I could not find a pre-warm option on my machine. You probably live in a colder climate.
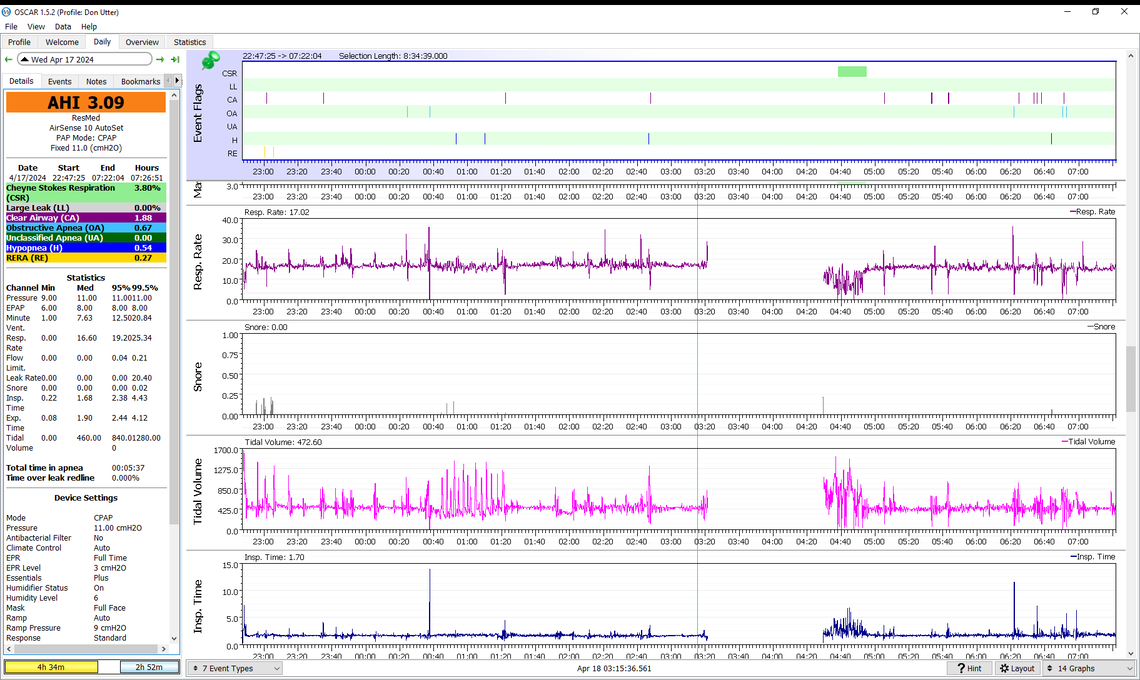
I took a try at zoom in. Did I get close?
Off to bed.
Just press the round button to "wake up" the machine. The top "My Options" window should be highlighted. Press the round button again to select it. The "Run Warmup" option will not be initially displayed but if you rotate the round button it will go further down. When it is highlighted, press the round button again to select it. And then once more to make it run. It will do the rest from there.
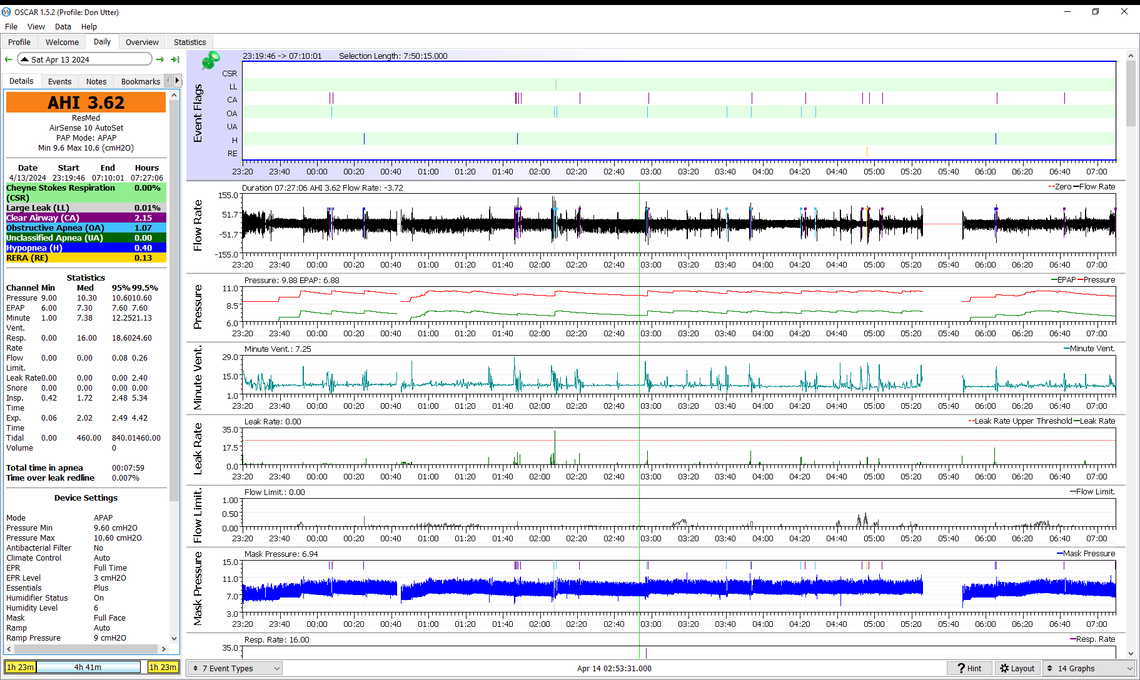
Is this what you are looking for? Interesting to see the flow rate and the mask pressure to become very regular just before 06:59
Didn't find water pre heat on my machine
Off to bed
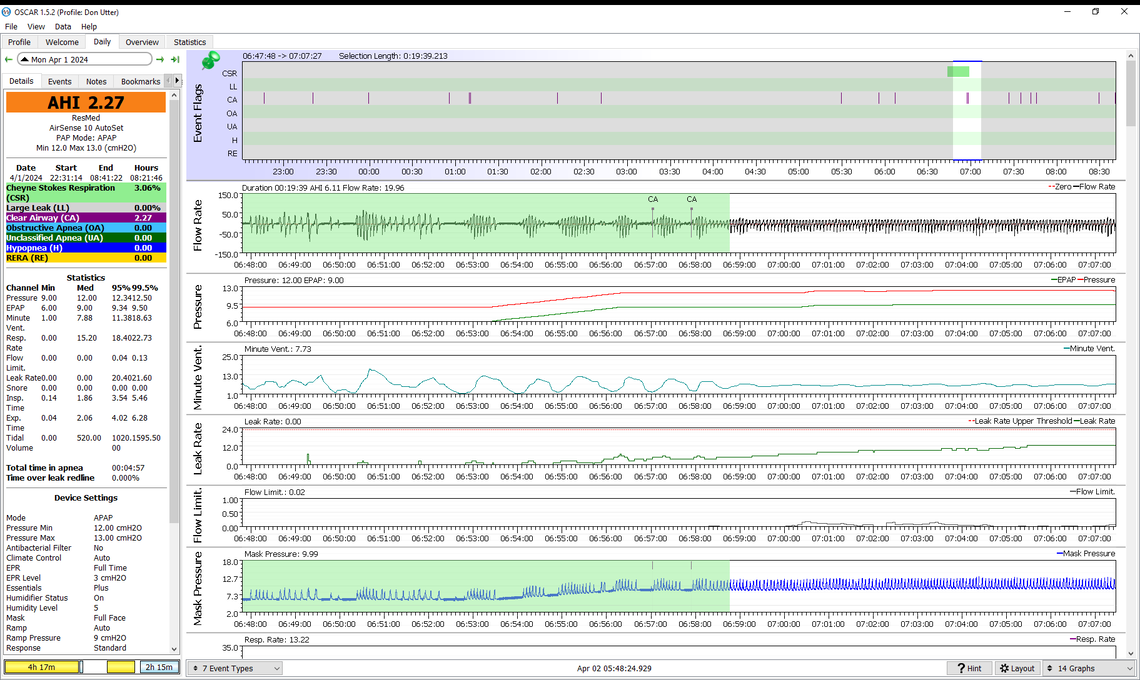
Yes, that is it. This is just when you are going to sleep. It appears as the pressure increases the cyclic breathing starts, and at the end is classic CSR with a CA event between the two waxing and waning events. If this is still happening by the time you get to see the sleep doctor, I would bring a printout of one of these events, along with your running summary of how much CSR you are experiencing. Along with that you need to bring your SD card and request that they look at the detail. The issue will be whether or not they will actually take the time to do that.
At some point if you cannot control AHI to less than 5 you may also want to consult with a heart specialist and show them examples of the CSR details.
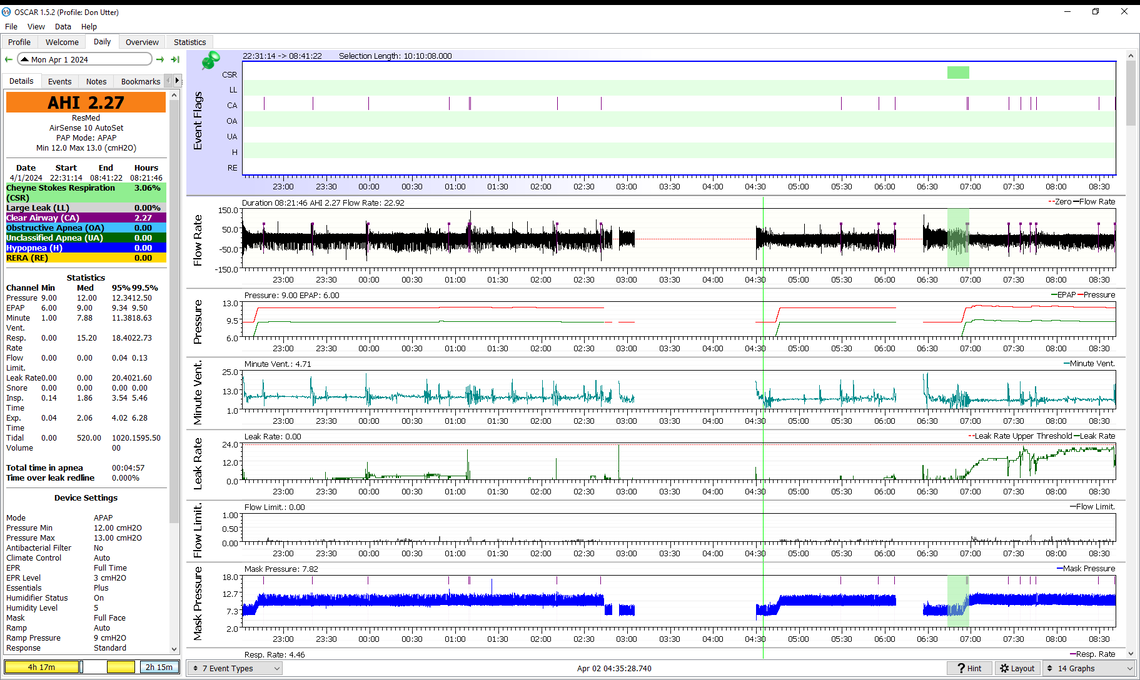
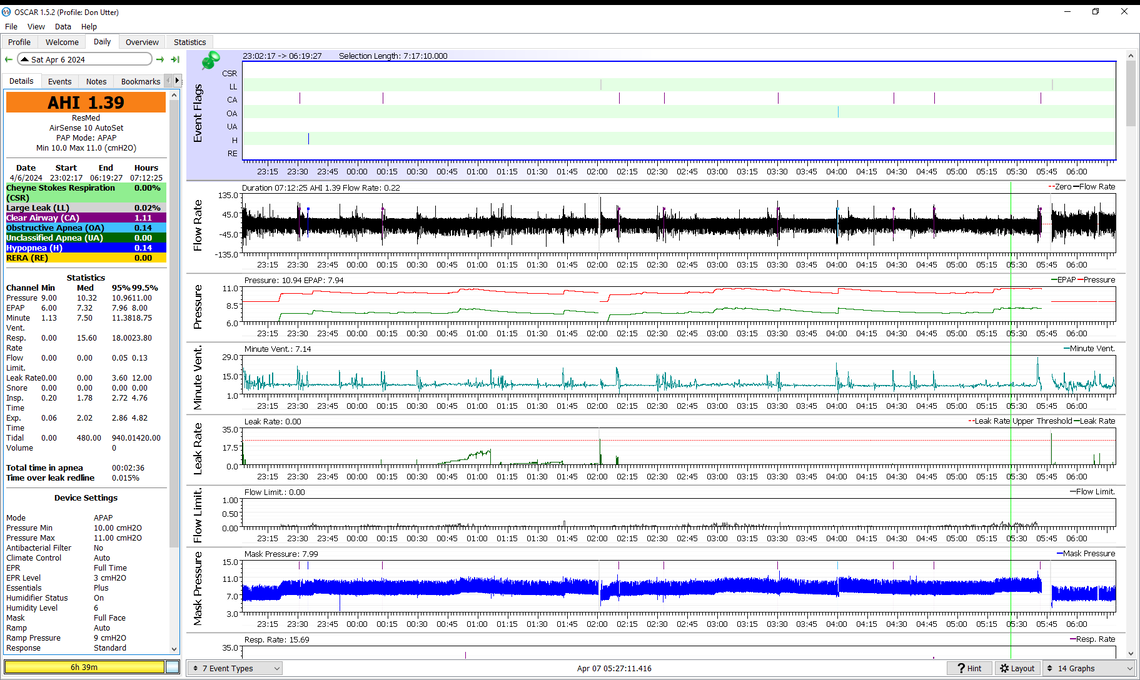
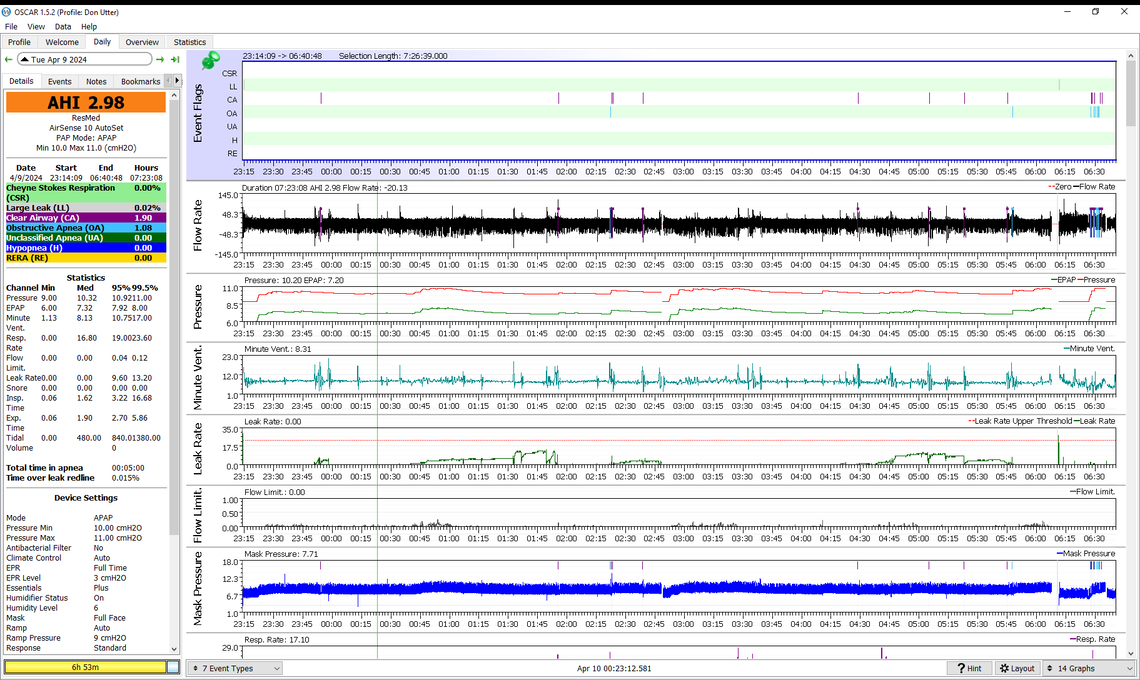
Incredible! Another night less than AHI of 2!
I slept for 7 hours before getting up to pee. Sorta went back to sleep.
Since you work with Zooms, here is the one that looked interesting to me.
A couple of interesting articles came up today.
"If You Want to Feel Young And Rejuvenated, One Habit Is Key HEALTH 03 April 2024 ByCARLY CASSELLA" The habit is sleep! Makes you feel 5 years younger! I can't thank you enough for the help! https://www.sciencealert.com/if-you-want-to-feel-young-and-rejuvenated-one-habit-is-key
The second article is by Joseph Mercola. He wrote the book on Keto diet that was the largest seller in the country. He may have excluded bibles which have topped the list for decades. He is issuing a warning about the problem with excess avoidance of carbs. In my Health quest, one area that is so full of contradictions that I have yet to sort out is diet. This article argues for a more expansive diet. It is interesting to see Dale Bredesen now recommending a Mediterranean diet rather than a struct keto diet and measurement of keto in his books.
"Consequences of Low-Carb Diets" by a guest writer https://articles.mercola.com/sites/articles/archive/2024/04/02/consequences-of-low-carb-diets.aspx?
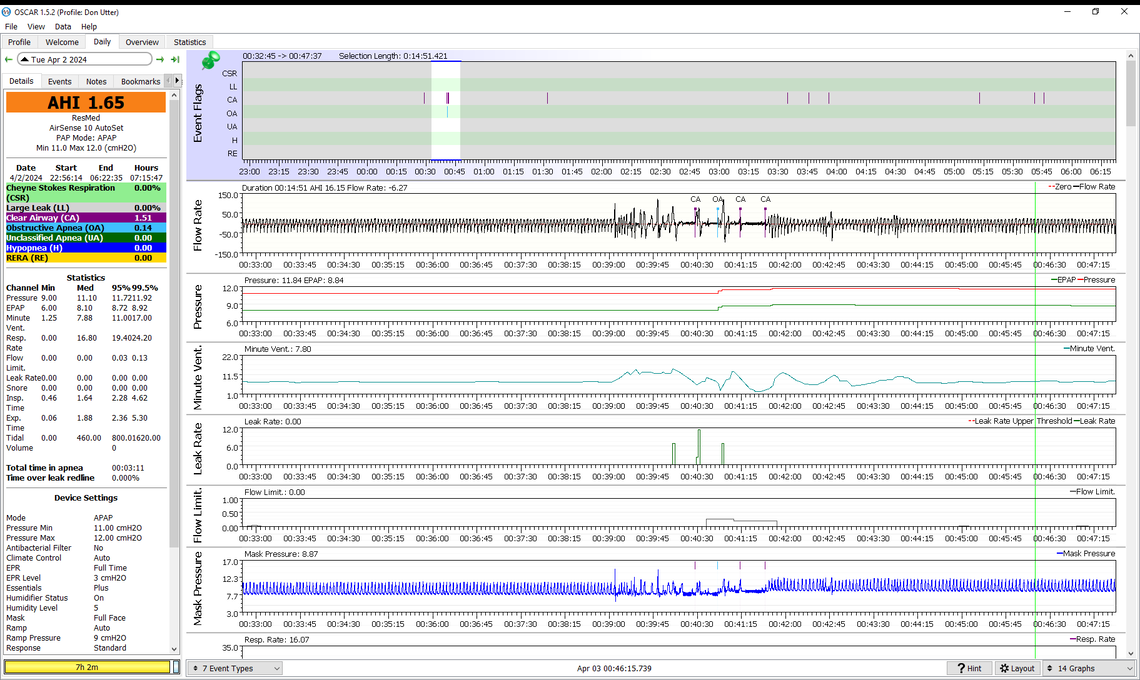
That is looking pretty good. I now see one OA event which you have zoomed in on. I suspect you may have woken up during that zoomed in portion and the three CA and one OA vent is probably what some call "Sleep Wake Junk). I think you are reaching the optimum point for pressure. However, to confirm you should probably try just lowering the minimum pressure from 11 down to 10 to see if OA becomes a bigger issue, and if lower pressure may reduce CA events.
I have been a type 2 diabetic for nearly 25 years now. I currently treat it with metformin and two types of insulin. I also wear a FreeStyle Libre 2 sensor to constantly track my BG levels. This helps me a lot in controlling BG. For a while I tried the 20/30 Far & Fiber Plan by Gabe Mirkin. I think it is a very healthy diet, but it makes it harder to control BG for diabetics. However, I still try to minimize foods that have high glycemic index carbs.
Sorry to hear about your diabetes. I faithfully followed flccc.net Front Line Critical Care Coiid associates since the start. I went to their convention Feb 1 to 4 in Phoenix a couple of months ago.
I started hearing about intermittent fasting and had been starting it for a few months, then in Sept 2022 Paul Marik, in their weekly update, said that he had cured his 25 year Type II diabetes. This was a turning point for me. I did not think that this condition could be reversed. Marik is an ER physician, the second most published ER physician in history and on a scale of publishing record he is over 100 and Nobel Prize winners are in the 30-40 range. I trust him and the work flccc.net does.
I was pre diabetic and along with beta blocker for blood pressure and a couple of other meds, I am now off them which I probably said before in these exchanges.
Here are 3 free documents from flccc.net
https://covid19criticalcare.com/tools-and-guides/what-is-metabolic-syndrome/
this is the one that turned me around to be responsible for my health
https://covid19criticalcare.com/poison-inc-processed-food-and-prescription-drugs/
The second doctor is kinda difficult to understand. He is called the Covid Hunter -- he was in the ER for 400, 500, or some number of days straight!!
Found this "A Houston doctor worked 715 days without a break once COVID was declared a pandemic MARCH 10, 20237:17 AM ET"
The next is on metabolic syndrome
https://covid19criticalcare.com/metabolic-syndrome-defined-and-how-to-treat-it/
That is a start. It takes a life style change. Maybe done best under doctor's care. I can find more links if you like.
That stuff is all in my "been there, done that" bucket. I was diagnosed with very high BG levels, and quickly got it under control and in the process lost something like 70 lbs. It did not cure my diabetes or even come close to that. Unfortunately the weight has slowly come back. But, my BG is best control it has ever been in.
DonMidwest: it’s very important to tell your physicians or surgeons that you have sleep apnea. They will monitor you very carefully, make sure an anesthesiologist is attending you at all times, and possibly use different anesthesia medications, if they know you have SA.
Thanks for the advice. I am trying to avoid anesthesiology as much as possible. But like the accident on April 1 (no joke!) things can change in an instant.
From my prostate surgery and urine leakage I have a urinary sphincter. There is a cuff around my urethra which is activated by a balloon in my scrotum. Squeeze the balloon, the cuff opens when finished, it automatically closes. I am supposed to carry a document describing how to press a button and open up the cuff before putting in a catheter. If they just shove it in it will mess things up and then it will be a big repair job to get things flowing again.
I sympathize. This aging gig is not for the faint of heart. It you aren’t already doing it, I suggest a medic alert bracelet, to give medical personal a heads up as to both the SA and any other problems you might need them to know about if you were unable to communicate on your own behalf. Another idea: keep a copy of your medical records etc., near the front door in case the EMTs come to your home.
Good suggestion. I will look into what this entails.
I mentioned I attended the flccc.net medical conference Feb 1 to 4. One of the speakers, Dr. Robert Lufkin, full prof at USC and UCLA, has a book out in June "Lies I Told My Students in Med School." I was looking through some Dr. Talks series videos and I saw him so I went to his web page and watched the first few minutes of the following video. He points out that there are 5 conditions that are the most likely to end our lives and they are handled medically as independent conditions with a treatment for each one. He was diagnosed with 4 chronic conditions that his dad died of and he had young children so he had to find out what was going on.
He found that all 5 have a common basis in metabolism. So all can be treated at once.
"How to Optimize Your Health Using Nutrition" Interview Feb 2024 https://www.robertlufkinmd.com/how-to-optimize-your-health-using-nutrition-nutrition-and-health/
That reminds me of what I think was an extremely rare and close to fatal complication of diabetes. I use insulin and have gotten into the habit of holding the very small plastic cap that goes over the insulin needle in my teeth while I set the correct amount and administer the insulin. I've done it thousands of times. On this occasion I had the unfortunate luck to have an uncontrolled sneeze. I gasped and inhaled this little plastic cap. I went to the hospital emerg and got some X-rays. They of course did not detect anything and they did their best to convince me that I had swallowed it and it would pass. I knew that was wrong and could feel the restriction and noise this cap was causing in my lungs. My doc prescribed more X-rays and of course found nothing. You can't see a tiny plastic item with an X-ray.
The reader's digest version is that I saw an ENT who did the endoscope thing in my nose and found nothing. Then I saw two pulmonologists and both prescribed pulmonary function tests (all during COVID). Finally one got me in for a bronchoscopy at our university hospital. They used fentanyl and other stuff and that went well. They had success in finding and taking a picture of the cap in my lungs, but could not get it out. Then I was referred to the hospital that specializes in pulmonary issues. They used a full general sedation and got the cap out. However, there was an issue. They used a drug to immobilize my muscles to allow the tools to go down into my lungs. It was supposed to act for a few seconds. But, it turns out I have a genetic issue called a Pseudocholinesterase deficiency which made the succinylcholine drug they used act for hours instead of seconds. Essentially I was unable to breathe for about 2.5 hours. They got me through it, which was somewhat amazing as this was at the height of COVID and my daughter, who works at the hospital, told me that they were down to 1 or 2 ventilators.
I am not sure what I cost our healthcare system with my dumb mistake, but I'm sure it was many thousands of dollars, and it near cost me my life. It sure makes me think twice about agreeing to a general. I had my last cataract surgery with just a Ativan tablet under my tongue and the numbing drops.
So I do have a medic alert bracelet that warns I am a Type 2 on insulin, and also about the Pseudocholinesterase deficiency. However, it does not mention sleep apnea. I don't consider that a life and death critical condition. The effect of sleep apnea is long term, and not an immediate critical condition.
I think we are now officially way off topic!
So sorry to hear about your deficiency. I had never heard of it and it is a life threatening condition.
I now understand why you have spent so much time on CPAP and OSCAR so that you can diagnose and recommend changes. With other things going on I have not spent as much time to much better figure out the condition and the readings from the graphs -- enough so in the future I can be able to adjust as needed.
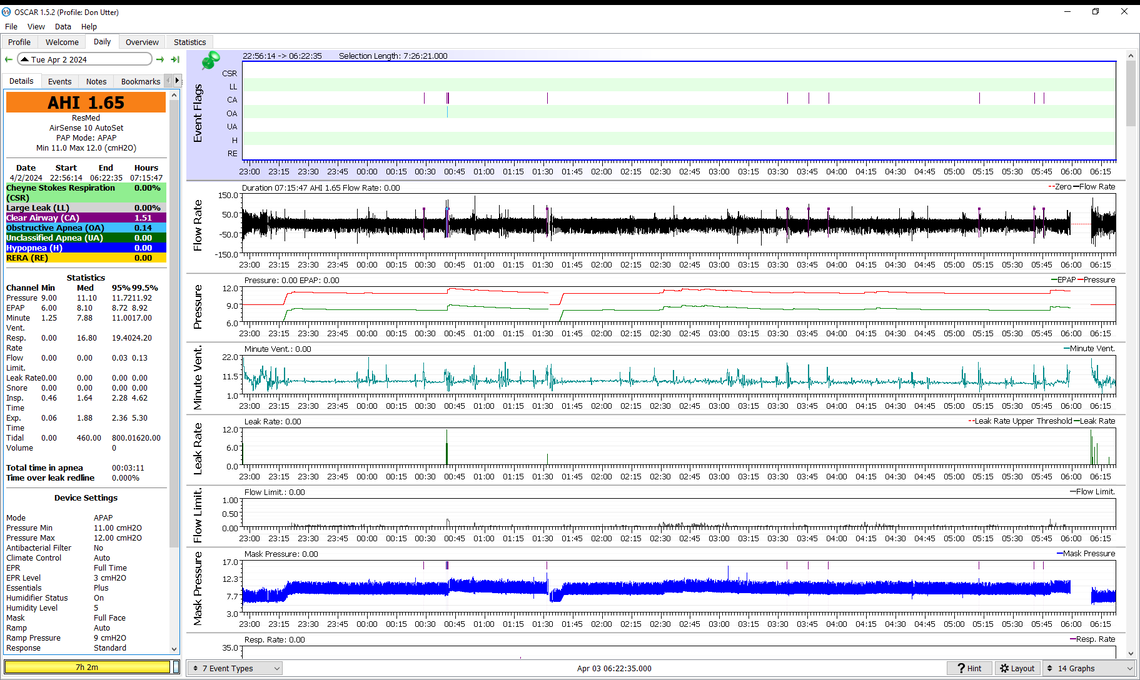
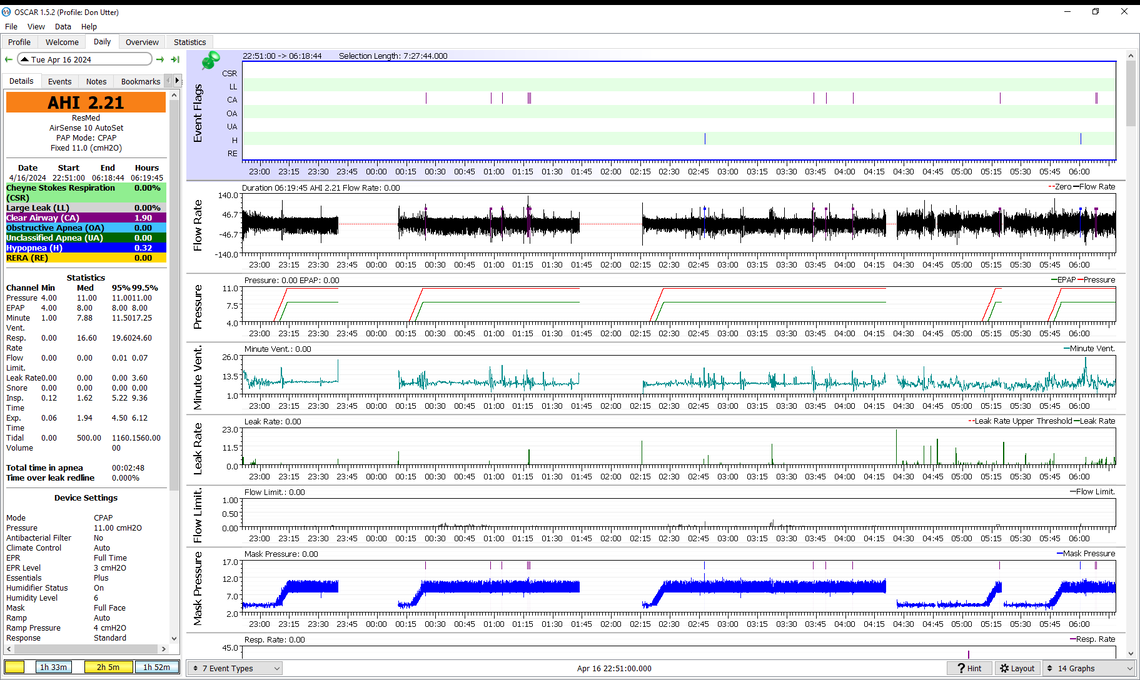
I slept straight through for about 6 and one half hours. Then a break. I think the apnea score went down from over 2 to slightly under 2.
What do the graphs tell you today?
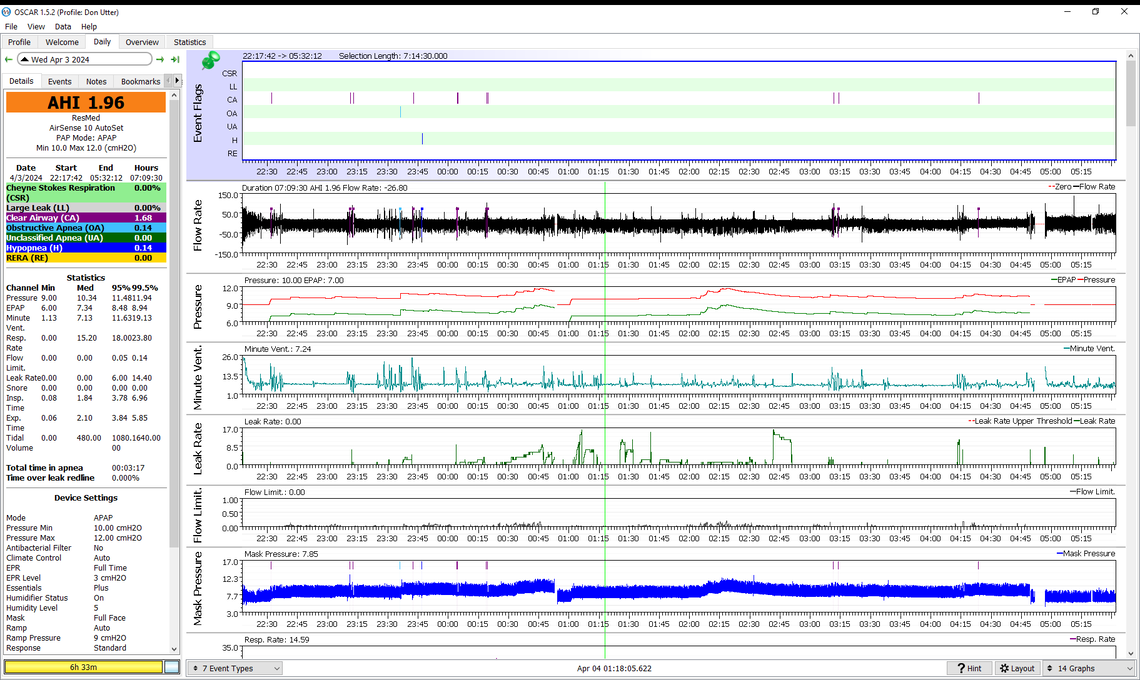
That still looks pretty good with only one OA event that looks like it happened at 10 cm pressure. Still no indication that CA events are coming down with the decreased pressure. I think the next step would be to decrease both min and max pressures by 1 cm to 9 cm and 11 cm to see what happens. Lower pressure should helps with leaks too. I see this night was excellent for leaks.
I see your Ramp start pressure is at 9 cm and you should be able to keep it there. However, if pressure is lowered more, it may have to be reduced, as I think the Ramp start has to be equal or lower than the minimum pressure.
When I first started with CPAP 13 years ago, I used the simple nasal mask. Pressure was at 10 all the time and I didn't use a ramp.
I now have to put on the mask, then the neck collar. Then I hook up the hose and it starts immediately I have been using the STOP button the top when I take a break.
From what I read, the CPAP masks seem to drive a lot of people nuts. Even with the collar, it is well worth it for me to get a good night's sleep. Actually, I am used to it and miss it when I don't have it.
I still have to work on going back to sleep after going to the bathroom. My current view is that if I make it to 6 and a half hours of good sleep then it is not so necessary to get more. Many places are saying 7, 8 or 9 hours. What are your thoughts on the length of sleeping?
Will make the adjustments now.
I find that the shorter I sleep the lower my AHI score. When I get apneas they seem to get concentrated to the last part of my sleep, especially if I try to oversleep. I consider 7 to 7.5 hours per night, ideally in one stretch, to be the best for me. What I have read is that we need to build up sleep demand during the day, and get one good sleep at night. Naps during the day should be avoided, but I confess to dozing off in front of the TV from time to time. But, I never lie down on a bed during the day. I also avoid all caffeinated beverages after 10:00 AM. I also try to avoid all liquids after about 8:00 PM to reduce the need to get up during the night. That works most nights but not all...
I have not had a nap the last few days since my sleep has been so much better.
I will discipline myself to not drink water after 8PM.
I drink one large cup of coffee 90 minutes after I get up. This was a suggestion to not waste the caffeine all at once and to spread it out.
After 13 years it is incredible to get such small apnea scores.
I will continue to wait a while before starting Gaba and/or Ashwagandha Root
Sierra: SA can be very a life threatening issue in the near term. Surgeons will usually ask you about your sleep status prior to any surgery, because if you have SA they will 1) use different meds and anesthesia; 2) monitor you with great care during and after surgery, probably keeping an anesthesiologist with you at all times for during surgery and perhaps keeping you in the ICU the first night; 3) they’ll make sure you have and use your machine anytime you sleep after surgery.
In an effort to lower post surgical death rates, some hospitals have even initiated pre operative SA testing for non emergency surgeries. I was terrified of going through a knee replacement, but they were able to use a nerve block rather than general, but still took all of the above precautions.
In the last three years or so, I have had two bronchoscopies, and 2 cataract surgeries. None of the anesthesiologists asked about sleep apnea.
Millions of people have sleep apnea and 8 of 10 are undiagnosed.
https://www.cbc.ca/radio/whitecoat/sleep-apnea-canada-challenges-diagnosis-cpap-machine-1.7108832
I never considered this. Since diagnosis with sleep apnea I had a surgery to replace a unitary sphincter, two colonoscopy's and cataracts. Since I probably had sleep apnea before it was diagnosed, I had a surgical removal of the prostate. The issue of sleep apnea never came up. And, the sleep doctors will hand out Provigil like it is candy. Rather than deal with sleep, they provide drugs to keep you awake. Have not taken it for a few years now but could get this narcotic at the drop of the hat.
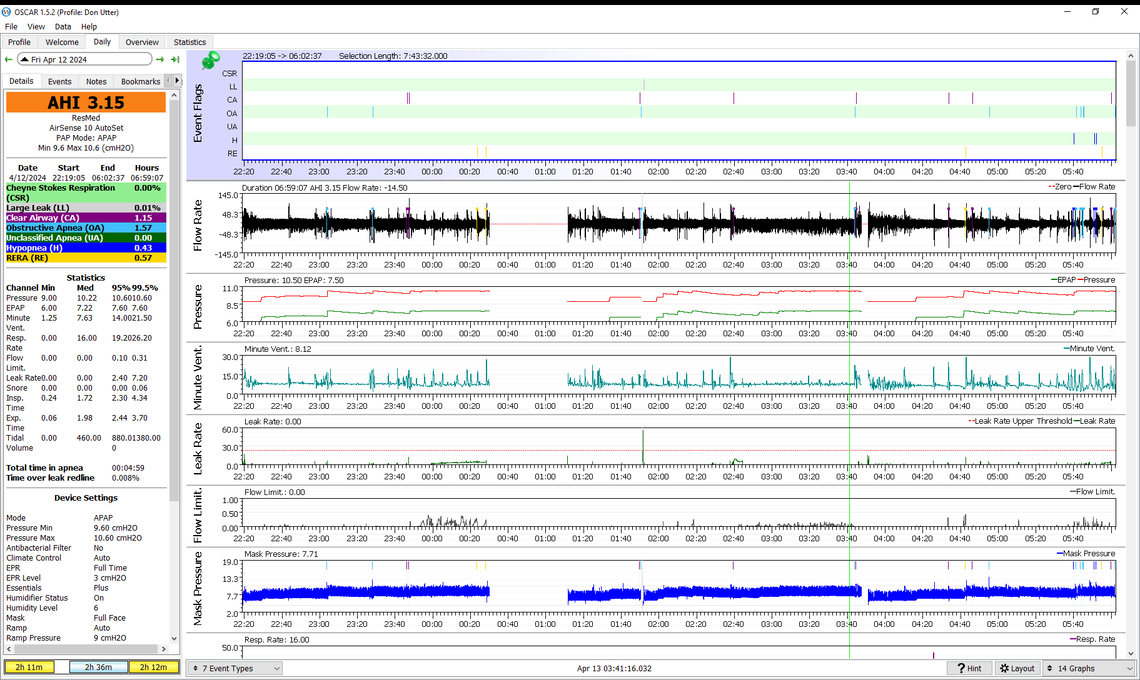
Another good night. I went to bathroom but didn't put mask back on so a blank period.
Watching some videos on how to read the graphs and the definitions of the terms CSR, OA, H, etc has been very helpful. Then a long video on Central Sleep Apnea by an MD. I bought an excellent medical reference book "Elements of Pathophysiology" which is a book for nurses. I am going to read the pages on breathing and ventilation. The book is available from Thrift Books for a few dollars and they pay for shipping. I bought it used a couple of years ago at the early stages of Health Activism and paid about $70 for a used volume. An older volume would still be good. When I was going all out I bought "Handbook of Internal Medicine" which comes in at 2,000 pages. Only looked at it a little bit. Might do that now as well.
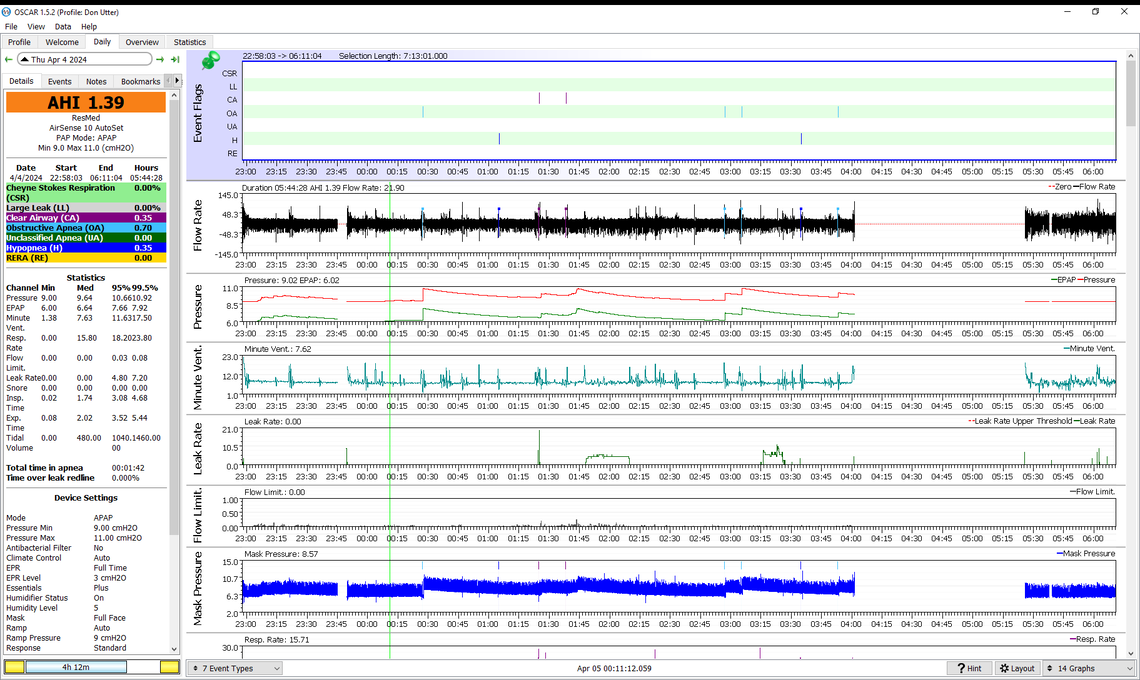
All considered that is a very good result with the lowest amount of central apnea that I recall seeing in your results. Your OA events are actually higher than the CA ones, so we have reached the point where it does not make sense to try going lower. My thoughts are there are two different ways you could go at this point. One would be to leave the maximum pressure at 11 cm, and increase the minimum pressure from 9 cm to 10 cm. The hope would be that CA events do not increase but OA events go down just a bit more. This is probably the fastest way to get to a final stable setting. It may be just fine to leave the machine in AutoSet and let it adjust pressure in this fairly narrow range.
The other way to go would be to switch to CPAP mode on your machine and go with a fixed pressure. One of the methods used by some sleep clinics to avoid the cost of a full in clinic sleep test where they titrate the pressures is to put the machine in AutoSet for some time and then go to a fixed pressure equal to the 95% pressure point indicated in Auto. In your case for this night this 95% pressure was 10.6 cm. You would run that way for a week or more to see what you get for a longer term average. Then you would try a pressure on each side of that pressure for a week at each pressure. This is fairly time consuming, but that is the way I went to settle on my fixed pressure of 11 cm.
Your choice as to which way you want to go. You of course could try both ways to see which works better. We do have to sleep every night, so there is nothing but time for testing. You seem to have reached a very stable condition which is much better than where you were when you first started posting.... The soft collar seems to have been the silver bullet in your case.
I am going to try min 10 cm and max 11 cm for a while to see how it works.
After a while I will try Gaba and some other things but I don't think that sleep can get any better.
You suggested humidity at 4. Now that I am not leaking there is very little water used. Cranked it up to 5 and still half full. Tonight I will turn it up to 6.
I was able to see in the data that I had apneas during the ramp so I understand why you start me at 9 with no ramp
With 10 min and 11 max a ramp start pressure at 9 should be fine with the ramp in Auto for time. That is what I use and find it quite comfortable. One of the tests I do to set the ramp start pressure is to take quick deep breaths when it is in ramp to see if the flow responds quickly and you get no feeling of air flow restriction. For me 9 cm is what it took. I am amazed that some sleep clinics send their patients home with the machine having the out of the box settings; 4 cm min, and 20 max. Trying to go to sleep with only 4 cm pressure would make me feel like I was suffocating.
I suspect you must be in an environment where the humidity is higher. The device on my desk says the humidity is 33% here. With a 7.5 hour sleep I use nearly all the water with Climate Control in Auto and humidity set at 4.
Victory! AHI 0,87 At the bottom of the left hand column, in yellow, is 6 hr. 15m . I think that is the time I was asleep. I woke up about that time to go to the bathroom, returned to bed but didn't sleep.
I can't thank you enough.
How many people have you guided through the maze to CPAP success? Surely, I was not the first.
The other day I mentioned the importance of dealing with a common issue to many diseases, metabolism, and this morning an article arrived about one of the conditions that will be the cause of our death. I am sending this because the supplement, GABA, is mentioned and I am just starting to take it now that the CPAP data looks solid, and CPAP scores are excellent.
"Alzheimer's Is Now a Leading Cause of Death Analysis by Dr. Joseph Mercola April 06, 2024" https://articles.mercola.com/sites/articles/archive/2024/04/06/alzheimers-death-rate.aspx?
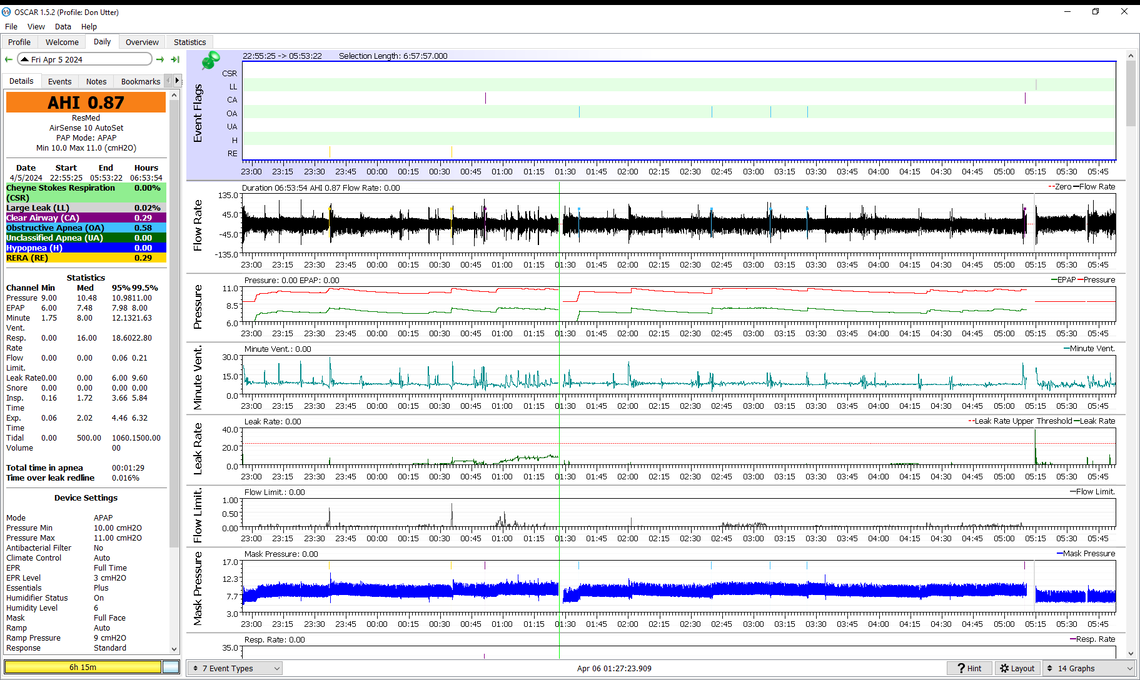
That is excellent. And the really good news is that your results seem consistent from night to night. 6:54 minutes would be your total time with the machine on. Just above the green CSA label on the left side of the screen. The bottom left if you scroll down further than what your screen shot is showing will list your "sessions" which are the individual times without breaks. It looks like you had three sessions. If a session is a wipe out there should be an on off switch beside each one where you can include it (green) or not (red).
I would suggest leaving your settings like this for a while. Feel free to keep posting and I will give you my comments.
I have lost track of how many people I have helped. I see I am at over 3,000 posts. Most turn out well, but not all do. Sometimes you just cannot get the CA events down to a reasonable number without OA events going too high. There is an ASV machine that sometimes has to be resorted to in the difficult cases. Good to see that along with the cervical collar you have gotten down to a good space with just the APAP.
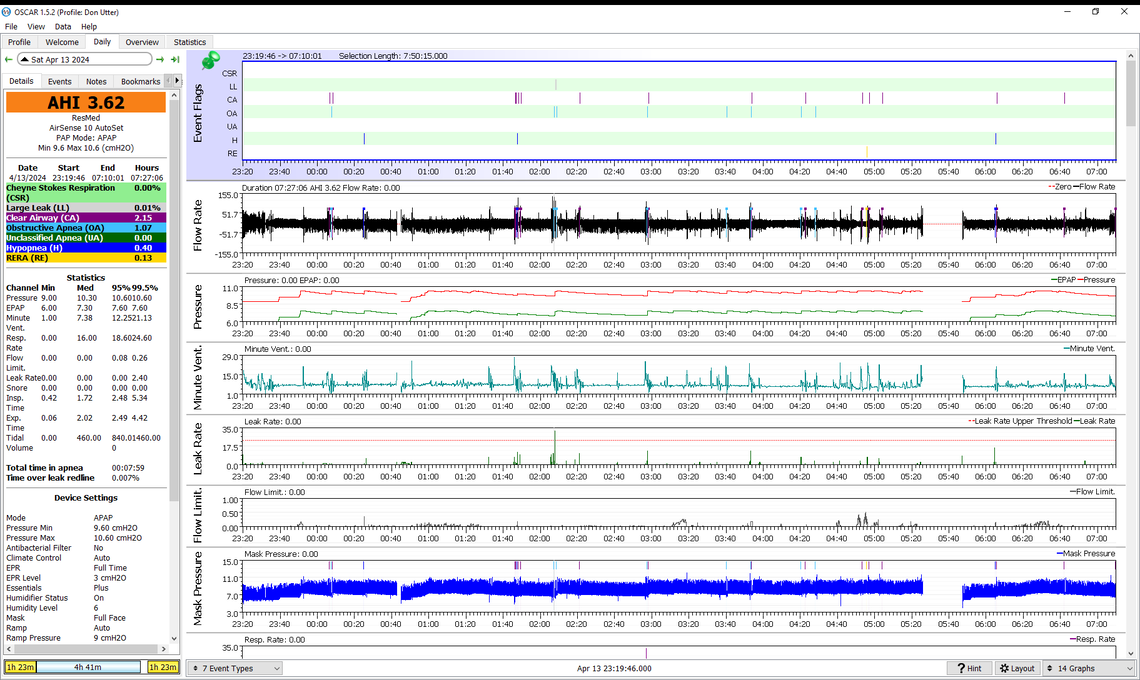
Another great night! Machine settings not changed.
Here are the other changes of note.
Our local opera company is putting on a totally new version of Mozart's "The Magic Flute." My wife has been an opera fan for years and in the beginning she had to drag me to concerts. To get ready for "The Magic Flute" in our local opera company in Columbus, OH, she checked out dvd of earlier versions and so far we have watched 2 in order for me to get a sense of the story.
Operas are often restaged moving from a time and a story when first performed to another time and place and sometimes story but original words sung. Actually what Operas do is to take one to a different time and place with the story, the drama and music and of course, singing. Sometimes operas underdo radical change, not only of time and place but rewriting the words of the songs requiring note by note fidelity to the original score. When they change the words or the language, they keep the music the same which means that the singing vocalizations is also congruent with the score, so they have to go through vowel by vowel and assure they remain the same.
This is related to the sleep report because I fell asleep watching the movie for between 30 and 40 minutes. That was shortly before I went to bed. I have not taken naps the last 5 days.
The other change last night was taking the supplement gaba before bedtime.
That looks very good. You also seem to have gotten your leaks under control too. I would watch for the ratio of CA events to OA events. This one is fairly high in favour of CA events. If that continues you may want to consider moving down the min and max a bit - like 0.4 cm each.
I got into high quality audio back in the 80's and have maintained my system over the years. I think I may have "The Magic Flute" on Deutsche Grammophon vinyl.
Well, excellent but could be better, I suspect. At the bottom of the left side material is a yellow area 5 hr 40 min and a blue area 2 hr 44 min.
When I did go the bathroom the AHI was around 1.6
Any insights looking at the graphs? Any suggestions about changes? I continued to take GABA but not sure if any influence.
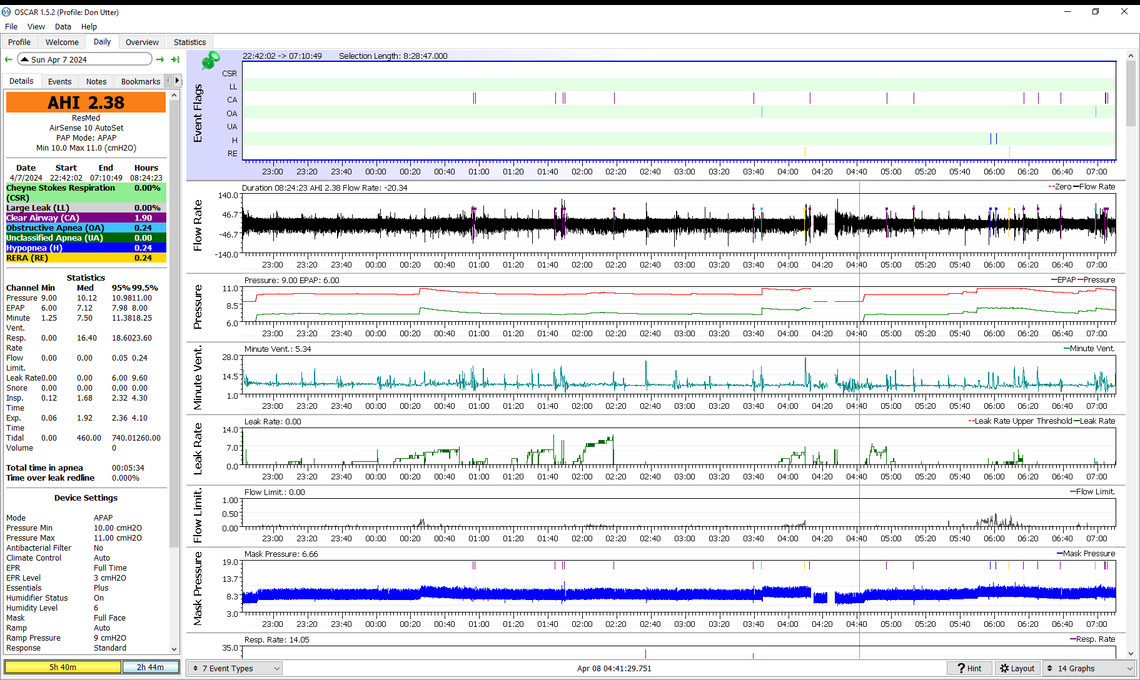
Still much better than where you started. The one thing I know for sure is that CA events are unpredictable. At what elevation above sea level do you live at? People at higher elevations and especially like very high ones like Denver can have a higher frequency of central apnea. We are at about 2,000 feet and I do notice a reduction in CA frequency when we vacation at sea level in Mexico.
The yellow and blue times in the bottom left are just the length of time for each "session" in the total sleep.
What I see is that around 0:25 flow limitations increased and the machine responded by increasing pressure. An OA event at 3:45 increased pressure again. At 5:50 or so, flow limitations caused pressure to bump up again. For the most part CA events are happing at the lower pressures. If the significantly higher frequencies of CA events continue you could try small steps down in both min and max pressures. On the Overview tab there is one graph of the Total Time in Apnea. If you keep an eye on that, minimizing this time is also a good thing to do.
Another great night! Some little things.
I have not washed the cushion for 13 days. How often should it be washed?
Heater set at 6 and I have 1/4 of water left in the morning
I looked at some statistics on average pressure
week 10.32 30 days 10.80 6 mo. 11.29 1 year 11.63
And as you well know, the 6 months and 1 year are not valid because mask seal was terrible.
The last 2 nights I have had terrible food. The standard American diet. Do things like diet influence sleep that quickly?
Only today am I going to begin exercise again. The accident threw me out of practice and I have just not done it.
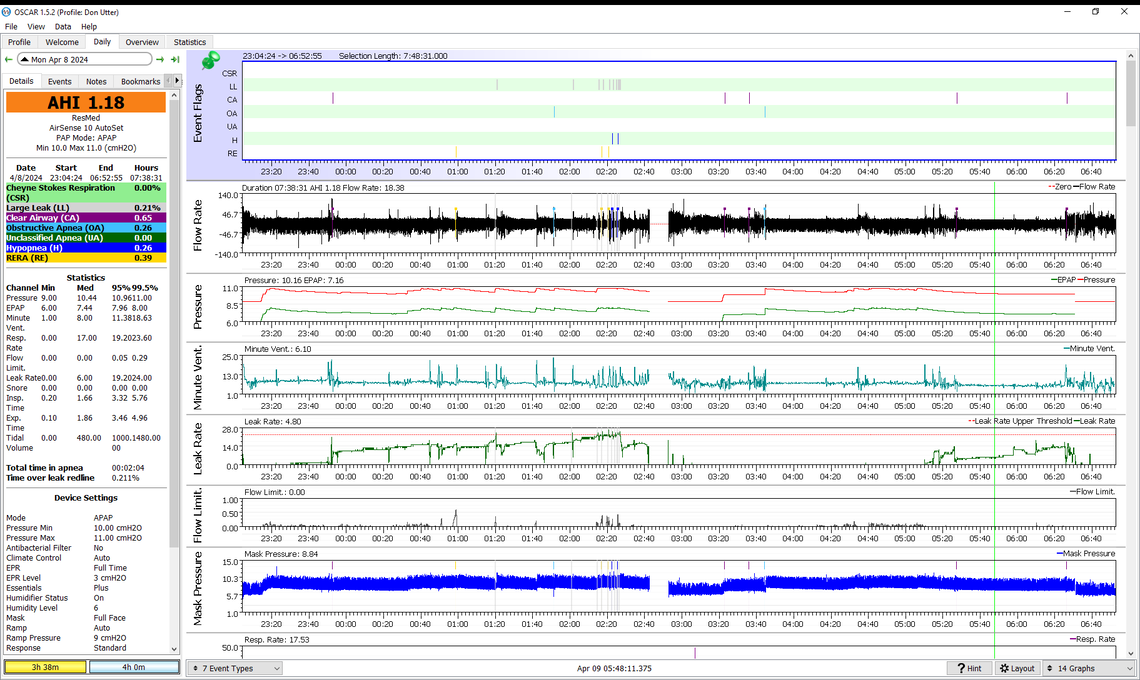
That still looks very good. I had a bad night, well actually a bad half night. Went until 4:00 AM with only one or two events, and then the last half of the night was a mess. AHI was 2.5, and CSR was nearly 10%. Our weather is warming up and it did not go below freezing last night. I think the room just got too hot for comfortable sleep. I think it is time to dump the comforter for the summer.
Exercise is good, but my recollection is that exercising in the morning is said to be better than later at night. Not sure about the impact of food. I do know from my Libre 2 data that food higher in fat and protein seems to impact BG much later. Ice cream at dinner has little impact until near bedtime. Pasta also seems to take a long time to digest. Not sure if that is good or bad. It does help to lower the impact on my BG though.
I suspect if you follow the "rules" the cushion should be washed every day. I think every one to two weeks is OK.
It looks like the bad stuff happened just before I got out of bed. I recall trying to sleep on my side I may have disturbed the mask.
Did a lot of running around today to get a back up camera installed. All Best Buy calls go to India and when I started I didn't know what I was doing so had to cancel order, more runaround from India, posted the credit card, sent an alert to credit card company because it is a change from India, got caught in the middle of IT - - so finally drove over to the store and it was necessary to talk to the technician because some special wiring required.
Confession: I have many times said that I was going to exercise. So far, I have failed to follow though. Today.
And also include the full evening. Without OSCAR I would have not have known the effect of my actions in the last few minutes because 2.98 in itself is a very good reading.
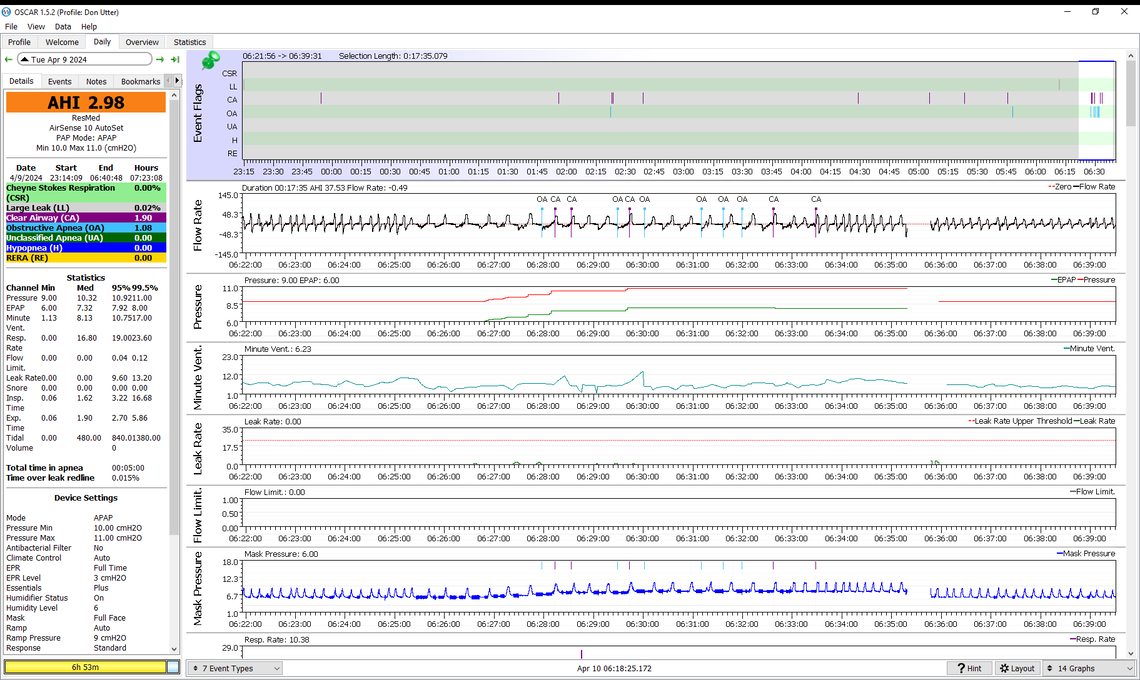
Unplanned experiment with a good outcome!
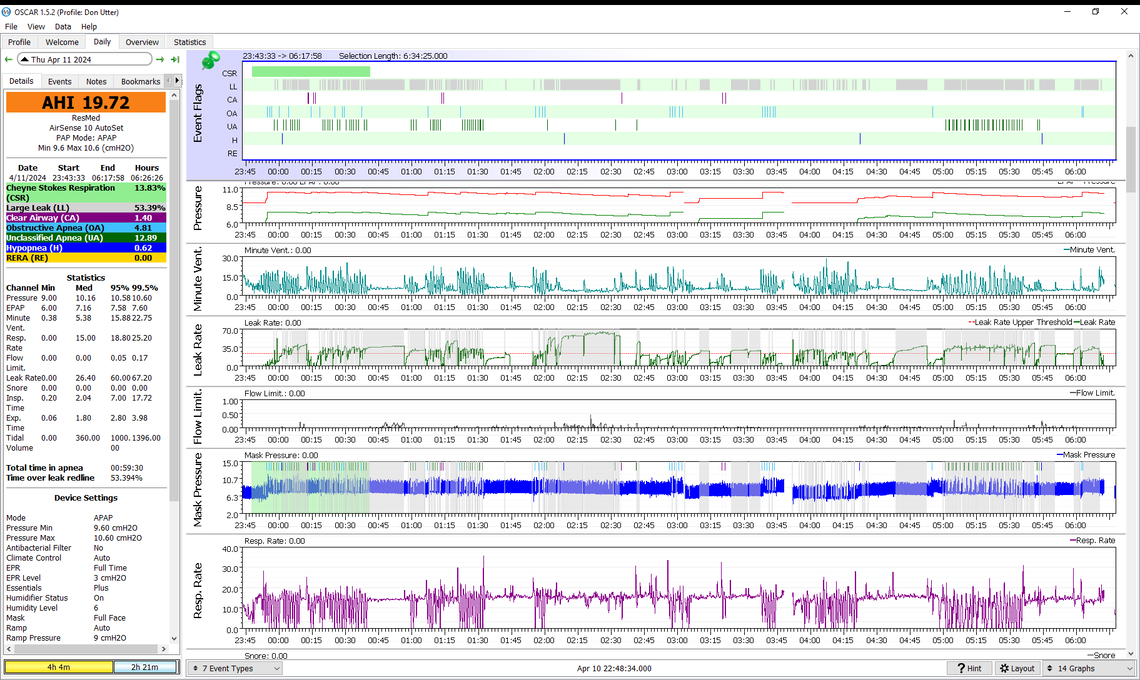
I forgot to put on the collar and guess what, I was awarded AHI of 19!!! When I went to the bathroom and saw 26 or so, I realized that I didn't have the collar on. I left it off for the rest of the night.
So with adjusted pressure settings, starting pressure, and all the other things you suggested, without the collar I failed. So important to lean this.
There are so many variables that a solid result like this is delicious. Wear collar from now on!!!
After 2 hours my AHI was 1.6. It looks like the machine was off for about 45 minutes. I must not have restarted it.
I didn't reseat either my cushion or my neck collar.
Would it be best to take both off when I go to the bathroom and put them on again?
I went to bathroom 3x, together with not reseating mask or neck collar and that may be the reason for the activity in the morning.
Yes, it looks like the machine was off from about 0:30 to 1:10. I used to leave my mask on when going to the bathroom by disconnecting it at the connection between the mask hose and the heated hose. Then this connection started to get loose and since I have just pushed the button on the top of the machine to stop it, and then removed the mask. It shouldn't matter if you take the collar off or not, as long as you put it back on again.
This is the first time OA and H have exceeded the CA event frequency. This suggests the minimum pressure point has been reached. I would suggest leaving the pressure the same for another night or two. Then if OA and H stay higher, it probably means going back to the 10 min and 11 max.
Thank you again for the ongoing assistance to uncover what is going on and the best response.
I would not have known to check OA and H exceeding CA event frequency. I will watch for it now.
Hot off the press! Get it early and it is only $299! Money back guarantee!!
"The Ultimate CPAP Mask Course April 2024 Limited Time Offer Learn from an experienced sleep expert on how to overcome your CPAP mask problems! Offer ends at midnight ET on April 18th!
Discover the secrets to mastering your CPAP therapy. This comprehensive program consists of:
12 pre-recorded videos a detailed workbook 4 LIVE online classes BONUS Course Included ($149 value): What You Need to Know About Sleep Apnea and CPAP "
I sent an email to Dr A Wells asking if she used OSCAR in her course. I am 99% sure she doesn't or she would mention it. Maybe a sleepydoctor cannot admit that they know about OSCAR.
I purchased her DrTalks "Sleep Deep Summit: New Approaches To Beating Sleep Apnea and Insomnia" and I have only watched a few of the 40 or so interviews. It was around $69.
I went to her web page and found another course: "21+ CPAP alternatives"
In case you want to check it out more, here is the link
https://www.supersleepmd.com/cpap-mask-course
** Once I know about OSCAR I can spot a fraud who focuses on the mask, and then goes into all kinds of behavioral advice like diet, cool room, no electronics in bedroom, etc. It is good to have the group sessions like AA meetings, but there is only one directly causal element, alcohol, and lifestyle changes can be life changing. And effects of alcohol or drugs on the person and their network is observable, but in contrast, a person does not know what is happening when they are asleep. The issue is the patient actually sleeping overnight with the graphs measuring what is going on. True, many of these other things can help and many are essential, but there is no way to know the causal relationship between the many variables.
Unfortunately getting the best mask is primarily a trial and error process. One can kind of narrow down what mask is likely to work the best, but the final test is actually using it. Places like Cpap.com have a return policy on masks, so you can try and return. Not sure if there is any catch to the process as I am in Canada and don't use them.
Well another night. Is it time to change the limits?
I don't know what happened at about 0:42. I thought I was asleep until about 05:25. I don't think that there was time to go to the bathroom. Or maybe there was time. Or maybe I was sleepwalking.
Would you like to see the details about 01:45?
I sent an email to Dr A Wells. She responded. I sent a long email with a copy of OSCAR graphic. I ended the email that now I can reliably get AHI of 2 and I don't think I could have achieved that with her course. She had heard about OSCAR but had not worked with it. I'll let you know if she responds. I mentioned lefty lanky 27 as a sleep technician on the web who works with patients using OSCAR. She is now in a bind. She has been exposed to a path that will help patients and it will change her practice. A cartoon I saw today was the new Hippocratic Oath: Don't do anything that risks your career.
Yes, you may have reached the limit of how low you can go with pressure. I would go another night or two to see if the same pattern is there before going back up in pressure. At 0:42 I suspect you moved the mask off your face and the machine stopped and restarted automatically. The pressure control went into auto ramp hold for a short period of time.
I have watched a couple of Lefty Lanky videos, and I really don't take him too seriously. I am not sure really suffers from apnea, but he makes out like he does.
Biggest score in a few days. Lots of CA and several OA. Suggestions?
I sent a MyChart message to my sleepy doctor to ask if the Mask Fitting had the new F40 masks. Have not heard back. The MD and sleep group are related and not related if you understand. A totally different company provides supplies. They don't carry F40 yet. Because of your help I could probably get by with my F30i, but the F40 looks better.
I heard back from Dr. A Wells. She thanked me for the information on OSCAR, she will look into OSCAR, glad that I am doing well, and she had heard about Lefty Lanky 27. My response was I was not particularly found of Lefty Lanky 27, but he is someone who works with OSCAR I found on the web. I suggested she look for someone else to work with. I wished her well on her CPAP Mask class that begins today. I did not sign up.
My thoughts are that the lower pressure is not helping the frequency of the CA events, but OA events have increased. Perhaps it is time to abandon trying to get the CA events lower, and just focus on reducing OA and H. I think it may be time to switch to fixed pressure CPAP mode and set the pressure at 11 cm to start with.
Interesting night. I need to write down data from the Airsense 10 window when I go to the bathroom. As I recall, I got up at elapsed time of something like 4.4 hours.
There is a gap in pressure and flow between 22:40 approximately and 00.12 approximately. I was asleep. You mentioned that might be a time when the mask was dislodged. I sleep on my back almost all the time and wake up on my back so something happened. Any more ideas? Should I tighten the mask straps? I must have been breathing during that time.
Or maybe I was sleep walking and got up and went to the bathroom. Going to the bathroom requires shutting down the CPAP machine and disconnecting the hose at the same time because of the automatic start.
I have included another graph of different variables.
After I wake up for the major bathroom break, I sometimes do breathing exercises to relax and go back to sleep. I know that CO2 is the gas that regulates breathing. Some of the authors I read say that there is a need to increase CO2 for health reasons. One exercise is breathing in a paper bag. Last night I used a modified 4 6 8 routine. Not sure about the magic numbers and didn't follow faithfully. But the strategy is to breath in quickly, 4, hold breath for a longer time, 6, and then exhale, 8, to maximize the CO2.
Does this explain the graphs for these variables? Title volume, Insp. time, Exp. time?

Here is how I can tell if I went to the bathroom in that first 15 minute break. I may have have mentioned that I have an artificial unitary sphincter to control leakage as a result of prostate cancer removal surgery. The nylon device is implanted. There is a bulb in my scrotum that when squeezed sends air pressure to open up the sphincter on the urethrae. It takes two hands to operate the device. Left hand to hold the top tube out of the bulb to stabilize the device and the right hand to squeeze the bulb. I have to stand up because if I sit down there is not enough gravity to empty my bladder and I leak on my PJs. I made an artificial urinal by cutting out a section of a 1 gallon plastic water jug. I use my pinkie (left smallest finger) on the left side of my hand, putting it in the handle of the jug, and the rest of the fingers on the left hand to hold the top tube, and then using the right hand to squeeze the bulb and aim. I can empty the the jug each time. So when I get up after say 5 hours, I can tell if I got up earlier and went to the bathroom earlier.
Given all the stuff around my head: cushion, frame and cervical collar, it might be sleepwalking.
I am very sure that the blank parts are due to the mask being off, and the machine shutting itself down automatically. Then when the mask is back on, it starts up. No way to tell why the mask has come off.
When I get up in the morning or for a P break in the middle of the night I get out of bed with the mask on, then press the button on the top of the machine to stop it, and once I have pressed the button I hold my breath until I get the mask off, or it will start again.
Despite the blank spots the outcome seems quite good for a fixed pressure. The hope is that a fixed pressure all night may be less disturbing to your sleep, compared to the pressure going up and down automatically. Time will tell.
The one thing I noticed is that your Ramp Start Pressure seems to have moved back to 4 cm. You should reset it back to 9 cm for more comfort while going to sleep.
I don't watch the tidal volume much on my OSCAR, so really can't comment from experience, but it seems like you were breathing very deep and erratically for that last part of the night.
My wife does this hold her breath breathing thing. Don't know if it helps with her sleep, but I know when she holds her breath for more than 10 seconds at a time the machine flags it as an OA event, and the more she does it, the more it drives up her AHI score!
It looks like I didn't restart the machine after I went to the bathroom. I thought that it would start automatically. That interval of machine off is over an hour. That meant that I was breathing into the mask for over an hour with no pressure assist. I was in a degraded breathing state.
The CSR happened when the machine realized that it needed to restart and did it automatically.
Is this a reasonable view? Even with this a very good night. Without the hour off it would have been a night over 8 hours and approaching 9 hours. I have not slept that long for years.