Now that I'll be starting my treatment within just a few days from now, I'm curious what other people's reactions and experiences have been. I'll be on ResMed APAP (Air Sense 10 Autoset) using the P10 nasal pillow mask to start out with.
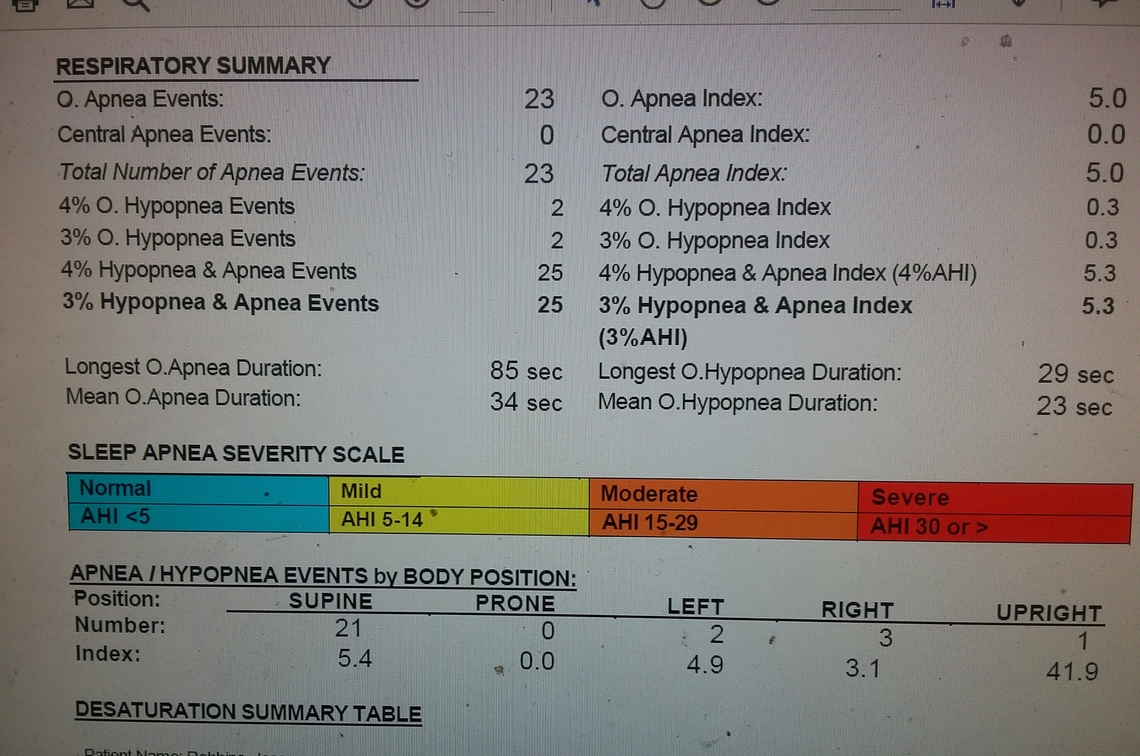
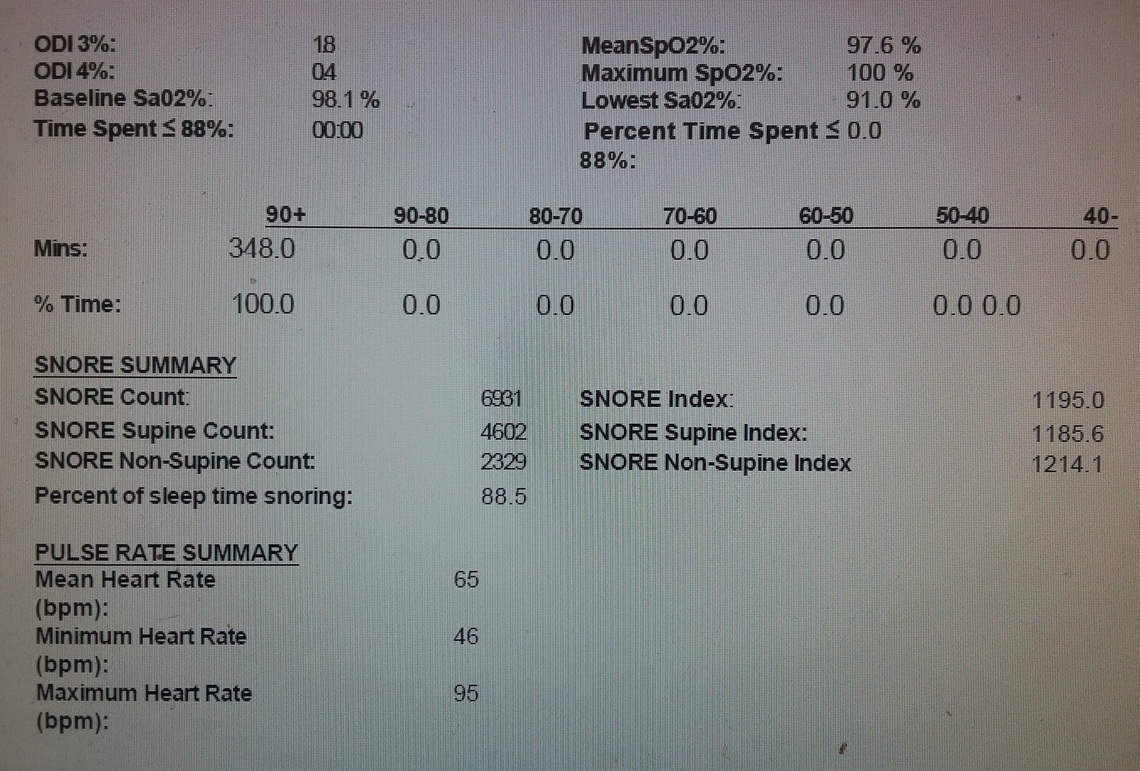
Between my in-lab sleep study and in-home study, I'm somewhere around upper 4ish to 5ish AHI. In-lab study also showed an RDI of 18. Not a lot as far as AHI, but I'm also one of the people who my ENT doctor referred to as the mild sleep apnea hitting very hard. I was told that some people are a 10AHI or higher and they don't feel that tired. Others like me are a 5 or more and feel awful every day. I walk around feeling like I could just lie down and take a nap after 8-10 hours of sleep. I never feel rested in the morning no matter how much I sleep. Riding as a passenger in a vehicle or sitting at home in my computer, watching TV on the couch, etc...I could fall asleep within minutes doing any of those. My cognition and attention suffers.
What did your APAP feel like when you first started using it? I know that it can be set to ramp up higher after you go to sleep. Does it feel like just some air blowing into your nose or what? Any feelings of panic? When I stand like a foot in front of a typical stand fan, I feel a "panic" that I think is caused by the air flow being misdirected/disrupted in my nose. Apparently this is common for people who let the windows down in a vehicle and stick their face into the wind. I read that it had something to do with the wind interrupting the air flow and making it circulate somewhere in the nose. Does APAP feeling like this?
I suppose I would sum it all up in asking: what exactly is the singular thing that makes it most difficult to get used to? The feeling of air being blown into the nasal passages? I don't really get claustrophobic in general. I know that some people feel that from the mask around their face from what I've read. What else?
I have never really liked using a snorkel mask. It always seems like it is restricting my air flow more than I like. When I first started using a APAP I was quite apprehensive. My machine was probably not set up as well as it should, and certainly not the way I would set it up today.
The main mistake that many new users make, and many professionals that set up machine is to start with a pressure that is too low. Out of the box the machine is set up to deliver a minimum of 4 cm of pressure, and a maximum of 20 cm. Many just get handed the machine and told to go for it. The reality is that 4 cm of pressure is too low, and for the majority of people it will feel like the mask is restricting the air flow (like the snorkel mask feeling).
What one really needs to do is get comfortable with the mask while sitting up and watching TV or something. After you feel reasonably comfortable then increase the minimum pressure 1 cm at a time and breathe in deeply. At some point it will start to feel like there is no restriction at all when you breathe in. That is a good minimum start pressure to use if it is reasonable -- probably in the 6-8 cm range. The second most important thing is to turn the Expiratory Pressure Relief (EPR) on and set it at 3 cm. This will reduce the pressure on exhale by up to 3 cm. It cannot reduce it below the 4 cm minimum of the machine. So for example if your minimum start pressure is 7 cm, it will reduce to 4 cm on each exhale and then increase to 7 cm on each inhale. Most find that very comfortable with it easy to inhale and exhale. The third step is to set the EPR to be on only during the Ramp because that reduction to 4 cm during sleep can promote apnea, which in turn will initiate a pressure increase by the machine. The automatic set pressure can be kept lowest if the EPR is automatically shut off when you are sleeping. Last the Ramp type should be set to Automatic. This way the 7 cm and 4 cm pressure cycling will be held at those pressures until the machine decides you are asleep. Then it will increase the pressure to the minimum automatic set pressure point (if it is higher than 7 cm). Reduction of the pressure on exhale will stop.
When set up this way, I find the mask very comfortable for going to sleep. It feels like you are wearing no mask at all, from an airflow and pressure point of view. Before I set it up that way, it was not so comfortable and I got frustrated when trying to go to sleep. Another trick is to use the user menu to start the humidifier prewarming about 15 minutes before you go to bed. This warms up the water so you will get the set humidity right from the start. Not essential but more comfortable.
An important point is not to put the mask on and jump into bed the first night. Spend some time with the mask during the day while watching TV or reading and just make friends with the mask. Adjust it until it is comfortable fitting and not leaking.
Hope that helps some. If you want a checklist in order of the items in the setup menu let me know, and I will give you my suggestions.
I have a slightly different take. If you are susceptible to Central Apneas as Sierra is he is dead on. I'll point out that most people are not that susceptible to Centrals. That said, based on your symptoms I would watch your daily charts, especially the makeup of your AHI, what events are contributing, how much to your AHI closely since Central events could easily be why the Mild Apnea is hitting you hard.
Mask choice is the single hardest thing to get down simply because all of us are different. While you are picking up your machine ask to try several different masks, preferably relaxed and lying down in your sleeping position because your facial "structure will change when you lie down and relax (sleep). Here is a link to a "Mask Primer" I put together [http://www.apneaboard.com/wiki/index.php?title=Mask_Primer]
On EPR I do not shy away from it until I see signs of increasing Central events from it. With ResMed Min Pressure should be set to 4 + EPR.
If EPR =2 Min Pressure should not be lower than Machine min + EPR = 4 + 2 = 6
If EPR =3 Min Pressure should not be lower than Machine min + EPR = 4 + 3 = 7
Lacking other info I like to start at Min Pressure = 6, EPR=2 (middle of the range) Full Time. If Centrals are an issue I'd back off the EPR.
A setting of 4-20 is a sure sign that your treatment needs to be optimized, or at least verified.
Actually my suggestions have nothing to do with central apnea. The purpose of discontinuing EPR during sleep is to reduce the frequency of obstructive apnea. They are as likely to occur during exhale or the inhale/exhale transition, so using EPR reduces the effectiveness of the pressure which is preventing obstructive apnea. The reduced pressure also improves comfort.
And you do not have to do any calculations at to where to set EPR. Just set it at 3 cm. The machine will not go below 4 cm in any case. It self adjusts.
EPAP is what manages OSA. By applying a little math when applying EPR you can preserve the effectiveness the EPAP was providing for the OSA or accurately adjust it in the direction it is needed. Just lowering EPR is a measure I frequently take to manage Central events. I always look at EPAP when managing Obstructive, thus when I add EPR and simultaneously increase the min pressure I never impact the efficacy of that portion of the treatment.
My apologies for thinking you were doing something for Centrals.
It is far simpler to cut to the chase and just turn EPR off when sleeping. No math needed. There is a reason that ResMed has that option to do EPR on ramp only. When you are awake it makes sense, and when you are sleeping it does not. And there is a reason that F&P resisted offering an EPR setting until very recently with their last model.
I hope you are lucky, like me, and it is not difficult to get used to. I can't really feel the force of the air flowing in. But if I pull the mask off before shutting the machine down, the air is really whooshing out. My mild apnea also hit hard in terms of concentration and attention. The improvement there is remarkable.
In-lab and home sleep studies showed no central sleep apnea. Lots of hypopneas and apneas. I'm hoping the machine shows no centrals, as well.
I can't focus to drive, it takes people repeating stuff for me to comprehend it and that sort of thing. I get "jumps" in my core muscles when I make certain movements. I wake up in the morning with bright red lips as if the blood pressure in them is high and sometimes a slightly red face that I believe may be from fatigue. All doctors have been puzzled. Bright red lips go away as the day progresses (chap stick helps mask some of the brightness) and the redness in the face also goes away. I also tend to feel short of breath all day. I forget stuff quickly (numbers, etc.) sometimes.
Odd that I can have an 85 second apnea and yet not drop below 91% blood oxygen. My apneas and hypopneas seem to hit me interchangeably. Snore index was unreliable for that home test due to no true audio testing.
It is always a good sign to see no central apneas in the sleep study. It does not totally eliminate the possibility that you will have them when under CPAP pressure, but it sure improves the chances that they will not be a problem for you.
When do you get your machine? Will they set it up for you?
I placed the order yesterday. They dropped the ball and missed the shipping window because the doctor's office was a day later faxing the prescription over. So I'll get it sometime early next week. I have to set it up for myself.
I have noticed that sometimes in the middle of the night when I am just laying there (drifting, but awake), it is like my airway just shuts off or something. There are times when I feel "too tired to breathe" when I'm just sitting upright in my chair after a rough day.
I feel like I may get used to APAP more so than the typical person. I feel sure that I have had this for about 20 years and I remember cognitive struggles and the general "not rested" feeling all the way back to my early school days. Doctors never recommended a sleep study. I wouldn't have gotten one at all had I not pressed for my GP doctor to give me one back in 2018.
I'm curious what you all thrink about this hypothesis and your corresponding thoughts on pressure settings and EPR.
I have complex apnea and central events are my nightly wildcard. Looking at the data in Sleepyhead it appears to me that they tend to occur at sleep stage transitions, as if my neuro-chem breathing control bobbles the ball so to speak in picking up breathing responsibilities since I tend to see CAs, and often flurries of CAs, over relatively brief periods of the night, and especially as either: (1) I am initially drifting off to sleep; (2) trying to go back to sleep after awakening or getting up to use the bathroom; and (3) near the end of sleep 20 or 30 minutes before I awake for good. Thoughts?
It is not uncommon for there to be apnea events when you are just waking up or going back to sleep. Some call this Sleep Wake Junk and dismiss it as noise. The CPAP machines generally do not start counting apnea events until after the ramp period is over, and at least in theory you are asleep. This is to avoid reporting noise and inflating the AHI number. On the EPR I will see if I can find the existing thread on the subject and bring it back for discussion.
Edit: I found the thread on EPR but it is closed for comments. However, here it is. It should give you more views on EPR than you really want to hear!
https://myapnea.org/forum/not-understand-epr-setting/1#comment-17050
I can completely relate to the low AHI score, but feeling awful. I was an empty headed zombie driving my car. I knew something was up because it felt like every time I was on the verge of deep sleep something would nudge me awake, but I just thought it was anxiety. Finally, a sleep test confirmed mild apnea. I don't use CPAP; however. I am using a tap appliance at the moment and can say for sure you will notice a big difference using your machine. I was immediately more clear headed and less groggy. I am still adjusting the appliance to get the maximum benefit. That is the frustrating part. There's definitely an adjustment period that takes place over a few months. Getting used to a thing in your mouth or on your face and then "tweaking" it to your situation. There is a bit of trial and error. But, I can say I sleep much more consistently now. I look forward to bedtime. Also, I rarely get up to go to the bathroom anymore. I used to get up like 3 or 4 times. Crazy how this little plastic thing is changing my life.
I had few problems getting used to the airflow, but I dislike the feeling of wearing it. I have a nasal mask, and it gets sweaty at the seal. The mask also makes it difficult to sleep on my side, which was my preferred position. I'm now, after ~ 6 weeks, able to sleep on my back. I had severe apnea, and while the CPAP immediately reduced my AHI from mid-30s to 2.6 or so, I found the quality of my sleep worse. I used to never feel groggy, but once on CPAP I had to take naps all the time. I'm now more comfortable with it, and I think the quality of my sleep has improved immensely, to the point where I think it's better than it was before, and my daytime naps are down from ~2 hours to about 20 - 40 minutes. But, although I'm more used to the mask, I still find it uncomfortable, and often take it off after about 6 hours (needed for insurance purposes) and go back to sleep. That sleep, too feels better than it used to. I used to have apnea-like events (a snore - snort) even while awake; those went away literally as soon as I started using the machine. I think the pressure from the machine's airflow forced some of the tissues in my throat to retract or something.
Overall, I think the CPAP was good for me, but I'm doing everything I can, lose weight, exercise more, and so on, to get rid of it. I find it uncomfortable, and think I always will. But what I really dislike is the feeling that normal, primal functions -- breathing and sleeping -- are dependent on a machine. It's profoundly disturbing to me.
One of the things I have found helpful is to avoid if at all possible any daytime napping. I try to focus on getting 7-8 hours of continuous sleep at night in one stretch. For me, less than 7 hours is not good in the longer term, and more than 8 hours is not good either. I think when one sleeps too much the quality of sleep deteriorates.
At first I had trouble falling asleep with the mask on. After I started falling asleep, I had trouble staying asleep and would wake up an hour later an be unable to fall back asleep. Then I got more used to it and was able to fall back asleep and stay asleep longer. For me, the main message was that you have to be patient and not give up if it doesn't work great at first.