I've recently completed two sleep studies and received my pressure number: 9cmH20. I bought a ResMed s9 on craigslist.
This setting is causing me issues. I wake up every three hours running it. The doctor told me that my AHI was 12. I've fiddled with the clinician settings while using 9cmH20, to my knowledge there are no other magic settings to make this pressure work for me. I have a standard and heated tube . Full, nasal and pillow masks. My AHI is usually 0.5-1.2 with these settings. I changed the pressure to 7.4cmH20 (I may have over did it), but I finally slept through the night, AHI 0.0-0.2. I sleep between 6-7 hours a night.
The issue is that I'm exhausted after 6 hours of being awake. My job requires concentration or else I'm extremely inefficient and unproductive. I've recently beat depression and anxiety, so I don't think it's that. My blood results have only showed a vitamin D deficiency, which I'm treating but still nothing.
Any advice would be greatly appreciated, I just don't want to be exhausted (near fainting) after 4 hours anymore!
These are my sleepyhead results on 7.4cmH20, 7.8cmH20 and 9cmH20.
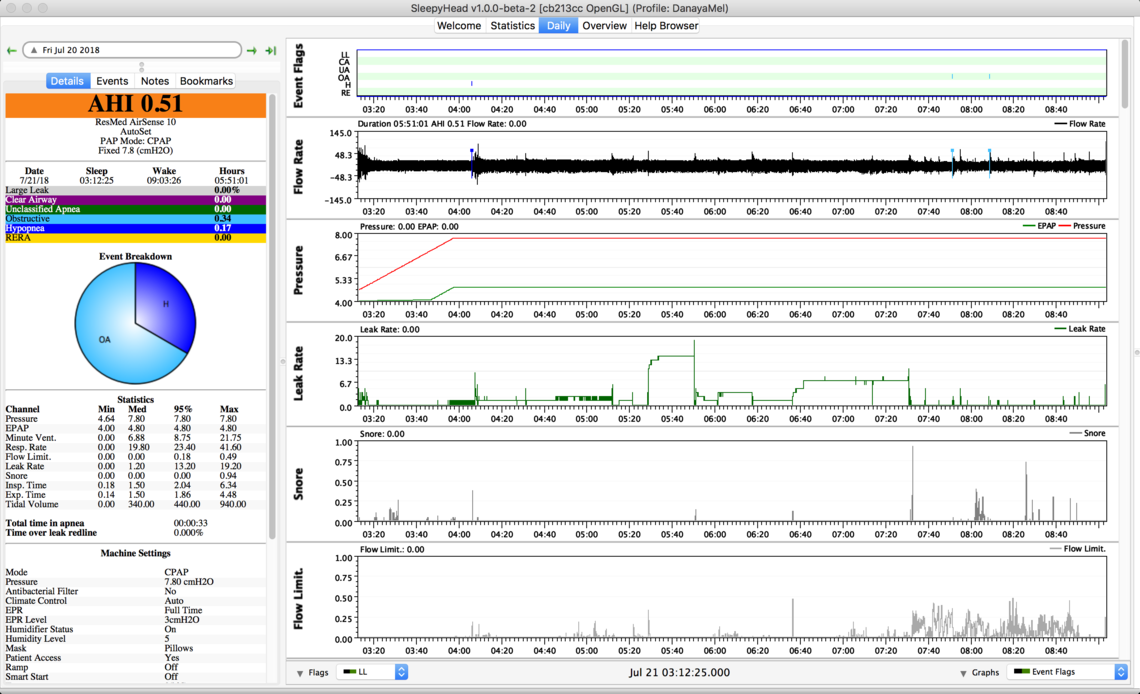
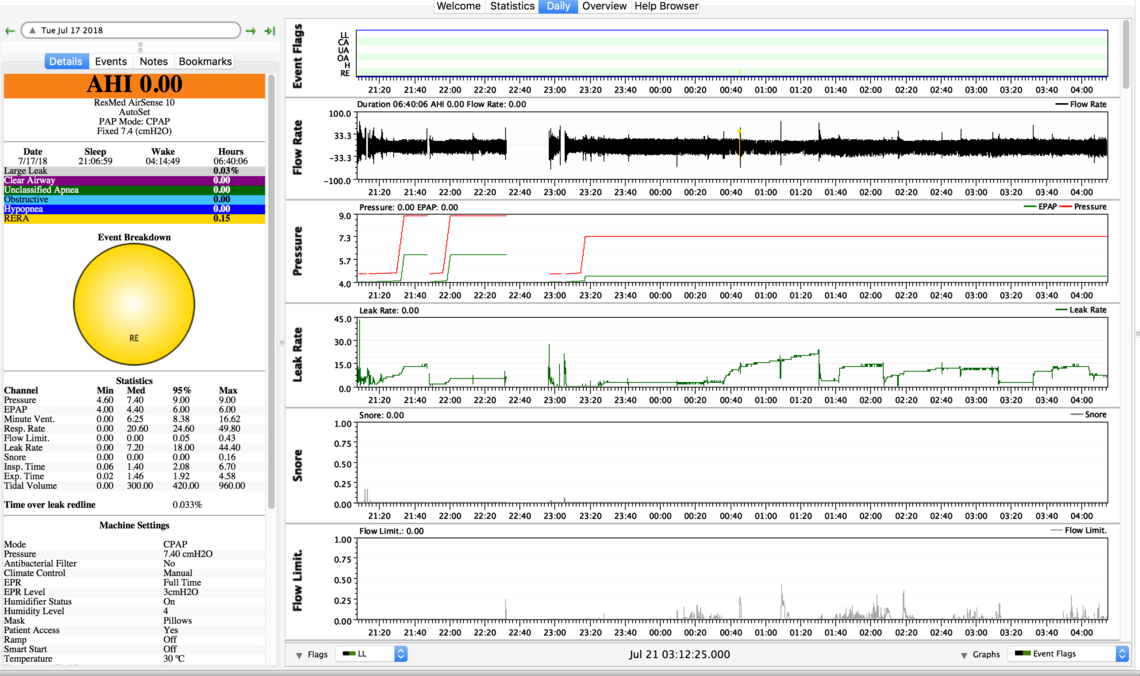
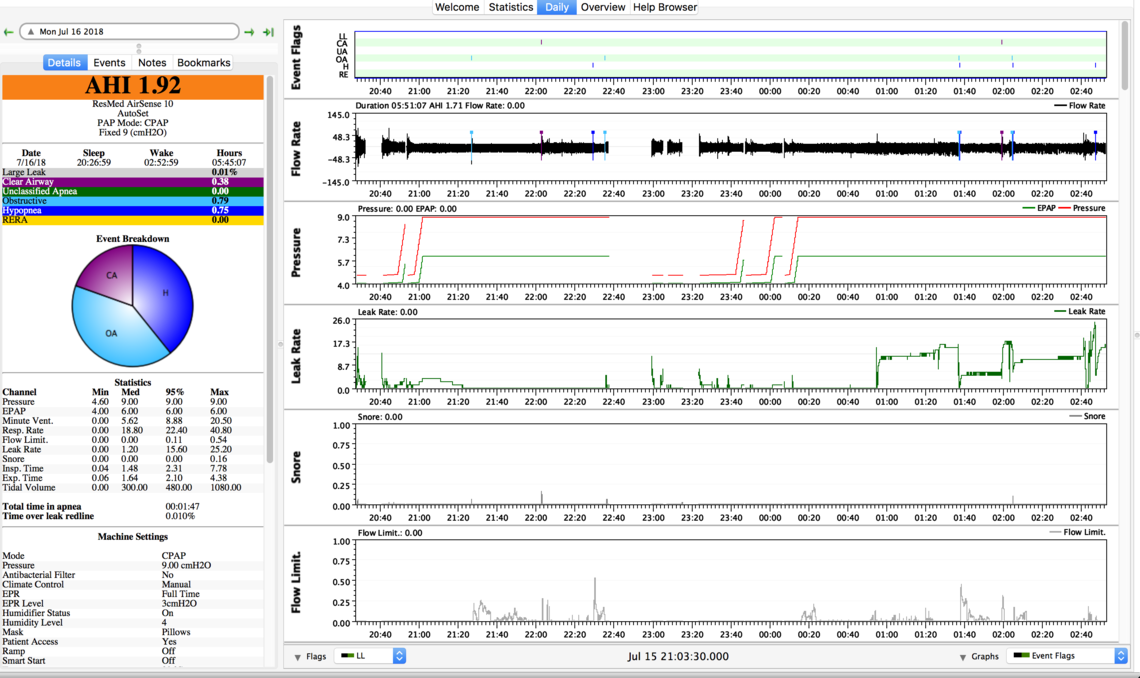
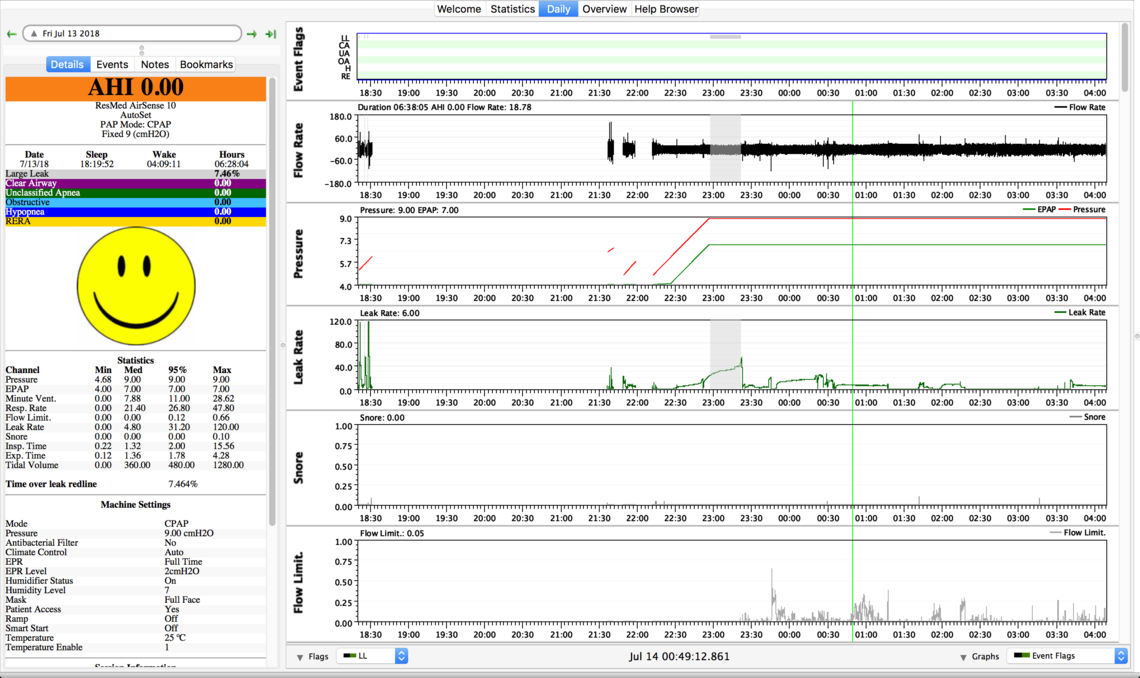
First, I would say that those Sleepyhead charts do not indicate any kind of real serious problem with the CPAP setup. You are not having a large number of apnea events with any of the settings. There are some issues with mask leakage on some nights. You have flow limitations and indication of snoring at the lowest pressure setting, but you say that setting gave you the best sleep.
I think I would focus on trying to figure out what is waking you up, and post again on your observations. Ideally one should try for about 7.5 hours of sleep per night to be fully rested for the next day. Waking up once or twice is not all that bad, but no wake ups is obviously good too.
Some comments on your CPAP and setup. You say you have a Resmed S9, but the Sleepyhead reports indicate it is an AirSense 10 AutoSet. I also see that you appear on some nights to be using the Auto Ramp feature that is in the A10, but not in the S9. I'm not real sure your setup is a problem, but if you want to try a new setup and you have the A10 model, here is what I would do. I noted that you know how to get into the Clinical Menu to adjust.
Set the Mode to AutoSet instead of CPAP - That will let you set a minimum and maximum pressure, and the machine will adjust between those limits to give you the minimum needed for treatment.
Set the minimum pressure to 7 cm. Set the maximum pressure to your sleep study recommended 9 cm.
Set the Ramp Time to Auto, and set the Ramp Start Pressure at 7 cm.
Set the EPR Type to Ramp Only.
Set the EPR to 3 (which is where I believe you have it now)
What will this do? First it lets the machine determine how much pressure you need, and it may result in a lower more comfortable pressure (within the limits you set). Using the Auto Ramp Time feature holds at the Start Pressure at 7 cm until it decides you are asleep. I think you may have it at 5 cm now. I find that pressure a bit low to be comfortable and you can feel a bit starved for air while trying to go to sleep. With the EPR set to Ramp Only with a setting of 3, this provides you with maximum comfort while you are going to sleep. Then when you go to sleep it stops the EPR reduction of the exhale pressure. This may also reduce the actual pressure the machine uses to treat your apnea while you are sleeping. Lower pressure not only improves comfort, but it may also reduce mask leaks, which can be annoying too, and wake you up.
So, while I am not sure your machine setup is the real issue, this method of setup could help by improving comfort some. But, most important, try to figure out what is waking you up.
Hope that helps some,
Thank you for your response, it really is a big help!!
I believe I do have a Airsense 10, sorry. I'll try the Autoset with those settings.
Sometimes after sleeping for 8 hours (with the machine), I am tired after being awake for 2 hours, is this normal for someone with sleep apnea? Also, this may sound weird but sometimes with a pressure higher than 5, it almost feels like my head is a balloon being inflated but the mask lol, I find that 5 is the most comfortable when falling asleep – It almost feels like the mask isn't there.
I sleep on my stomach and side, so about twice a night I wake up for about 5 seconds to readjust and fall back asleep.
Once you change your Mode to AutoSet and let the A10 control the pressure, and then look at it in SleepyHead, you will get a much better idea what pressures you need. Too low of a pressure can be as uncomfortable as to high. I like to see the actual pressure reach the max pressure setting 2-4 times a night, but not flatline there. On the minimum side I like to see it reach minimum about that many times or perhaps more. It is OK for the pressure to flatline at minimum for periods of time.
CPAP can certainly help to resolve wake up issues due to apnea events. However, it adds some complexity/discomfort to the sleep process. It takes time to get comfortable with the machine, and it certainly improves over time. There can be other issues in getting a good nights sleep. I stumbled onto a website which was started by a pharmacist in Canada that believed too many people were unnecessarily using sleeping pills. He is also a University professor, and I suspect the website is probably a grad student project. He does not seem to be selling anything, and I believe he is getting government support for the project. In any case, he advocates the use of Cognitive Behavioural Therapy for Insomnia, or CBTi. Whether you suffer from insomnia or not, there are some good tips there for getting a good night's sleep. I have started following some of the recommendations made. In any case here is the link if you want to check it out.
Hi everyone. My husband was just issued a ResMed AirSense 10 by his insurance. We've been PAPping together since 2012. He got to take a step up from his Respironics System One and I was wondering how it worked. Thank you Sierra...I have a clearer picture now. I recommend the sleep disorder glossary found at sleepyhead.sourceforge.net online. It's very helpful in interpreting NiyaNiya's sleepyhead results.
I wish everyone had great health insurance that pays for everything but there is great disparity out there. I know that some, out of sheer survival, must do a lot of things that are usually reserved for the health professionals. Those of us who have great insurance don't have to do anything with our machines or with our therapy because it's all done for us...well, it's supposed to be, but actually, it often isn't, but we never know, so I guess we're happy with that. We don't have to learn anything about sleep apnea or about our machines or our therapy. Lots of us are just plain disinterested in the whole she-bang. We just want to sew our quilts, see after our babies and/or elderly parents, go to our jobs, eat, breathe, drink, (hopefully exercise) and let the doctors and their machines do it all. I'm not at all sure that we are well served by this.
So, some of us must fiddle with our therapy and obtain what we need in any way possible. And we inquisitive folks must know...we just have to find out all about our particular apnea and how our therapy works and how to detect the problems that our health professionals must be made aware of, and how to call for help when we should. The rest of we patients get seen once per year to get our data checked. The data that gets checked is: how many hours of compliance we have achieved and what our AHI is to confirm that our therapy is effective...period. This is very important for those on Medicare and some other insurances because we get checked after starting our therapy at the 3-month point. If we are not compliant (4 hours of recorded therapy per night), our machines are taken away from us and we must buy our own equipment and supplies. It's expensive...really expensive, especially for those on low, medium or fixed incomes.
Congratulations NiyaNiya on winding up with an amazing device! Your timing was excellent as Sierra is a newbie on the forum - and as you surely must suspect, is drawing on his own experience to help others. Please do see after the possible insomnia issues. I noticed from your data that there is wide variation in your sleep time...you're making it to bed anywhere between 3:00 am. and 9:00 pm. and are arising anywhere from 3:00 am to 9:00 am (and all this within a few days or a week). That wrecks havoc with something called our circadian rhythm and sleep becomes quite disturbed. You might have to adhere to this schedule because of swing shifts, etc. If so, you could contact your doctor and see if he/she would approve a course of melatonin to coax your body along with the hectic schedule you must keep. It's available over-the-counter, but it would be good, if your doctor agrees that this course is wise, to have it all charted in your medical record. By the way, that medical record might fish you out of a jam some day when you get passed around to different health providers. An added benefit to the melatonin is it might extend your sleep time a bit...maybe 8 solid hours. Wouldn't that feel good?
Wow...I'm all typed out. Anyway, I'm rooting for you...keep up the good work! Success is what counts.
I find it very helpful to have a Clinical Guide Manual for the AirSense 10 AutoSet as well as the user manual. While many are not comfortable making their own adjustments to their machine, others do. And, even if you have no interest in making changes, ResMed includes a lot more detail in the Clinical Guide as to how the machine actually works and what the various features are about. If nothing else the first dozen pages or so are a good read. The only issue is that the guide is kind of hard to come by. I just stumbled on a link that has a copy of the guide (see below). I would suggest downloading it and saving it as a PDF for future reference. The other thing the guide does is explain the difference in how the For Her version works compared to the standard version. The interesting part is that the For Her is just another option in your Mode selection, so you can buy the For Her version, and make it operate like the standard version. I was not aware of that when I bought my standard AirSense 10. If I had known I would have bought the For Her version, even though I am male. And now I know how it works, and what my needs are, I would probably operate it in the For Her mode instead of the standard mode.