So I tried to take a nap, lying supine, yesterday evening and had a flurry of centrals and never was able to fall asleep. Last night I chose to make every effort to stay on my side or stomach and it was a very different story. Here are some screenshots to look at. So far, it seems the machine is wiping out the hypopneas I had in my PSG, with very little pressure, and that my centrals are truly positional. I now know what is causing me to wake up feeling slightly anxious and to have a bit of trouble falling back to sleep...central apneas.
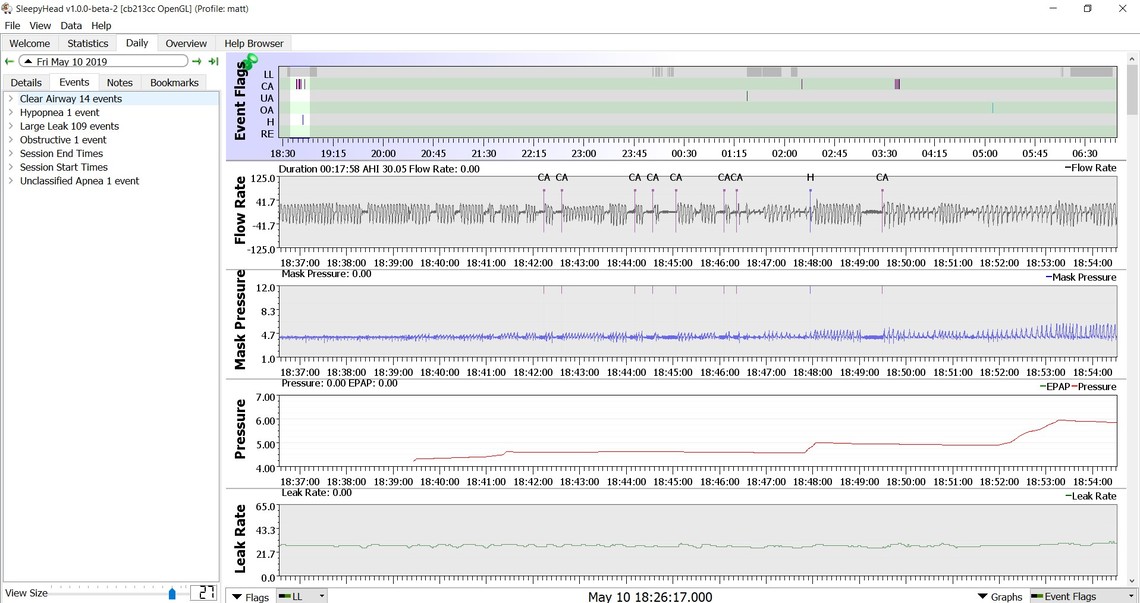

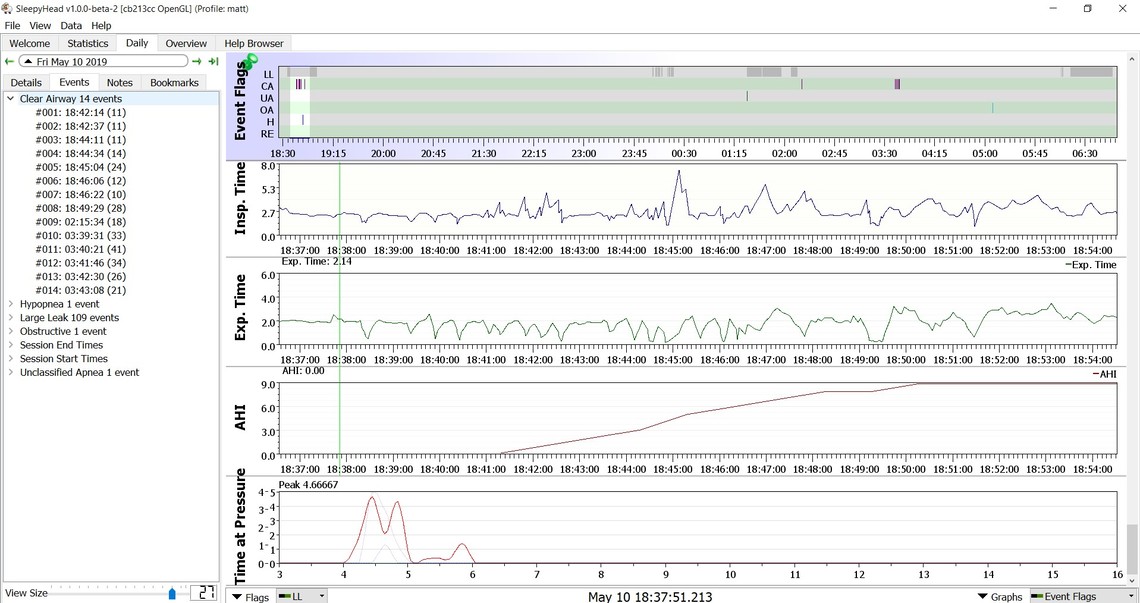
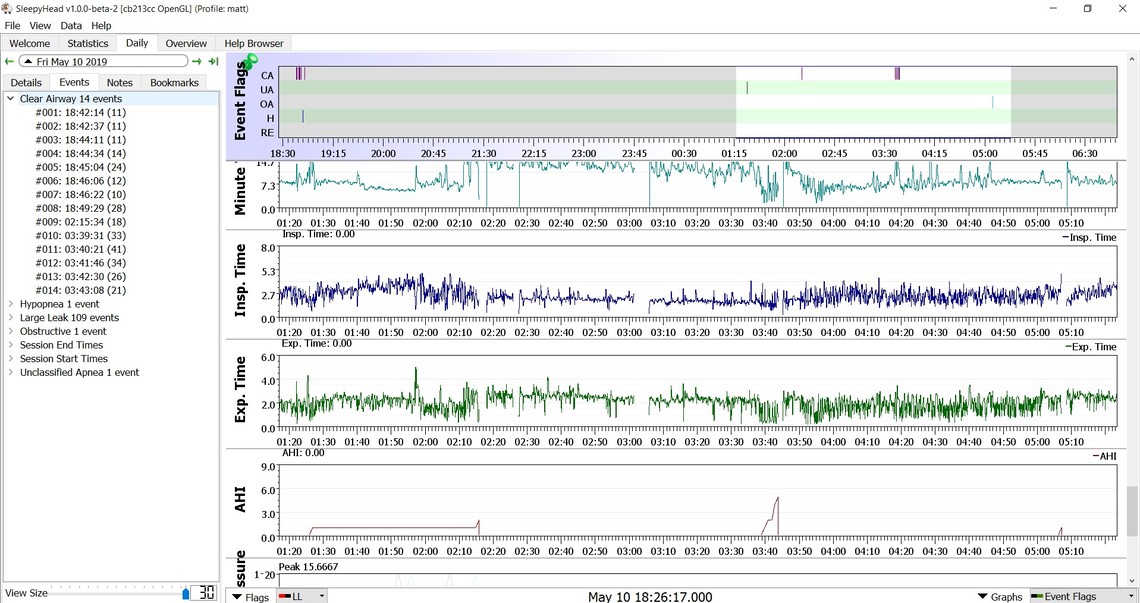
I'm not sure if these are even loading correctly as I can't see them when I sign off. Anyway, my AHI seems ok at 2.17. The time in apnea might be an issue at 4+ minutes. There are leak issues with the mask it seems, though they don't seem to be impacting my AHI. In contrast to my in lab sleep study, it seems like the apap is removing most all of the hypopneas and leaving me with the centrals, which I guess is to be expected. Any thoughts?
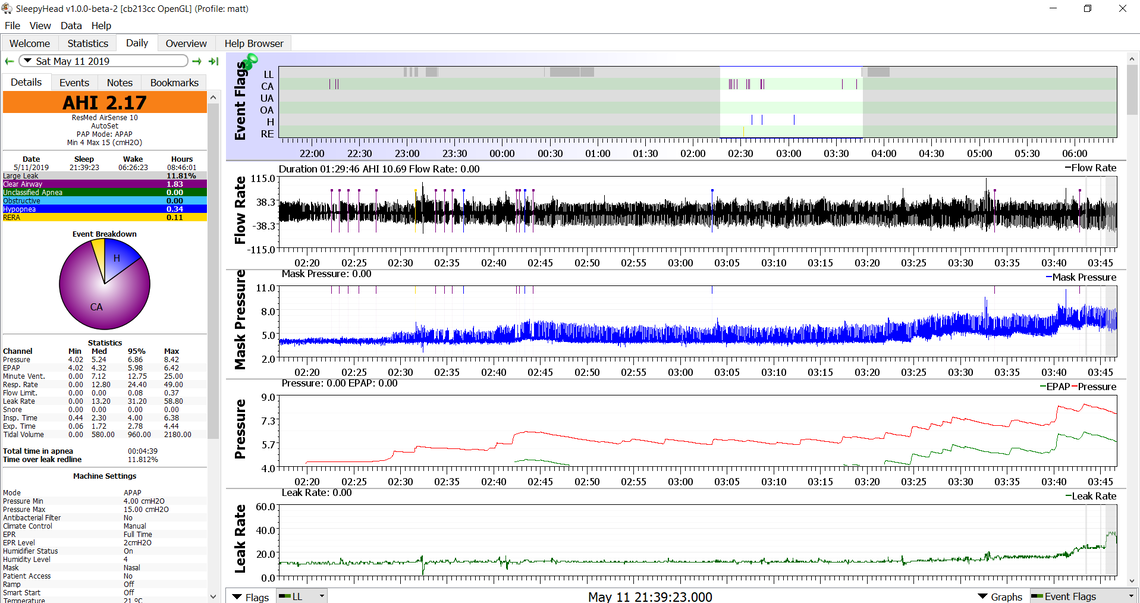
My initial thoughts would be to increase the minimum pressure to 5 cm and turn off the EPR or set it to zero. It would seem even low pressures are causing your centrals to increase. Turning EPR off should reduce the pressure required to stop the hypopnea or obstructive events. You could even leave minimum pressure at 4 cm if you find it comfortable to sleep with a pressure that low, but still turn off the EPR.
Thanks for the information about the spam filter and the machine advice.
I’ll ask about EPR adjustments tomorrow with the respiratory therapist.
I am a bit concerned about the positional nature of the centrals. I’ve read where it’s often about Cheyne Stokes respiration, heart failure or possibly some sort of brain stem problem. While I need to get these centrals minimized as much as possible, I’m thinking it might be equally important to try and determine the cause. It just seems odd that positional centrals would be idiopathic.
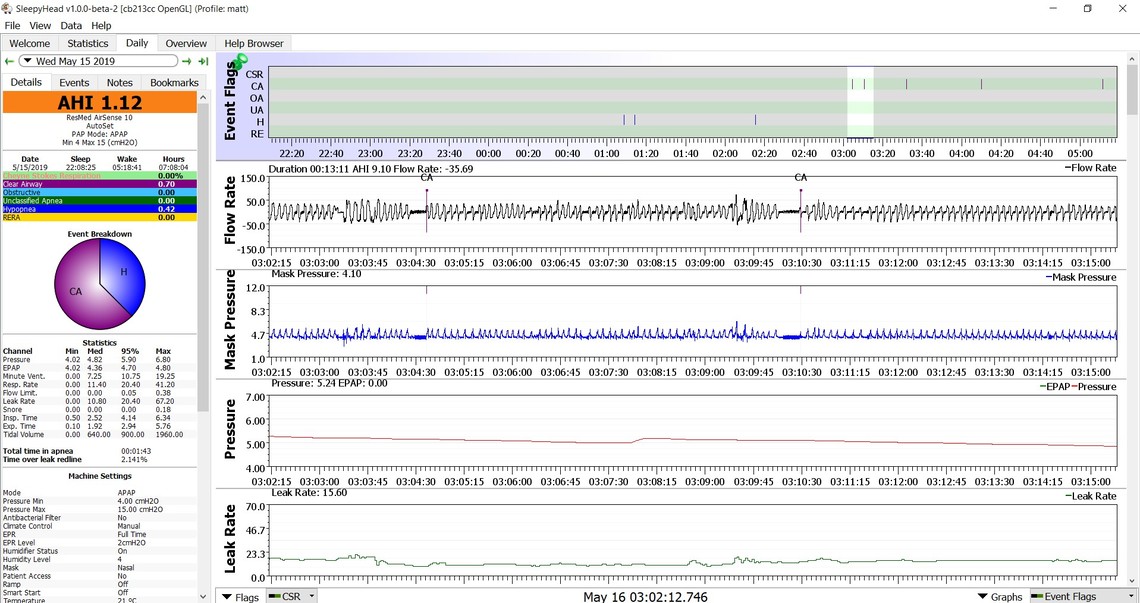
If you can post a zoomed in report of those centrals there might be more to be learned. It seems the machine does not think that it is Cheyne Stokes or they would be highlighted in green. However if they are very regular and repetitive then it is a bit suspicious.
The problem with leaving the EPR on is that you can get hypopnea and obstructive events on the exhale part of the breathing cycle. The only way for the machine to respond to that in auto is for it to increase the inhale pressure. So with EPR turned on you can get the worst of the worst. The higher inhale pressure causes more central apnea, while the lower exhale pressure can cause more hypopnea. It is better to turn it off. Or if you need it for comfort in going to sleep set it to be on in the ramp only.
Another thing to ask about is the maximum pressure setting for your machine. What I have found is that my AirSense 10 tends to chase the hypopnea events with more pressure. My feeling is that some, or even most of the hypopnea events are central in nature, not obstructive. So what you end up with is the machine chasing central hypopnea events with more pressure, and that pressure causes even more central events. So what you should ask about is significantly reducing the 15 cm max pressure to something much lower -- perhaps as low as 7 cm or so.
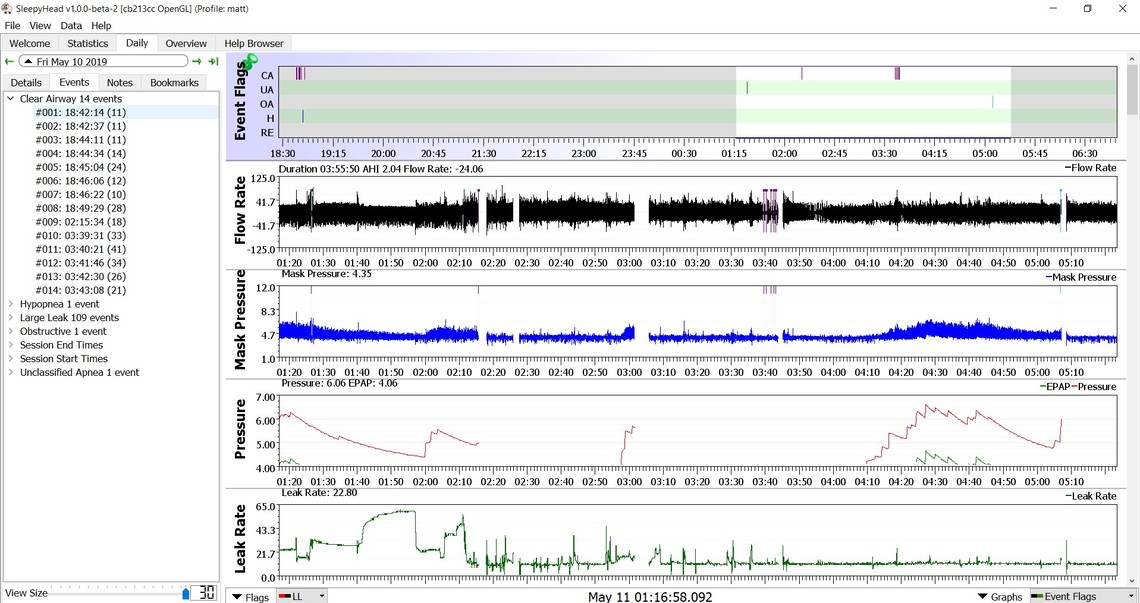
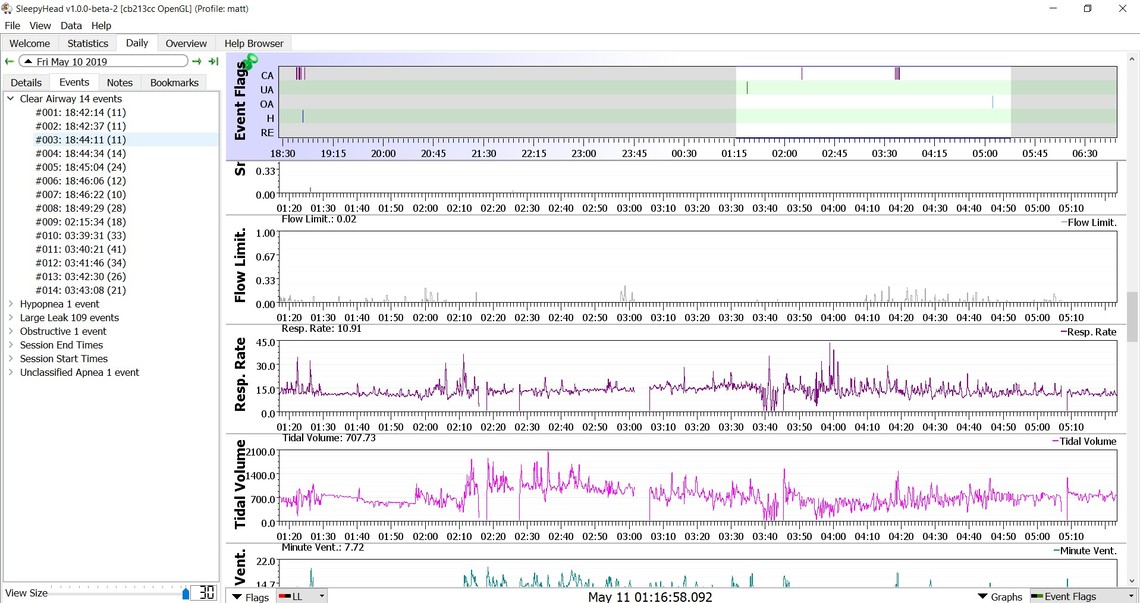
Here's a zoom. And now I'm showing CSR! This just keeps getting better and better.
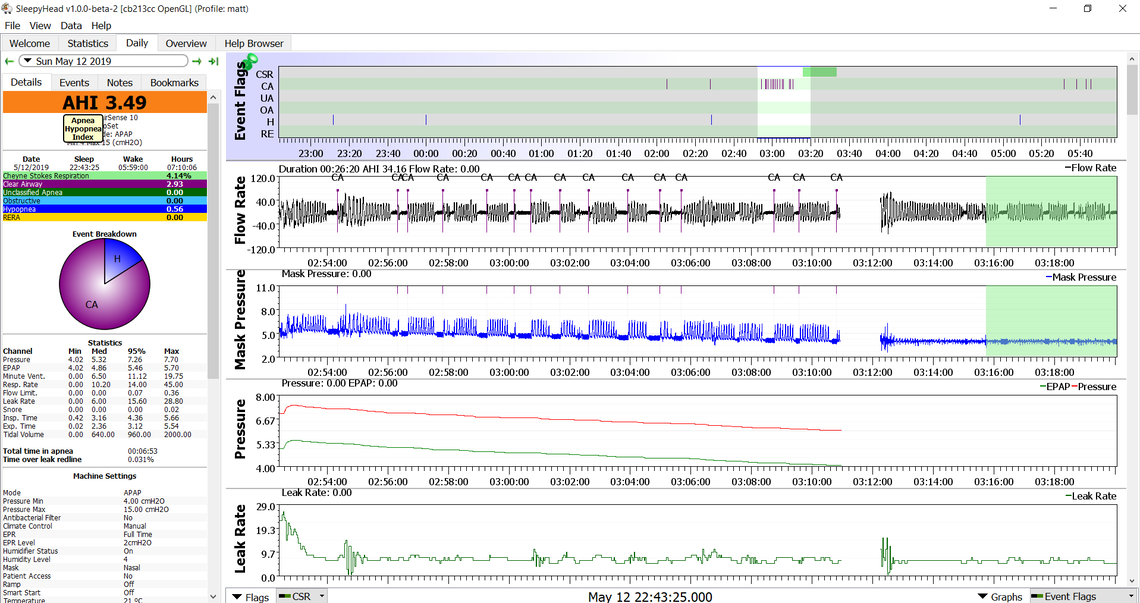
That is quite different CA events compared to what I see for myself. Also that area highlighted in green for CSR does not look like classic CSR. Here is what I saw in mine a few nights ago. The first few events are typical for me.
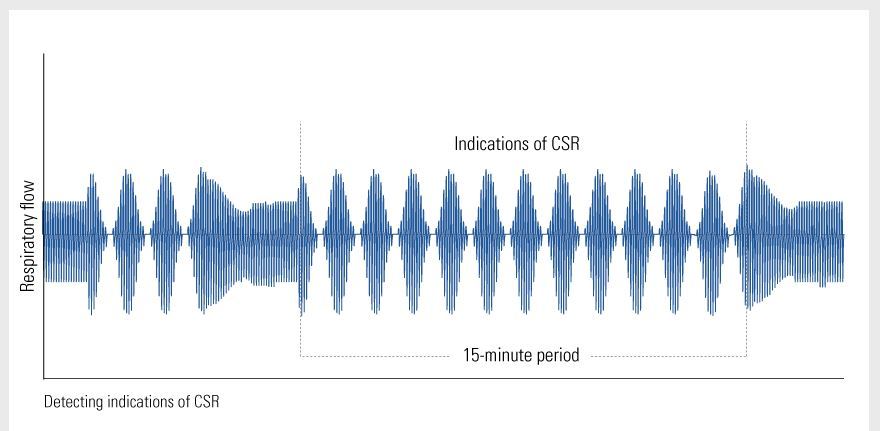
Here is what ResMed has shown as an example.
You probably should discuss these events and what is showing up in SleepyHead with your doctor. Keep in mind that to some degree these events could be caused by your APAP pressure. But, that said, there is some reason why such a small amount of pressure is causing CA.
I do plan to get in touch with my doc today.
With respect to the CA, I’m not sure that the APAP is causing them. I had 18 of them in my in lab study along with 28 hypopneas. So perhaps the APAP is wiping out hypopneas with little pressure and the CA’s are just hanging around for some underlying and mysterious reason.
Central Apneas tend to increase with increased pressure, or with increased pressure variance. It is not uncommon for one who has Centrals, and not enough to justify an ASV machine (which is designed to treat Central Apnea) to end up on a fixed pressure. Keep in mind that your current machine cannot treat Central Apnea, the auto algorithm will do nothing when a central is detected. Centrals are "treated" by avoiding them.
Treat your CSR indication as Periodic Breathing. While CSR is Periodic Breathing your pattern is not that typical of CSR. That said your Periodic Breathing should be brought up with your doctor.
Looking closer, my CSR flagged area looks like my CA flags, just slightly shorter and not enough to be called an apnea.
Might I be one of these persons with Centrals that aren’t enough to justify an ASV? Could my machine be set to a fixed pressure and do a home titration? Start at 4 and work up, see if it’s effective?
The standard treatment goal is to have 5 or less for an AHI in North America. So if your centrals are always pushing you over, then you may need to consider an ASV in my opinion.
In the UK for example they do not consider mild apnea (5-15) serious enough to treat with a CPAP, so it is kind of a grey area.
Last night was my best night thus far. 5 CA and 3 Hypopneas. I've been below 5 since the 2nd night with most nights being 2's or 3's. I'm curious why the centrals are going away when my machine isn't really capable of treating them. It leads me to believe that the CA was being brought about by hypopneas and awakenings.
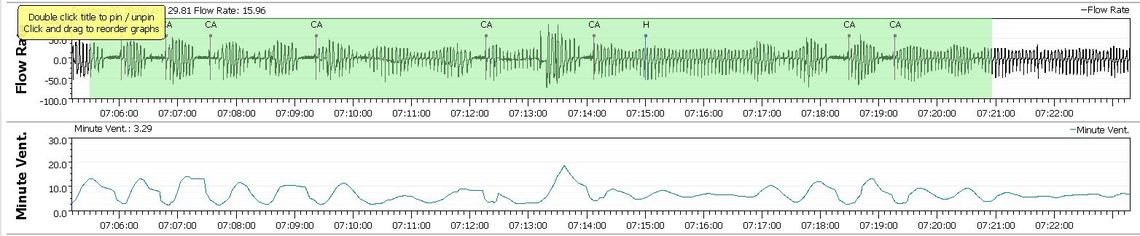
One of my personal theories based on my central apnea is that an obstructive event or possibly an obstructive hypopnea can start a cycle of waxing and waning breathing that can end up as a central apnea. You can explore that by checking the around what happens before a CA. In the graph above I don't see any events close to the CA events, so they may have occurred just due to arousals as you suspect. If my theory is correct, then a CPAP can to some degree reduce CA events by preventing the hypopnea or OA events that may trigger the unstable breathing. I find that dragging the Minute Ventilation graph up on screen lets me see when the waxing and waning of breathing starts relative to the Flow Rate graph.
My thoughts on where you are now, would be to increase minimum pressure to 5 cm and reduce the maximum pressure to 7 cm. This will get your pressure up to 5 cm right away and perhaps avoid some hypopnea or OA, and as a result avoid the CA's. Reducing the max pressure to 7 will keep the machine from chasing hypopnea events and increasing the pressure too much and causing CA's. In the end you may be best switching to a fixed pressure CPAP mode and set the pressure somewhere in the range of 5-6 cm. That may be high enough to stop any obstructive hypopnea and not high enough to create CA events.
Another possibility is that with CPAP you are breathing better, and your arterial CO2 drops triggering a Central Apnea. The setpoint at which Centrals are triggered changes with sleep and over time your body adjusts and fewer centrals are triggered. Better breathing actually can wash out more CO2 resulting in the failure to trigger a breath.
It sounds like you might be one of the ones where your centrals disappear or greatly dimish with time.
My AHI is now regularly below 1 with some nights occasionally between 1 and 2. However, I still feel like garbage when I wake up and feel groggy for much of the day. Almost like I’m dealing with sleep inertia that won’t subside. Interestingly on nights when I just don’t sleep well I tend to feel better in the morning. On Tuesday night I was up until nearly midnight and was out of bed before 6AM, a full 2 hours less sleep than usual and I woke up a lot that night. Somehow I felt better on Wednesday after that short night of sleep than usual. I do have a lot of awakenings at night, probably close to 8 if I had to guess. I’m not up for long but it’s an interruption. I’ve started taking melatonin, 1.5mg, for last few nights to see if that helps. So far it hasn’t. Thoughts?