I have had very little help from sleep doctor #1 (Nov, 2021 in-lab sleep study was useless) or CPAP Vendor. I am waiting for results from in-lab sleep study conducted Jan, 2022 ordered by sleep doctor #2, who seems to be very competent, but extremely hard to schedule time with. In the meanwhile I have been using a Resmed S9 with well-fitted Resmed AirFit N30i nasal mask, and reading all I can about CPAP treatment and how to 'dial in' the correct settings. I just received an Airsense 11, but suspect it may be defective (delivers fixed pressure when settings are on Auto, causing bad headaches when I wake up), so trying to find the best settings on S9 before I start dealing with the AirSense 11.
I would greatly appreciate some help. I was impressed with the way Sierra found personal ideal settings by following a protocol of: find lowest possible max pressure possible to achieve low AHI; narrow pressures; find a fixed pressure (if possible) with EPR on Ramp Only, lower max pressure to reduce central apneas, then turn EPR back on to Full Time Level 2. Can you help me follow the same protocol to find my ideal settings? I have 18 days of Oscar data, with last night's data posted below. Please let me know if my Oscar data is not in the proper format. I welcome your questions and your advice.
Your layout is fine, except that the font sizes are so small that I cannot really read the numbers. But from what I can see, it looks like you have it in Auto mode with a minimum pressure of 6 cm and max of 9.6 cm? It appears that you are getting a large number of obstructive events when the pressure is at maximum. The first thing I would try is to increase the maximum pressure to say 11 cm and see if that improves things. Minimum could probably go up to 9 cm to narrow the control band some. Some people have issues with the head and neck position causing a rapid succession of OA events. You may want to try a different pillow, or some use a soft cervical collar that you can get at Walmart.
If you go to File, Preferences, Appearance you can set font sizes there. And, if you can post an updated Daily Report I may be able to see more. Also if you left click on the vertical scale of the pressure chart you can manually set it to 15 cm max. Then it will be easier to read the actual pressures. If you need to go higher you can change the scale later.
Hope that helps some to get started.
Thank you for your quick response, Sierra. I have made the chart changes you suggested. The charts are much more readable. I will look into a different pillow and cervical collar.
BACKGROUND
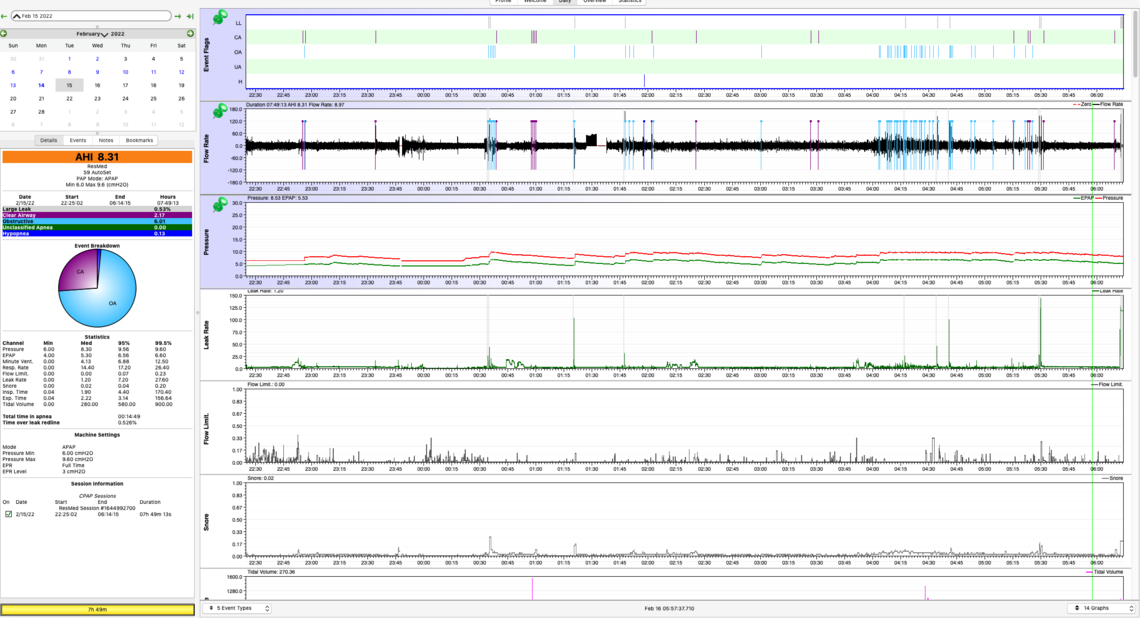
You are correct. Here are my current settings. Resmed S9 Mode: Auto Min Pressure: 6.0 Max Pressure: 9.6 Ramp: 30 min EPR: Level 3
Some additional information:
In this period of adjustment, I’m working out the ‘bugs’. In 27 days of using CPAP, I’ve experienced each of the following: a. I had an ill-fitting uncomfortable mask (9 days) with large mask leaks. Now have a proper fitting mask with no leaks. b. My mask came off while sleeping c. My machine suddenly quit and had to be reset d. I forgot to insert the SD card e. I forgot to fill the humidifier f. Therefore, I have ~13 nights’ data that I think are reliable
I believe the CPAP machine sometimes records apneas when I’m awake. When I know for sure the time intervals when I was awake (sometimes 1-2 hrs at a stretch), I manually filter these ‘awake apneas’ out. a. 13-night average, CPAP Recorded AHI: 7.87 b. 13-night average, Manual Filtered AHI: 4.46
SETTING THE CORRECT PRESSURE
TYPE OF APNEAS
I received my in-lab Sleep Study report yesterday. This study did not include titration with a CPAP machine. Total sleep time: 3 hr. AASM AHI: 79/hr Obstructive Apneas: 1/hr Central Apneas: 38/hr Hypopneas: 40/hr
OSCAR data from 13 nights’ at-home CPAP data (Manual Filtered) AHI: 4.46/hr Obstructive: 2.52/hr Central: 1.29/hr Hypopnea: 0.65/hr
Questions:
GENERAL QUESTION
Please feel free to ask for clarification or more information. I am so grateful for your help.
"I have been increasing the max pressure gradually. When I have tried to set a higher max pressure too fast, I experience headaches in the morning. I also feel that if I base the max pressure on the # CPAP Recorded AHI (7.87) rather than the # Manual Filtered AHI (4.46), I may set the max pressure too high. Can you comment on this please?"
It is prudent to increase the pressure in small steps. I think 1 cm steps are reasonable, but if you are having issues, then do less than that. Pressure is typically adjusted based on when you are having apnea events. You can expand the scale by clicking on the area of interest and using the up and down arrow keys, or repeatedly left clicking. What I am seeing with the level of detail I can see, is that the large majority of your OA events are occurring at the maximum pressure of 9.6 cm. I would expect the machine would go higher but it is being limited by your 9.6 cm max pressure setting. The machine can go up to 20 cm, but that is a high pressure and not usually comfortable. The trick is to reduce the OA events with as little pressure as possible. Everyone is different, but I can pretty much stop my OA events at a pressure of 11 cm.
Can you estimate what the optimal max pressure should be, judging from the median (8.64) or 95% (9.56) measures? I realize the max pressure of 9.6 in the attached daily example is too low and acts as a ceiling for the 95% and 99.5% measures.
It is not currently possible to estimate it because your maximum pressure is being limited. If you had a higher maximum pressure the 95% pressure number is a rough estimate of what fixed pressure you could use in CPAP mode.
Is the goal for the 99.5% measure to never reach the max pressure?
The real objective is to reduce the frequency of OA events to a reasonable number. The overall AHI treatment objective is to be less than 5 for AHI, but many people can achieve less than 1.0 for AHI.
Can you tell from the Time at Pressure chart approximately how much higher the max pressure should be set? In the graph, Time at Pressure for 9.6 (max pressure) = 44 minutes.
I don't use that time at pressure chart at all. I just look at the pressure when each OA event occurs.
"Can you help me understand why the proportion of apneas is inverted between the in-lab with no CPAP (more central apneas) and the at-home with CPAP (more obstructive apneas)?"
No, the numbers you got on the sleep study are very strange compared to your CPAP treatment numbers. Normally what happens is that CA events are low in the sleep study, but then emerge when CPAP treatment at pressure is started. Your pattern seems to be the reverse. Your very high CA index in the study is a red flag. It is usually very hard to treat central apnea with a CPAP as the CPAP reduces obstructive apnea with pressure, and pressure often makes central apnea worse. I don't understand what you have. Your CPAP reported central apnea is quite good, but your obstructive apnea is too high. So, I don't understand it, but the numbers indicate you can reduce your OA frequency with more pressure. Or, if they are being induced by the head neck position, a soft collar may help too.
"Are at-home CPAP machines usually accurate in distinguishing between obstructive and central apneas?"
Both my sleep study and that of my wife's were done with at home kits - Phillips Alice NightOne. We have no reason to think that they were inaccurate. I was diagnosed with an AHI of around 37, and my wife at 83. Interestingly her AHI under treatment with a ResMed S9 is 0.58. I suffer from central apnea and I cannot get that low. But, with my latest adjustments I am getting 0.86 for AHI.
"Can you tell from flow rate patterns with some certainty when you are awake or asleep?"
That is not easy to do. If you expand the flow rate chart so you can see each breath you should see that each breath is regular and almost identical to each other when you are asleep. Another clue is the leak rate chart. Leaks generally occur when you are asleep. If you see the leak rate chart trending around zero it is a hint that you may be awake.
All in all, I would stick with my previous suggestion to increase the maximum and minimum pressure to see if things improve. I expect they will. Do it in steps that you are comfortable with. Post your Daily report with the increased settings and I can comment. The first chart you posted with the pressure, flow, etc is enough. At this point you are mainly interested in the event chart and what the pressure is at when events occur.
Your answers have been incredibly helpful. A great big THANK YOU! I will post again when I have something to report or have more questions.
How are you making out? Have you sorted out your issues with the AirSense 11? I have been trying to think of reasons why it would stay at a fixed pressure. If the AutoRamp mode is turned on it will stay at a fixed pressure (Start Ramp Pressure) until it determines you are asleep. If you can post a daily screen from the A11 it may be helpful in determining what may be wrong with it.
Good Morning Sierra! Thanks for checking in. I am so appreciative of your continuing to help me troubleshoot my CPAP therapy.
I’m still using the S9 to ‘dial in’ the correct min/max pressures. I haven’t wanted to complicate matters by using the Airsense 11. As soon as I feel the min/max pressure is close to optimal on the S9, I plan to switch over to the AS11. I may try the AS11 for a night or two in order to provide you with data to help troubleshoot the problem.
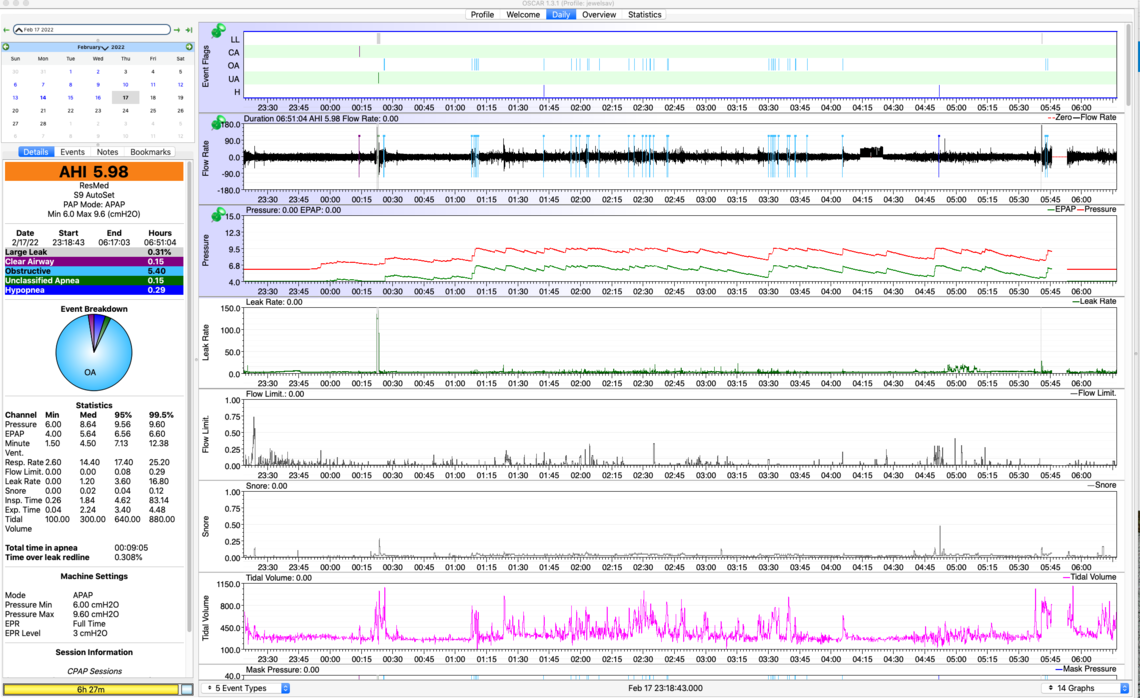
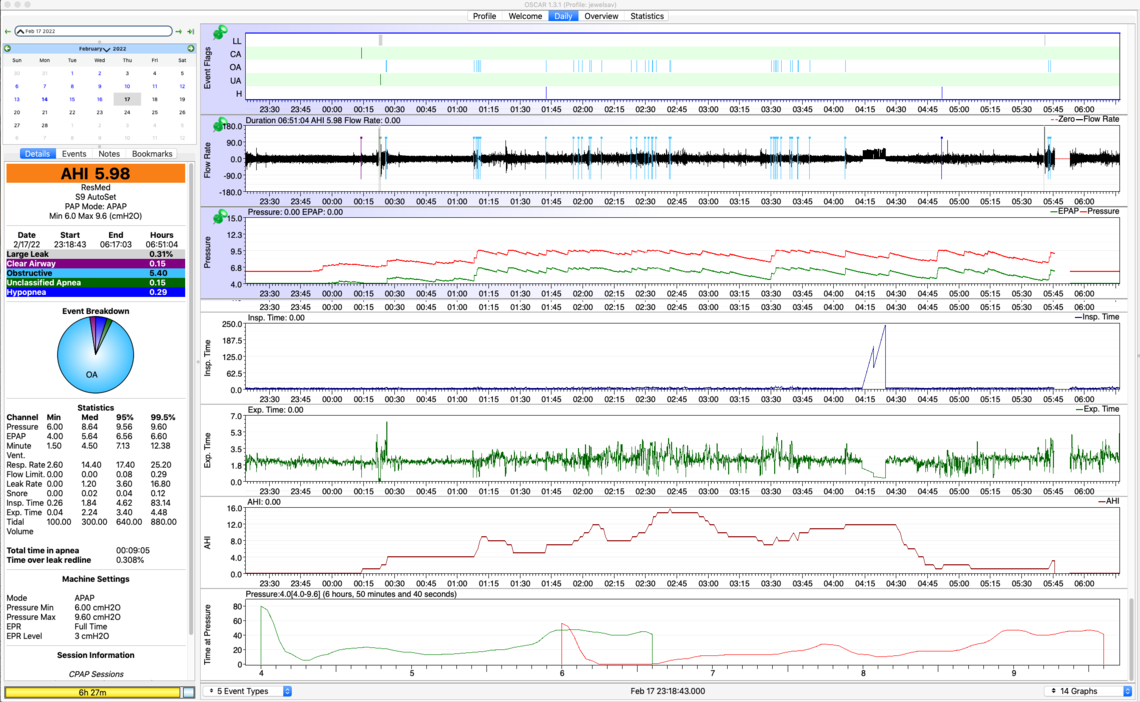
Thanks for offering your suggestion about why the AS11 may be at a fixed pressure. The problem is it stays at the MAX PRESSURE, not the START RAMP PRESSURE, despite the fact that I've set a min pressure (6.0) and a max pressure (9.4). (See OSCAR data for Feb 10 below.) I have spoken with both the vendor and with ResMed customer support about the fixed max pressure, but have gotten nowhere.
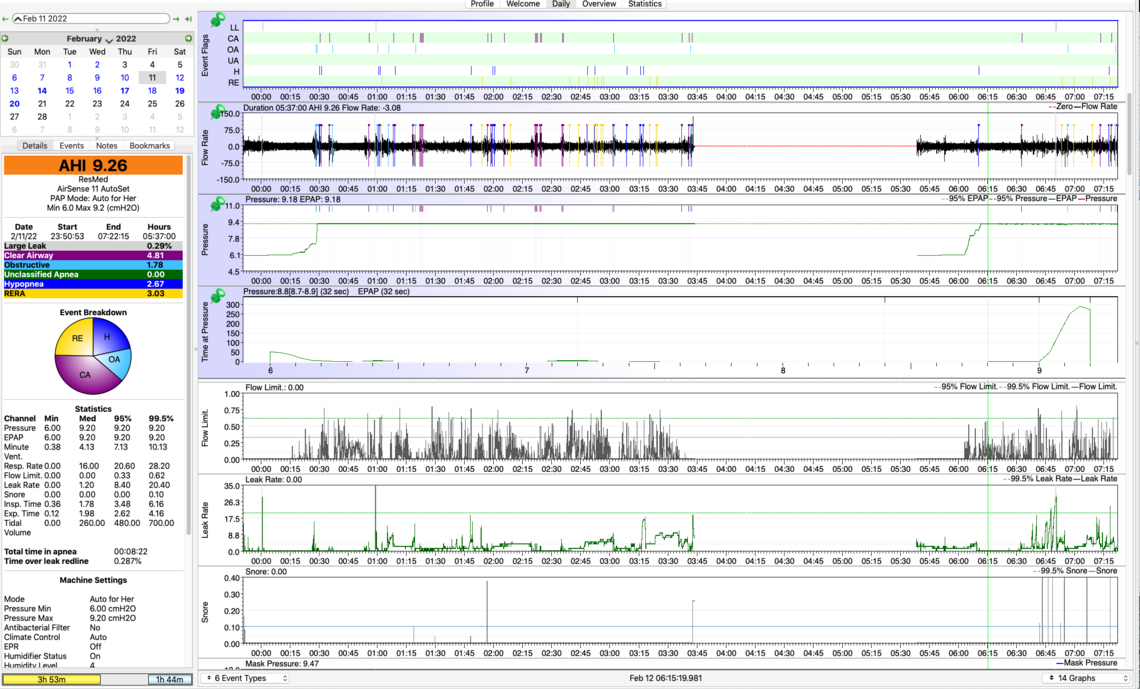
On Feb 11, I mistakenly set Mask = Pillows instead of Nasal (Air Fit N30i). Would this setting account for the large Flow Limit (typically my Flow Limit on the S9 is <.20)? What effect would the inaccurate "Pillow" setting have on pressure delivered? (See OSCAR data for Feb 11 below.)
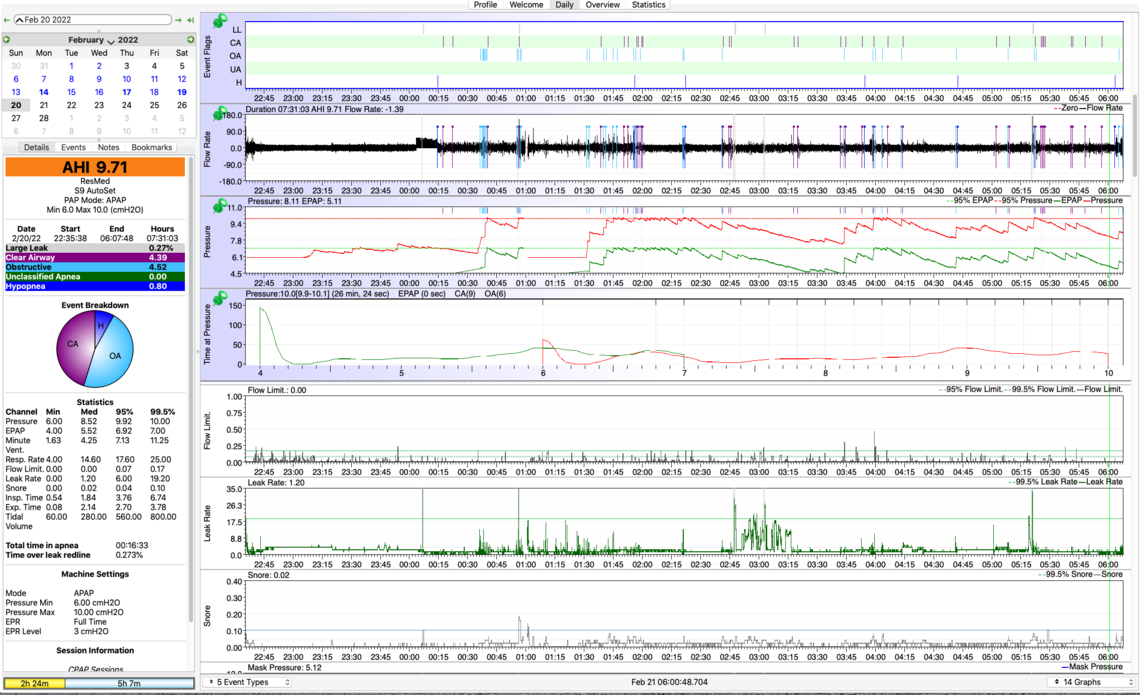
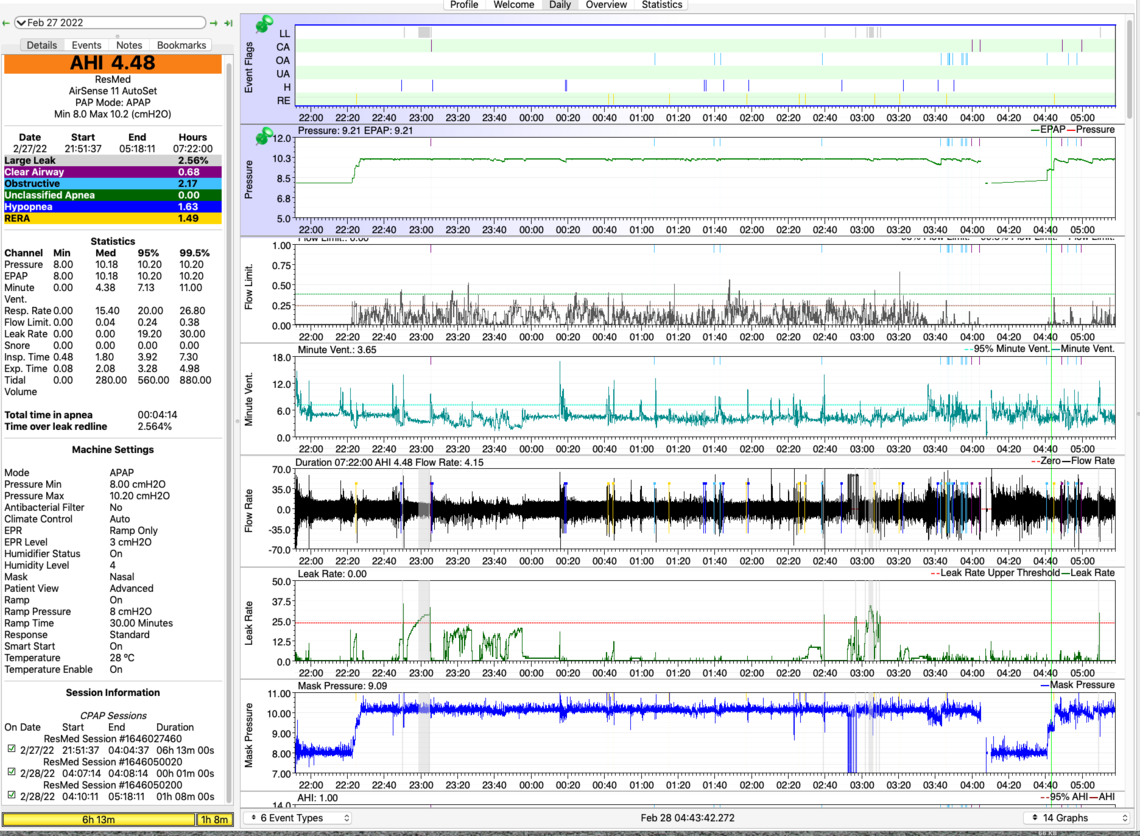
In terms of my CPAP treatment, I’ve been doing well following your protocol. I have been increasing the max pressure by .2 cm every 2-3 nights. With these tiny increments, I am able to avoid morning headaches caused by too big a jump in pressure. As of Feb 20, I’m up to max pressure = 10.0 (see OSCAR data for Feb 20 below).
Results: I got 6.5 hr sleep (vs 3-4 hrs), woke up just once last night (vs 3-7x), but awoke and stayed awake from 1-2 AM (typical not to fall back to sleep quickly). I felt moderately refreshed this morning (vs feeling very tired upon waking).
It may sound obvious to you, but your advice to observe at what pressure apneas were occurring was a key to my understanding how to determine optimal pressures. I’m still experiencing most apneas (OA and CA) @ max pressure, so I will continue to slowly increase the max pressure. I’m watching central apneas closely to see if they increase.
Two questions: Once I establish a max pressure (let’s say, 10.5), why would increasing the min pressure reduce apneas? What is a typical pressure range – 2 or 3 cm (ex: min=7.0, max=10.5)?
This forum is providing me with support and useful information to achieve effective CPAP therapy, which I’m not finding anywhere else. It would be much more frustrating and lonely without myapnea.org. I am grateful.
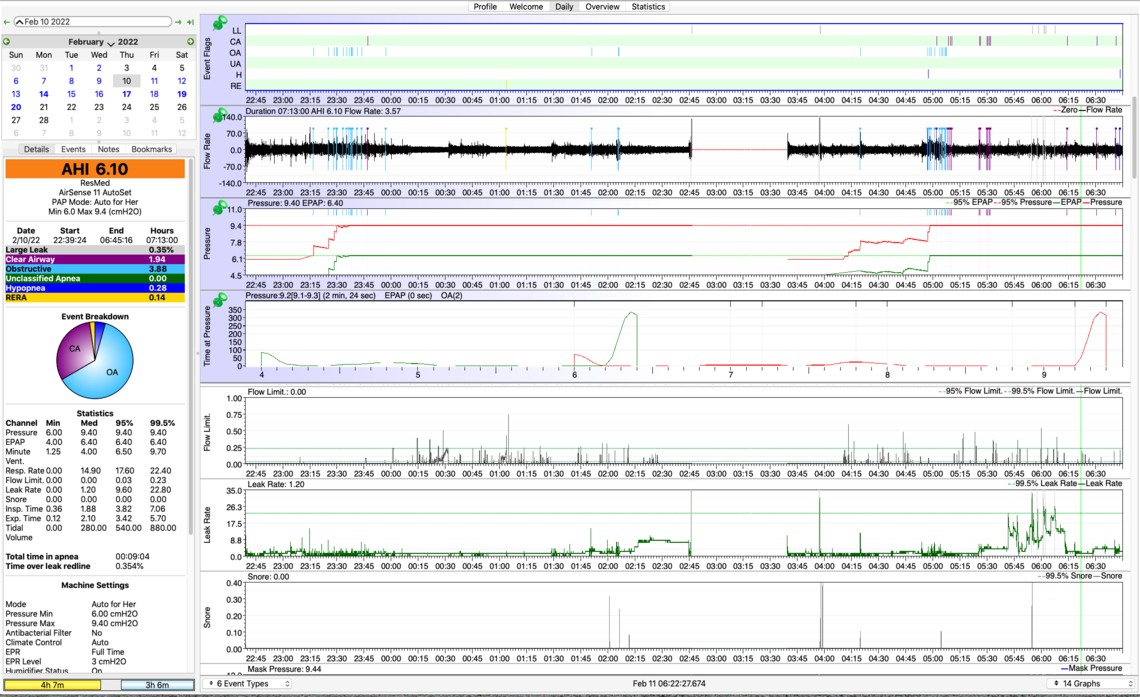
First on the AirSense 11 machine, I think the issue is that you have the machine set in the "For Her" mode. This algorithm is different than the standard Auto mode. It increases pressure faster and holds it higher longer. I see that it also adjusts the minimum pressure up. I suspect that is the reason you are seeing the pressure going up to maximum and staying there. This machine can be set to the standard Auto mode and then it should behave much more like the S9 in Auto mode. Here is a link to an article about the "For Her" mode. It is kind of long and complex, but if you skip down to the "AutoSet for Her Algorithm" section it explains what is being done differently. The article:
Obstructive Sleep Apnea in Women: Specific Issues and Interventions
On your S9 graphs I see quite a few central apnea events starting to show up. I think you may want to change strategy a bit. I would switch the EPR mode to Ramp Only, and lower your maximum pressure to 9 cm to see how you do there. The issue with using EPR full time is that if you have obstructive apnea events on the exhale part of the breath, the EPR is reducing the effective treatment pressure by the amount of the EPR used. If you get a reduction in the obstructive events with EPR turned off then I would continue to reduce the maximum pressure in small steps to see if you can find a pressure where OA's are not high, and CA's are also not high.
You asked about the purpose of increasing the minimum pressure. It can have benefits if you are having OA events at lower pressures before the machine can automatically increase the pressure to stop them. It also keep the pressure from cycling up and down so much during the night. When I was using the Auto mode I set the minimum pressure as high as only 1 cm less than the maximum. Then I switched to a fixed pressure when I decided what was the optimum, without using Auto mode.
Thank you for your quick response.
I will set the AS11 to 'Auto' Mode rather than 'Auto for Her' mode.
My husband tells me that the pattern of my apneas is that I inhale, then exhale, then there is a long pause before I inhale again. Would you consider this pattern to be 'apnea on exhale' or 'apnea on inhale'?
To clarify, if I just described 'apnea on exhale' you're suggesting (1) reset the EPR to 'Ramp Only' from 'Full Time 3', (2) reduce Max Pressure from 10.0 to 9.0, and (3) continue to reduce max pressure to get a minimum number of OAs and CAs. If I've described 'apnea on inhale', what EPR, Max Pressure, and other settings do you suggest?
Many thanks!
It is really hard to tell exactly when your apnea is happening. You can expand the flow chart until you can see each breath leading up to an obstructive apnea, and see if you can tell when it is happening. On this graph, up is inhale, and down is exhale. An apnea could start at the beginning, end, or during the inhale. I am not sure what that would sound like when you are sleeping. Also keep in mind this only applies to an obstructive apnea event. With a central event, you simply stop breathing with the airway open.
Yes, I would go back to a max pressure of 9 cm in the hope that without EPR your results will improve. Switch the EPR mode to Ramp Only, and leave it set at 3 cm. It will reduce pressure for comfort on exhale during the ramp period, but will stop when the ramp ends. What you are looking (hoping) for is that this will reduce the number of CA events you are having without increasing the number of OA events. If OA frequency is reasonable then you could try stepping it down some. If OA events are still high, you will probably have to increase the pressure some again.
What you are trying to do is reduce the pressure as much as you can without causing excessive obstructive events. Having EPR active on ramp only may help with that.
@Sierra, Last night I changed the settings on my Resmed Auto S9 to the ones you suggested. I was quite excited to see the results. However, the SD card did not record any data. So, I’ll have to wait another night to see how well those settings work. Darn it!
Settings...Min pressure: 6.0, Max pressure: 9.0, EPR: Ramp Only, EPR: Level 3, Sleep Quality was ON, The SD card was unlocked. The machine recorded it was used for 8 hrs
How I Felt...I woke up a bit groggy, with a slight tension in the front of my forehead, but no headache. Symptoms dissipated within an hour, but I’m feeling a bit tired.
I had this problem once before and simply unplugged and re-plugged the S9 to reset. Perhaps I need to do this every day. What do you think went wrong?
Did you get an AHI on the top display when you push the Info button? My wife uses an S9 machine and the one issue I have had occasionally is that the SD card is not fully inserted. The location of the slot and how it works can make it look like it is fully inserted when it is not. When it is fully inserted you should get a "Please Wait- SD card in use...." message that stays up for quite a long time, before it can be used.
If an AHI was recorded you should get some idea how well it worked.
When I insert the SD card, the message reads "Reading the SD card, please wait". The message disappears after 10 seconds, and on past nights, the SD card was filled with data by the morning. Last night, I got the same message, so I assumed all was well. AHI = 7.4 last night vs. an average for 11 previous nights of AHI=8.23 (range 3.43 - 16.03). I will post again when I have data with the new settings. Thanks for your help.
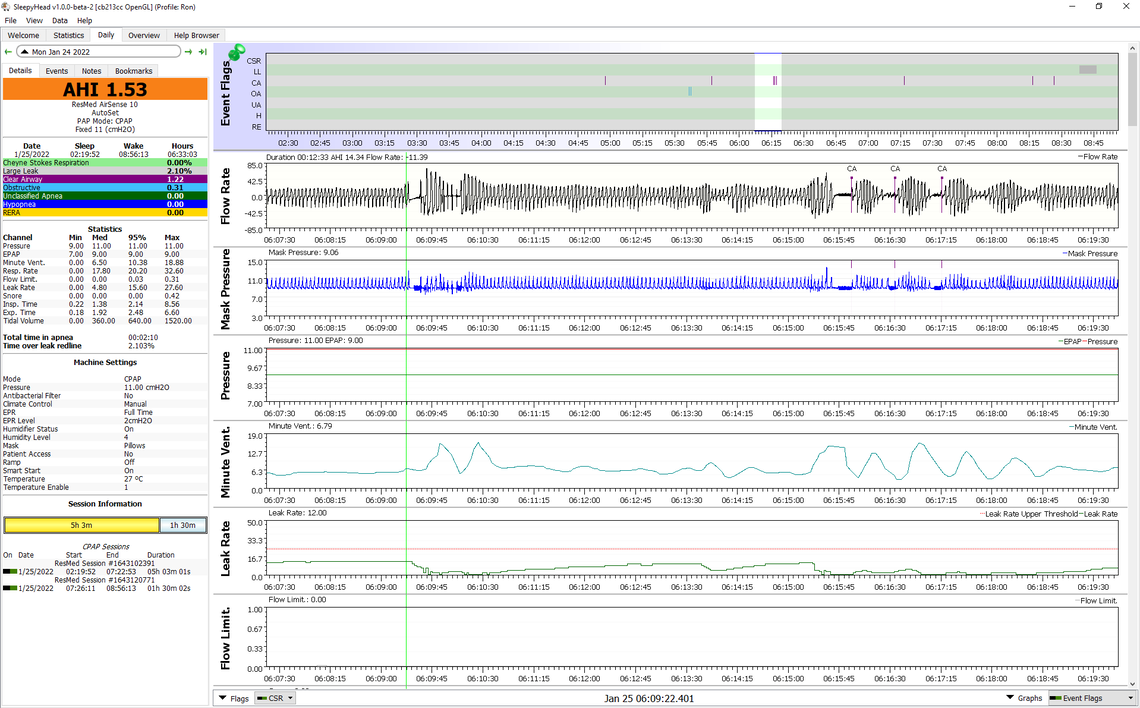
Your more recent Daily graphs are showing a much higher incidence of CA or central apnea events. Sometimes these events occur when CPAP treatment has been started, and are primarily due to the increased pressure of the CPAP upsetting the breathing control system. In these cases the CSA is called treatment emergent central apnea. In most cases this effect goes away in 6-8 weeks after treatment is started.
In an earlier post you said that your sleep study indicated a very high proportion of CSA events. That is a bit unusual in that no pressure is used during the sleep study test. And the first OSCAR report you posted showed very little CSA which was unusual considering the sleep study outcome. However now you are showing more CSA. This makes me a little less optimistic that minimizing pressure for your treatment may bring your AHI down, or at least the central part of it. You should have a look at the article at the link below to see if any of the causes of central apnea may apply to you. I have seen outcomes from people that live at high altitudes have issues with central apnea for example. There are heart conditions that may lead to central apnea. And there are medications which can cause it as well. The main ones are opiates. I have never taken them, but I do take a beta blocker (bisoprolol) for my blood pressure. It slows the heart rate and at least in my opinion must reduce blood flow rate. Reduced blood flow from heart conditions can cause central apnea. I discussed it with my doctor and convinced him to cut the amount of bisoprolol in half. I think he was skeptical but it did seem to help me. In any case have a read of the article to see if any of the causes may apply.
Central Sleep Apnea and Obstructive Sleep Apnea
The combination of obstructive and central sleep apnea is sometimes called complex apnea. The combination can be tough to deal with. More pressure can reduce the OA events, but cause more CA events. Some sleep clinics push people to move to a BiPAP machine if an APAP (like your S9 or A11) does not work. A BiPAP provides more pressure and more of a differential between inhale and exhale. Neither is really helpful for dealing with central apnea. If you do end up with persistent central apnea that cannot be treated with fine tuning your APAP, you may need to investigate an ASV (Adaptive Servo-Ventilator) with your sleep clinic. I recall you have an upcoming appointment, and that would be a good time to discuss. That said I still hope that there may be opportunity to further reduce your apnea without resorting to that option.
One of the patterns that I see very occasionally (once every month or two) is CSR ( Cheyne-Stokes Respiration). I believe that is associated with poorer blood circulation or perhaps other cardio issues. Here is what it looks like.
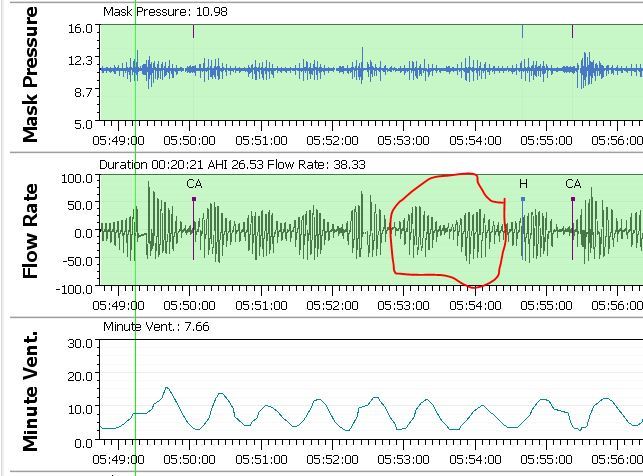
If you left click on your graphs repeatedly (or use the arrow keys) you can zoom in on the flow chart to see this level of detail. This may give you some help as to the nature of your central apnea. I click on the left end of the Minute Ventilation chart and move it up near the flow chart to see the relationship. When you see the Minute Ventilation cycling up and down that indicated unstable breathing control.
I hope that helps some. But, I have not given up on you being able to improve things with the machine you have now. The AirSense 11 is not really that much better than the S9 but you could give it a try in standard Auto mode. The biggest advantage of the A10 and A11 is that they have an AutoRamp feature. I see from your OSCAR chart that you must have that turned on. I like it.
@Sierra, Thank you very very much for taking the time to help me sort out my apneas and CPAP treatment.
OCCURRENCE OF CA's I don't think CAs have gone up with increased max pressure. In fact they appear to have gone down over time, with 2 notable exceptions (noted in yellow). Please let me know if I've interpreted the data wrong. Here is a google sheet from Feb 1 - Feb 20 with max pressure, CA, AHI (reported by CPAP machine) and AHI (manually corrected to subtract apneas when I was awake). https://docs.google.com/spreadsheets/d/122kA5EJiwUXKilxmQYR6FRRvGxNRau7Tufwssk3-Etw/edit?usp=sharing
Trying to add more information and respond to your suggestions...
BACKGROUND MEDICAL CONDITIONS Your exploration of what is causing the apneas are very welcome. I don't take any drugs other than levothyroxine for hypothyroidism. I live at sea level (San Francisco Bay Area). My blood pressure is 116/69, resting heart rate ~63. In December, I had my first and only episode of heart arrhythmia (not atrial fibrillation, something else) which was severe enough to send me to the emergency room. Doctors said the arrhythmia episode was due to sleep apnea. (Hence my heightened urgency to figure this out!) A follow up echocardiogram and a 14-day Zio patch (24/7 heart monitor) revealed no problem with my heart. The sleep study tested negative for Cheyne-Stokes. That distinctive pattern in my Oscar charts may be when I was awake, trying to get back to sleep. Some nights I can't get back to sleep for 1-3 hr. During the awake time, the CPAP machine is still counting irregular breathing (normal for being awake) as apneas. I manually subtract these out to get a more accurate AHI.
What is the difference between the AS11 AutoRamp and the S9 AutoRamp? I like that feature on the S9 too.
I'm not sure what time zone you are in. If it's not too late in the evening...what settings would you recommend if I try the AS11 tonight? If too late to respond, I'll await your suggestion tomorrow and try the AS11 tomorrow night. My hesitation is that last time I tried the AS11 and set min/max pressure, it only delivered max pressure, and I woke up with a headache.
Sending a great big thank you.
A quick response to try to catch you tonight. I am pretty sure the issue with the A11 is that it is in the "For Her Auto" mode. If you switch it back to the regular Auto mode it should behave like the S9 if all the settings are the same. That chart you posted showed it controlling pressure early in the night and then going to the max pressure and staying there. However, if you don't want to take a chance on it overnight, then perhaps try it for an afternoon nap.
You are obviously taking this very seriously and tracking your results. It reminds me of my early days trying to sort out my issues where I was also using a spreadsheet to track things. If you think things are getting better with respect to central apneas then that is a good sign. They may be treatment induced and are going away. Lets hope! One of the things I have found with my apnea which is about 2/3rds central on most nights, is how erratic it is. In the space of a week I can have a night over 2.0 AHI and another night at 0 AHI. I just take comfort that I am now averaging less than 1.0 for AHI.
I have never tried to correct my AHI for apnea when I am awake instead of sleeping. I think it does happen. Some call it "sleep wake junk". Fortunately I sleep well enough that I have never thought it was significant for me.
On the Cheyne Stokes Respiration I did some checking. It is reported and highlighted in green on the A10 machine and I assume the A11. It appears that feature was not in the S9. However it is easy to recognize by just looking at the flow chart zoomed in right before central events occur. It also helps to put the Minute Ventilation beside the Flow graph. Here is an example of what it looks like. Towards the left there are two events which did not last long enough to be flagged. I suspect they were obstructive events. This disturbs the breathing and you can see the Minute Ventilation gets upset. It settles out and then gets disturbed again. This results in three CA events in a row. When you see that wave in the breathing I am breathing deeper and deeper and then more and more shallow. It can start another cycle or cause a central. In any case that to me is what happens when the breathing control system is unstable. If it repeats enough times it gets flagged as CSR. When the breathing goes in regular cycles like this I believe I am asleep. My thoughts would be to look for times when you are seeing a number of CA events to see if there is any pattern like this. Or, look at the time after an obstructive event to see if breathing starts to cycle.
The AutoRamp on the A10 and A11 is really a hold, rather than a ramp. You select a ramp start pressure and the AutoRamp holds the pressure at that level until you fall asleep, then it ramps up to the minimum pressure. If you don't fall asleep in 30 minutes it ramps the pressure up anyway. I find it a comfortable way to go to sleep as I can set the pressure at what I find comfortable. and not have the pressure ramping while I am still awake.
@Sierra, I received all your messages last night. If it wasn’t for your encouragement, I would not have tried using the AS11. But I did use it, and it went well. Barring any unforeseen occurrence, I will be using it from now on. S9 is still available as my backup.
SETTINGS CHANGES
I tried changing from EPR Full Level 3 to EPR Ramp Only, and lowered the max to 9.0 from 10.0 (min/max 6.0-9.0). The result of the EPR change when I was trying to fall asleep I couldn’t catch my breath, it was hard to exhale and I was starting to get a headache. So I re-engaged the EPR to Full Time Level 2 (had been Level 3), and increased the min/max back to 6.0-10.0. Then I was able to fall asleep.
I realize the goal is to set EPR to Ramp Only in order to lower the max (where apneas are occurring), but wondering how to do that without the discomfort, and without losing sleep at the beginning of the night. Is the min of 6.0 too low?
AWAKENINGS
I woke up briefly 3 times @ 1.40, 2.50 and ~4 AM (my usual is 2-7x), but was able to go back to sleep quickly. The peak of the night for apneas was 2.40 AM. Is that what woke me at 2.50? After 5.5 hrs of sleep (avg: 6.5 hr), I woke up a bit tired. Hopefully I’ll wake up refreshed one morning.
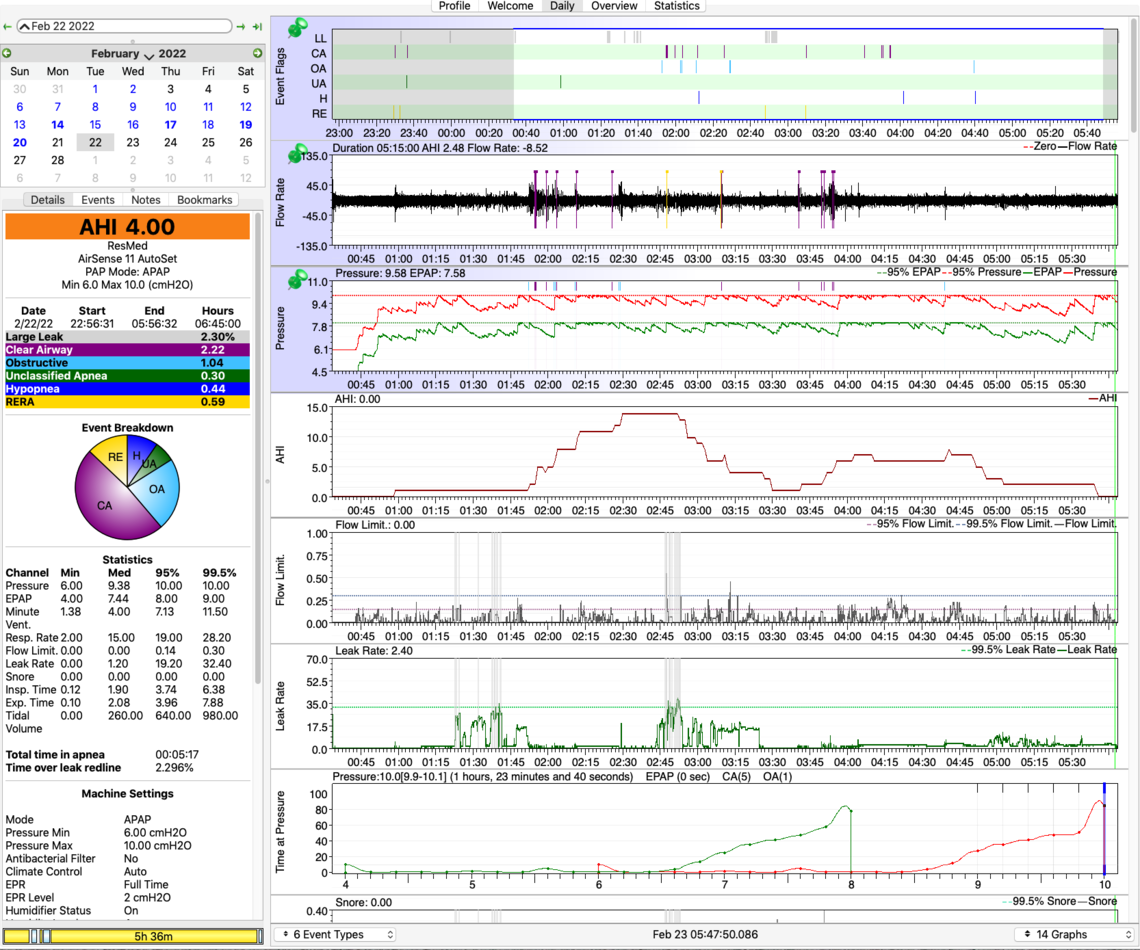
CPAP STATS
Last night’s stats show OAs are down, CAs are up: (12-day avg in parentheses): OA=1.04 (2.78), CA=2.22 (1.43), H=0.44 (0.70), RERA=0.59 (no avg available).
AHI = 4.0 (avg=4.14 when awake apneas removed); machine-reported avg: 7.90. I’m not yet concluding that AS11 can tell the difference between asleep/awake, since I didn’t have long stretches of being awake last night. But it would be nice if AS11 could do that.
I know most people don’t look at the ‘Time at Pressure’ chart, but I’ve found it useful. I spent 79 minutes at max pressure 10.0. Events occurred at these max pressures:
Max 9.0 OA: 1, CA: 0
Max 9.2 OA: 0, CA: 3
Max 9.4 OA: 0, CA: 1
Max 9.6 OA: 4, CA: 4
Max 9.8 OA: 1, CA: 0
Max 10.0 OA: 1, CA: 5
As you’ve mentioned, the trick is to strike a balance when raising max pressure between reducing OAs and increasing CAs. Would you suggest continuing to slowly increase the max in order to reduce OAs at the cost of increasing CAs? Would that pattern make the case for getting an ASV rather than an APAP?
What settings would you suggest going forward?
THANK YOU!!
First, it is good that the A11 is now working better. I am not certain the setup for the AutoRamp is quite right yet. You have the display zoomed in somewhat so I can't see the pressures at the start of the night. In any case this is how I would set up the AutoRamp. Here is a rundown on what I would suggest for settings:
Mode - AutoSet Minimum Pressure - 6 cm (but I would suggest trying 7 cm) Maximum Pressure - 10 cm (but you may be able to reduce that after some experience) Ramp Time - Auto Start Pressure - 6 cm (but I would suggest trying 7 cm, Start Pressure cannot be above Minimum Pressure) EPR - On EPR Type - Ramp Only EPR Level - 3 cm
When you have the Ramp Time set to Auto, it will hold the pressure at the Start Pressure level of 6 cm. But as I suggested setting minimum pressure and the Ramp Start at 7 cm may be more comfortable and more effective. With the EPRR on, set to Ramp Only, and the EPR Level at 3 cm, it will reduce the exhale pressure by 3 cm until the auto ramp decides you are asleep (up to a maximum of 30 minutes). However when the Ramp Start and Minimum pressure is at 6 cm, it cannot reduce the pressure any lower than 4 cm as that is the lower limit on the machine. So you will only get an EPR of 2 cm. However if you start at 7 cm, then you will get the full 3 cm EPR. If you move the Mask Pressure graph up you can see the pressure being reduced on each exhale, and then flattening out once you go to sleep. When set up like this it should be easy to breath without restriction while you are going to sleep. I find a higher pressure makes it easier. My Ramp Start pressure is 9 cm. Looking at your results it seems you pressure never goes below 8 cm, so you minimum and Ramp Start could be set as high as 8 cm. That would make breathing easier when going to sleep.
Once you fall asleep the machine will stop reducing the pressure on exhale. The hope is that the pressure will not be as high however, and the pressure does not go so high in auto. The overall object with doing this is to control the OA events without having the pressure go as high. And if the pressure does not go as high, then hopefully the CA events will be reduced too.
If a sweet spot is not achieved, then there is one more adjustment that could be tried. That would be to switch the machine into fixed pressure CPAP mode. Then you adjust the pressure up and down to try and find a sweet spot where both OA and CA frequency is low. But, I would exhaust the settings in Auto first before trying that.
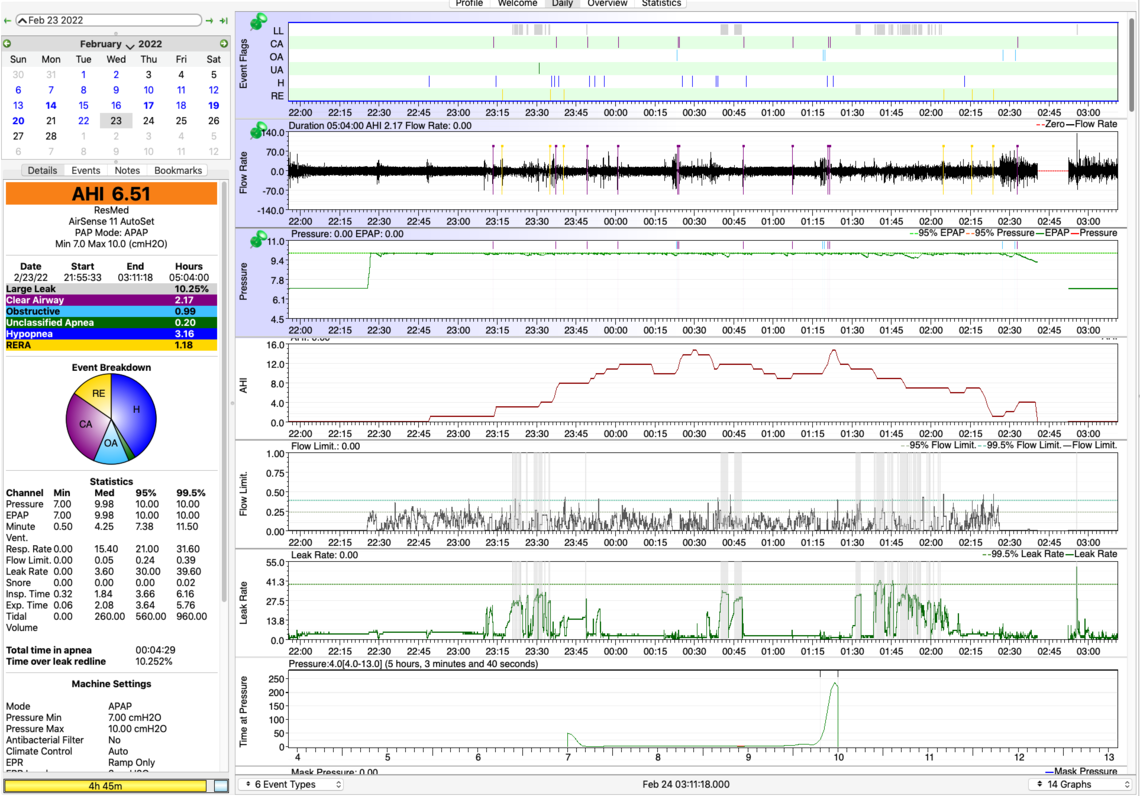
@Sierra, As you suggested, I increased AutoSet Min Pressure to 7.0, and EPR=Ramp Only. It was quite comfortable while falling asleep. See results below.
Unfortunately, my cat made a clatter in the closet at around 2.30 AM which woke me. My nose had gotten stuffed up, so I couldn’t breathe through the mask. I discontinued CPAP at that point. Yet another ‘this never happened before’ event: stuffed up nose. As each ‘never happened before’ event occurs, I check it off my list and feel thankful that I’m one step closer to finding the right CPAP settings for me.
Results: AHI was 6.51. An AHI comprised of CA = 2.17 and OA = .99 would be a very good night for me. However, the AHI of 6.51 also contains H=3.16 + RERA=1.18. Is there a way to tell if the Hs and Rs are due to obstructive or central apnea? I see some Hs on the inhale, some on the exhale. Or are Hs and RERAs not very important?
After ramping up, pressure went to the max, 10.0, and stayed there.
Based on 22 nights, Oscar data show at max<10.0, CAs averaged 1.5. When max>10, the CA average doubled to 3.0. Conversely, at max<10.0, OAs averaged 4.0. When max>10, the OA average dropped in half to 2.2. There are only 3 days’ data at max=10.0, not enough to draw a conclusion at this point, just to suggest a possible trend. Will keep watching.
What settings do you suggest over the coming nights to continue to home in on the lowest possible CAs and OAs? Do you suggest maintaining the same settings for a few nights before making a change?
I’m encouraged by the progress we are making. I’m feeling a little better rested today than usual.
Yes, I think you are making progress. I would suggest some simple cosmetic things that will help make the OSCAR Daily report a little more useful.
You asked about the seriousness of hypopnea and RERA. I do consider them less harmful than full CA or OA apnea events. The issue with hypopnea events is that they can trigger pressure increases, which in turn can trigger CA events. My thoughts at this point would be to switch to a fixed pressure CPAP mode to see if you can get better results. I think I would start with a lower fixed pressure setting of 9 cm. Keep the EPR in ramp only and set at 3 cm. This would be a trial to see if that reduces CA events without increasing OA events by much. Then if that works, the next step would be to try EPR at full time, and then with increasing amounts of level. Start at 1 cm, 2 cm,... But, first I would try the fixed pressure of 9 cm. It may have to be adjusted a bit before bringing the EPR back into it. My experience is that EPR full time can reduce hypopnea, but I would leave that for now to see what fixed pressure only can achieve.
It is difficult to determine whether or not hypopnea events are central initiated or obstructive initiated. If they are central in nature then increasing pressure in response to them is not helpful. That is the reason for going to fixed pressure CPAP mode. But, if you want to explore, expand the scale before H events occur and see if you can see in cycling in the breathing flow rate pattern. It will also show on the Minute Ventilation graph with it cycling too.
Hope that helps some. Be patient, as I think this will take some time to sort out.
@Sierra, I took your suggestions about chart layout. Happy to make more changes if it makes interpretation easier.
PRESSURE SETTINGS
I’m still experimenting with increasing max very slowly until there are no apneas @max pressure. I’d also like to increase min pressure to create the minimum range before I go to a fixed pressure (9.0, as you suggest) so I can compare fixed 9.0 to an optimal tight min/max range.
LIFE WITH AIRSENSE 11
I’m experiencing no discomfort from CPAP with the AS11 and even slept for 5.5 hrs without interruption last night until 3.30 AM, then couldn’t get back to sleep as usual. That’s a record for me. I’m feeling less tired during the day as a result.
With AS11, ‘Minutes in Apnea’ has decreased from 10 to 5 min, but Large Leaks has gone up from ~1.5% to ~ 2.5%, with 2 nights as high as 10%. I’m using the same mask – Resmed Airfit N30i, which is very comfortable, and I don’t feel any leaks while awake. Is 2.5% significant? Not sure how to fix the problem.
OSCAR CHART QUESTIONS
What is the relationship among Flow Limit, Minute Vent, Flow Rate and apneas? I’m trying to observe which occurs in what order. How do these metrics explain what is happening when CA and H events occur? Do you see any patterns of when OAs, CAs and H’s are occurring and how to reduce them? Or do we need more data?
Is there a way to remove sleep/wake junk (SWJ) data from Oscar charts at times you know you were awake? If I can’t remove the SWJ data, is there some way to denote on the charts the times I am awake?
A new day is dawning when I feel like a human again. Thank you so much!
Yes, that is a reasonable way to go. The advantage of having the machine in auto is that on each night you can see what the impact is of different pressures. The only thing that I would caution you with is that the hypopnea events may be increasing the pressure higher than it needs to be. At some point you could try switching the EPR to full time at 1 or 2 cm to see if that reduces the frequency of hypopnea events and hopefully in turn reduces the pressure in auto.
When you go to manual fixed pressure mode adjustment takes more time as you really need to leave it at one pressure for a week or so to determine that the impact is.
In any case this report is more encouraging with the OA frequency being higher than the CA. This suggests there is room for more pressure. When I got to this point I found that the tradeoff point was 11 cm of pressure. But each of us is different in that respect. The other hope is that you may be getting used to the higher pressure without it causing more CA events. This is what happens in some cases.
Have you tried the AutoRamp yet? If find that to be a very comfortable way to go as you do not have to guess how long it will take you to go to sleep. The machine decides when you go to sleep and then puts it into auto mode and discontinues the EPR when it is ramp only.
Thank you for your encouragement!
Just to confirm...you mention "The advantage of having the machine in auto is that on each night you can see what the impact is of different pressures." When you say 'auto' are you referring to the Mode Setting, which is on AutoSet, with the current Pressure Range: 8.0-10.2?
And, when I set the A11 to AutoRamp, are these the best EPR settings:
EPR: ON; EPR Type: Ramp Only; EPR Level: 3
Thanks a million!
Yes, when I said the advantage of having the machine in Auto was in reference to the AutoSet mode that lets the machine vary the pressure during the night.
The settings I would suggest for an Auto Ramp:
*The Start Pressure can be as high as your minimum pressure if 7 cm is not enough to feel comfortable.
Here’s an update…
I have officially used my Resmed Airsense 11 for 21 consecutive nights for >4 hrs and have a doctor’s appointment next week to confirm my compliance, so my insurance company will pay for the AS11 and consumables.
I have gradually increased min and max pressures over 3 weeks (see spreadsheet). The results (7-day averages):
AHI 4.40
Obstructive .94
Central 1.43
Hypopnea 1.87
My sleep dr seemed amazed that I achieved this AHI, given my January 2022 sleep study AHI of 79. He was surprised the CAs were low, given almost 100% of my sleep study apneas were CAs.
When I increased the max pressure from 10.4 to 10.6, OA, CA and H all decreased. I’m probably close to that tradeoff point you mentioned Sierra. If I increase max pressure, OA may go down and CA and H may go up. Will continue to make small pressure changes and hold them for awhile before making additional changes.
The AHI numbers may be moving in the right direction, but I still wake up 2-5x/night, with the longest stretch lasting only 2-3 hrs. I never feel completely rested, but am feeling a bit better than I did a month ago.
It’s taking a lot of patience to change only 1 variable at a time and giving it sufficient time to work. I will continue dialing in max pressure and other settings for CPAP, and will be trying a few more things to improve sleep quality. I tried melatonin, but it didn’t work for me.
Does my experience match MyApnea members’ experiences? How long did you use CPAP before you started feeling well rested? I realize everyone is unique, but it helps to have a realistic expectation.
First, I have to say you are doing an amazing job in tracking your progress and keeping the detailed spreadsheets. In looking at the spreadsheets a couple of things jump out to me. First since Feb 28 when you increased maximum pressure to 10.4 cm the OA frequency with the exception of one night has been really good. The average is under 1.0. This suggests to me that 10.4 cm is probably enough to control most of the OA events. The second thing that jumps out is that when you were using the S9 machine with EPR at 3 cm full time your Hypopnea was much lower and looks like it is well under 1.0 compared to nearly 2 now with EPR on ramp only.
Putting this together this is what I would do. First switch the machine to fixed pressure CPAP mode. You are spending very little time at less than the maximum pressure, and gaining very little with increasing minimum pressure. You may as well go to one fixed pressure that you can control. My suggestion based on your spreadsheet data would be to try 10.4 cm for the single fixed pressure. I would try that for a couple of nights just to confirm what it does. And next I would switch the EPR to Full Time with it set at 1.0 cm. Then if everything looks OK, increase the EPR to 2 cm and then 3 cm to find out if that will reduce the Hypopnea. The objective would be to only use enough EPR to reduce the Hypopnea but not increase the OA frequency.
And then after you determine the optimum EPR (the minimum you can get away with), then you could try lower fixed pressures to see what pressure you can get away with, without OA events going up. You may be able to get away with less than 10.4 and less might reduce the CA frequency.
You asked about sleep quality and I am a poor one to ask. I was diagnosed with an AHI of 37 or so, and next to zero CA events. But with treatment the CA problem emerged. And before diagnosis I was sleeping well (but snoring!). So, I did not see a big improvement in sleep quality, but I'm sure my wife appreciates the reduction in snoring. On the other hand, my wife was diagnosed at an AHI of 73 or so. Her treatment has brought her AHI down to 0.6 and she says she has an amazing improvement in sleep quality. But, I think my sleep quality is better than hers. She insists on having daily naps while I do my best to avoid naps during the day and try to sleep between 7 and 8 hours each night.
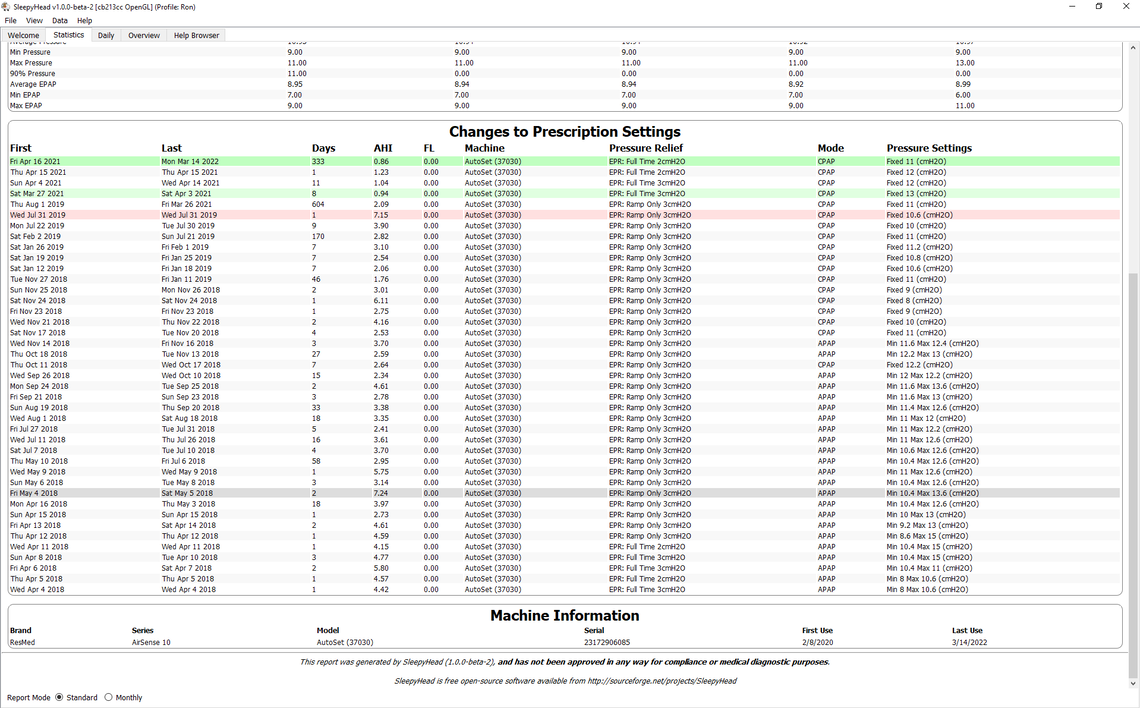
To give you some idea what it takes to get the machine optimized here is a screenshot of my statistics since day 1 with my A10 machine back in 2018. I kind of went through phases where I reduced the gap between min and max pressures. and then switched to a fixed pressure with many attempts to determine the best tradeoff pressure, and then finally to try EPR at 2 cm. I should probably try EPR at 1 cm but have not done that yet. As you can see, it is a long and winding road to get to some kind of optimum setting.
Thank you @Sierra. Brilliant insights! I really appreciate your feedback.
I've gotten so much from the MyApnea community, so I wanted to share some knowledge, even if it's just a tiny morsel.
Even when holding many variables steady, we are not robots, and AHI can vary for no apparent reason on some nights. It's important to tease out which AHI variations are due to a change in settings and which variations are due to random "noise". When I looked at AHI for individual nights, there was no way to make the distinction. Looking at a 7-day average, trends were more obvious.
I definitely saw that OAs were <1.0 when max pressure was 10.4 or more. But I didn't know how to make that actionable. Thanks to Sierra's experience, he recommended setting a 10.4 fixed max, then sequentially trying different EPR settings and seeing which worked best. Can't wait to try it.
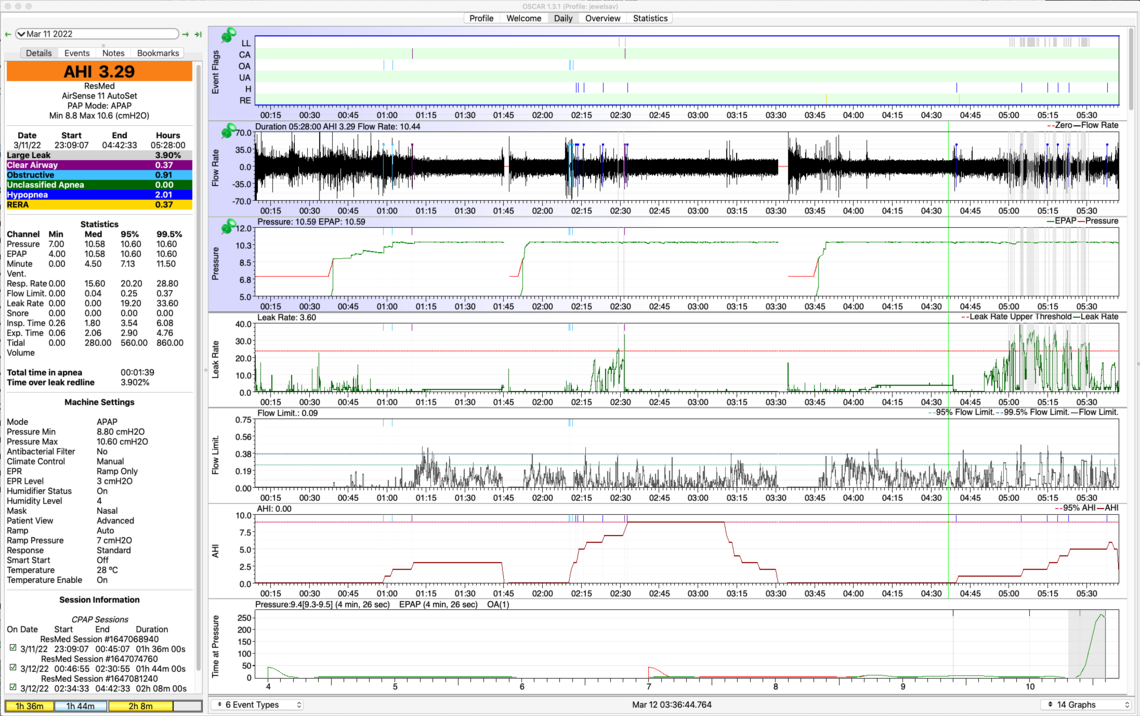
Time for an Update...
CPAP THERAPY
As you suggested @Sierra, I made a change on Mar 17 from Min/Max 8.8/10.6, EPR: Ramp to Fixed Pressure 10.4, EPR 1. After 1 week, AHI, OA, H and R are all down significantly. Yippee!! But CAs are up slightly. So, for the next week, I will try lowering the fixed pressure to 10.2, while maintaining EPR=1. See https://docs.google.com/spreadsheets/d/122kA5EJiwUXKilxmQYR6FRRvGxNRau7Tufwssk3-Etw/edit#gid=0 for details.
AHI down from 5.16 to 2.50
OA down from .48 to .37
H down from 2.14 to .77
R down from 1.91 to .53
CA up from .63 to .87
SLEEP QUALITY
Fortunately, my jumping out of bed like a ninja, and screaming like i'm in a horror movie have ceased. My parasomnia diminished to speaking in a conversational tone, my not waking up, and having no recollection of dreams (my husband reported the events). Then, at least for a week, all these events have disappearing altogether. We purchased a Wyze outdoor camera for ~ $35, mounted it with a wide angle view, so for the next few weeks I can see if I have sudden movements or outcries. I expect these behaviors/vocalizations may appear from time to time, but this is a vast improvement over events happening 2-3x/week. I had a preliminary diagnosis of RBD, but it (hopefully) will turn out to be pseudo-RBD with parasomnias brought on by sleep apnea and long term sleep deprivation.
I still wake up 2-3x/night, and get only 5-6 hours of sleep/night. I am waking up a tiny bit more refreshed. From reading others' experiences on this forum, I figure it may take weeks to months to feel less tired. Any suggestions are welcome.
DEALING WITH $#@&
My (excellent) sleep doctor referred me to a movement disorder neurologist within the same health organization (Stanford) to run some tests to determine if I have RBD. It took 3 weeks for the Stanford neurology department to decline the referral and tell me to contact them again in December 2022, at which time they "may or may not" schedule an appointment for me sometime in 2023. I emailed my sleep doctor and asked for a referral to UCSF (US News & World Reports rates the UCSF Neurology department #1 in the US). My dr's admin assistant (without even showing him my request) emailed me back that Stanford has a policy of not referring patients outside their system. Fortunately I had a zoom call with my dr yesterday. He was dismayed that there's such a policy (if there even is one, since he's never heard of it), and said simply "Why would I do that?"
Between the time I heard back from the ding-a-ling assistant until I saw the dr, I asked my primary care physician to make the referral, which she did within 24 hrs. As it turns out, my sleep dr and the UCSF neurologist are good friends and did their sleep fellowship together. My dr highly recommends the neurologist. He offered to pick up the phone and call her then and there to make the referral, if I wished. He lamented, "We both work for organizations with a lot of bureaucracy."
So while I feel I am in good hands both with the sleep dr (who gave me his direct email for future communication) and the neurologist, roadblocks and obstacles continue to suck the energy out of me on my journey to get a good night's sleep.
Another energy-drain is the DME. I have asked for six weeks for nasal cushion replacements for my Airfit N30i mask, which should be replaced every 2 weeks. I finally raised my voice, and was told they weren't in stock, the DME would have to order them (wouldn't give me a time estimate), and then they would have to go through the usual shipping channels (+1-2 weeks). Then I raised my voice even louder, screamed a bit, and lo and behold, the nasal cushion replacements arrived 3 days later. With the old cushion, I was experiencing a sore throat and headaches. I used a new cushion last night - woke up just fine.
Thanks for allowing me this one-time rant. I realize everyone on this forum has stories like these and worse. Why does it have to be this way? Sigh. I'm just so awfully tired of these nuisance roadblocks. This has already been a 3-yr journey to get to this point - I won't bore you with the details. But now I have the finish line in sight, thanks in part to the help you have generously and compassionately given me. I am truly grateful.
It looks to me that you are making very good progress on the total AHI number. My only suggestion is that you may want to try lowering the fixed pressure in larger steps than 0.2 cm. I have found that 0.2 cm is a pretty insignificant change and the impact of it can be really hard to determine in a reasonable length of time. The impact gets lost in the day to day noise in the results. I think I finally resorted to making 1 cm step changes to test the impact of it, and to see if I was going in the right direction. And when I get close then I started to make smaller refinements in pressure.
On the RBD @Biguglygremlin here is the expert. He suffers from it and has tried a number of things. Hopefully he will check in and provide comments. If not, then try making a new post on that specific topic.
Your experience with the DME sounds similar to what others report. Fortunately we don't seem to have anything similar to that in Canada, or at least not in our province. But, on the other hand unless you have private insurance there is no help provided by healthcare. You are basically on your own to buy a machine, and maintain the supplies.
This post is in response to people who likely have undiagnosed RBD. If you have dream enactments, especially vivid and often violent dreams that you remember when you are aroused by the enactment or in the morning, you likely have RBD. The frequency of dream enactments typically come on slowly over a few years, gradually increasing in frequency and intensity. The gold standard for diagnosis is an overnight sleep study with a polysomnogram. I agree with BigUglyGremlin's opinion that if a person is experiencing increasingly frequent, violent and vivid dreams over time, this sleep disorder is sufficient evidence to pursue treatment for the symptoms to avoid serious personal injures or injuring your sleep partner. RBD is not well known across the variety of medical practitioners which is a major challenge. My journey involves participating in clinical studies and keeping up with medical research publications. To learn more about RBD and consideration in participating in the largest clinical studies, go to naps-rbd.org and PPMIonline.org. Safe Travels
Thank you @RayRBD for your thoughtful response. I was originally going to wait until I had 2 months of data, but will post my very preliminary results now.
I started taking ashwaghanda 2 weeks ago. [Douglas Laboratories, Ayur-Ashwagandha, 300 mg, 1 capsule/night, 1-2 hrs before bedtime, $20.80 for 60 capsules.]. It can take up to 2 months to see the full effect. So far...
• AHI ~ 3.0
• 8/14 nights slept >7 hrs vs avg 5-6 hrs
• 12/14 nights woke up 2x/night vs 3-7x/night
• 14/14 nights longest period of sleep >2 hrs (average: 2.66 hrs) vs avg 1-2 hrs
• Time to fall asleep ~ 7 min vs avg 8 min (about the same as before)
• 0/14 nights RBD behaviors, movement or vocalizations, vs ~2-3 significant events/week (screaming, hurling self out of bed)
• Waking up relatively refreshed vs feeling run over by a truck
• No side effects
CAVEAT 1
There’s no way to separate the effects of ashwaghanda from the cumulative effect of being on correct CPAP therapy for one month. I may be predisposed to wanting ashwaghanda to work. But my skeptical husband noticed a difference immediately, and my sleep doctor did not believe the results were solely due to CPAP therapy.
It's possible that I had/have pseudo RBD due to long term sleep deprivation. It's also possible getting more REM sleep as a result of starting CPAP was responsible for the recent greater violence and greater frequency of RBD type behaviors I experienced before I started taking ashwaghanda. Time will tell.
CAVEAT 2
My highly trusted integrative physician recommended ashwaghanda for my sleep disturbances. This is a supplement which you don't need a prescription for. Supplements are not regulated, so quality can vary wildly. Douglas Laboratories is a very high quality firm, and it has the highest percentage of the active ingredient (7% withanolides vs 1.0-1.5% in other brands) of the ashwaghanda supplements I've seen. As with any therapy suggestion, please do your own research if you are considering taking this supplement. I'm not a medical professional, and I have only presented the experience of 1 patient (me).