I am an extremely compliant cpap user of about 17 years and have never had difficulty switching machine, mask etc... until now. I had been using resmed s9, pressure 10, ramp 45 min starting at 5 pressure, and no epr. Used climateline tubing and Swift nano pillows. Enter the new equipment: resmed airsense 10, airfit p10 pillows with slimline tubing. All settings are the same. Since day one of using new machine i am exhausted when i first wake up and tired all day. Any suggestions?
Error in my original post. Original mask was not swift nano ... it was swift fx pillows
The model name should be on the front bottom right of the machine. The four models are CPAP, Elite, AutoSet, and AutoSet for Her. I believe all of them save detailed data except for the CPAP model. You can download OSCAR at this link. It requires a PC or Mac, and a SD card reader.
You can also set your machine to display a more detailed sleep report on the display itself. You have to set the "Essentials" option to plus. See page 17 & 19 in this AirSense Technical Manual.
Sierra, thank you so much for the additional info. The cpap is an Autoset. I have reset the Essentials to Plus now and have access to more details.
When i get in my pc tomorrow i will download the OSCAR software and see what more i can do with the more involved information.
I am looking forward to trying my old mask tonight and hoping that will again provide a better nights sleep, like i was getting before the equipment was updated.
With additional research i am beginning to suspect that the mask may be the issue. I do remember being told by an anesthesiologist at my last colonoscopy that i am a” shallow breather” (so have to have professional oversight when i am being put under), so am suspicious that i am not getting into a deep enough sleep, possibly because i am not eliminating enough carbon monoxide on my exhale. That would explain the headache as well as being so tired. If that’s the case, the swift fx may be a better choice for me than the airfit p10.
Of course it is entirely possible that i am totally screwed up and that this has nothing to do with it....
One other note, on the three nights i have used it two have been with epr on and one off. No difference in symptoms
I should have asked you earlier, but what are your AHI numbers like? With the Essentials turned to Plus, you should be able to see an average of all the data you have collected to date with a breakdown of the obstructive, hypopnea, and central apnea events. You can set the time interval that the data is averaged over.
I also have an AutoSet machine and have it set for a fixed pressure, which in my case is 11 cm. I have issues with central apnea and have found that if I use a fixed set pressure the machine does not get carried away and increase the pressure too much and cause even more CA events.
I do have my machine set up a little different though. The AirSense has more features than the S9 (which is the machine my wife still uses). One is the AutoRamp feature. I use it and like it. It monitors your sleep and ends the ramp automatically when it decides you are asleep (to a maximum of 30 minutes). It is not really a ramp as it just maintains the pressure at a fixed value that you set with the Ramp Start pressure. I find 5 cm is much too low for me as a ramp pressure, and I currently have mine set at 9 cm. I like to be able to breathe deeply without feeling that air flow is restricted.
The other thing I do is set the EPR to 3 cm, and further set it to Ramp Only. This way during the ramp I get 9 cm on inhale, and 6 cm on exhale. I find that more comfortable when I am going to sleep. When it decides I am asleep it switches to a fixed 11 cm, and stops the EPR, so inhale and exhale pressure are both at 11 cm. The benefit to that is that it can reduce obstructive apnea events which can start during the exhale phase of each breath. It allows for a lower set pressure which is more comfortable and at least for me avoids some of the central apnea events.
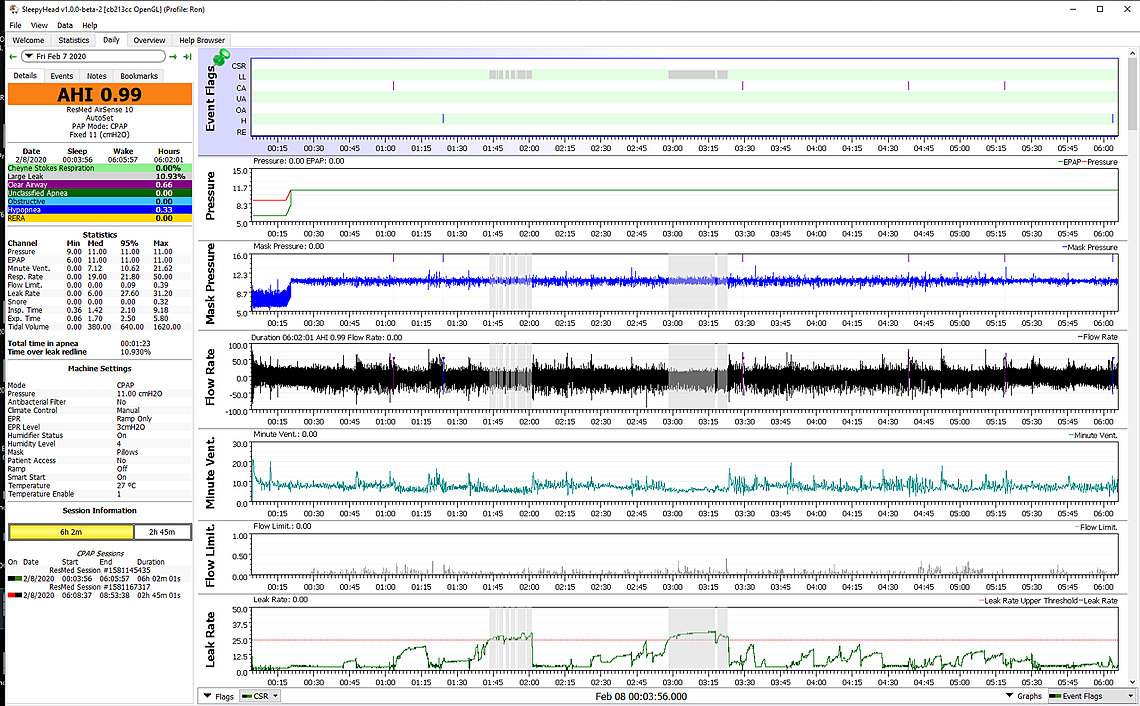
I hope that helps some. If you have any questions just ask. This is an example of what you can see with OSCAR. I am still using the previous version called SleepyHead, but it is very similar to OSCAR.
One other thought. If you still have the S9 machine and more importantly the SD card in it, what you should do is first download the data from the S9 into your OSCAR program. Next you can download the data from the AirSense 10 machine. Then you will be able to go back through your S9 sessions and see in detail how it was behaving. And, you will be able to compare that to what you are getting now with the AirSense 10. OSCAR is smart enough to recognize both machines and display the data from both.
Just looked and what i show is AHI 0.2, AI 0.1, central 0.0. I think those numbers are fine... I’m just not sure I’m getting deep enough sleep for some reason.
Looks like the oscar software will tell me quite a bit more than even the Essentials... anxious to see the results there too.
I think I’m going to have to look at some changes ... but keeping my fingers crossed that going back to my old swift fx pillows helps tonight. That would at least narrow my problem down.
An AHI of 0.2 is excellent. It is possible your pressure could be lowered some although 10 is not that high. How did you end up with a fixed set pressure? The other option you have would be to put the machine in Auto and allow it a max pressure of 10, and perhaps minimum or 7 or so.
One other thought. Did you set the new machine up yourself? I believe the default setting for an AutoSet is to be in Auto mode. Is it possible you have it in Auto with a minimum pressure of 5 and max of 10?
No, the machine was set up by Apria and i received shipment from FedEx. But the first machine i received had a major noise issue and had to be replaced. They were both set on fixed 10. But they weren’t both the same as far as humidity and epr. One even had the tubing programmed wrong!
I have never had an Autoset programmed on any machine but think that’s another great idea to try It and then i could see if my body is demanding 10 or not. I have been on that same pressure most of my 17 years... they put me on fixed 7 in 2008 and i started getting tired again... but it wasn’t as intense as it is now.
I think I’ll try the mask change tonight and then maybe the autoset range tomorrow night.
You have been so helpful and informative... I’m not sure how to say thank you loud enough!
Do you have a heated hose, which ResMed calls the ClimateAir? If so, when you plug it in with the AirSense 10 it should put the humidity control into Auto. I find mine works fine in Auto Humidity control. I leave my temperature setting at the default. The only time I have a problem is when I forget to fill the humidifier with water. That is not comfortable at all. I usually figure it out some time during the night, and get up to fill it....
I have the heated hose on my old s9... but Medicare opted to pay for slimline only on the new unit. If i can get this new unit to work for me I’ll probably step up and buy the new climate line until Medicare decides i need it. It’s not too bad on Amazon. Although we have moved to the desert now, so really don’t have the variations in bedroom temps and humidity that i used to have. Really loved the old climateline when we would camp in unheated trailer/cabin and the temps got down into the 40s. In the new home if we get down to the high 60s that’s a cold night!
I too have let my tank run dry a time or two... not a smell you can sleep through ...
Update after switching to my older swift fx mask from the new airfit p10.
MUCH BETTER today. I think it may take a few nights to get back to normal though. But, after just one night my thought processes are clear again (not in a fog), my energy level is substantially better, I feel more rested but not 100%yet, and my headache has diminished quite a bit.
So my conclusions: for me the airfit p10 is not a good fit. This may be due to my diagnosed “shallow breathing”, resulting in elevated co2 and rebreathing. The symptoms of too much co2 are markedly improved after one night with my old mask that doesn’t have the mesh vent.
Amazing how bad i felt after using the p10 for less than a week... so will hope that it continues to improve after the switch back to the swift fx.
Gotta say i am kind bummed overall, cuz the p10 was a very comfortable mask...
I have used the P10 mask pretty much from day 1. I did try a F&P Brevida but did not like it as much, but my wife did, so she now uses the Brevida. I also tried the Swift FX nasal pillow mask, but I could not tolerate the high velocity air exit from those holes in the mask. It kept waking me up during the night. My issue with the P10 is not the mesh vent, as I love that part of it. I find it amazingly quiet and no high velocity air. What I dislike about the P10 are the flimsy straps. Tried various things, and then finally decided to make a hybrid mask which is the P10 modified to accept the Swift FX headgear. That is what I use now. Here is a link to a post where I described how I made it.
I am not sure what to think of the CO2 being a problem. These masks are all designed for a certain vent flow that is to keep the CO2 in control. In general the larger the volume of the mask, the higher the purge air flow.
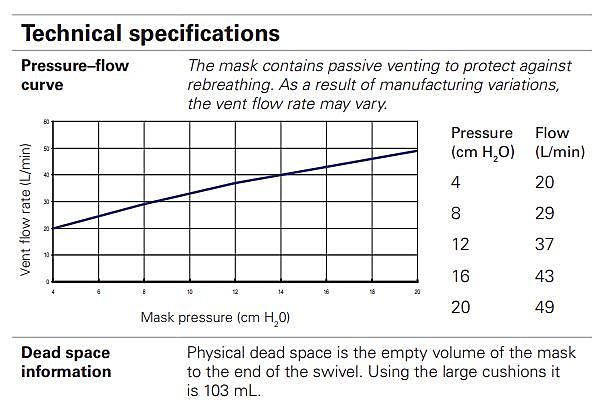
This is a clip of the technical specs for air flow on the Swift FX. At 10 cm pressure it looks like the air flow is pretty close to 32 L/min. The volume of the mask is 103 ml.
And here is the P10 mask. I see the air flow is almost identical, but the volume of the mask is a bit larger at 123 ml. So yes in theory on a relative basis to the volume the FX has a higher flow.
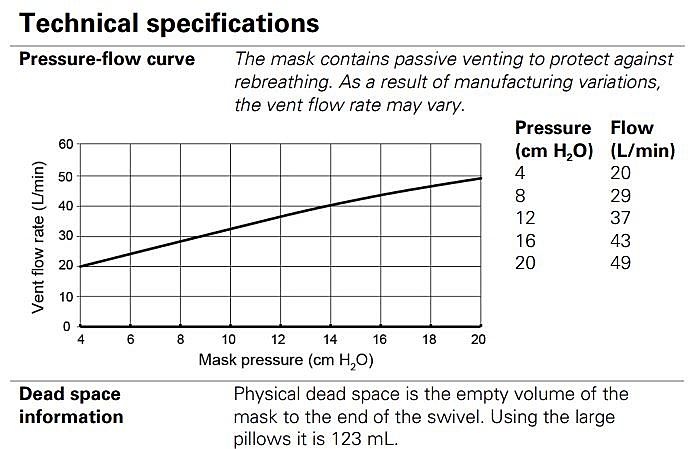
These specs can be found in the user manual. For my purposes in reducing central apnea, the lower purge rate, and higher CO2 may be helpful to me.
I can only think that it is my shallow breathing making it worse ..., and probably the intensity of the vent probably helps to dissipate. I will be checking with the dr on my return Medicare required compliance visit.
I did get the oscar software downloaded today, and my initial download done. The main difference for night after i switched from p10 back to swift fx was the AHI increase from 0.2 to 0.6. Still fine.
Tonights changes are switching to autoset, and changing ramp to auto with a higher start pressure. Be interesting to see what difference, if any, this makes.
I am just so relieved that the fatigue, headache and mental fog are so much better. Again, thank you so much for your help... very appreciated.
You can get some idea of the volume of air you are breathing by looking at the "Minute Ventilation" graph in OSCAR. It tells you the effective air transfer rate in Liters per minute. Ideally this should be a fairly smooth graph and not vary during the night. I have no idea if my value is typical or not, but when the level is smooth and steady it is about 5 L/min. With OSCAR you can left click on an area of interest to zoom in, or use the up and down arrow keys. The value on the graph will be displayed right at the top of each graph. This graph indicates how stable the control is of breathing. If it cycles up and down it indicates your body is trying to find the right level. In my case it is one of the sources of central apnea events. CO2 plays an important part in how your body controls breathing rate.
Just checked my wife's graph and her normal Minute Ventilation looks closer to 7 L/min. She never suffers from CA events. Perhaps I am a shallow breather as well...
There is a wealth of information there...i think it will take awhile to begin to understand it. Maybe this weekend i can take some time and delve into a good tutorial.
I did look at the minute ventilation you mentioned, and mine seems to average on 5(5.05) with some fluctuation up and down.
With the changes i made last night the pressure did go almost to the 11 number of times... but seemed to be around 9 most of the time. So the 10 they prescribed years ago still seems to be pretty close. I think i will leave these settings for about a week and see how i do. If i push the top much i may increase the max to 12 to see if 11 is enough. The AHI was 0.3 last night... so all good there.
I have not had a full blown sleep study since 2007. They tried this year but i never slept deep enough to have any issues. I think i should have had a drug first since they wanted two hours deep sleep without my cpap. After 17 years use, that is difficult. They then did the home study, and did give me drug... so at least they were able to confirm the severe apnea.
Most importantly, all the other items are still good today... so going back to the old mask seems to have solved those problems. Had i faced those issues when i first went on cpap, i never would have been compliant... it was miserable!
I am not so sure about the value of a sleep test if you are sleeping well and the AHI is low. The pressure you need to achieve that AHI is an indicator or how severe your apnea is. With a pressure of 10 cm working well for you, that suggests moderate apnea, perhaps at the higher end. But it is not really more than a curiosity if you can control apnea with a pap machine.
I know my recent home study reported an AHI in mid to upper 30s without cpap... so the therapy is definitely doing its job.
I remember years ago it was much worse... when i was first diagnosed. But a move to a lower elevation a couple years ago has definitely helped. (5000 ft down to 500 ft)
I was so bad initially i could have kissed the drs after the diagnosis... it made such a difference in my life. In addition, i had very bad refux which only occurred in my sleep. And cpap therapy stopped that. Plus improved my blood pressure ... as well as made me just generally a more happy person cuz i was finally getting some good sleep. I had dealt with it so long i thought that was normal for me... what a revelation it was to really sleep good.
As a result i am about as compliant a person as you have ever met... On the rare occasions i haven’t used my cpap (power outage etc), the reflux starts again... and then it’s45 minutes of burning hell before i can breathe well, swallow without pain and get back to sleep.
Definitely a fan of the cpap ...
Elevation is one of the things that can aggravate central apnea issues. I live at only 2000 feet, but do notice an improvement when I manage to go on vacation at sea level. Have not gone to higher elevations since starting using a CPAP, but I expect it may not be good in a place like Denver.
I'm new here but I feel your pain. I've experienced the exact same thing. I just got a replacement resperonics dream station, matched pressures, thought I slept well, woke up with the worst jet lag feeling, yuck!!! I hate that feeling. For some reason, the slightest change can ruin a nights sleep, mask, machine, fine pressure settings etc. I think your brain adjusts to the new mask, pressure setting, over a period of a week or so. Otherwise I've never found a explanation for this.