Hey everyone,
I recently started using a BiPAP after completing a titration study. The tech and doctor said that in the study, they were able to get my AHI down to 3. However, with the BiPAP at home, my numbers have been significantly higher. As high as 30-40, but most recently down to 15, as they have been adjusting setting. Is this common that it still takes adjustments and time? I'm falling asleep fine with the mask on and feel comfortable in bed with it, but I end up waking up halfway through the night, from what feels like an apnea. Have others experienced something similar?
Thanks, Ari
It always takes some time to get a CPAP or BiPAP optimized, even if they are of the automatic type. There are a couple of things you could do. Your machine probably has a SD card in it that tracks all the detailed data during the night. Sleep clinics can see some high level data on your machine wirelessly, but most do not monitor individual machines, and in any case do not see the detailed day. You can take this SD card to an in person appointment and have them look at the detailed data and graphs. They should have the software to do it. From this they also should be able to determine what needs to be adjusted. The normal target is to have AHI under 5. The unfortunate part is that most of these clinics make their money on selling you (or your insurance company) the machine, and don't want to put much time into it, after the sale.
Another alternative is to download some free software called OSCAR. It lets you view the detailed data yourself. If you post it here you can get suggestions on what may be wrong or could be improved. The software requires a PC or Mac and a SD card reader.
Sierra,
Thanks for your response. I saw the doctor and looked a little more at the data using OSCAR, happy to know about that software now! It looks like the OSAs are very minimal, but the central apneas are now very high (30-60 AHI). My titration study showed virtually no central apneas. After a bunch of internet searches, I've stumbled across the idea of "treatment emergent" apnea. Is this just my body reacting to the machine? Do you know of resources available to learn about this? I'm wondering if wearing the machine when I'm not sleeping will help my body adjust at all.
Thanks, Ari
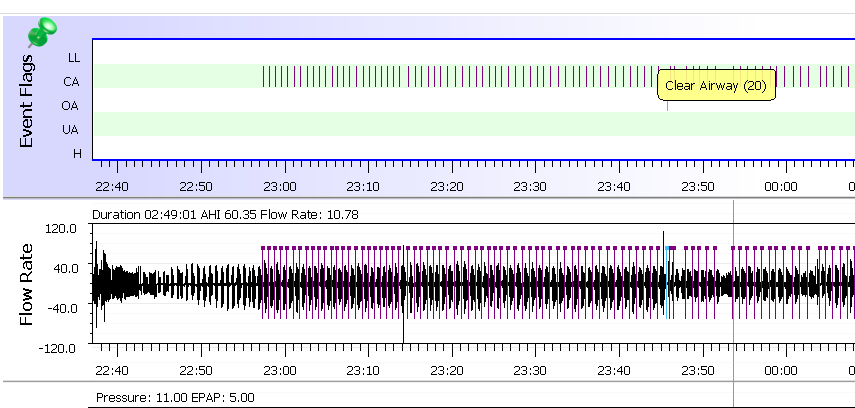
Your Oscar chart shows an incredibly high number of CA events, highly unusual. A BiPap machine algorithm basically looks at the flow rate and if your airway is open but you are not exhaling, then there is no resistance on the flow rate and your machine algo registers this event (if it lasts more than 10 seconds) as a "central" event. I am guessing that you have been given a Resmed machine but without its model, I can't be much help on correcting the titration in order to get rid of the centrals because it could very well be that you are not having that many central events and the machine algo is incorrectly reporting it because of titration. Also, what was the result of your original sleep study? (was it 90% CSA and 10%OSA for example?) I am asking because your doctor should have prescribed a ASV machine instead of a bipap if your CSA events were higher than 20% of the time during your sleep study. The reason you need a ASV type is because the algorithm on an ASV is designed to monitor and react to your respiratory function, on a breath-by-breath basis, so it will constantly adjust its IPAP and EPAP pressures within a wide range in order to "stabilize" your "Minute Ventilation".
A non-ASV BiPAP is only designed to drop EPAP pressures to a preset limit at expiration and vice versa for inhalation. The algorithm does not otherwise attempt to stabilize Minute Ventilation or any other respiratory characteristics. It just provides positive pressure to keep your upper airway open in order to treat your OSA with the added comfort and precision of having a secondary pressure setting for exhalation.
Look up Adaptive Servo Ventilation (ASV) therapy online. There are a lot of very good articles about it. The machine itself looks exactly like a CPAP machine but the turbine and software are designed for ASV function.
The OP indicated this in a second post.
"My titration study showed virtually no central apneas."
It looks like it is treatment emergent central apnea, and an ASV would not have been indicated as a result of the lab titration. However, one may be needed at some point, if other changes cannot bring it into control. At one point I was convinced I needed an ASV, but that has not turned out to be the case. The right settings in a simple CPAP fixed pressure mode has worked for me.
Your OP does not indicate specific lengths of time or wether your original study showed Centrals or OSA. That being said, "Treatment emergent CSA" does not necessarily happen to every OSA patient under treatment, nor does it happen after a relatively short period of time. It usual takes over a year of OSA treatment according to studies , but then again I am not sure how long you were recieving OSA therapy before .
Look, your machine is registering way too many Centrals. That is because even though it recognises these events, its algorithm is NOT designed to take action to break them up, so it just observes and reports. You need a machine that can break your centrals , not just report on them and if indeed they ARE legitimate centrals and not false flags, then regardless of how much you tinker with your machine, it is not going to work because it is not the correct machine for central apnea.
All the best and keep us in the loop..
"It looks like the OSAs are very minimal, but the central apneas are now very high (30-60 AHI). My titration study showed virtually no central apneas."
It looks like you may have treatment emergent central apnea. This is when the pressure used to reduce obstructive sleep apnea causes an increased number of central events. I had something similar happen to me. In some cases this type of central apnea can go away after 6-8 weeks or so. In my case it did not go away. I have made some changes to limit the pressure the machine uses and have been able to average about 0.8 for AHI, but it still goes much higher on certain nights when central events happen.
If you could post a full screenshot of the Daily Report it would be helpful to see where you are at. The events bar, pressure graphs, and flow graphs are the most important and should be at the top From what you have posted it looks like you may be getting into Cheyne Stokes respiration (CSR) or if you have a DreamStation machine they call it periodic breathing (PB). A starting point to look at is to determine when central events are occurring. Then you can see if higher pressure is related to when they occur. If that is the case then you look for opportunities to reduce the pressure. In my case I believe my machine (ResMed AirSense 10) was seeing Hypopnea events and responding with increased pressure. Hypopnea can be central in nature or obstructive. If they are central then increasing pressure is not the correct response for the machine. I addressed that by limiting the pressure it could automatically go to.
Do you know why they selected a BiPAP machine? It may not be the best solution for you. I have an Auto machine but I now run it in simple CPAP mode with a fixed pressure, and do not allow the machine to automatically increase pressure. I set that fixed pressure based on what I saw when it was in Auto mode and then with just trial and error to see how low I could reduce the pressure before obstructive events started to occur.
In any case if you post a full screen it would help a lot to understand what is going on in your particular case. Where you are now with those regular CA events running up your AHI is not a good place to be.
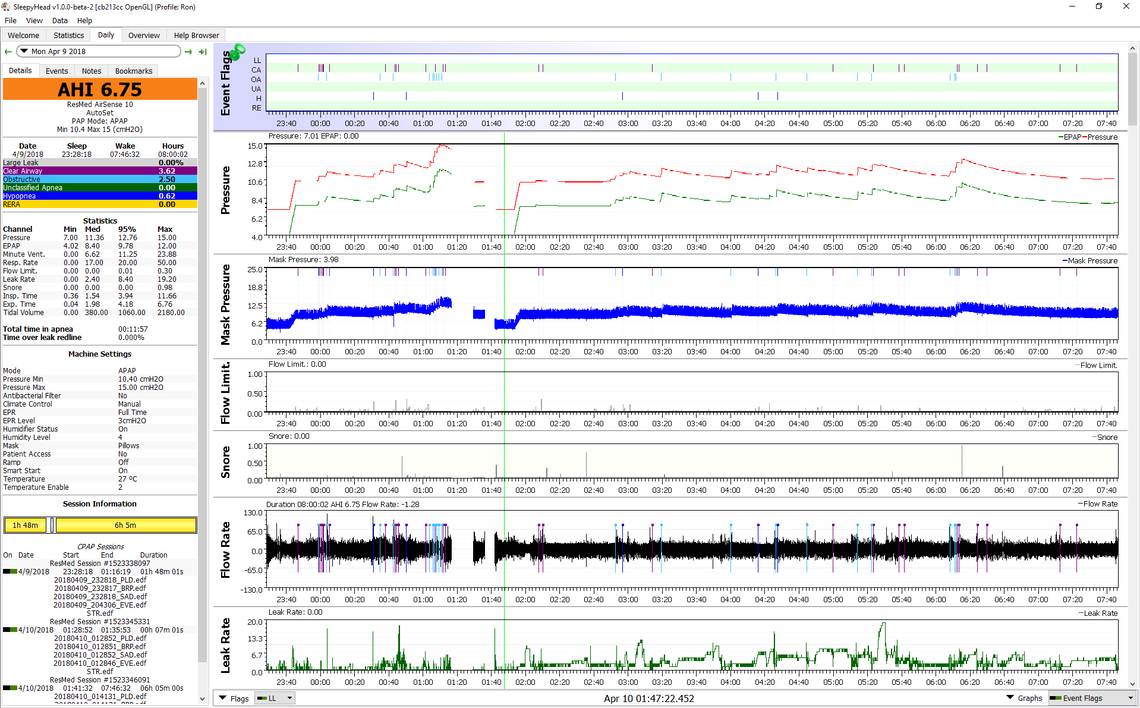
Here is an example of the trouble I was in back in 2018 in Auto mode of my machine with EPR (like pressure support) at 3cm.
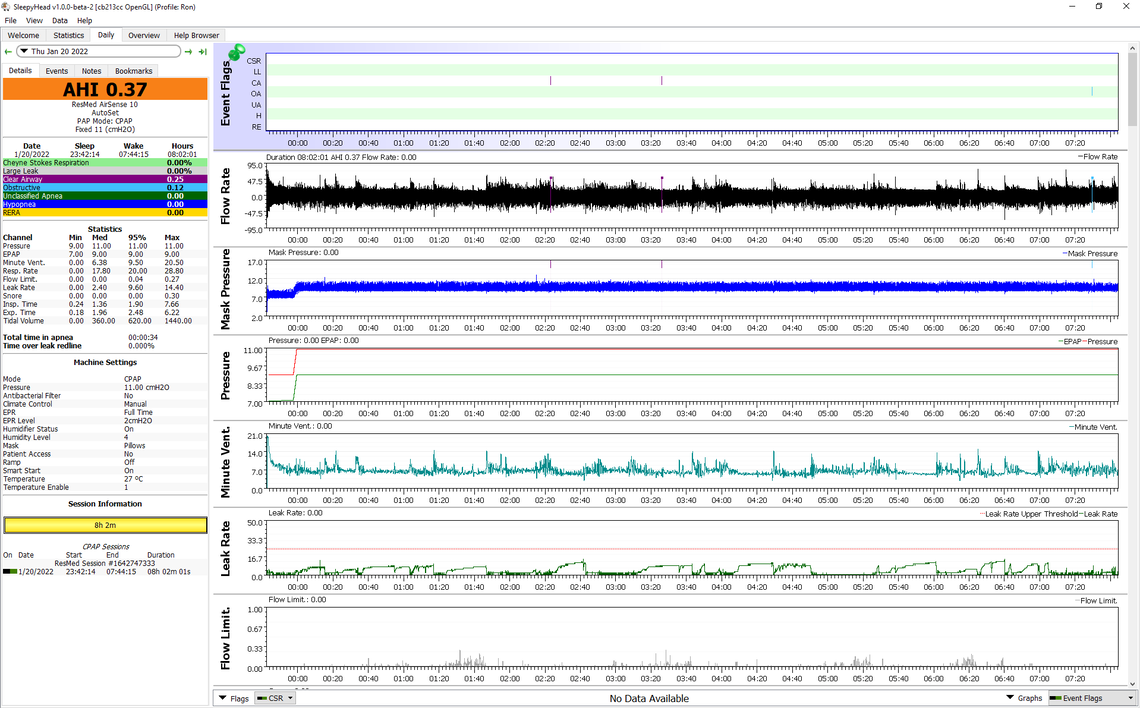
And here is my report from last night. This in fixed pressure CPAP mode with EPR at 2 cm. It is not always this good, but I do now average 0.83 for AHI over quite a long time.