Following up on what seems like a never-ending chase. 36 year old male, 160 pounds. Very active/athletic. No known conditions. Over the course of this year:
Primary care doctor, had all kinds of blood work done, thyroid checked, etc. Nothing found. Had an MRI of the brain, requested by my primary care doc with nothing unusual. The MRI was read with a side-note that stated deviated septum.
Neurologist: They saw the jerks/minor tremors that I have had since I was a kid and asked if I have had an MRI of my back (I haven't). If I try to do sit-ups, the core of my body violently shakes sometimes when I'm directly in the middle of going up or coming back from the movement. Only at the middle point. That can also happen sometimes when lifting weights, but the shaking is more so the muscle itself that is being used. Since I was a kid, I have always been "jumpy" in the sense of my body over-reacting. If I was about to drop something, instead of the one arm/hand moving (like a "normal" person's reaction), my whole body would react and move. If I walk into a store and the heat/air conditioning directly over the entrance blew on my head, I would automatically want to jerk my head and whole body down as if I nearly hit my head. If I sit back in a seat and the back of my head unexpectedly touches the back of the seat, my body wants to "jerk forward" for some unknown reason. I want to say that the "jerks" come from my lower back/core region. No one has figured out what that is.
ENT doc saw the MRI and requested a CT scan of my sinuses, which resulted in turbinate reduction/deviated septum surgery in July. My breathing is better, but I wake up feeling flat out exhausted every morning. I have struggled with poor sleep, couldn't concentrate in school and still have trouble focusing enough to drive a vehicle at 36 years old. I bought a simple SPO2 monitor and my pulse rate and oxygen levels spike up and down after I have been asleep for typically 2-4 hours. Pulse rate can go up above 100bpm and SPO2 goes down to and bounces back from the lower 90's back up into the upper 90's throughout the night. Something is clearly going on.
I had an in-lab sleep study earlier in the year, with only 2.75 hours of sleep. Of that, just a handful of minutes of REM sleep were present, so they never saw the full REM-side of things where everything seems to go wrong. There was a lot wrong with that sleep facility, the staff acted weird, the bed was hard, pillow was too tall, etc. They should have told me to take a couple of melatonin before I arrived, as well. The "first night effect" may have also been a contributor.
My brain is so tired of being tired that it now instantly tries to figure out what is going on the split second I wake. I thought my airway was closing or my tongue was falling back when sleeping on my back. Then I started feeling like it was doing it when I was on my stomach and side, too. Other times, it literally feels like I'm "too tired to breathe" like my lungs aren't wanting to take full breaths (unless I concentrate on breathing more deeply) the more I relax when I'm laying on my back. That could just be because I'm so exhausted, however. Then there are times like this morning when I woke up because my head and body "jerked" me awake with like 4-5 rapid-fire neurological jerks all done within a few seconds. I'm just getting to my wits' end and don't know what to do now. They do not seem to be hypnic jerks, they seem more like myoclonic or some other type of neurological jerk. Nothing about that was noted in the previous sleep study. No trial of CPAP. I'd have to buy it and if it is neurologically-related and doesn't help, I'll waste hundreds of dollars.
I'm wondering if those who work in the sleep field can recommend any neurological suggestions for me to consider that could interrupt my sleep. I'm started to wonder if there isn't something neurologically going on that a CPAP may not correct. I'm planning another in-lab sleep study after my insurance kicks in at the first of the year so that I can throw money towards my deductible for next year. What kind of conditions would cause my head and body to "jerk" away multiple times like that within a few seconds? There's no telling how many times I do that each night. That may very well be why I'm exhausted.
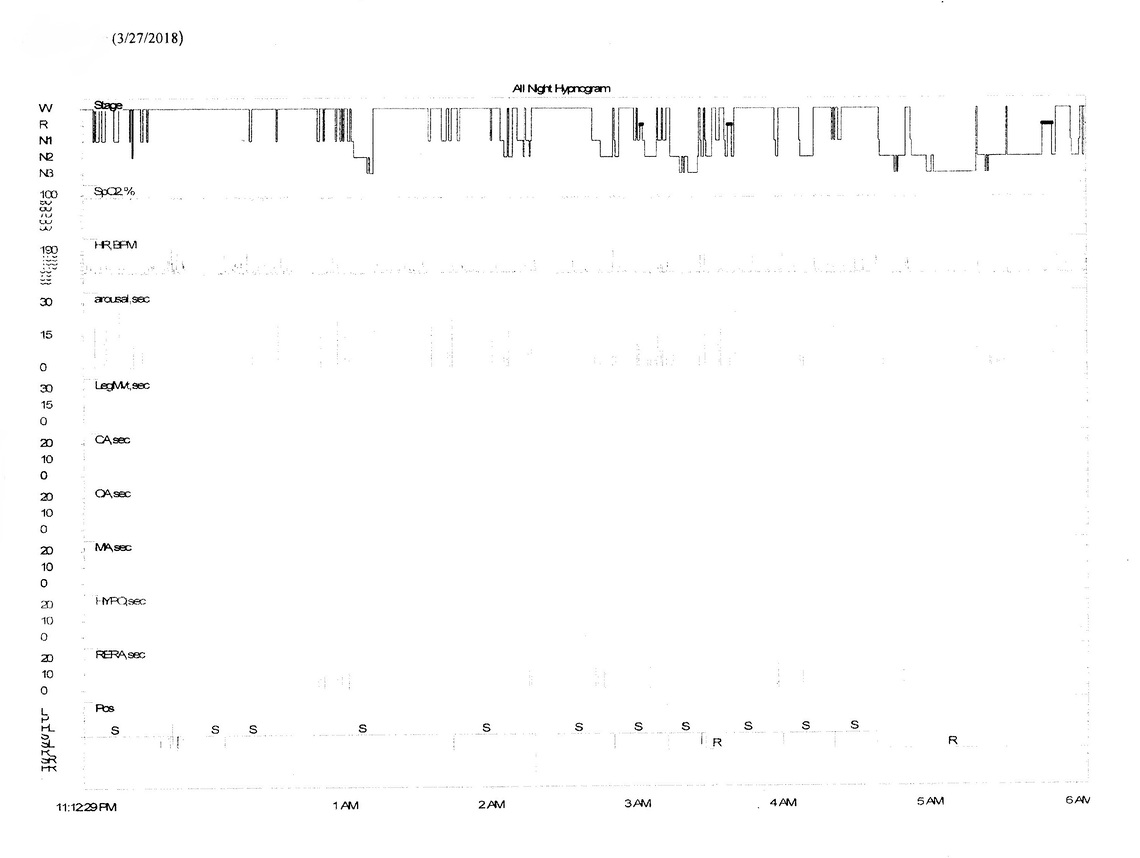
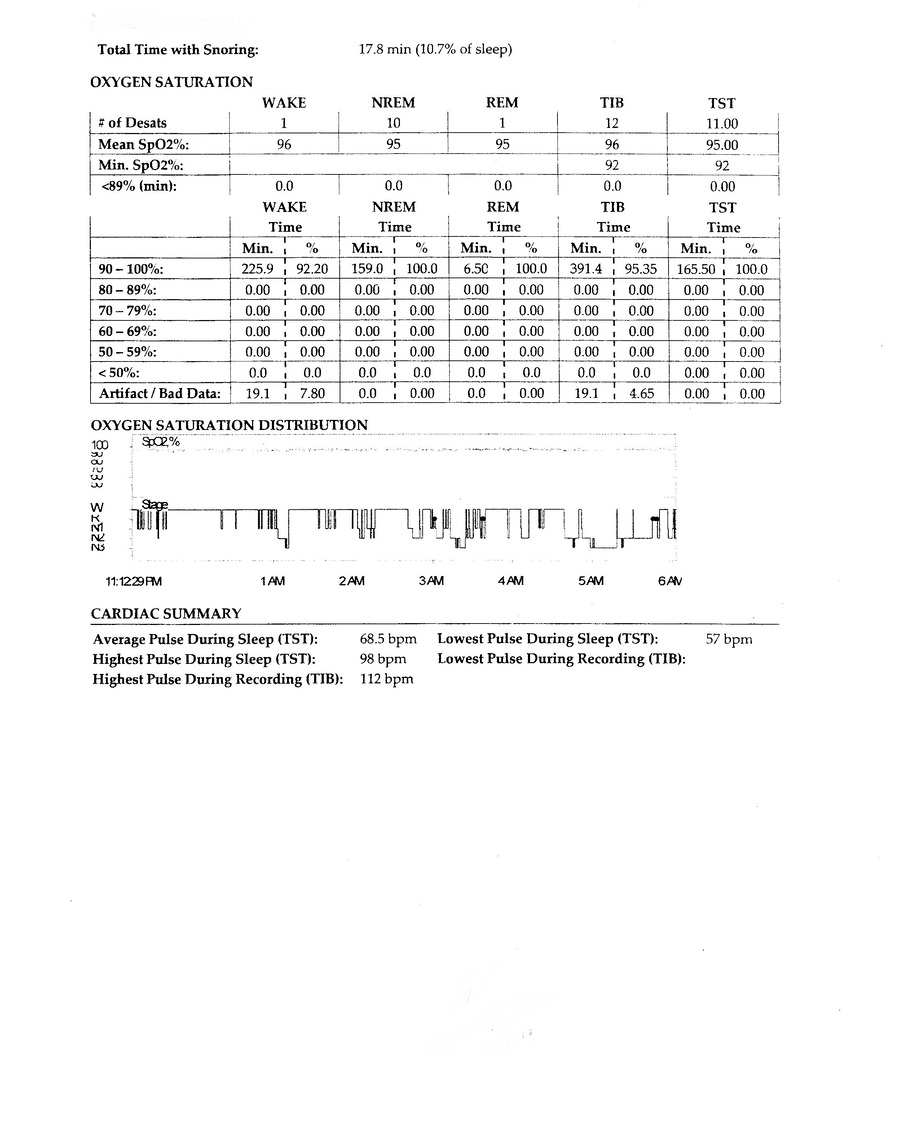
Sleep results from the March 2018 sleep study:
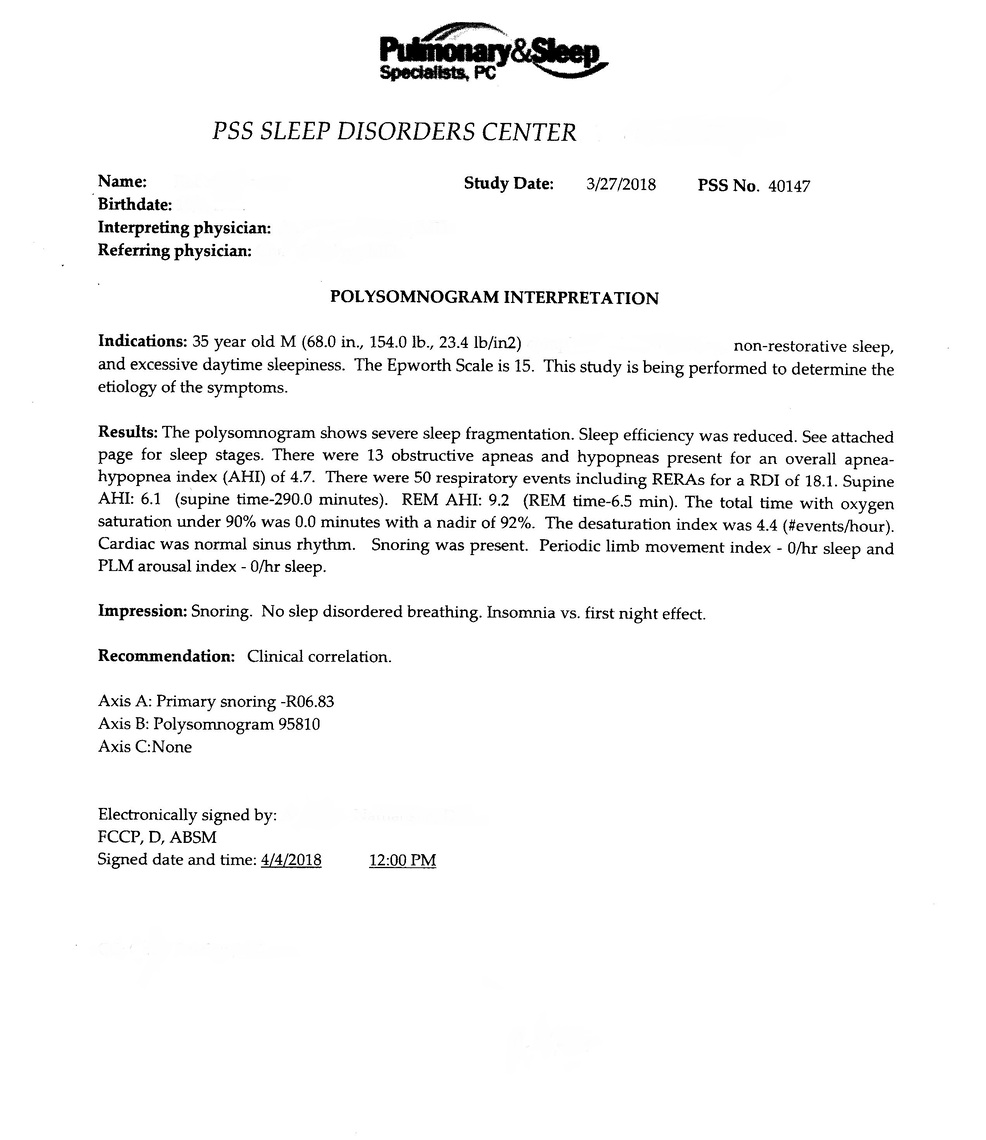
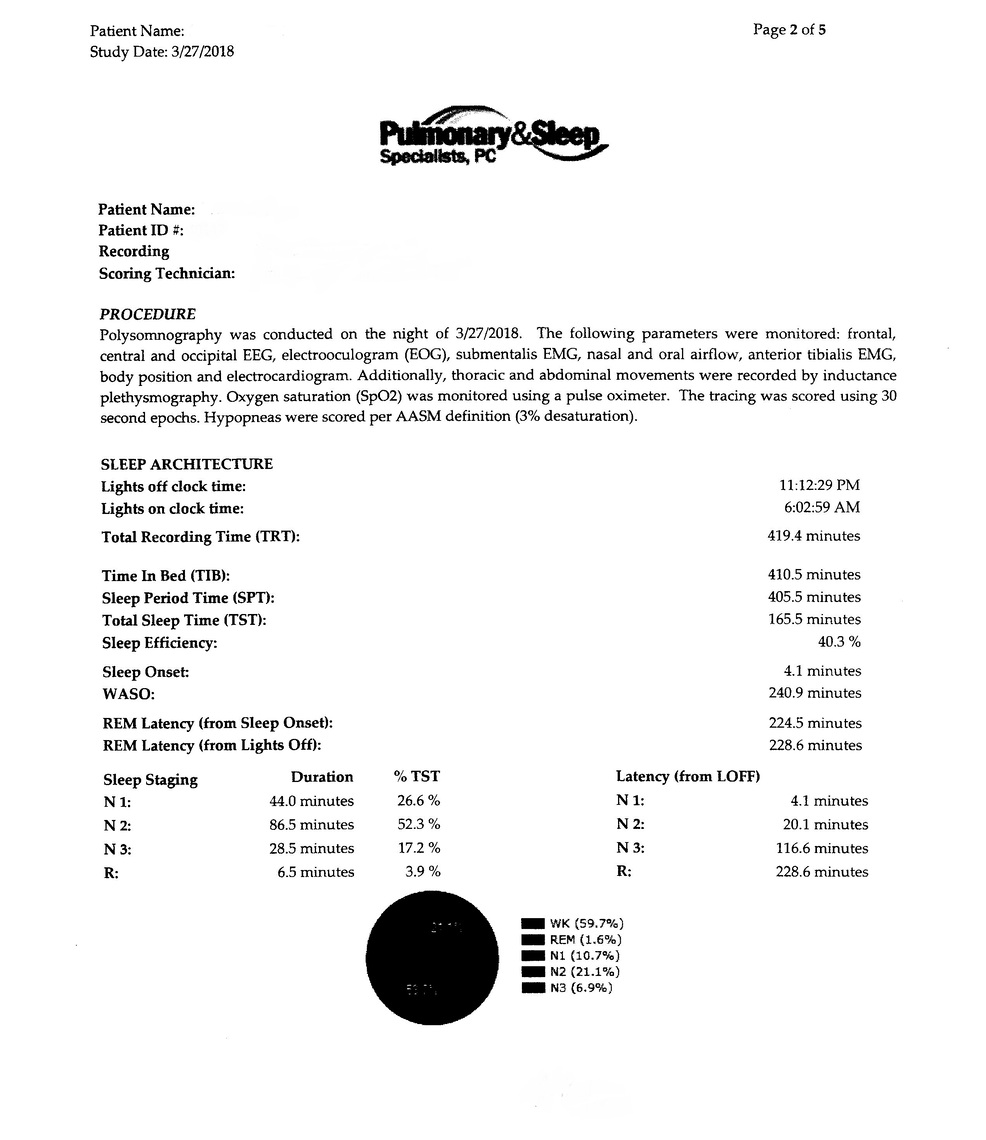
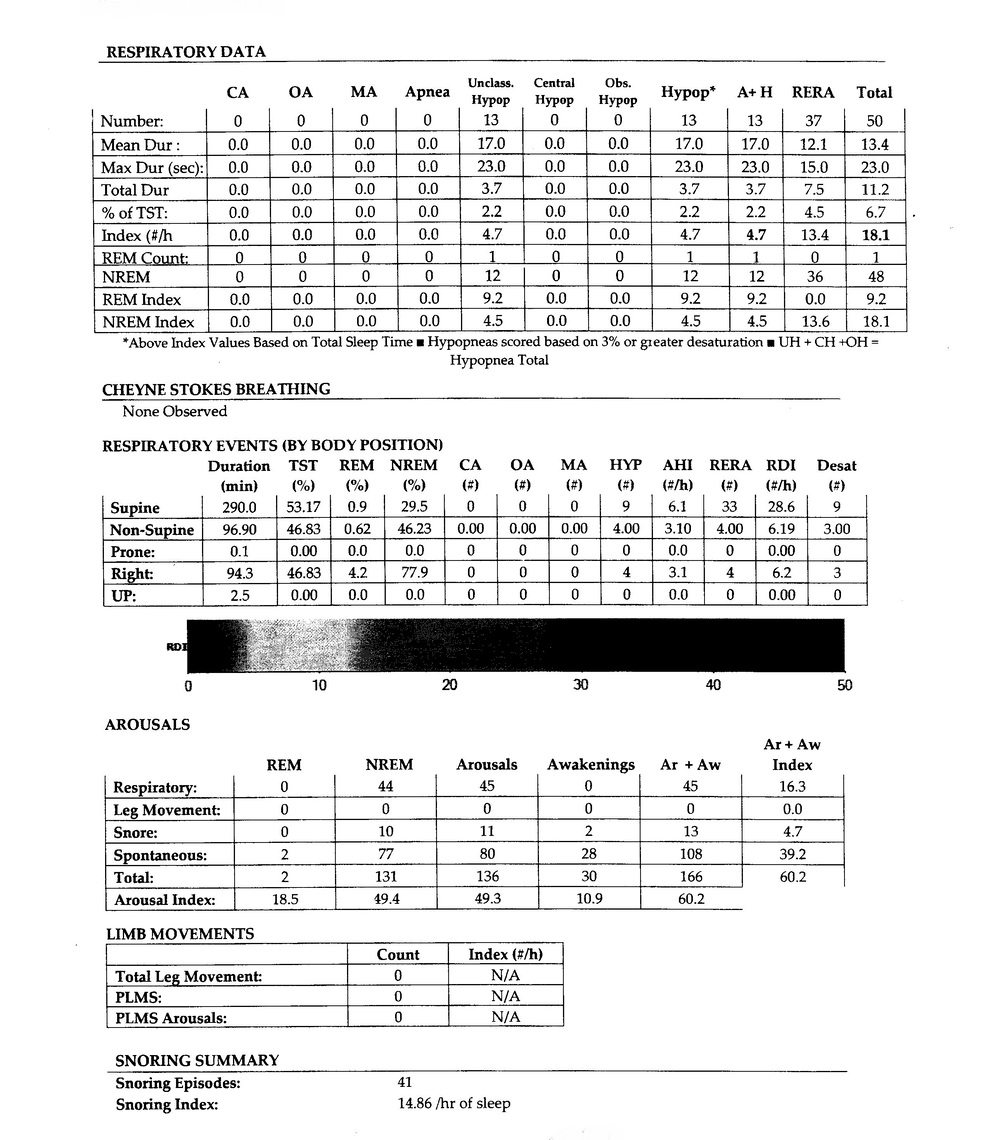
I am not a medical professional, and know little about the issues you have identified, other than the apnea part. Based on your previous thread and reported outcome of a sleep study I recall you had a diagnoses AHI of 4.7 which is just short of the Mild apnea classification based on API. However, I also recall you had some significant RERA events for an overall RDI of 18. In the province in Canada where I am, RDI is used equally with AHI, and you would be classed as having moderate apnea with a RDI of 18. Practice guidelines in this province would then offer a health care covered cost of a CPAP trial. A CPAP trial with an auto machine that records all types of apnea, hypopnea, and RERA would be very informative.
It is possible that the RERA events are a main cause of your sleepiness. They often do not cause the large O2 excursions and are not caught with O2 testing. Good CPAP machines however can detect them. They don't to my knowledge increase pressure based on them though.
The other consideration is that CPAP treatment can create apnea, especially of the central type, and the more pressure you use to treat obstructive apnea the more central apnea may increase. This condition is sometimes called Complex Sleep Apnea. Here is a good article on the subject of Complex Sleep Apnea written by Dr. Robert Thomas, M.D., Associate Professor of Neurology, Harvard Medical School and Beth Israel Deaconess Medical Center. It can also be found in the Blog section of this site.
When you get your insurance coverage back, I would do another sleep test, and if it confirms an RDI in the 18 range again, then push for a CPAP trial. The machine I would recommend is the ResMed AirSense 10 AutoSet. It will record the data you need to see, and it can be viewed in SleepyHead, so you can come to your own conclusion as well as get one from the Sleep Clinic.
Hope that helps some,
Have you tried seeing a Neurologist and or had EEG done? I suffered for years complaining how tired I was and had jerks as well. After a long time I went and had an EEG done and come to find out I was having Silent Seizures. Meaning I don't thrash.
Saw one. She said I was normal. EEG of apparently three different types was done during the sleep study.
Least you can rule out seizures Hope you find out soon what's causing your health issues
Not so sure that I can just yet...maybe not seizures specifically, but something weird is going on with my body neurologically and is mixed with other sleep apnea-like symptoms. If I had a full night of sleep, those numbers would likely be considerably higher.
What kind of treatment did you get for your silent seizures? I do feel "less jumpy" when I sleep better/longer to make up for the arousals, but I still had the odd jumps and jerks throughout the day with no rhyme or reason when doing daily tasks. My physical therapist noticed them when I was getting treated for my tibial torsion (leg bones are twisted outwards, causing me to toe-out a bit more than normal when walking). She wanted me to get it checked and noted my higher than normal pulse rate when exercising. Not to mention I fainted on the table during a blood draw at a clinic for about 15 minutes at the beginning of the year. Never fainted from needles or a blood draw. I was exhausted, walking 5-6 miles at work, had not eaten much that morning, skipped lunch and went to the doctor and that happened. They spilled the blood all over me and I woke up with my left arm numb from the blood pressure cuff and I felt tingly all over. Blood pressure was 60/60 and 52bpm on the monitor in front of me. The doctor literally tried to refer me to a psychiatrist to get meds for "anxiety" to suppress those symptoms, then argued with the nurses about my vitals while I was basically halfway dead. So I didn't get any answers from that episode. I had never had that happen and it seemed to be from pure exhaustion.
Went to my doctor and got another blood draw a day or two later and not so much as a fainting spell, so there are some weird things going on with my body that they haven't figured out. There was a little speculation that my lack of sleep in younger years could have caused the minor tibial torsion due to lack of proper rest for the bones and muscles to develop properly. The surgeon said no to surgery and told me to deal with it and that I'd have aches and pains in various areas of my knees and legs for life. So they 'weren't sure' if lack of sleep contributed to it. Poor sleep for half of my life has definitely taken its toll on me. I'm so ready to get that next sleep study.
I posted the results from the sleep study, but I don't know what all of them mean. My sleep doctor was a bit of a quack and said he had sleep issues, himself. So I wasn't that confident in that whole process and my next sleep study will be at a "better" clinic (this one was in a sketchy area of town with odd staff, a complacent sleep doctor and the whole test seemed sort of skewed).
I had a look at your sleep report. The basic data you covered with a post in your other thread pretty much covers the results. Some comments:
I am assuming you are located in the US? I found this undated article from what appears to be a US sleep clinic which covers the issue of diagnosis using RDI vs AHI. My short read of it is that Medicare are playing a dirty trick and while they use the term RDI, they exclude RERA events, which makes it essential the same as ADI. And worse still it appears virtually all insurance company follow Medicare rules and ignore RERA. Your insurance company may be different, but it would seem most likely they will not pay for a CPAP unless you meet the AHI criteria. They should pay for a sleep study however.
At What Severity Will Insurance Cover CPAP for Sleep Apnea?
That brings up another question you could ask a prospective sleep clinic you are considering for a study. Do they use Medicare guidelines or American Academy of Sleep Medicine (AASM) guidelines (which include RERA events). If they use AASM that would significantly improve your odds of getting a positive diagnosis and a prescription for a CPAP. You will need a prescription for a new machine even if you pay for it yourself. A used machine may not need a prescription though. Not sure. That article includes a link on where to get a CPAP machine at low cost. One of them is SecondWindCPAP. I believe they are a reputable place to buy from new at a fairly good price, or used. One thing to watch for is that the machine captures detailed data, distinguishes between central and obstructive apnea, and identifies RERA events. The safe bets are the ResMed and Respironics (DreamStation) Auto machines, (ResMed preferred).
I recall I told you before that all your current data suggests you may not benefit from a CPAP. Now that I see the RERA issue more clearly, I have to change my mind. I think it is quite possible that the RERA and hypopnea events may be disturbing you sleep to a significant degree. Just my thoughts, and again I am not a medical professional. Just giving my opinion!
Is there any correlation between taking melatonin and test interference, I wonder? I'll be using a couple of 3mg tablets next time to make myself be sleepy and try to get a full night of sleep so that they can see exactly what is going on. Most people associate sleep with being good and feeling wonderful, but I hate it because it makes me feel so bad. I can only assume that based on the data of 2.75 hours of sleep that my numbers for all of that might be almost triple that if I would have gotten 8 hours. So that sounds more like 120-150 "breathing events" since they noted 50 of them separately from the 13 hypopneas in the 2.75 hours. That would theoretically mean almost 3 times as mean hypopneas during a full night, as well. However, the old sleep study in March was before the deviated septum/turbinate surgery, so my breathing won't be as noisy as before. They noted a lot of snoring.
I'm not 100% sure that I can rule out anything neurological at this point. I have seen videos of people who have central sleep apnea and how frequently they wake up. I have seen videos of people with OSA. But then the multiple rapid-fire jumps/jerks this morning of my head/body that jolted me awake was a bit disturbing. It was like a hypnic jerk 4 or 5 times in a row instead of the single that I am used to once or twice a month. I've never had any issue with seizures or anything like that.
I have never seen any issues raised with the use of melatonin, other that it is questionable whether or not it helps sleep at all. Ambien may be of help and apparently some doctors prescribe it for a sleep test. The consensus seems to be that it does not adversely impact central apnea, but some disagree in that view. You may want to ask your doctor about it.
Keep in mind that AHI and RDI are events per hour, so if you sleep three times as long, and three times the number of events occur, the index numbers remain the same.
You may want to do a little research on Upper Airway Resistance Syndrome or UARS. It is essentially a RERA condition. Here is one link to an Overview, Symptoms, and Treatment, but there may be many other better ones.
From what you have described of your symptoms I suspect you may be suffering from UARS or Upper Airway Resistance Syndrome. This is not a medical opinion, but just a matching of your symptoms with those of UARS. It does not account for the "jerk" issues you seem to have, but it does pretty much describe many of the other factors in your case; younger, not overweight, unrested and unable to sleep, low AHI under the apnea diagnosis level of 5 (just), frequent hypopnea and RERA events, and no full apnea events.
Here are some articles to read. My conclusion skim reading them is that the condition exists, not all doctors know about it or consider it controversial, and the fact it is not recognized by Medicare, and most insurance companies, it most often goes untreated. CPAP treatment using a nasal or nasal pillow mask seems to be effective in treating it, but compliance is an issue, in many cases because insurance companies or Medicare refuse to cover the costs. Dental devices and surgery are also options, but I recall you have been down that road already.
So here are some links in order of depth they go into the issue:
My thoughts would be to try and find a sleep lab that is well aware of the UARS issue, and is willing and able to test and diagnose it, as well as OSA and CSA. And you would want a clinic that is willing to write a prescription for it -- such as a CPAP and nasal mask. But, you probably need to be prepared to cover the cost of the CPAP equipment yourself, unless you get a positive sleep apnea diagnosis based on AHI alone.
"Dental devices and surgery are also options, but I recall you have been down that road already."
Yep, had the sinus surgery and that did improve the breathing, but not the sleeping apart from the fact that I don't breathe as loudly when I sleep and it doesn't take as long to get a breath in or out. There is a "sleep apnea" surgery aka UVVV (Uvulopalatopharyngoplasty) where they scrape away tissue from the throat and/or remodel it. Very dangerous surgery and usually doesn't help much, if at all. A coworker's husband had it and nearly bled to death after his stitches in his throat popped loose. My brother had something similar happen to him where the stitches popped loose, as well. Dental devices...they seem to cause even worse TMJ for a lot of people and also they definitely move teeth to the point of making them crooked for a lot of people. I've had a ton of dental work in the past, so I don't want to mess all of that up.
I'll start researching sleep labs around my area and figure out which ones can check for UARS. There is some kind of test that some sleep clinics can do to check the strength of your esophagus/airway using a tube. They cram a tube down your throat and do some sort of pressure test or something like that. I saw a video where a little girl had that done before her actual sleep test and they stuck a tube so many times into her throat that it started bleeding and they abandoned the test.
I'm also wondering if a nasal pillow mask would try to deviate my septum again due to the pressure of something in my nose pushing on it. I think one side of the incision is still healing even though the surgery was in July and the ENT doc that I have seen a number of times after the surgery said that's pretty normal and it can take up to a year to heal completely.
The invasive test you talk about may be called Esophageal Pressure Measurement. On a quick check I think it is essentially putting a pressure measurement device down you airway so they can measure the pressure drop in the airway (airway resistance). Sounds a bit rough, and for that reason very few labs do it.
Here is a link to an article that proposes an alternate way to diagnose UARS. It is quite simple. They just use a standard CPAP titration test. That is the test that is normally done when you have been diagnosed with sleep apnea and they want to find out what pressure your CPAP needs to be set at. It is quite necessary for a fixed pressure CPAP, and not so necessary for an auto machine. Their postulation was that if the auto titration came back with a pressure of no more than 4 cm, then you do not have UARS. It it is higher then you have it, and you also know what pressure is needed to treat it. Not real hi tech, but it sounds like it works. In the study group they tried it on, which was already pre screened to be candidates that most likely had UARS and no apnea, the average pressure from titration was 7 cm.
The practical problem remains however that unless you are diagnosed with apnea (AHI >5) from the sleep test, they are not going to want to pay for a titration test. Catch 22. And if you are forced to pay for the test, then it is probably cheaper to just by the CPAP machine and test yourself...
I recently stumbled onto a ResMed paper on their AutoSet for Her algorithm. Interestingly it has been designed to address a number of factors including that women typically suffer less from obstructive apnea, and more from upper airway resistance. As a result this mode has been optimized for those differences. It would seem to me if you go down the APAP road this model could offer some significant benefits for someone suffering from UARS, regardless of sex. The machine still has the standard AutoSet mode available for use, it you find out the For Her mode does not work for you, or you eventually need more pressure. The only permanent downside to the For Her version might be the appearance of the box, if that bothers you.
Obstructive Sleep Apnea in Women: Specific Issues and Interventions
Would the long-term health effects of UARS be similar to that of someone with mild sleep apnea? I'm quite certain that I've dealt with this since before I was a teenager. My sleep was always awful, I always wanted to stay up late and had trouble going to bed earlier, had trouble focusing in latter elementary school and high school. The school work didn't make sense. Some of the stuff at jobs didn't make sense sometimes, but I would make myself get good enough at it that it was like second nature so that I wouldn't mess up as much or at all. Even if I ride as a passenger in a car, within minutes I'll get sleepy from the bumps and such on the road. I have ridden on 15-20 minute trips before with a relative and literally went to sleep in the passenger seat and they'd tell me to wake up when we got home. I would just get so sleepy that I couldn't help it. I fall asleep in front of my computer at home. My sensitivities to sounds (pages flipping, watching people perform tasks, relaxing sounds, etc.) seem much higher than everyone that I have come across. Yet I don't think I have anything like Narcolepsy. My cognition for driving a vehicle definitely isn't there enough, however, even though I can operate 40-foot industrial machines at work with no problem during the day. This also puzzles me. Exercising - stuff like pushups - causes my entire body to shake rapidly. I have been unable to find the source of this. I suspect that my general light "shakes" that I've had since I was a kid may just be benign tremors, but the violent shakes when exercising seems to be like chasing the wind. I don't see other people having that when they work out. I'm starting to wonder if I haven't damaged something in my brain or neurologically due to lack of sleep over all of these years. :-/
A quote from the link below.
"UARS patients present different features than other Sleep related Breathing Disorder (SRBD) [6,7,8]. The most frequent symptoms are excessive daytime sleepiness, fatigue and sleep fragmentation. However, UARS patients also present significantly more often with sleep-onset and sleep-maintenance insomnia, postural hypotension, headaches, gastroesophageal reflux, irritable bowel syndrome, anxiety and alpha-delta sleep [9,10,11]."
If I called and convinced my sleep doctor from the previous sleep study to give me a CPAP prescription or trial based on the 18 RDI...would this essentially solve the UARS problem or would it possibly be questionable? Seems like it would be uncomfortable trying to sleep on my side or stomach with a hose on my nose. I see that they make pillows with cutouts on each side for this. I would want the nasal pillows and ResMed Auto. I'll probably just end up buying at machine in December or January sometime, whether a trial is available with my current results or not.