In 2018, I got a doctor referral for a sleep study, finally in my 30's. Unable to function, brain fog, waking up exhausted every day, etc. Had an in-lab sleep study that showed 4.7 AHI, 18 RDI with 50 events in 2.75 hours for the whole night. Sleep doc said I didn't have sleep apnea. No major drop in O2 levels below the low 90's. Couldn't get a CPAP. My ENT doc requested a CT scan of my sinuses. Deviated septum and enlarged turbinates. Got surgery for both and I breathe easier now, but still sleep poorly. Requested a home sleep study via mail order on my own a few months after surgery. 5.2 AHI. I got my ENT doc to write me a prescription for an Air Sense 10 Autoset and I've been trying to get that to work. I have it to 7.6 starting pressure and max of 10.4 in APAP mode, because it never goes above about 10.1 no matter how high I set the max. Anything below 7cm makes me feel suffocated.
3 ER visits December 2019 - January 2020. Racing heartbeat out of nowhere at night before bed, trembling/shaking all over, feeling like I couldn't breathe, feeling faint, so much adrenaline that I felt like I couldn't walk, etc. A few EKG's, tons of blood work at the hospital each time. Nothing. Blood pressure went up as high was 170/100. I'm a healthy and muscular caucasian male, 5'8 and 150 pounds. Never been overweight. No large neck. Nothing outward screams sleep apnea.
February 2020 - my family got a violent stomach bug. 3 members of the household. One had violent vomiting for a couple of days along with diarrhea. The two of us just got black diarrhea. I had it for days. After that, my stomach was killing me for weeks with burning and pain all night. Finally had an Upper Endoscopy (EGD) at the Gastroenterologist. He saw a red and inflamed stomach lining. They did biopsies and found no bacteria (like H. Pyloria) and no cancer. He put my on a PPI med for months and I eventually ended up on Nexium 40mg twice a day, which I've taken for like 5 months now.
I've been to two primary care doctors, a Cardiologist for a full Stress Echocardiogram with ultrasound of the heart before and after the treadmill walk. He said my heart is healthy. Wore a Holter monitor 24/7 for 31 days. They caught half of a second of arrythmia and it wasn't even during a time when I reported symptoms. He said he thinks it is my sleep issues. I have Dysautonomia that started 2-3 months ago. Dizziness in my head, tingling on the top and back of my head, my heart rate increases and decreases suddenly, I feel faint-like sometimes. Suspected Postural Orthostatic Tachycardia Syndrome or Dysautonomia. My new primary care doc put me on Fludrocortisone, a steroid, to try to help with the Dysautonomia. Hasn't helped much, if at all. I've been to an Endocrinologist to make sure it wasn't thyroid related, had all kinds of blood work done again, etc. Nothing.
Earlier in 2020, I found a new sleep doctor and got an exam. He went up my sinuses with the endoscope and said they're clear, but turbinates are again enlarged. Covid-19 was happening, so he sent me home with a sleep test. 13 apneas/hour. He said he didn't believe that and when he looked at my throat, he said I don't look like someone with Upper Airway Resistance Syndrome, either. Did an in-lab sleep study at his lab because he wanted to know that they're counting apneas correctly as 10 seconds or more. I had 64 apneas/hour and slept for half of the night. Went back for a titration sleep study last week. I brought my P10 nasal pillow mask and she said it did well. My sleep tech was actually the sleep lab manager and previously owned her own sleep lab. They use the OmniLab titration system. During the earlier part of the study, I felt like I was floating up to the ceiling and then it went away. I don't get that at home when I use CPAP. Not sure why I got it in the lab.
Outside while waiting on my ride the next morning, off the record she told me that she started me off on CPAP at 6cm. She kept upping it and later told me that it wasn't working for me, so she switched it to BiPap and it started working. She said she saw some central apneas, as well. I also get autonomic dysfunction with the dizziness, muscle weakness, feeling faint, etc. General Dysautonomia. I also tend to have throat tightness all day long on both sides of my throat and it feels like I can't breathe or like there is a lump or swelling or something. It has been like that for days and days, so I doubt it is anaphylactic. shock or anything. I have no known allergies to food, etc. I'm waiting on my next virtual sleep doc appointment next week to get results and see what is next as far as treatment. Don't have the results back yet from the in-lab titration study that found the centrals, but she said I "slept well" once on the BiPap, even though I felt like garbage that whole day. She also commented that the monitoring system in CPAP/BiPap machines is junk and PSG is about the only true way to tell if it is working.
I've been using CPAP on my own for about 6-8 months now. At this point, I don't know if I have Upper Airway Resistance Syndrome, Obstructive Sleep Apnea, Central Sleep Apnea or a mix of OSA/CSA and/or UARS. Some days I get just a few obstructive apneas showing up in OSCAR and maybe a few hypopneas with an AHI of 1.5 for an whole 8 hour night. Other days I might have 7 to 8 AHI, slept horribly, ripped the mask off after an hour or two, etc. I'll see mostly centrals in OSCAR, say 10 or so Centrals within under 2 hours and they're usually mixed with just a few hypopneas or obstructive apneas. Then I'll have other days with no Centrals and not many apneas/hypopneas under the exact same settings for no rhyme or reason. Lately, lots of Centrals has become the common theme.
How should this be approached from a diagnosis point of view? Try BiPap first to see if it works and then seek ASV? Curious why CPAP didn't work in the lab and BiPap did. She said she started at 6cm on CPAP and I guess kept upping it. Maybe it caused me to have a lot of centrals and get reduced oxygen for a short while? I had a floating up to the ceiling feeling I think while I was on CPAP in the lab and it went away when she went to BiPap after the saw the CPAP wasn't working. I don't get that floating feeling at home on CPAP, so that's odd.
Curiously, I have times when I wake up ahead of my heartbeat increasing. So my brain wakes up first, then my body about 10-15 seconds later and it feels scary as my heart "starts up" from a slow heartbeat to a more rapid heartbeat. As best as I understand it, most people with OSA wake up WITH a pounding heart, not with it starting after waking up. My brain wakes up first, then if I just lay there for 10-15 seconds or if I physically move my arm or something, my heartbeat will increase. I fall asleep on buses on the way home from work (30 minute ride tops), fall asleep in my chair in front of the computer, fall asleep in the passenger side of a car on a 20 minute trip across town to a store, etc. Sleepy all day. Sleep is not restful.
When I use the CPAP, I feel like I'm fighting myself breathing. When I don't use it, I'm obviously having lots of apneas on my back (like the 64 apneas/hour in lab), but but they claimed none on my side. I think the ones on my side may be Centrals. I have days when I feel irritated, hot all over, feel like the blood pressure is high in my face and hands, etc. I'm dizzy, my digestive system and bowels are all messed up (soft stools that come quickly with short notice and smell terribly).
As noted, next week is my doctor's appointment. I have a team of doctor's, so I'm not asking you to treat me. I'm asking for opinions, tips, anything helpful along this journey. Thoughts? :huh: I feel so bad that I can't even drive at all. My body doesn't want to work right sometimes. My muscles feel jumpy/jittery some days. I have trouble swallowing food and drinking liquids sometimes and not at other times. I get the pressure on both sides of my neck in the area where you check the pulse rate. When I check my blood pressure with an electronic monitor, the "irregular heartbeat" icon lights up even when the blood pressure and pulse rate are normal. As noted before, the Cardiologist found nothing in the Stress EKG or during the entire month of wearing a Holter monitor with 5 electrodes stuck to me 24/7 and looking for anything odd. My stomach/intestines "twitch" and feel like they are contracting a lot or something. There are times like right now when my heart is beating normally speed-wise, but I can see my entire stomach jumping lightly with each beat.
I'm attaching a couple of screenshots of OSCAR data from June 6 and June 10 to show the differences in what I'm dealing with. I had to do regular screenshot grabs because the F12 button in the program is capturing just a blank image. One day seems fine and the next I'm ripping my mask off after an hour or two and then putting it back on later and having a crazy amount of central apneas. Why would I have so many on one day and sleep terribly and then sleep 8+ hours on another day and not have as many?
Does this pretty much guarantee that I have both Central and Obstructive Sleep Apnea? What can I do to stop pulling off my P10 mask?
June 6 - https://i.ibb.co/PGw9swh/6-6-2020.jpg
June 10 - https://i.ibb.co/PhLM9st/6-10-2020.jpg
I am not a doctor and will restrict my comments to your two posted daily report screen shots.
June 6 - This one looks fairly normal and many, including myself would be quite happy with a result like this one. I tend to have more CA events than you had on this night. That said your ratio of CA to OA events is higher than normal. Most people have almost all OA events. The one change I would make is turn off the EPR except for ramp only. I would use the auto ramp function, set the start pressure at 7.4 cm, set the EPR at 3, but also set it to Ramp Only. When set that way you will get 7.4 on inhale and 4.4 on exhale until you fall asleep. That should be quite comfortable for going to sleep. Once you go to sleep the reduction on exhale will stop and the pressure will be the same as on inhale and vary according to what the machine thinks you need. There are two potential benefits in doing this. First it eliminates the low pressure on exhale which may be causing your OA events, and as a result of having the events, the machine is increasing pressure. The increased pressure may then be causing CA events. If the OA events are better controlled, then the machine will not have to increase the pressure as high. The pressure may not have to even go much above your minimum 7.4 cm.
June 10 - This one is not nearly as good. The first thing I would wonder is if you were actually asleep when having those CA events. They may be sleep wake junk, as some call it. You are waking up and going to sleep and in the process just holding your breath long enough to count as a CA event. You can get some idea what is going on by expanding the time scale to see the nature of the flow curve. If you move the minute ventilation graph up a bit you can compare to what it is doing. It seems during this time it is very erratic. Ideally it should be a flat smooth curve.
Both Charts - I cannot see any obvious benefit in having a BiPAP machine. You are no where close to needing 25 cm of pressure. You are also not going to be able to take advantage of the higher differential between IPAP and EPAP (pressure support) as you can't go lower than 4 cm, and look like you don't need more than 8-9 cm. With EPR turned off you will likely need even less for pressure. And if anything, using EPR in the sleep phase may be hurting you more than helping you.
Another option that might work for you is to put the machine in CPAP mode with a pressure of 7.4 cm, and with EPR on ramp only. It could work just as well or perhaps better than Auto mode.
Hope that helps some,
I do think that the APAP mode ramping up and down could wake me up, as it seems to do that for a lot of people.
I don't quite understand what it does in the settings when I set EPR to auto ramp while in CPAP fixed pressure mode as opposed to APAP mode. I know that EPR set to auto ramp in APAP mode will take away the EPR that you've set it at from whatever pressure it is ramping up to. What does it do in CPAP mode since it obviously won't be ramping? Just doesn't take any EPR off at all?
You currently do not appear to be using Auto Ramp at all. It does not really ramp the pressure up when going to sleep, it just holds it at the Ramp Start pressure that you set. When it detects you have gone to sleep it ends the ramp and give pressure control over to the machine in APAP mode, or if in CPAP mode it just goes to the set CPAP pressure. The other thing it allows you to do is to set the EPR Type to Ramp Only. That allows you to have EPR pressure reduction on exhale for comfort during the ramp period when you are not sleeping, but then have it turned off when you go to sleep. Here is an example of how I have mine set when using CPAP mode. But it is essentially the same in APAP mode.
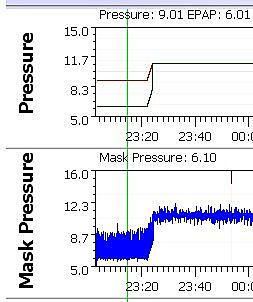
My specific settings are for a Ramp Start pressure of 9 cm. I have EPR set at 3 and the Type set to Ramp Only. What this does is give an inhale pressure of 9 cm (red line on graph) and exhale of 6 cm (green line). Then when the machine detects I am asleep it ramps pressure up to my set CPAP pressure of 11 cm, and at the same time stops the EPR pressure reduction on exhale.
The only difference between the CPAP and APAP mode is that in CPAP it stays at the set fixed pressure. In the APAP mode the pressure adjusts automatically between your min and max depending on what the machine is seeing.
I seem to respond quite terribly to EPR. Even taking it down to 2 from 3 has a significant impact on my exhale breathing and makes me feel like I'm laboring to exhale.
I tried fixed CPAP mode at 7.4 this morning. I've tried EPR set to Full-Time and Ramp Only for the EPR. Also tried 2 and 3 and both of them, in both Full-Time and Ramp Only modes, make me feel absolutely awful when exhaling. It feels like I'm suffocating. Makes it hard to sleep.
I don't think you are understanding what EPR and Auto Ramp is.
Both of your posted charts show you are using full time EPR at 3 cm. Neither has any kind of Ramp, either timed or Auto.
I've never felt a need for a starting pressure ramp to increase when I go to sleep because I prefer to start out with a specified minimum pressure and either keep it constantly in CPAP mode or use APAP mode to adjust up to whatever pressure is needed and then go back down again.
As I had explained before the AutoRamp is not actually a ramp up in pressure. It holds the pressure at a Ramp Start Pressure that you set. For example you could set the Ramp Start at 7.4 cm. It will just hold it there until it decides you are asleep. The advantage of using the AutoRamp is that it lets you select the EPR type as Ramp Only. That way you can get the EPR comfort for going to sleep but not have it negatively impact the effectiveness when sleeping. Having the EPR on full time as you have it now is most likely causing some of the central apnea you are experiencing.
Hello, This post is a few years old, but just wanted to toss it into this thread for reference... https://myapnea.org/blog/2016/02/what-is-complex-sleep-apnea