Hi Folks,
I ought to mention up-front that I'm in the UK and I get the impression that Sleep Apn(o)ea is better handled in the USA. Here in Old Blighty, I'm in need of additional help to that which is provided by the NHS.
I was diagnosed as having severe OSA just over a year ago. During that time, I have been using a Philips Respironics DreamStation. I also have an Amara View full-face mask. I use this gear every night. The User data from this machine is confusing. I have been using a Viatom VisualOxy wrist-worn pulse oximeter (whilst asleep) for a couple of months and I get a lot of oxygen desaturations. My ODI on 24 Oct, for example, was 5.7 and the lowest SpO2 was 80%. Average HR was 55 bpm. To test the oximeter, my wife tried it overnight a couple of days ago. Her ODI was a mere 0.3. She does not have sleep apn(o)ea.
For as long as I can remember (I'm now 66), I have had anxiety issues. For many years, it has been severe at times. I have an anxiety disorder diagnosis. I'm very concerned about the impact that my sleep is having on the anxiety. I should perhaps add that I stopped drinking alcohol almost exactly three years ago to the day. I was also diagnosed as having Types 2 diabetes about six weeks ago but I am getting that well under control with a low carbohydrate diet and frequent finger-prick blood glucose monitoring.
Would anyone care to comment?
Thanks in advance.
jaypeecee
I use SleepyHead to monitor my apnea treatment. OSCAR has replaced SleepyHead, and at least for now is pretty much the same. It requires a PC or Mac, and a SD card reader to get the data to your computer. Assuming it is the same as SleepyHead it accepts Oximetry data if your meter is supported. That would allow you to see that data along with your sleep data. That said I have never used an Oximeter and have just assumed O2 would drop during apnea events, and have just focused on minimizing apnea events. How is your AHI? The goal is to be below 5 and ideally around 1 or less.`
I have had diabetes for 20 years or so. I try to focus on a balanced diet, and then treat the diabetes to manage that diet. I currently take metformin and use insulin. My objective is to try and achieve an A1C of right around 6.
Hi Sierra,
You asked about my AHI. It varies considerably. For example, on 1 October (last month), AHI was 1.8 and, the next day (2 October), it was 14.1. My mask fit figures were 100% and 98%, respectively. Furthermore, for each of these days, total obstructive apneas was 4 and 62, respectively. That would indicate to me that something isn't right. My AHI is showing anything from 'Normal Sleep' to almost 'Moderate Sleep Apnea'. All data taken from Philips DreamMapper.
I would value your comments.
JPC
What is your breakdown of AHI into the CA, OA, and Hypopnea types? Central apnea can be erratic and harder to deal with. On the times when you have AHI in the 14 range, it would be helpful to know the breakdown to see how much of it is central apnea compared to obstructive. OSCAR will tell you this. All the historic data should be on your SD card, so you can go back and review specific days.
Hi Sierra,
Thanks for your reply.
This Philips DreamMapper app leaves a lot to be desired. It now jumps from 30 Sept to 2 Oct. I now have no data for 1 October but, fortunately, 2 Oct is still listed! To answer your question, the Total Clear Airway Apneas, Total Obstructive Apneas and Total Hypopneas are 5, 62 and 35, respectively. This was on 2 Oct when AHI was 14.1.
I have yet to try importing data from my SD card into OSCAR but I will try to do this within the next few days.
JPC
OK. That one set of numbers suggests obstructive apnea is the main issue that drove the AHI up. I suspect you would learn a lot from using OSCAR. It provides much more detailed data. And as long as your SD card was in your machine, it should all be on the card. Have you checked to see that there is a card. Some providers do a nasty trick and pull the card out of the machine.
Hi Sierra,
I am very grateful for all your valuable help - thank you!
Today, I imported data into OSCAR from my DreamStation SD card for the very first time. A few teething problems but then - Wow! - there it all was in glorious technicolour. What I hope to do is see if there is any correlation between this data and the data that I get from my Viatom VisualOxy pulse oximeter. This oximeter does not currently appear to be compatible with OSCAR. I do hope the developers of OSCAR have added my model to their to-do list. I now need to spend time familiarizing myself with OSCAR.
JPC
Hi Sierra and Everyone,
How do I determine what is causing such a large variation in AHI from 1.8 to 14.1? The problem seems to be obstructive apneas but isn't CPAP supposed to reduce/eliminate these? We're talking about an 8:1 variation. When I was last talking with one of the NHS physios, all he did was talk about the average AHI reading. That seems to 'paper over the cracks'. From my layman's perspective, it suggests that the Philips DreamStation isn't up to the job. Just thinking out loud but frustrated with the situation I find myself in.
JPC
It would be helpful if you posted a Daily Report screen from OSCAR. There are some things you should do first to clean up the default screen though, assuming OSCAR defaults are the same as SleepyHead. This assumes you are on a PC. Mac should be somewhat similar.
All these things use up valuable screen space. Make sure the Event Flags are pinned to the top. Click and drag the graph titles so the Pressure, Flow Rate and Leak Rate show.
Again on a PC the F12 key will save this screen shot as an image file. Just note in the popup where it is saving the file. Then when you navigated in Windows File Explorer and find the file, you can click and drag the file to the body of a post. Just make sure you start with a new post in the thread so you get a full width post.
If you post it here, I can give you my comments. It would be good to post a good day and a bad day.
Hi Sierra,
Here is data from 1 October 2019, which was a good night:
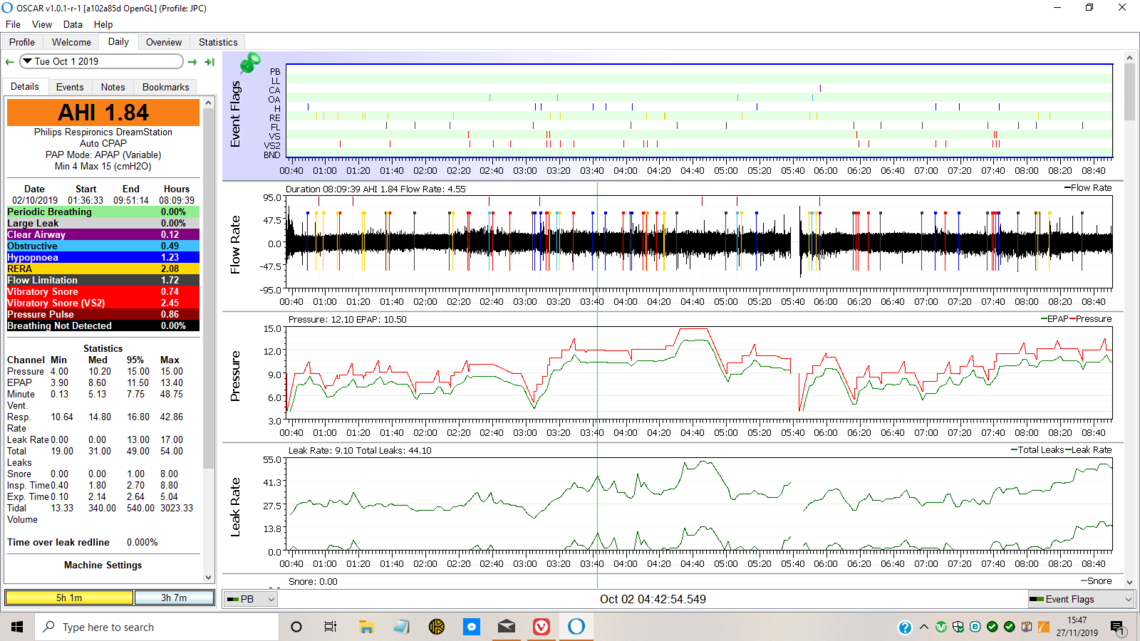
This is the easier one to comment on and suggest improvements. First I think your minimum pressure is too low and seems to be just set at the default minimum of 4 cm. I would suggest a minimum of about 10 cm. This may prevent a few of the obstructive, hypopnea, and RERA events which are occurring at a pressure of less than 10 cm. CA events are very low, so central apnea does not seem to be an issue. It appears you are using a ramp at the beginning of the night with the Ramp starting at 4 cm also. I would suggest setting the ramp start pressure a bit higher at about 7 cm. For most a little more pressure is more comfortable and less suffocating while going to sleep.
Hi Sierra,
Here is data from 2 October 2019, which was a bad night:
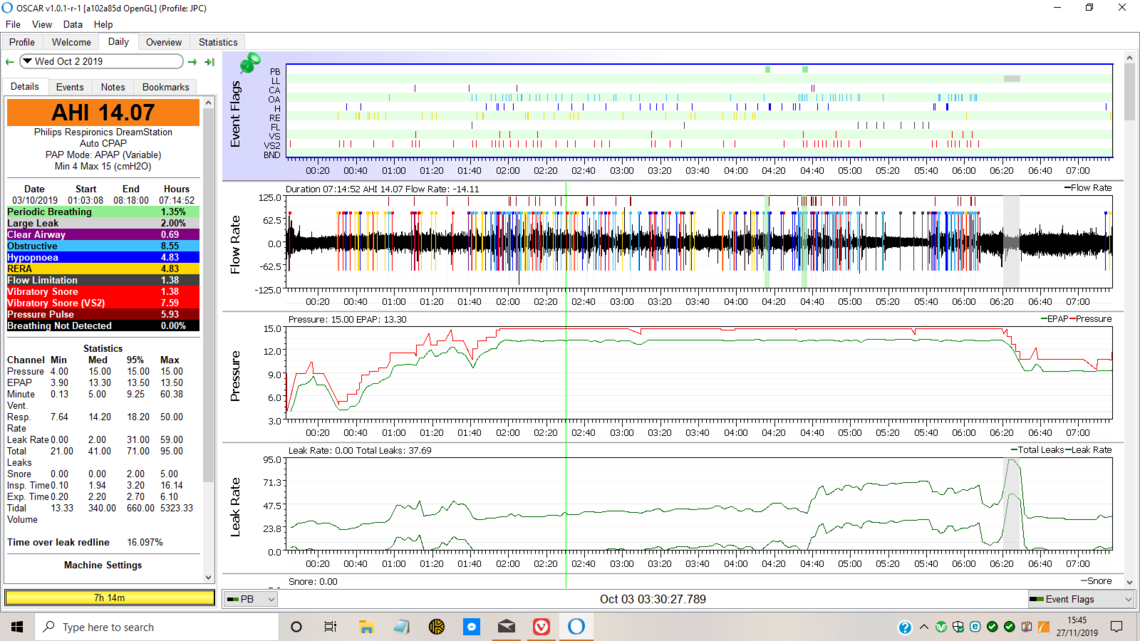
CA events are a little higher, but not much, and not concerning. The OA events are the main problem along with hypopnea. RERA is high too. The large majority of these events are occurring when the machine is maxed out on pressure at 15 cm. The obvious solution is to increase the maximum pressure to 16 or 17 to see what this does. The Machine Settings are not showing, but I'm guessing from the Pressure chart that you have Flex turned on and set at 2 cm? If you turned Flex off, you might gain a little without increasing the maximum pressure. I would try that first, and if you still get bad nights like this, then go to the higher maximum.
Some people seem to have trouble with positional apnea where they get their neck into a cramped position while sleeping which in turn promotes obstructive apnea. When this happens it can result in short periods with very high rate of apnea. Yours does not really look like that, as the rapid apnea events extend over a period of about 4 hours. But, you could keep that in mind. You can buy a soft cervical collar at places like Walmart for about $20 that some wear to keep their neck from getting into a cramped position. I have never tried it, but others report success with it.
That is about all I can think of for now; increase minimum pressure, turn Flex off, and if necessary increase the maximum pressure.
Hope that helps some,
Hi Sierra,
Wow - that was a quick reply. Thanks!
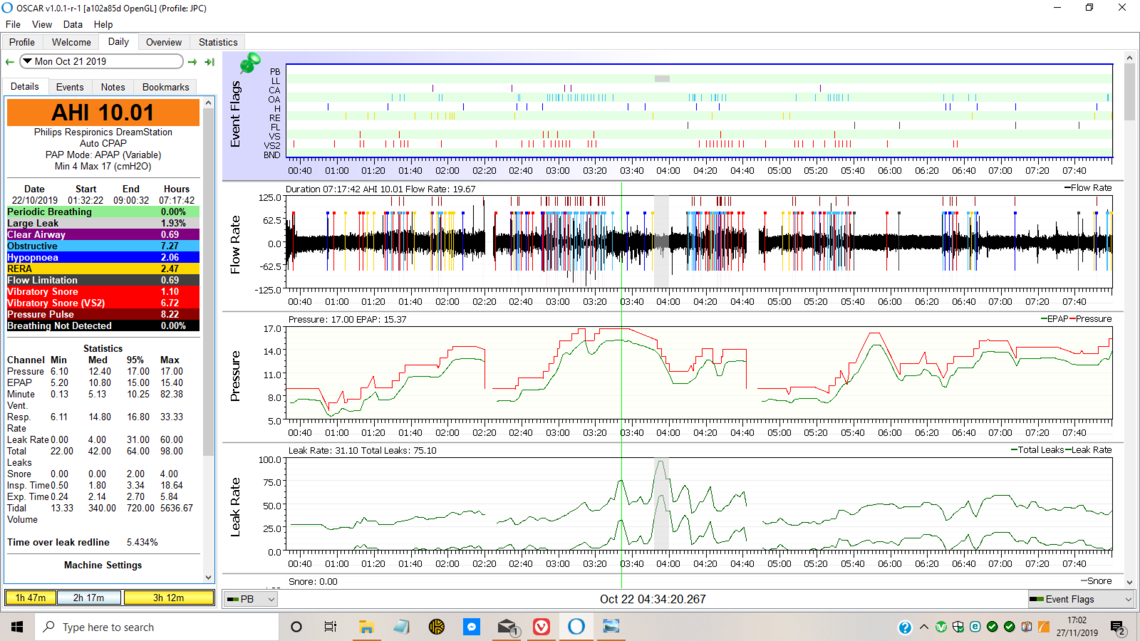
Firstly, the minimum pressure of 4.0 cmH2O. Although that is the machine setting, when I first switch the machine on at bedtime, it starts at around 9.5 cm H2O (as shown on the DreamStation display). Following a phone call to my physio on 10 October, the max. pressure was raised to 17.0 cm H2O at my request. Here is the OSCAR screenshot for 21 October when things were not too good:
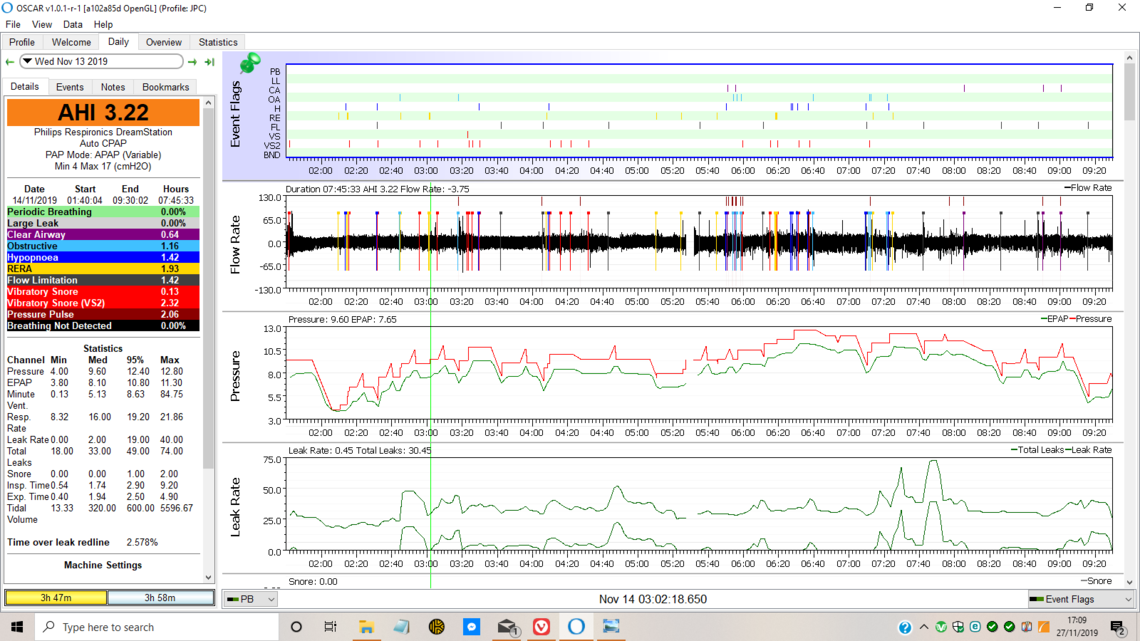
And here is another for 13 November when things were better:
I await your comments and am very grateful for your help.
JPC
Interesting. There is something strange about the starting pressure and minimum pressure. I am less familiar with DreamStation machines than I am with ResMed. On a ResMed you cannot set the Ramp Start pressure higher than the Minimum Pressure. It appears you can on your machine, as it looks like it start at 10 cm and then goes down to 4 cm when the Ramp is over. ResMed machines would not allow that. I wonder if someone tried to set the minimum at 10 cm, but changed the Ramp Start pressure instead of the Minimum pressure?
My suggestions remain the same. I would get your provider to change the Minimum Pressure from 4 cm to 10 cm. Then the pressure should never go less than 10 cm all night. Also same suggestion with the Flex. Turn it off. It reduces pressure on exhale, and you may be getting more obstructive apnea when exhaling at the lower pressure. When Flex is turned off the red and green pressure lines will be the same, not split. It may allow you to get away with a maximum pressure of 17 cm. It is still maxing out at 17 cm for short periods of time. Once you see how it works with a higher minimum, it may have to go higher still, perhaps as high as 14-15 cm. A Ramp Start pressure at 10 cm seems a little high, and you could set it lower at 7 cm or so, if that feels more comfortable.
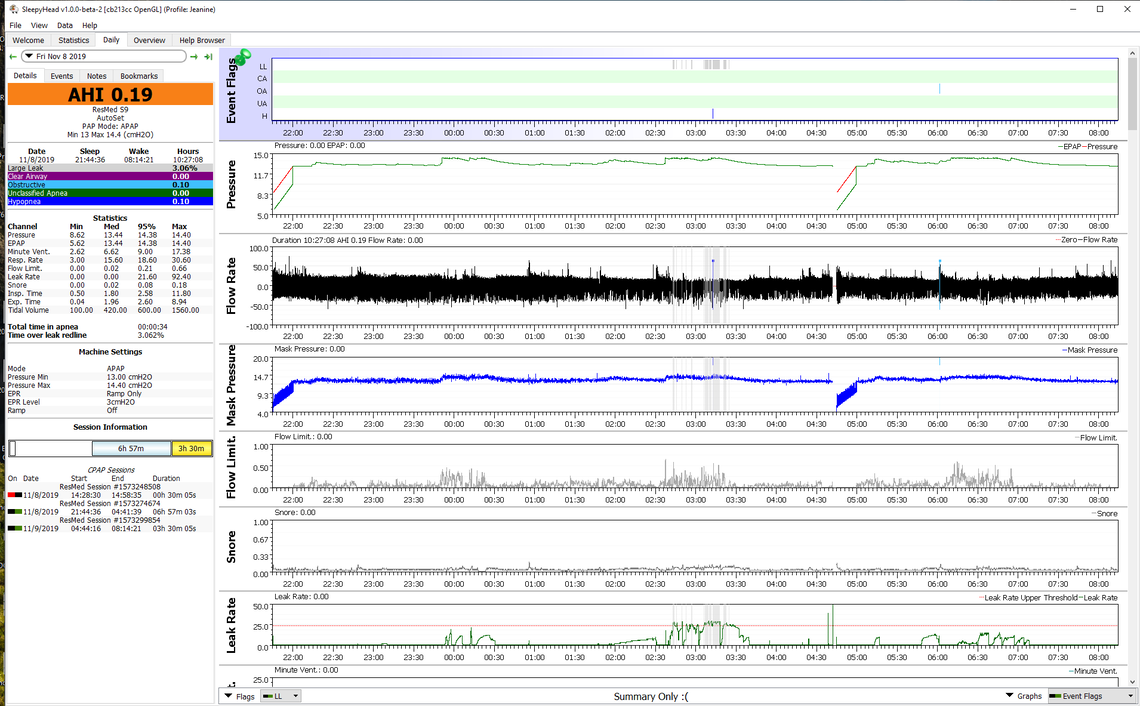
DreamStation machines behave a bit differently than ResMed when in Auto. The DreamStations like to ramp pressure down (if you allow it) to see if you get apnea, then it ramps it up again if you do. When your minimum pressure is set low like at 4 cm, it can cause extra OA events as it hunts around with pressure all night long. You can stop that by elevating the minimum pressure. When the pressures are set up well there is often a very narrow range between minimum and maximum pressure. My wife has a ResMed but she still has a narrow range with a minimum of 13 cm and maximum of 14.4 cm. She typically gets under 1 for AHI. Here is what a good night looks like for her. She was diagnosed with an AHI over 80. Note the narrow range between minimum and maximum pressure.