Alright, I'm attaching my recent titration study interpretation and what they used in lab to treat it. I know that in the lab they used an OmniLab for the titration. I wore my own P10 mask for the titration study. I have basically been treating with APAP since last year. Some days it would work and others I would have a ridiculous amount of events for no rhyme or reason. In APAP, I figured out that my max was 9cm and I would usually start out at 8cm and have it set to ramp to 9cm if needed. EPR was set to 3 full-time on an Air Sense 10 Autoset. Yet I also have central apneas that the APAP of course cannot treat.
So last month I had my titration study. The sleep tech started with CPAP and central apneas spiked (got really dizzy, the room was spinning with my eyes closed, had an out-of-body experience likeI floated up to the ceiling), so she switched me to BiPap. As you can see, in the lab they apparently brought it under control to reduce my hypopneas, obstructive apneas and central apneas using BiPap. Then I was holding for a BiPap appointment with my sleep doctor. Just had that Wednesday morning.
I researched the various BiPaps ahead of time. Some people were telling me to push for BiPap ST instead of S for me centrals because the timed mode helps with centrals. I sent an email to my doctor's office ahead of time asking about the type of machine. I also called. They gave me the, "Whatever machine you get will be based on your titration study."
Ended up with Air Curve 10 S. 6 months rent to own if I'm compliant for like 70% of the month and sleep at least 4 hours per night on the machine for about 21 nights.
Per the lab titration results, my settings needed were 9 IPAP and 5 EPAP. Easy-breathe is on. Ti max is default at 2.0s and Ti Min is 0.3s. Trigger set to Med, Cycle set to Med. 20 minute ramp time. Start EPAP is 4.0 and goes to 5.0 after 20 minutes.
This was my first night on it last night. I pulled it off a few times to take a break because I woke up feeling like I wasn't breathing (central) even while using the machine. I felt awful this morning.
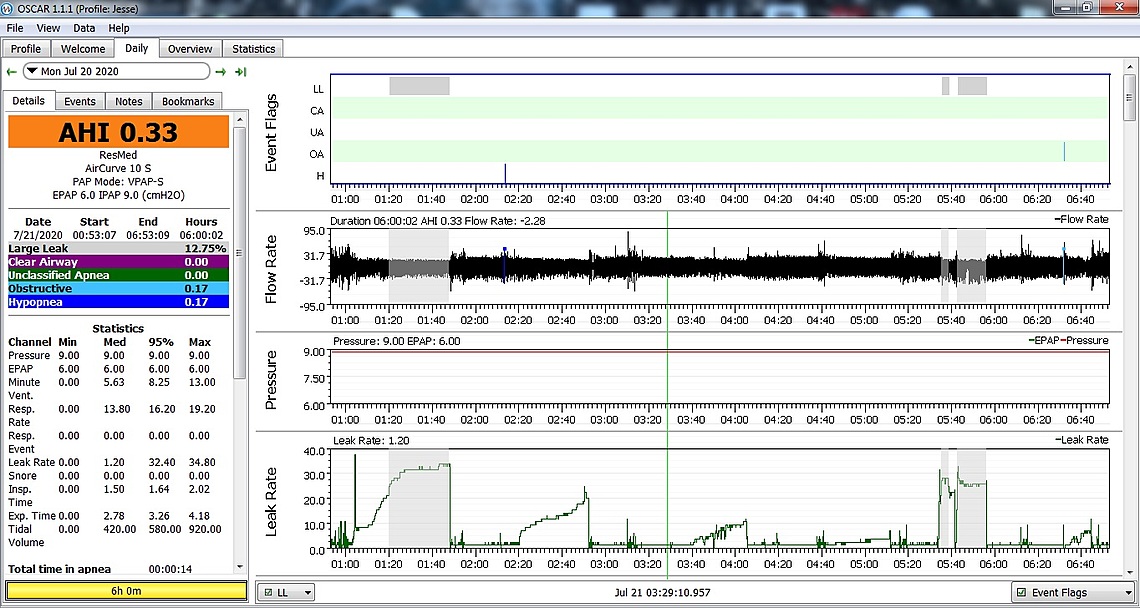
Looked at my data in OSCAR and I saw 45 CA events in 5.25 hours with just a couple of hypopneas and apneas.
The sleep manager lady who set me up with the machine to take home was rude and direct. She gave me her card yesterday and said, "If you have any questions, reach out to me."
So this morning I emailed her with the same screenshots from OSCAR that I'm posting here. My email to her said: "I picked up my Air Curve 10S BiPap yesterday and wanted to share results of my first night. I had an extremely rough night and as you can see from the screenshots, I have followed the exact settings given to me 100%. There were a few times when I had to take my mask off for a little break because I kept waking up so much from whatever was going on. I use a software called OSCAR, which is commonly used to review CPAP/BiPap data for patients. I also use the ResMed MyAir app. It registered 45 Clear Airway (Central Apneas), 1 hypopnea and 3 obstructive events for the 5 hours 16 minutes that I kept the machine on. My obstructive apneas are pretty much gone and my hypopneas are gone, but my centrals are quite high. Do you have any advice that might be of help?"
Got a rude reply:
"Sir,
This is the first night you use the machine. It is not a magic wand. Also the software you are currently using is not FDA approved. 45 clear airway is also not central apneas, the abbreviation is probably the same but central apneas is not clear airway. Just continue using the machine and we will analyze it when you come back from you visit. For the mask, you are in the adjustment period. Give it a time to adjust.
Thank you"
If they are not centrals, what else could they be? She's from another country and obviously the language skills for typing are not there. I'm confused. My understanding is that CA in OSCAR is central apneas. Centrals went down in the lab titration, but spiked at home. Using the same P10 mask (she gave me a new one with the machine, too). What do you make of this?
Primary care doc is going to do an MRI of my head next week to check for various stuff.
I toss and turn all night, every 30 minutes or less per the motion camera trained on my bed. But in between, I probably move all night long about every few minutes. I just shift in position on my bed or move an arm or leg just a little. I'm thinking this may be centrals...I saw a little boy's central apneas video one time while he was sleeping and he woke up sometimes seconds apart without a machine. Wondering if my centrals are doing that.
Any advice?
If the BiPap S is not working, what will happen to it? Get another machine on the insurance and keep this one or return it? Doc doesn't seem to like used machines. I asked my sleep doc about my APAP (Air Sense 10 Autoset with low hours) that I was self-treating with before and my sleep doc said, "We usually just throw them away. Nobody will want it, especially around this time." I saw someone with an auction for one on Ebay at $400.
I have an appointment at 1 months, 2 months and 3 months from now and they want me to bring the machine to each appointment.
What is the reason why I'm so miserable while using the BiPap at home if it worked in the lab? I also have times in the later afternoon while just resting/sitting where I'll just get short of breath like I'm going to faint and it comes and goes in waves. Odd twitches/feelings/tingles all over my body. Primary care doctor suspected POTS/Dysautonomia. Heart was checked by Cardiologist - good. Full Stress EKG and ultrasound with ColorFlow. Had my thyroid checked by an Endocrinologist. Nothing wrong. Lots of blood work. All fine. I have times when I feel like I have to force myself to breathe while sitting upright during the day. It is like I have central apneas sometimes while sitting up during the day and I just "stop" breathing until I force myself to breathe. Very odd. Should I see a Pulmonologist?
I can't open those links to look at the images. If the CA is at 45 for the night, that is not good. When you asked for advice about a BiPAP I recall I told you that it would be very unlikely to help you. An APAP set to 9 cm and 3 EPR is very little different from a BiPAP set to 9 cm IPAP and 5 cm EPAP. It is just going 1 cm lower on exhale. Insignificant difference.
They detected central apneas during the lab titration and felt that BiPap would be more helpful. I fixed the links above and they work now, it did something weird with the coding. Curiously, this morning I only had about 25 centrals over a total of 9 hours or so. The majority of them are within the first hour, specifically 30 minutes to 1 hour after going to sleep. If I remember correctly, my titration study stated that most of the centrals were NREM.
Does a "getting used to it" time period exist for going from CPAP to BiPap or just a lucky night where I didn't have as many centrals? Even on fixed CPAP mode with my Air Sense 10, I saw a number of centrals each night. Usually 6-10 using 8.4cm pressure all night.
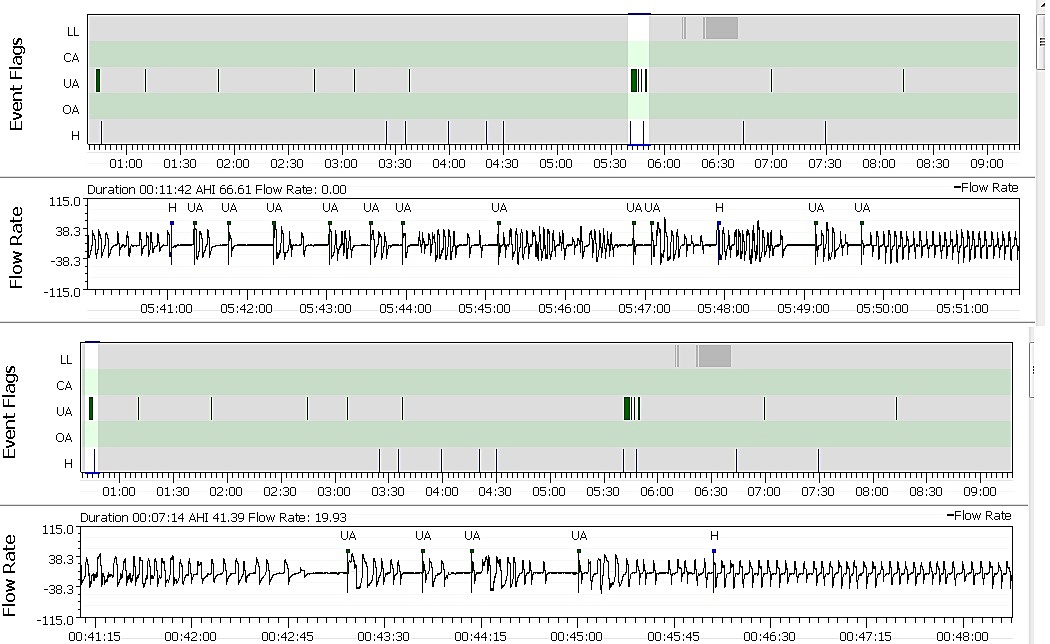
Yes, that is an excessive number of CA events. If you could post an expanded view of the flow rate chart and mask pressure for a short period of time where the whole series of CA events occurred, say around 2:15 or so, that could help understand what is going on. The time scale needs to be expanded so you can see the breathing pattern leading up to each CA event.
I don't think there is a "getting used to" for an BiPAP compared to a APAP. They may need a period of time to adjust the additional settings that a BiPAP has. However, I am not optimistic based on what I see. You are getting an effective pressure of 5 cm (EPAP) but at the same time you are are undergoing a pressure up to 9 cm on IPAP. That could be the worst of both worlds. The IPAP is causing the centrals, and the low EPAP is allowing obstructive apnea too. I still think you could achieve more with an APAP set to have NO EPR during the sleep period, with a fixed pressure only high enough to stop the majority of the obstructive apnea.
I uploaded photos to the site, but they were tiny and hard to see for some reason.
https://i.ibb.co/m6TBCWX/Centrals1.jpg
I changed my settings to see what it would do on BiPap. Went down to 8.6 and turned off Easy Breathe. Instead of Clear Airway events, I got a whole lot of green Unidentified Apneas in their place. I actually do remember waking up with those...felt like the airway was blowing my throat closed or something.
Didn't sleep for very long or very well because of a super early work morning on a Sunday and fireworks were going until 2am or after.
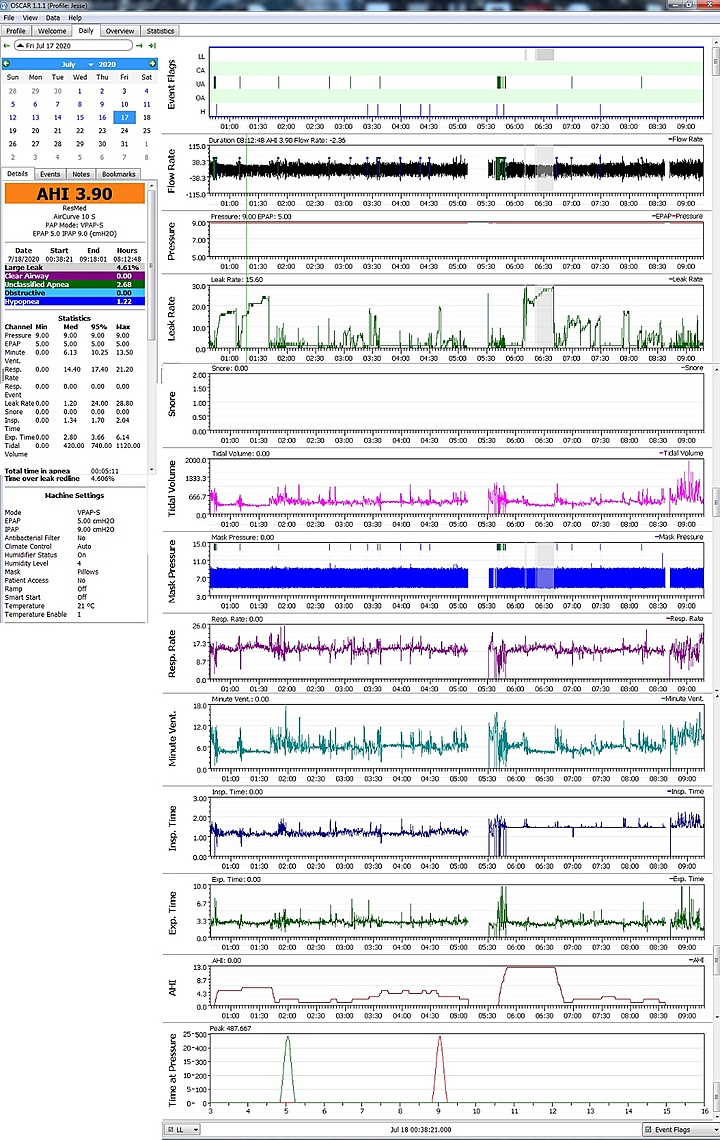
Alright, so I still feel quite dreadful everyday. Still seeing lots of events on the Air Curve 10S at 9/5 settings.
I think I go back on August 2 or something like that for them to review the first month of data.
My POTS/Dysautonomia has been giving me a run for the money lately. Doc wants to put me on an anti-depressant for the 'anxiety' that it is known to cause due to the symptoms. Those seem to be pretty bad for the body. The 24/7 dizzy thing, feeling like I'm going to faint if I lean slightly over the sink to wash my hands and such. It's pretty miserable. Stomach aches and feels weird a lot, intestinal paints/discomfort every day, not going to the bathroom as often as I should be, sometimes kidneys/bladder don't seem as regular, etc. Just had a brain MRI with and without contrast last week. My primary care doc's statement to me was: "One of the first things I would say is that I feel extremely confident that there is no heart problem, lung problem or brain problem. That does not mean that what you are experiencing does not exist but that the fear that it is a sign of a more sinister underlying disease is misplaced. Because dysautonomia / POTS is not a disease that is measurable it is more a disease or condition that we have to diagnose largely based on a person symptoms. It's not like blood sugar or blood pressure necessarily where we can track it and anticipate problems. Essentially we learn from other people who have had this and what has helped and what hasn't. We have no idea why it starts and nobody else that I had with dysautonomia has had a strong family history so it does not seem genetic. Also interestingly most of my patients who have had it will outgrow it eventually. My patients who have had the most success with it over the years have been the ones who have accepted and often have started on an antianxiety medicine to help modify the anxiety associated with the symptoms. Certainly there are other things that one will learn such as having extra salt, sometimes using medications to boost blood pressure, being aware that very hot environments are likely to induce lightheadedness, etc. You will learn how your body functions best. I would also continue to work to optimize sleep but rather viewing yourself as someone with a potential life threatening disease, view yourself as someone with a conditions that needs management and once you figure out your optimal management it should only be a nuisance."
Then I have all of these "Unclassified Apneas" that keep showing up no matter what each night. Before I turned the Easy Breathe off with the 9/5 pressure, I had a huge amount of centrals with an AHI of over 9. Just back to back rapid-fire centrals in clusters. I turned off the Easy Breathe the second or third night after I got the BiLevel and those central apneas in OSCAR show up now as Unclassified Apneas. They look like either obstructive apneas or central apneas. Is there a true way to tell? I just feel uncomfortable and agitated all night, especially with my stomach and abdomen feeling weird or having a dull ache.
At this point I'm really confused. Is it just a pressure setting that is wrong or do I need something like ASV? I'm in the process of trying to get my original sleep study before the titration study to see if any centrals showed up on the regular sleep study. If they did, would I need ASV?
My newest settings allow me to at least breathe more normally:
IPAP 9.0 EPAP: 5.0 Easy Breathe off Ti Max 2.5s Ti Min 1.5s Rise Time Min Trigger Very High Cycle High
The original BiLevel settings that it came with new out of the package were ridiculous. It was something like TiMax 1 or 1.5 and Ti Min was about 1 or less. The other settings were also different and it made me breathe so quickly to try to keep up with it. I haven't changed IPAP/EPAP yet because I wanted to see what my doc office says after a month of seeing all of these. He did say if the BiLevel didn't work out, we'd try something else.
I'm considering going to a POTS/Dysautonomia doctor with Emory. There are a few of them locally and one does a tilt table test. I've met my deductible already.
I feel absolutely fatigued daily. It honestly feels like I sleep better on my side/stomach without the machine than with it. All that I feel like doing every day is laying down to relieve the POTS/Dysautonomia. I've noticed that when I go to work feeling dizzy and bad in the morning, once I get to lifting things and moving around, the dizziness tends to go away and I feel better in general. I guess because I get the blood flowing more or something. I'm also increasing my cardio workouts regardless of dizziness.
Anyone out there had POTS/Dysautonomia and got rid of it? How long? Is it just because of my sleep?
I looked back at the month of June when I used APAP under various settings lower than the 9, usually 7.4 to a little over 8. I still had centrals popping up here and there. Sometimes a lot on one day and a little on another day under similar settings.
So here's an odd question for you...I was using the above settings for the previous thing. Then last night on a whim, I turned the Easy Breathe on and my EPAP went from 5 to 6. I'm assuming the machine made this change because I don't remember doing it.
So I went from all of those weird Unidentified Apneas to one single hypopnea this over 6 hours this morning.
Does that lack of obstructions pretty much guarantee that I don't have central sleep apnea or can it "skip" some nights even if you do have it?
Or could this simple change change that I made last night indicate that it treated my CPAP-induced sleep apnea?
Or is it possible that my doctor's office CPAP person changed this setting wirelessly? I know for sure that it was 9/5 and it is now 9/6. Double checked on the machine, too.