My adventure on this journey started about 6 months ago when I finally agreed to talk to my primary care Dr about my sleep issue... Actually it was my wife's sleep issues... She couldn't get good sleep because of all the sounds I was making at night.
From there I was sent to an ENT. The ENT then sent me to both an allergy specialist and recommended a sleep study. I already knew I had seasonal allergies so I had no issues going down that road. They did the back prick thing and told me I'm allergic to just about every tree, weed and grass they tested me for. I'm now getting shots to hopefully lessen the effects there.
It took insurance about a month to approve the first sleep study. I went in and they hooked everything up and off I went to sleep. They told me that if my numbers were to low that they would hook me up to a CPAP machine. I slept through the whole night but they never hooked me up to the CPAP.
A couple weeks later I talked to the ENT about the results and was told I would need another sleep study, this time with the CPAP for the whole night. Apparently during my first sleep study they said I had complex sleep apnea. There were several obstructive someway but about 1/3 of all my apneas were central apneas.
During this second study (which took almost 2 months for insurance to approve) the sleep tech was pretty much dialing in what type of CPAP settings I would need... As well as testing the different type of CPAPs and how they worked on me.
A couple weeks later I got the results back from the second sleep study and was told I needed to be on an ASV machine. It took the DME company almost a month to get approval and order the machine for me.
So about 2-3 weeks ago I went in to get this new found miracle machine and hope for the best. With no previous CPAP experience I just took what they have me and went home.
I received a ResMed AirCurve 10 ASV and a Philips Nuance Nasal Air Pillow. I guess that's the closest to what they used at my sleep study.
I was told to try and get at least 4 hours on the machine each night. So the first night I had high hopes of possibly getting my first full night's sleep. Not so. I woke up after about 2 hours with severe abdominal pain and lots of bloating. After I released a ton of gas I went back to bed and tried the mask again, since I didn't get to my 4 hours. Once again after 2-3 hours I was awake. So much for a good night's rest. I knew I had my 4 hours so off went the mask and bed to sleep I went.
The second night was pretty much the same. The third I had little less gas and bloating and was on the machine a little longer but woke up with my mouth wide open and my wife complaining about all the noise of the air leaks.
It was then the I tried to contact my DME supplier to discuss what has been happening. When I called I ended up at a voice mailbox. No response that day. The next day they called back but due to the nature of work I'm unable to answer phone calls. So we played phone tag for about a week. After about 10 days I managed to get an appointment for a mask refit. During those 10 days I did a lot of self education on the web and though trial and error figured out that the "air swallowing" or Aerophagia was my biggest issue.
Here's what I believe has been happening to me. I would got to sleep with my ramp up rates of 5-9 increasing to 10-15 and then as high as 25 during central apnea events. Air would be forced into my digestive tract during the higher pressures causing bloating. I would then burp causing my mouth to open. Once opened the constant high pressure wouldn't keep it open until I woke up with a dry mouth and lots noise from the air pressure leaking out my mouth. This would happen a few times each night.
During these 10 days of self education and lack of response back from the DME I went out on my own and picked up a chin strap. This worked great for 1 night. The next couple I would still burp but just my lips would open...still the same effect, dry mouth and waking me up.
So 3 nights ago I finally got in for my mask refit. I ended up getting a Dreamwear Full Face mask and ClimateLine tube. The first night was great. I had virtually no leaks. The second I must not have had a good fit as there were some air leaks. Last night went much better also with no leaks. I still have a dry mouth when it pops open to burp but it doesn't fully awake me. I just lick my lips, close my mouth and drift back to sleep.
I'm hoping over time that the "air swallowing" will continue to decrease as my body adapts and that I get more and more good nights of sleep.
This was my response to your post in another thread on the aerophagia issue.
"I have not suffered from this air swallowing thing which is referred to as aerophagia. This link on the causes and possible resolution may be of help.
Aerophgia Causes and Resolution
The issue of letting air escape out of my mouth is one I do suffer from. The best resolution I have found is to use mouth taping. I tried a couple of full face masks, but found I was mouth breathing and would wake up with a sore throat. So I have gone back to a nasal mask and tape. It is not as awful as it sounds. Here is a link to a video on the technique. I am not sure if it would help the aerophagia or not.
How to Mouth Tape for a Better Sleep"
Mouth Taping with the nasal mask may be worth a try. I found I needed to use a chin strap as well as mouth taping to keep my mouth closed. I don't know if it would stop the air swallowing or not though, as I said, I have not had that issue. I use the Nexcare 1" gentle paper tape from 3M.
As far as getting the best out of your ASV machine, have you considered using SleepyHead? If you have a PC or a Mac and a SD card reader you can transfer the detailed data to your computer and view the results over time. It gives you a very detailed picture of what is happening overnight. I certainly would be interested in seeing the results you are getting with the ASV. At one point I was thinking an ASV was in my future to control central apnea. However, for now I seem to be able to get my AHI down to the 2-3 range with the AirSense 10 AutoSet machine.
I've read about the mouth tapping and considered it when my DME and I were unable to communicate with each other. I really didn't like the chin strap. It felt to confining for me and the neoprene began to stink after just a couple nights even after daily washings. I have been using the Sleepyhead program to look at my machine data. I will post a sample night tomorrow morning.
So far, I have been enjoying the Dreamwear Full Face mask, even if I've only had it for 4 nights. It's not as confining, doesn't require as tight of a fit as the chin strap and is much easier to keep clean compared to the neoprene. My wife also likes that I can communicate better with the full face mask on. While my speech may be muffled from the mask, talking doesn't introduce any air leaks when I open my mouth.
A "Good" night:
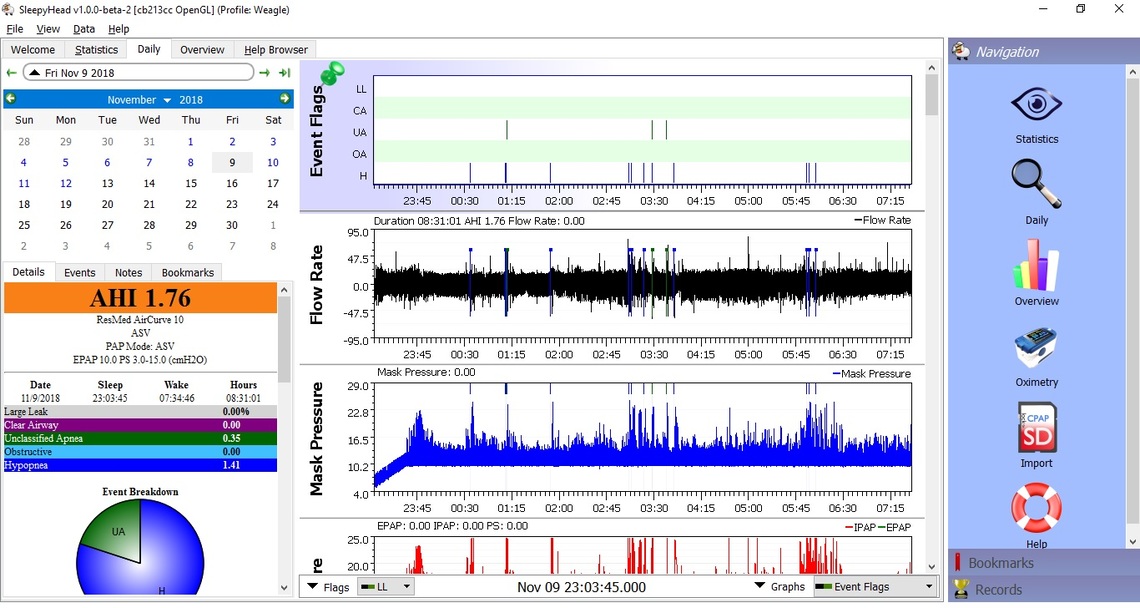
A "Not-so-good" night:
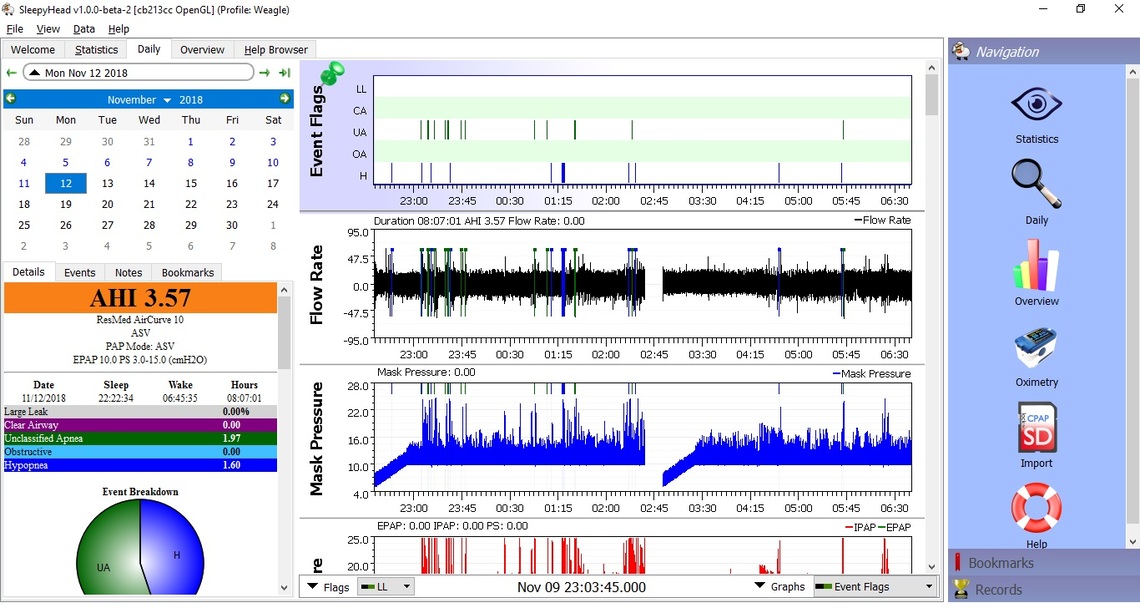
Those are very interesting reports. The ASV seems to be very effective in normalizing CA and OA events. However, it seems they may not really be eliminated, but are instead classed as unidentified apnea. I also consider hypopnea events to be potentially either obstructive or central events in development, but do not go to full apnea.
I am not a medical person so really can't say if avoiding mouth breathing with taping would help to prevent aerophagia. It may be worth trying just to see what it does. Your machine is certainly using lots of pressure on IPAP, right to the limit of 25 cm the machine is capable of. It seems well documented that more pressure can cause aerophagia. I would not hazard any kind of guess to suggest whether or not lower EPAP and/or PS would be possible. Something to discuss with your sleep doctor though.
It would be helpful to optimize your SleepyHead layout a bit so more data can fit on the screen. The F10 key hides the right menu, as it is kind of redundant anyway. Clicking the triangle beside the date hides the full month display and lets more data below show up. And if you go to File, Preferences, Appearance, and then uncheck the pie chart display box, that will hide too. The breakdown still appears in the colored bars above it. Last drag the gray lines between the graphs to scrunch them down a bit so more graphs can display on the screen. In addition to what you have, I like to see Flow Limitation, Snore, and Leaks.
Have you zoomed in on those times/events in the night when you are getting a concentration of events and the PS is peaking in response? I just do it by left clicking in the area of interest until I can see the individual breath flow curves. The left right and up down arrow keys also work to fine tune it. If you zoom in you may be able to see what the machine is doing or not doing to address those events.
The bottom line is that the ASV seems to be working for you, if you can keep AHI under 5. I'm curious. What was your original diagnosis AHI?
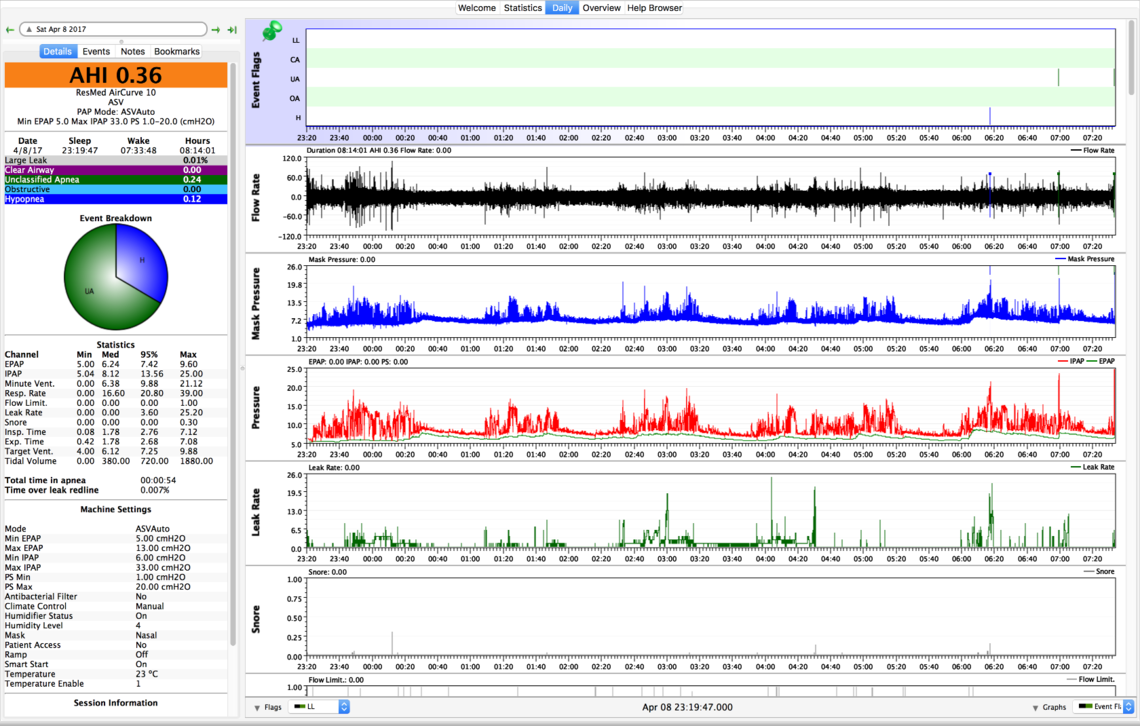
I did a little searching on line for SleepyHead charts with an AirCurve 10 ASV machine. I found the one below, which is showing a very good AHI. The pressures seem to be set up a little differently than yours with the minimum EPAP lower at 5 cm and the pressure support range higher at 5-20. Pressures tend to be individual, and I don't think you really want more pressure. However, one significant difference I noticed is that the Mode on this machine is set to ASVAuto, while your machine is set to just ASV. Here is what I see in the clinical manual about the difference. A quote:
"ASV mode
In ASV mode, the expiratory positive airway pressure (EPAP) is fixed and can be manually adjusted to eliminate obstructive events. The Pressure Support (PS) varies between the Min PS and the Max PS to answer to the patient's need. Mandatory breaths are delivered at the patient’s recent spontaneous breath rate, ie, the timed backup rate is automatically calculated to match the patient’s needs and is applied appropriately in the case of an event.
ASVAuto mode
In addition to the functionality of the ASV mode, the device in ASVAuto mode automatically adjusts the expiratory pressure in order to provide only the amount of pressure (EPAP) required to maintain upper airway patency. The device analyzes the state of the patient’s upper airway on a breath-by-breath basis and delivers expiratory pressure within the allowed range (Min EPAP and Max EPAP) according to the degree of obstruction. EPAP is automatically adjusted depending on three parameters: inspiratory flow limitation, snore, and obstructive apnea."
A question you might want to ask of your sleep doctor is if there may be some benefit to you to switch to the ASVAuto mode. It sounds like it gives the machine a little more flexibility in keeping the EPAP pressure lower, which may help with the aerophagia. Also there may be some opportunities to limit PS and IPAP as well.
I will play with the formatting of the SleepyHead output later tonight when I get home. During my first sleep study, done back in June, (without any CPAP machine at all) the tech wrote the following:
Mild snoring was present. The patient exhibited an apnea hypopnea index of 13.3 events per hour of sleep and a restaurant disturbance index of 37.8 events. Events consisted of 29 central apneas, 62 hypopneas and 167 respiratory effort-related arousals. The REM index was 6.4, supine was 40.5, lateral 30.3. The central AHI was 10.5 The mean saturation of 86% with 0.4 minutes with a saturation less than 88%.
A lot of gibberish I don't fully understand.
Here's a more condensed display from SleepyHead. Harder to read the details though.
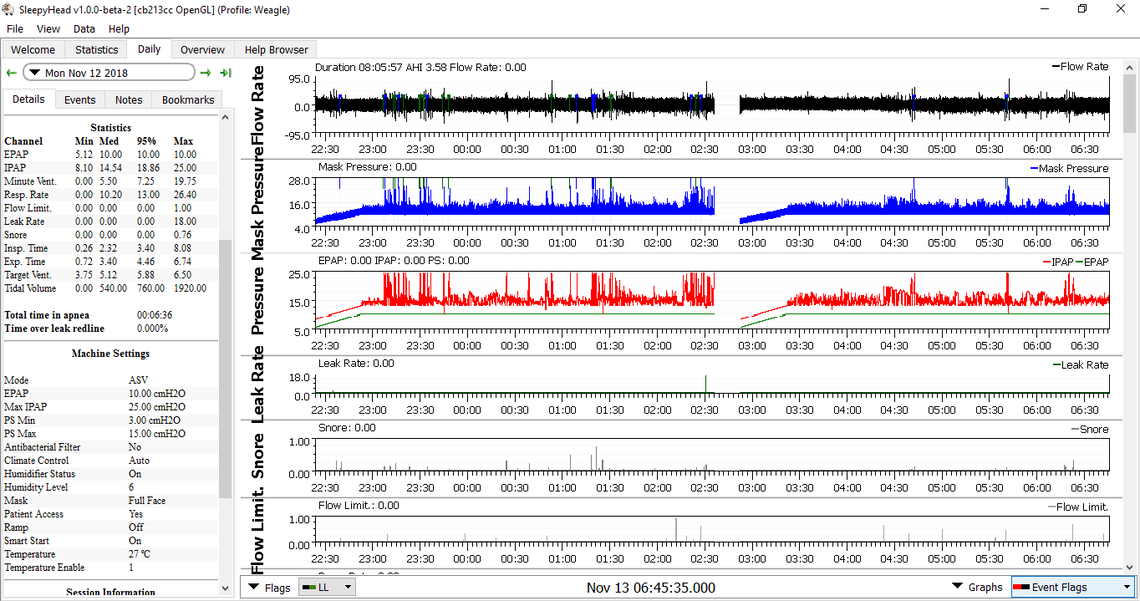
That is better. I like to leave the events bar pinned to the top though. It seems like you may have a wide profile display monitor. Sometimes it helps to maximize your SleepyHead window to full screen before you do the screen capture. It is always good to leave the summary of events bar on the left showing. No need for the pie chart, but the bars with the breakdown of events is good to see. If your leak rate is always that low, bump it off the bottom. Looks nearly perfect, especially with the higher pressures you are using.
As I suggested above you could ask your sleep doctor about setting the EPAP lower, and the Pressure Support lower, and putting the mode in ASVAuto instead of ASV. The objective would be to try and get the average treatment pressures down, and possibly AHI down.
Just when I think I have a great setup with the Dreamwear Full Face mask for when my mouth opens, my body seems to change. Last night between 2am and 3am, I found myself relaxing my jaw, opening my mouth and causing a leak which kept waking me up. I don't believe it was a bad leak, just enough noise and air escaping blowing near my eyes to be a distraction to me. I haven't looked at SleepyHead yet, but the MyAir app shows little to no leaks. But to me, after waking up 4-5 times, I reluctantly put my chin strap over the full face mask and slept great the rest of the night. I'll be interested in seeing what SleepyHead shows this evening.
Are there any tips to retrain my mouth/jaw muscles to stay closed when sleeping? I suspect that over the last 10-15 years of seasonal allergies and clogged sinuses has something to do with my mouth getting used to opening at night. I've been taking allergy shots for several months now trying to alleviate those issues and right before bed I use a nasal spray to keep my airways as open as possible while on my ASV machine.
The tip that is frequently given to keep your mouth closed is to position your tongue on the roof of your mouth and up behind your top teeth. That certainly works when you are awake, but the more difficult trick is on how to maintain the position when you are asleep and the CPAP pressure is up. I now both mouth tape and use a chin strap with my nasal pillow mask. Not sure if you could mouth tape with a full face mask. It might mess up the seal on your face. As for a chin strap I have tried a few different styles including a home made one from a tensor bandage. The one that works the best for me is the Breathewear Halo one.
Well another weekend has gone by and I'm making progress ever so slowly towards getting a better night's sleep. I've found that a chin strap in conjunction with DreamWear Full Face mask seems to be the best fit for me. I'm still experimenting with the chin strap under or on top of the mask to see which works better.
When I put the chin strap on first, the frame of the mask is a bit tight but workable. I just have put pull the lower section by my chin out from under the seal of the mask. This give a great seal, since the chin strap also adds additional pressure keeping the lower section of the mask sealed to my chin when my mouth opens at night.
When I put the mask on first then put the chin strap over top, the frame of the mask fits great around my head. My concern is that where the chin strap goes over the frame of the mask that it may be pinching the tubes a bit lowering the pressure, especially when I lay on one side or the other. I don't think it's too badly impeeded though as the machine hasn't complained of any blockages.
Lastly I also ordered a different type of chin strap to try out. I'm still nto entirely sold on the neoprene one I have. it tend to pull my chin back while holding it closed. I ordered the PAP-CAP from CPAP.com I will report back how it works once it arrives.
Lastly I'm still also trying to get in touch with aa Dr. who can authorize a presssure change on my ASV machine. I get a full night's sleep about once a week. The rest of the week I get 4-5 hours and wake up completely bloated and uncomfortable due to air getting in my intestinal track. My ENT who prescribed the machine on the recommendation of the Dr who analyzed my sleep study isn't comfortable making the recommended changes himself. Nothing seems to be easy in this process.
With the Breathewear Halo chin strap I use, I put the P10 mask on first, and then the chin strap second. However, I need the chin strap for two purposes. One is to keep the mask from slipping off, and the other to keep my mouth closed. In your case I can see it may make sense to put the chin strap on first.
On the doctor issue, you need to get someone who has experience with the AirCurve 10 ASV machine. It is a pretty sophisticated and complex machine. Sells for about $5000 on line in Canada. If they were not so expensive I would buy one. I have put that decison off until I am unable to keep AHI under 5 with the standard AutoSet model.
I found a document that you might be interested in. It basically outlines the ResMed view on how to titrate the settings on the various machines, including the ASV model. Here is a link to it:
The section that covers your ASV machine starts on page 30. The basic setup for the ASV and ASVAuto modes are given on page 33. Your machine appears to be the basic setup for the ASV mode, but with the EPAP set at 10 cm instead of the recommended starting point of 5 cm. This could be because they tried it in the lab and had to increase EPAP to eliminate obstructive apnea? Or, it could have been just a guess. There is a possibility that it is too high. But that is not certain as your hypopnea has not been eliminated. I do not see any OA events though.
There is another recommended setup for the ASVAuto mode. It is pretty much the same as the ASV except there is a range allowed for the machine to adjust EPAP in, with a recommended setting of 4 cm minimum and 15 max.
So if you can get in to see a doctor that understands the machine, I would ask them if it could be changed to the ASVAuto mode with the recommended default settings. The Auto mode may allow the machine to use less pressure. That in turn would make the mask more comfortable, and hopefully reduce the gas problem too...
Hope that helps some,
Well the saga continues with trying to change my ASV machine settings.
First I called my DME and as I expected they can't make any changes without the prescribing Dr's authorization.
Second, I called my ENT who prescribed the ASV machine per the recommendation from the Dr. who did the analysis on my sleep study. He's not familiar with the machines or what setting they should be set at. They told me to contact the Dr. who did my sleep study analysis.
Last I called the Dr. who did the analysis of the sleep study and since their office just did the analysis, not the one who initiated the process, they can't make any changes until I'm "under their care."
So now I'm waiting an additional 2 weeks until their next "new patient" opening is available. So I guess I get at least 2 weeks of feeling bloated each and every night until this appointment before any changes can be made. I'm reluctant to make the changes myself since I already know they will be pulling the SD card and analyzing the past several weeks history before they make any changes.
The sleep I am getting feels better, I just wish I didn't wake up after 4-5 hours of sleep nearly every night.
Yep, you are in a Catch 22 situation. I understand it, but have to feel sorry for you at the same time. As far as pulling the SD card and checking up on you, they probably already are doing that. Each morning after you shut the machine down you will see some activity on your display. That is the machine using WiFi to transmit your data to the provider already.
I managed to get into the Dr's office and they did lower my EPAP from 10.0 to 5.0 and I've been using that for the past week. After a week being at the new settings, my AHI did go up, it's constantly between 1.0 and 2.0 every night.
I'm starting to feel more tired throughout the day and while the bloating has gone down. I think I'd prefer a couple hours a day of bloating versus being tired all day. I guess on the bright side, I think being on the machine for a month has made an effect on me. When we changed the machine to lower levels I didn't get the same quality of sleep and tend to be dragging the more nights I'm at the lower settings.
I've been told to put the EPAP back to 10.0 to get my centrals back under control. According to the Doc, the bloating should get better with time. Guess I'll give it another week and see if I'm back to where I was.
I haven't asked about the ASVAuto mode yet. I'll pose that after this week of getting back on track.
An AHI of 1-2 is actually not that bad. I struggle to get mine into the 2-3 range with the AirSense 10 AutoSet. Most of that tends to be central events. I'm still thinking your best bet may be to get the machine into the ASVAuto mode. The hope would be that pressure would be controlled to a lower level, and only raised when necessary.
As I understand it when the machine is in ASV mode, the EPAP pressure is fixed, and only the pressure support changes to control central apnea. If that is correct, then switching from 10 cm EPAP to 5 cm EPAP is a huge change. It is quite possible that even without going to ASVAuto, some EPAP pressure between 10 cm and 5 cm could be more ideal. A change of 1 cm is a much more reasonable amount to change at a time. That would give you two options. You could start at 9 cm and reduce it in steps of 1 cm after a week or so at each pressure level. Or you could go the opposite way, which may be better, and just go up 1 cm to 6 cm and try that for a week or so to see what that does, and then another step up, if AHI is not acceptable. Perhaps a fixed EPAP of 6 cm or 7 cm would give you good results without the aerophagia issues.
And the other option of course is to put it into Auto and let the machine do it.