Sorry, I posted in other topic and should have started a new one
Great forum, thanks. My home study showed AHI of 31, just in the "severe" range. Over 10 months, using SleepyHead for data, I was never able to get my average AHI below 10, trying every mask and a range of settings in the process. I just had surgery to correct my deviated septum, and can now breathe thru my nose, for the first time. But this has thrown my CPAP treatment off. Where I used to get my best results with max pressure set to 18 (I would have gone to 20 but could not stop mask leaks), post surgery it was difficult for me to exhale, even at 14. I tried using EPR = 1, but started getting irregular heart beats, indicating distress. My PCP told me to stop using CPAP until a new, in lab sleep test is done in 6 weeks. I have had to figure out things on my own, with help from a friend in the US, and from a friend in Amsterdam. My Pulmonologist was not helpful, and I will get a new one in two weeks. It's been almost a year! Thanks for listening.
As I responded in the other thread what is your ratio of central apnea to obstructive apnea? Central apnea is a very different problem and CPAP pressure alone does not help, and usually makes it worse. EPR while you are sleeping is most often not helpful. It tends to increase the pressure needed to treat obstructive apnea. I use EPR during ramp only, when I am still awake.
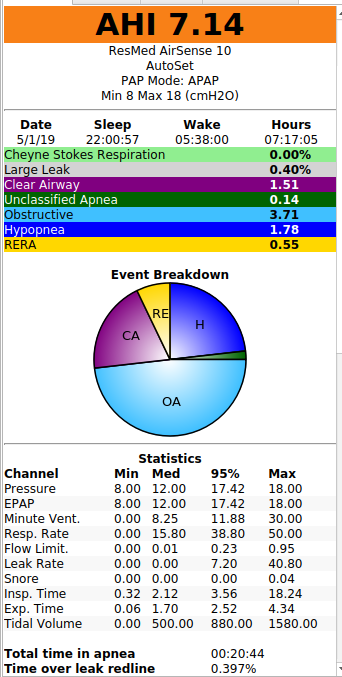
Here's a better one, from the day before surgery.
It would be much better if you could post a complete screenshot of the Daily report screen. It would be helpful to know when and at what pressure you are having the obstructive apnea, and the same for central apnea. These numbers suggest there is no EPR used. Pressure and EPAP seem identical.
That May 1 daily report indicated that you were getting your obstructive apnea events in very close succession right after going to sleep. Some report that when they get bursts of obstructive apnea it can be a sleeping position thing, and get some relief from it by using a cervical collar to keep their head aligned. In your case since it was before surgery it may have been related to your medical condition.
The interesting part is that after those bursts of obstructive apnea you had virtually none for most of the night with the pressure relatively low. That part of the night would suggest you only needed about 10-12 cm of pressure.
There is a bit of central apnea near morning. It did not seem as far as I could see to be related to higher pressure. Sometimes when we are waking up there is an effect called sleep wake junk which can get mistaken as central events by the machine. It may be a bit of that.
When you post a daily report like that it helps to use the orange "Write a Reply" button at the bottom of the screen. That will give you a full page width to display the graph.
Thanks! Your comments are very helpful! I used the machine last night with max pressure set to 12 and no EPR. I had data from less than 5 hours because I pulled the mask off, without knowing it. Average AHI was greater than 28 with one spike to 50, while both pressure and mask pressure stayed pegged at 12 most of the 5 hours, so tonight, I am going to set max pressure to 14 and compare the results.
Over my months of using the machine pre-surgery, that was the pattern I saw, with best results at 18. 20 was not possible due to leakage, which is why I requested a titration lab study to see if Bi-Pap might be better for me, and an oral device evaluation. The oral device is being made, and the titration study is in 5 weeks. I'll let you know how tonight goes.
last night:
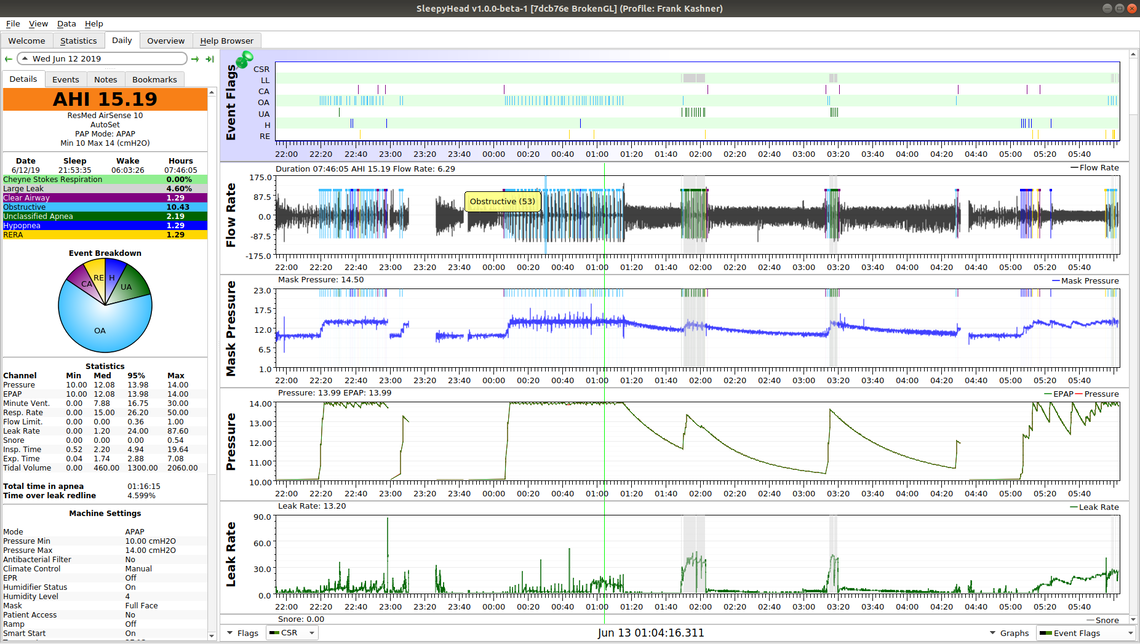
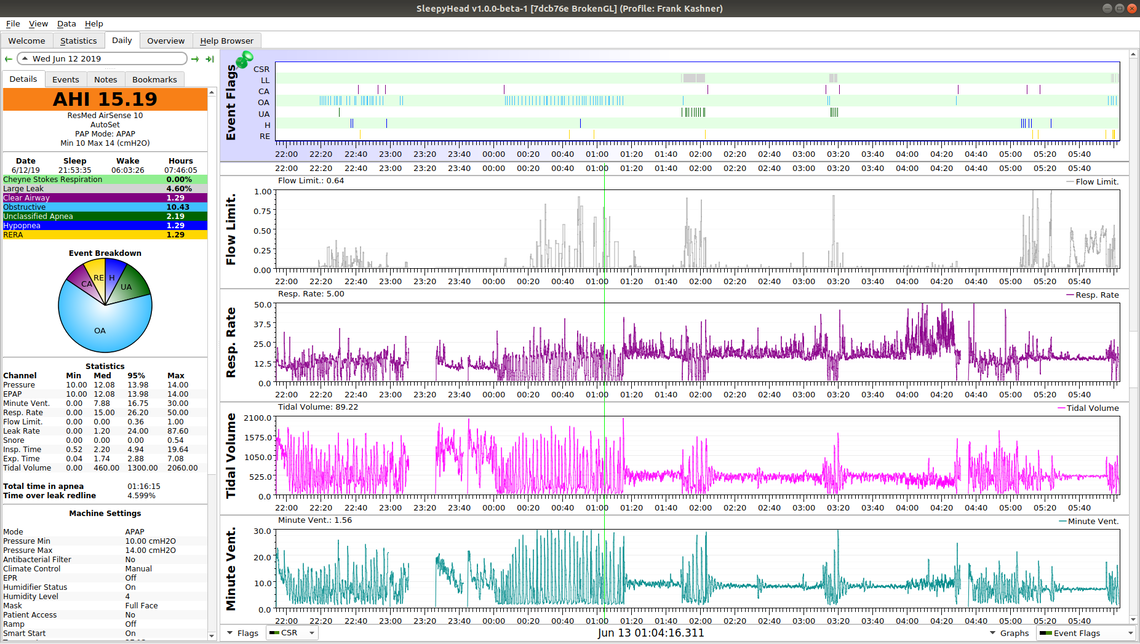
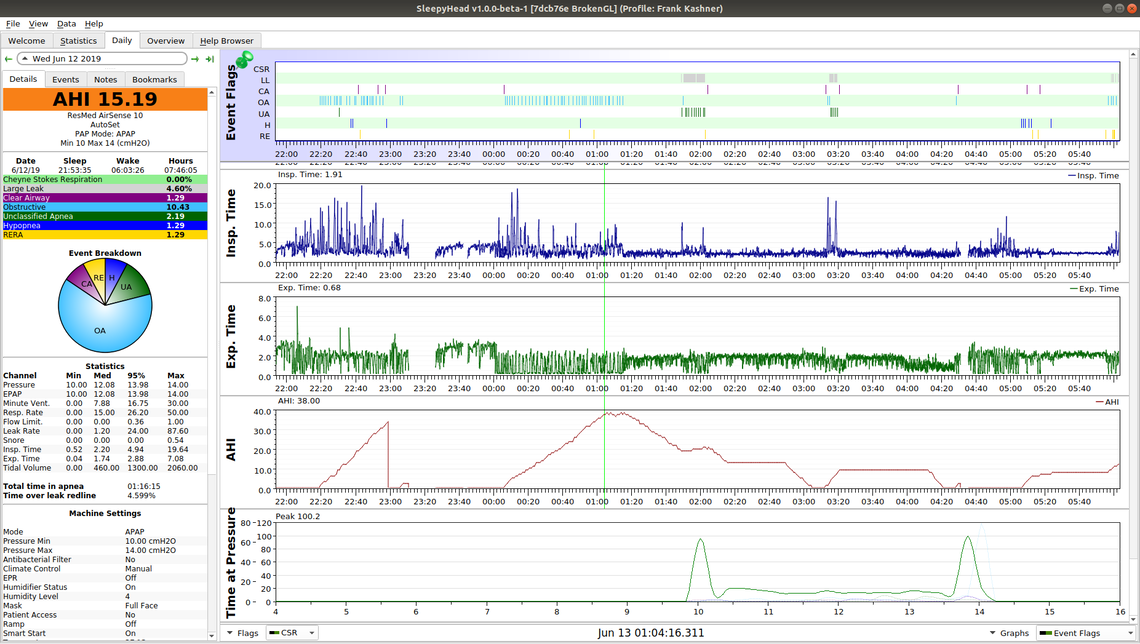
You really need to see a sleep apnea specialist doctor. About all I can say is that central apnea is there, but is far from your main problem. It would seem you may need a BiPAP machine to deal with the obstructive apnea, but I do not have the experience to make that suggestion. The CPAP does not seem to be causing your issues, but, it is not helping a lot either.
See how the obstructive apneas are clustered. This is in all of your charts, some early when they may be SWJ but others not. This pattern usually indicates a positional apnea caused by your chin tucking and restricting the airway. The best way to resolve this is via either an anti-snoring collar (Dr Dakota is popular) or a loose fitting soft cervical collar (ReLeaf is popular). I would like to see the results from this before I suggest other changes.
Here is a wiki article where the user decreased there AHI dramatically with a collar.
http://www.apneaboard.com/wiki/index.php?title=Optimizing_therapy#Positional_Apnea