSCAR recommended locking the card and I did.
I have a years data. AHI for the year is 6.77. The last month it was 9.41.
The original question involved Stage 3 and REM sleep levels. Maybe the color codes on the graphs will tell the story but in the short time I have looked at it if doesn't jump out.
The doctor signed me up for a titration in May so I have some time to work on things.
A couple of years ago I had trouble with leakage and switched to a foam cushion full face mask that covered mouth and nose, and rested on the bridge of the nose. It worked OK for a couple of years. Then the pressure went up and to keep the leak under 20% I tightened the straps and ruined the flesh at the bridge of my nose.
Over the life of masks, 13 years, they have always been medium.
I am now using a Resmed F30i which is considered a full face mask. It covers my mouth and nose.
An online offering, MaskFit, cost $10 and recommended three masks. They asked demographic questions and took a scan of my face and my nasal openings. Their three mask recommendation were all large. And they are all nasal only masks.
#1. Fisher & Paykel Eson 2 #2 Phillips Respironics Pico #3 Resmed AirFit N20.
I have had trouble for years on the leak rate. I have been on the F30i for most of the year. My yearly leak rate is 22 and I though it was worse because almost everyday on the screen of the Airsense 10 it comes up red (failure to keep below 20%)
I have taped my mouth for over a year. Leave space to breathe.
Take a nap a couple times per week.
I would appreciate your thoughts.
Sincerely
Don Utter
Hi again. I looked at the video information for OSCAR and looked at daily data. My current max pressure is 13. The first day I looked at maxed out at 13! In other words, I need to increase the upper limit. I will set it for 16 this evening and look at my OSCAR report tomorrow.
All the days I looked there was no snoring.
One of the days the AHI was over 11.
The sleep technician said not to worry about numbers like that. She sees numbers in the hundreds. When I went in for my sleep study in Feb at 5' 9', 160lbs the other patients were obese.
I am trying to really improve my health. The goal is AHI less than 5 and lots of Stage 3 and REM sleep.
OSCAR sure provides a lot to play around with.
Don
Hi Hi I just found leakylefty27 on youtube. He has a video that leaky mask can cause wake up which messes things up. The other thing is the variable pressure.
Feel free to send me to various links to learn more.
It makes me angry that the medical system hides tools like OSCAR which allow people to be responsible for their own health. Making money and a prestige job seem to be what is important.
Don
A leaky mask used with a variable pressure machine, such as an APAP, etc. can result in soaring pressures. I found myself trying to exhale against what felt like a hurricane. My normal average pressure was about 11, but it went to 18 with a bad leak. That will wake you up for sure, and probably many times a night.
So, the first order of business is to get the best fitting mask you can find, and eliminate mask leaks. People often have to try five or six to get one that works optimally. You also have to eliminate mouth leaks, so use a chin strap, if necessary.
However, there IS something else that can be done: optimize your pressure settings. Your sleep lab can adjust the pressure settings to a narrow band around your average pressure. That way, even if you experience a bad leak, the upper range of the variable pressures will stay within reason, and you will avoid the feeling of trying to exhale against a hurricane.
Finally, assuming your machine has the expiratory assist setting feature, make sure it is turned on. In general, you should study your user’s manual and familiarize yourself with your machine operations and settings.
Finding is good mask that suits you is difficult. I use a ResMed AirFit P10 nasal pillow mask. It is a very minimalist mask and is comfortable. If there is a weakness, it is the headgear. Fairly recently they have come out with a somewhat improved headgear for it. I believe it is the most popular mask used. But if you open your mouth in your sleep, it is best to use mouth taping. I mouth tape every night.
With the ResMed machine events are not reported when the leak rate of the mask exceeds the redline of 24 L/min. If evens are flagged during a high leak period they should be identified as Unclassified Apnea (UA) events, and the machine does not respond to UA events. So, pressure should not increase while the mask is leaking. You can confirm that by looking at the OSCAR pressure graphs to see what the pressure does when you are having a large leak - there will be grayed out areas of the graphs when the leak exceeds the redline.
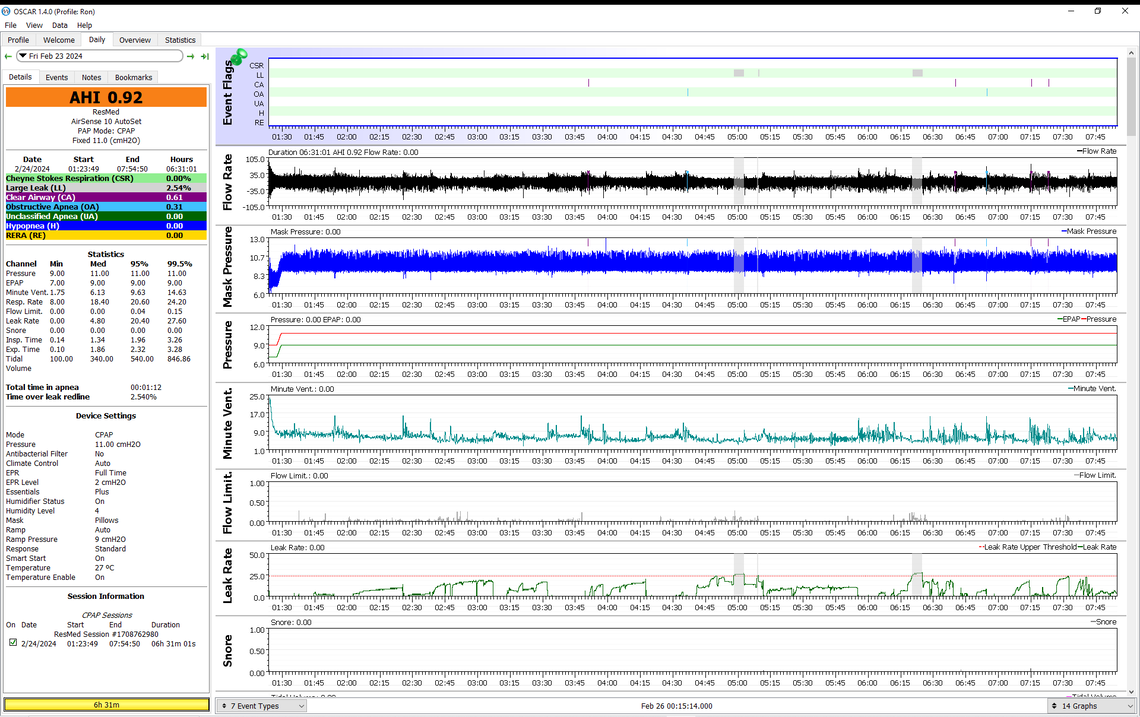
If you want to post a typical OSCAR Daily Report screen here I can take a look at it to see if there is anything obvious that can be done. To do that on a PC make the Daily report full screen with a full screen window and press F12. A box will pop up asking where you want to save the screenshot image. Save the file. Then with a full width post here, find the file with File Explorer, left click on it, and then drag it into the post here. It should upload.
Based on what you report your AHI readings do seem fairly high. What is the average breakdown of the various components of the AHI? You should be able to see that on the Statistics page. AHI, OA, H, and CA events are the important ones. The 95% pressure is also a useful number. If you have imported a year's data there should be some good averages there.
However, I can tell you the most if you post a Daily report screenshot for a typical night. I posted an example of one in an earlier post.
Hi Sierra, After finding out yesterday that my pressure was maxed out, I changed the upper limit to 16. I am going to try pasting the first page of my report from last night. This is my first attempt. Don
The first thing I would try is turning your EPR on, and set it at 3 cm. That has the potential to reduce the hypopnea (H) events, and possibly the RERA (RE) events as well. And, you have to find a way to stop the mask leaks. The leakage is way too high, and is keeping the machine from determining what kind of events you are having. It is just reporting them as UA's, or unclassified apnea which is not very informative. Of the events reported clear airway (CA), or central apnea events are the highest. More pressure does not resolve CA events as the airway is already open, and in fact higher pressure can make it worse. I think the pressure may be going too high. I would suggest you reduce your maximum pressure to about 12. Post another report after you make those changes. If you need help making the changes just ask. There are some other changes for comfort I could suggest, but this is probably enough for a first change.
I made the suggested changes. EPR = 3 Max Pressure = 12
I don't tape my mouth completely closed. Last night it was a open too much. Tonight I will be shut more.
I use standard surgical tape.
The lankylefty27 recommends not using auto sense. That may be something to try in the future. Try different pressures at different nights.
I am now going to take a walk in the sun. Exercise seems to help my sleep. But there are so many changes that I can't tell.
The bedroom is dark. The temperature is low with window open a little. My wife does charge cell phone and hearing aids in the room. Is it because I shaved? What I ate? When I went to bed? So much variation that I know something is not working.
Yes leakage has been a problem, probably for over 3 years. The doctor stopped commenting on it so I have not focused on it. Now that I learned that leakage can set off the machine and/or wake me up, and your comment that various measurements are compromised with poor seal, this will be a priority.
You + OSCAR have already given me 5x, or 10x more information than the "doctors" in 13 years. They have a racket. I am on Medicare advantage with 80% coverage. I feel sorry for people paying retail price for this equipment.
I am a determined mouth breather. My solution has been to use two layers of tape. The first layer is 1" wide 3M Micropore tape which you can get at Walmart. I fold the end over to make a tab that I can quickly remove the tape in an emergency. I have never had to actually do it. At first that is all I used, but found it was coming loose at night and not sealing for the whole night. So then I added a wider second layer of tape 4" wide which I cut to about 60 mm long. It is called Molnlycke Mefix. It is more flexible and keeps the first layer on through the night. You probably have to go to a medical supply place for this or to Amazon, which is the last place I bought it at. Again I fold the edge over in case I have to remove it during the night. This works for me. You may get away with the Micropore tape only.
This said, I think your leaks are so large that I suspect your mask is become dislodged at night totally breaking the seal to the face. The first step may be adjustments to the headgear. Unfortunately too tight is not good either. It may take a different style of mask to get to a happy place. What mask are you using currently? I see it is set for full face.
There is nothing wrong with having the mode in AutoSet at least initially. However, when you nail down the best pressure it can be worthwhile to switch to fixed pressure CPAP mode. That is what I do. My wife still has her machine in AutoSet but with a very narrow band between min and max pressure. That is almost the same as fixed pressure mode. She averages less than 0.5 for AHI so I don't like to fool around an change it. Also if I change something and she has a bad night sleep then guess who gets blamed?
As for quirky things to blame or solve issues here are a few of mine. I blamed the weather, and more specifically the atmospheric pressure. After tracking it for a while I found that was a red herring. On the more successful side I have found that keeping the temperature cool at night seems to help. And the other thing is using a down alternative pillow that conforms to my head, and a satin pillow case cover. I believe it is slippery and helps to not drag the headgear out of place on my head. And I find the down alternative does not push back against my face and move the mask out of position. You mention shaving. I shave and wash every night before I go to bed as I think that makes the tape stick better and not come loose during the night!
After thinking about your OSCAR screenshot a little longer I realized that if you are using mouth taping, you must not be using a full face mask. The machine should be set to match the type of mask you are actually using. Setting the wrong type of mask can make the leakage rate less accurate. However if you have it set to full face and are using a nasal mask the error would be in under reporting your actual leakage rate. Each type of mask has a calculated vent flow which is subtracted from the total flow to give the leakage rate. The full face has the highest vent flow and the nasal pillow the least. So if you have it set for full face and are using a nasal pillow then air leakage will be under reported.
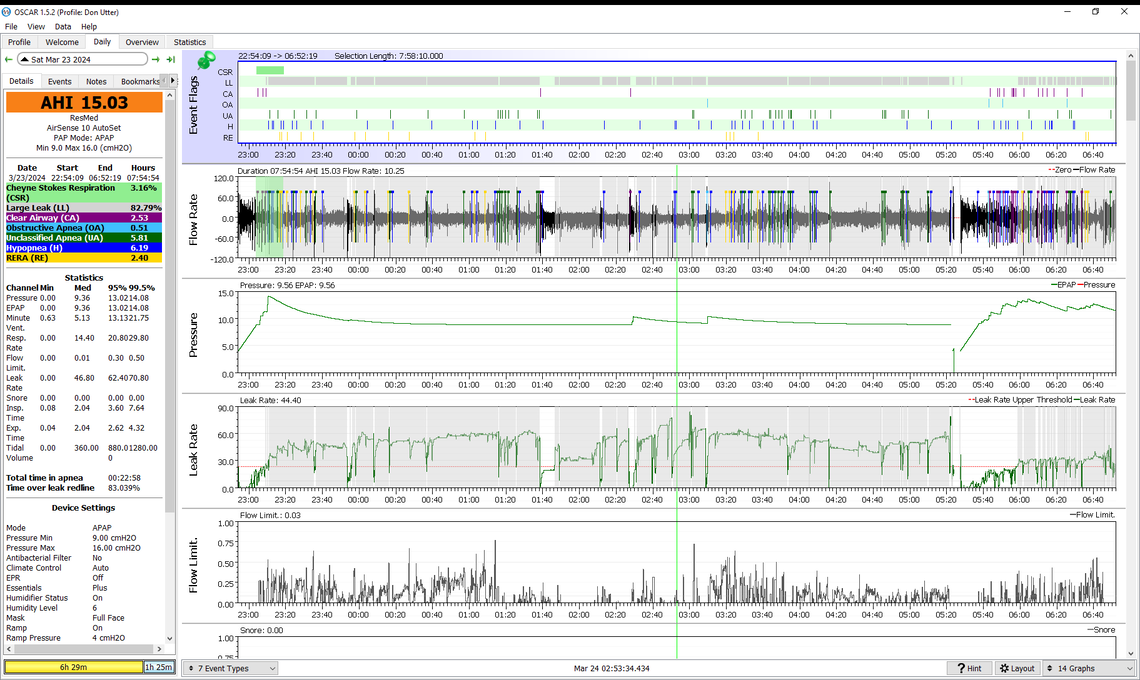
Amazing night last night! Thanks for the suggestions!
I taped mouth shut but by morning the tape was loose and allowed a small opening. I had never taped mouth shut before: always left a small opening.
I was using a reasonably hard foam pillow with indents thinking it was a CPAP pillow. I changed to a feather pillow.
Feel great this morning. Maybe didn't realize how much sleep has been lost with the CPAP attacking me because of leaks and mouth breathing.
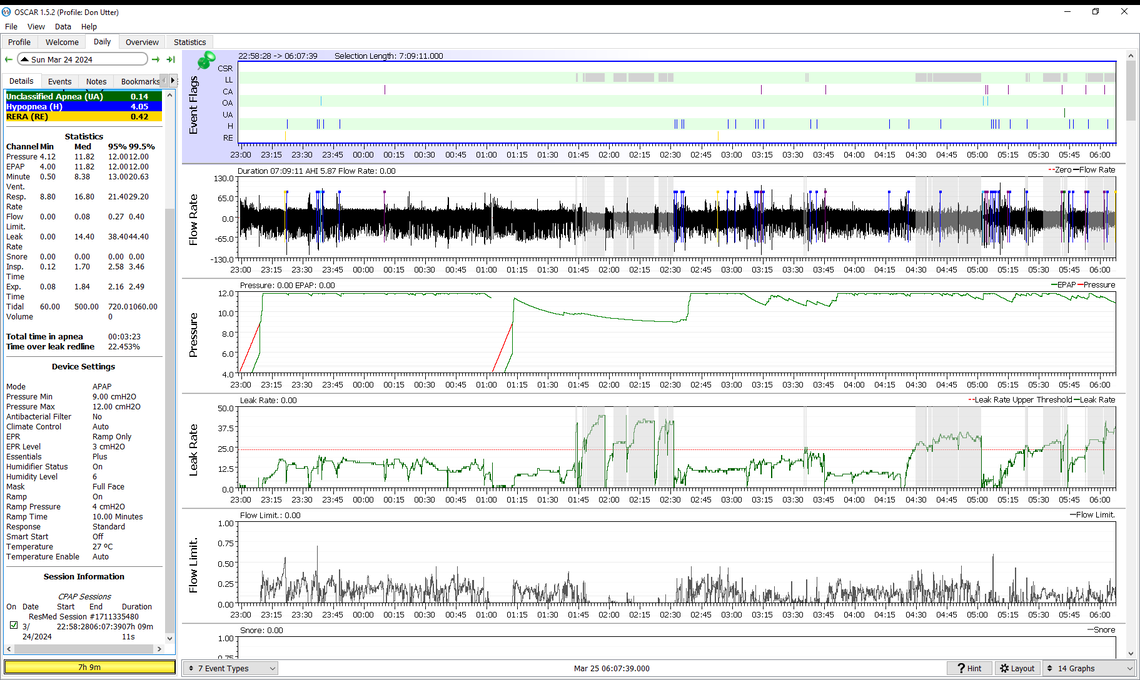
I realized that I had scrolled down on the daily report and posted the end. Here is a new image of the top scales. I also scrolled down on the information on the left to display the settings on the machine.
That looks better. On the mask the Full Face is the right setting. However, there is no leakage reduction benefit in taping your mouth while using a full face mask, because your mouth is already covered. Mouth taping is typically only used with a nasal or nasal pillow mask. I have heard from others that when you tape under a full face mask the tape gets soggy and does not stay on. Some also have expressed concern that the tape may be more difficult to get off in the case you need to get it off in a hurry...
Your EPR is on Ramp Only, and needs to be switched to Full Time. That may improve your Hypopnea and RERA event frequency. Lets see that that does to the flow limitations. They seem to be driving the need for more pressure. Perhaps with EPR on full time they will decrease and pressure will decrease too.
On the humidity control I just leave it in Auto, but my level seems to default to 4 not 6. But, with a long night's sleep I do use most of the water, but not all.
On the pillow a down or down alternative is a good choice. I try to sleep with my head resting on the pillow but with my mask hanging over the edge of the pillow. And the satin pillow case seems to help too.
Try the EPR on full time and see what happens to the pressure.
I changed EPR to Full Time. I changed the humidity level to 4. I will not use tape this evening or as long as I have a full face mask.
How long have I been causing problems for myself? Like taping with full face mask?
Given my past sleep, last night was outstanding. It sounds like it will get much better as I follow your suggestions.
I went back through several days and found days with apnea over 10 minutes. And found days with mask leak problems over 20 minutes. And even the second graph, the flow rate, is now heavier and concentrated more in the middle. As I looked at this and other graphs I saw that they changed dramatically day by day. That could be the reason for the grasping at straws trying to figure out what was going on.
Are there any particular graphs that I should follow?
Also, as I recall it was OSCAR, who warned about changing the memory card to locked because of potential problems that the computer would overwrite the data. I an using off the shelf WIN 11 and I don't think it will be a problem if I always leave the card unlocked.
Again, thanks so much! Don
I don't bother to lock the cards before downloading the data. Both my machine and my wife's are AirSense 10's and I don't think they have this issue. Her previous machine was a S9 and OSCAR claims that might be a problem.
I look at that Daily screen primarily to see when the apnea events are occurring, and at what pressure they are occurring at, and of course the types of apnea and how much each contributes. Next I look at the Overview page. This has a bar chart by day which breaks down the contribution of each type of event. You can quickly see from that what types of events are occurring and if they are increasing or decreasing in response to settings changes. Last I look at the Statistics page to get a little more detail on the breakdown of events. This page will give a running average of your AHI for each setting. A new line starts each time you change the settings. It keeps a useful history of what setting you have tried and what the AHI outcome was for each.
A couple of comfort and convenience things you could consider are:
Good luck! Post what you get with EPR at Full Time. That may make a significant change, hopefully for the better.
changed settings: ramp time to AUTO. Ramp start to 7. Start smart ON
Looked up the definitions of: CSR CA OA UA H and RE
Amazing! Shape of wave. Physiology of lungs and throat and other parts of the body's tube, lungs, and brain signaling when to breathe.
Does the medical profession think we are dumb? Thanks to Resmed to record this data.
I will post tomorrow AM and then going off to Cincinnati with granddaughter to see Pompeii exhibit.
There is a lot happening in the area of reversing Alzheimer's disease. One of the early pioneers is Dale Bredesen whose book in 2017 is "The End of Alzheimer's: The first program to prevent and reverse cognitive decline." He has written two books since then. He works in 32 areas rather than a magic bullet of a drug to target something. Toxins, treatment of diabetes because Alzheimer so connected that some call it diabetes type III. Nutrition, exercise, life style change. At the bottom of his pyramid of treatment, the largest area, is sleep. This is why I have spent so much time trying figure it out and why I will be forever grateful to your help.
Starting today is "Discover 50+ Ways to Overcome Memory Loss and Cognitive Decline at the Reverse Alzheimer’s 3.0 Summit!" There are talks which are free each day. Then a new set of talks on remaining days. I went ahead and ordered the entire segment for $69 so I can watch it at my leisure.
https://drtalks.com/reverse-alzheimers-summit/
It is an exciting time for so many health approaches. Biggest problem is lifestyle change. Diet change. Many of these programs are similar because of emphasis on mitochondria.
Again thanks for the help. Now I can see why these folks place so much emphasis on sleep!
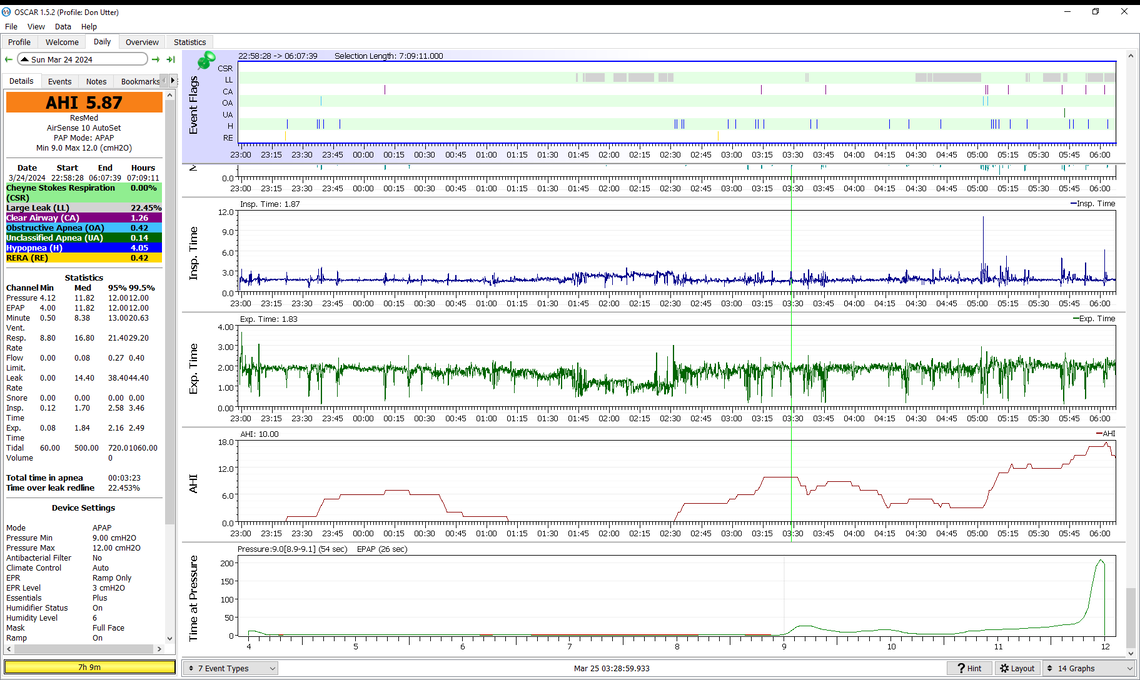
well, well, well
mixed results. Another step but not the linear improvement that I had hoped for
the mask felt better on my face. The whole experience was smoother.
Today, Tuesday 3/26 going to spend 4 hours in the car and time standing at a Pompeii exhibit in Cinn OH. Was that on my mind?
Anxiety? Blurry eyes? I woke up and misread the screen saying 8 hours elapsed but it was 5+ hours. I got up . Was up for a bit then went back to bed with CPAP and didn't get back to sleep. Got up, ate (I usually eat after 11 am, not 6:30, but, hey, the day starts early for the trip.) Went down to family room and slept for about an hour. Now I am writing this.
I don't know what to make of the night's data.
I am leaving in less than an hour so won't see your reply until early evening.
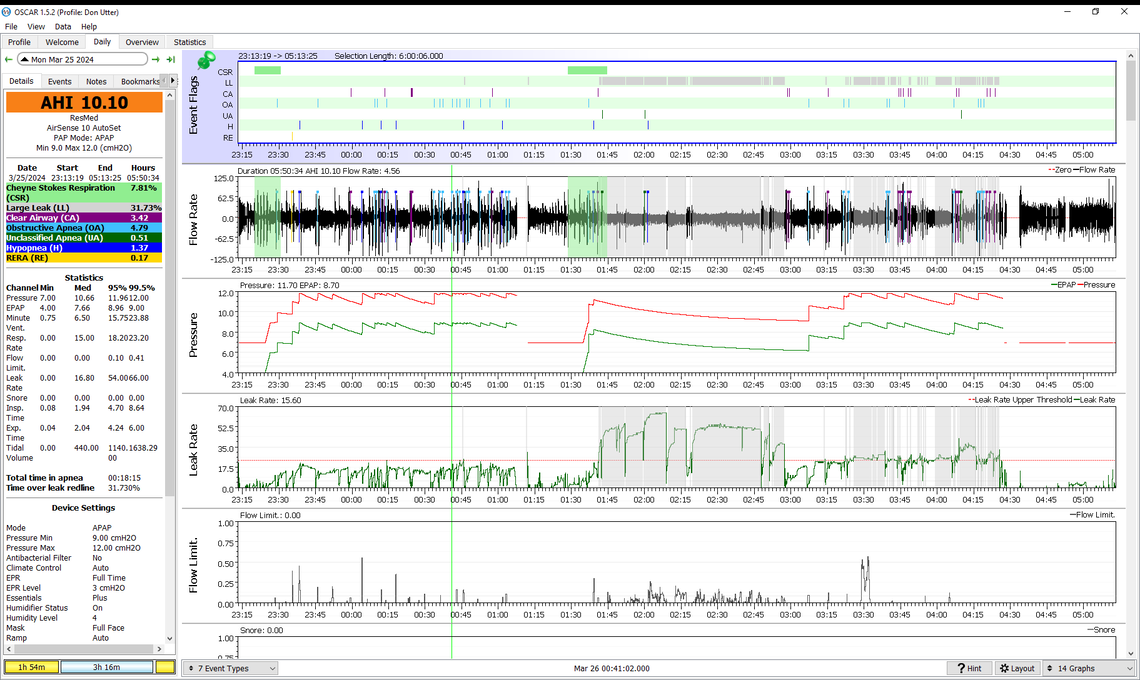
Yes, some good things, and some not so good. The auto ramp worked as it should. Hypopnea, RERA, and Flow Limitations are down, which is good. However, OA events are up, and especially when the pressure is at max. My suggestion now would be to increase the minimum pressure to 10 cm, and the max to 13 cm to see if that helps with the OA events.
And as you can see the first part of the sleep was not too bad for mask leaks, but the second part was not so good. Perhaps more tweaking to the adjustments of the mask.
When posting screenshots it helps to get a full width window so the screenshot is larger on the screen. Use the orange Write a Reply button at the bottom left to get the full window. I have had cataract surgery and am trying to be eyeglasses free! That last post forced me to dig out my readers... I'm 75, the pleasures of getting old...
I changed range to 10 min, 13 max
On the size of the screen shot. I appreciate how difficult it is to read because even on full screen with my 21" monitor it is not easy to see.
Since we have exchanged so many messages the width is getting smaller and smaller with each response. Even if I go full screen, these are built in size restrictions because we are so deep into responses.
On the image. I followed your instruction of F12 to get it to the Picture folder. But to drag it over here, I had to make the screen smaller because even with one image in Picture, it took up 3" of the screen. If I made this page full screen, the dragging failed. Someone gave me a hint to make this screen smaller so I could see the image and this screen and drag it over.
Since the image size is small, and there are many nested layers bounding the image to a smaller and smaller area, maybe a different way to send you an image would be useful.
Here are two things I just did
I dragged the image into gmail and sent it to myself
I attached the image in gmail and sent it to myself
With both of these one can bring up the image and manipulate it on your computer. That would address the small size.
I would need your email to do this.
And it is good to keep a record of our conversation here. I once started another conversation and I couldn't find it. I worry that I could loose contact with you through some mistake.
I could both post the image in My Apnea for a record, and send it to you by email.
In short on the image size: it might be best to put it in two places. I could drag it here so it would be part of the record. And I could send you the jpeg file (think that is the format) and you could use image/picture tools to resize, zoom, and do various other things.