I started CPAP therapy over 8 years ago and used a Phillips Respironics Remstar Pro C-Flex + System one. In May last year I got a Airsense 10. It took some time to get the settings right on that. When I don’t use a cpap, I can’t sleep. It’s not my possible. My body jolts me awake as soon as I start to fall asleep, presumably when I stop breathing. With the AirSense 10, no matter what the settings are (EPR, no EPR, autoset, cpap, lowering ramp, etc) I have nights (not every night) where my body does that. As I’m falling asleep I’ll jolt awake, heart racing. If I’m lucky it will happen once or twice that I’m aware of. I’ve had nights where it will last hours or in a couple of instances, all night. Im at a total loss. I can’t go back to the Phillips because of the recall. My results on my air score is always 100. It says I have 1.5 - 3 AHI per hour.
I never had anything like this in the 7 years I was using the system one. My sleep doc just kind of shrugs and says the reports look fine.
It might be useful to get another data point by checking your O2 levels while sleeping to determine whether you are desaturating. If so, you are likely experiencing apneas. You can do that yourself using an overnight recording oximeter. They are available online, and communicate via bluetooth with your smart phone.
If you aren’t having apneas, could you be experiencing hypnogogic jerks? And if you ARE having apneas, are they obstructives or centrals?
Thank you, I’ll look into that. I don’t know that I’d be able to tell what I’m looking at when I get results though. I did wonder about hypno jerks, but haven’t been able to find any info about ones that literally will last all night. Because they don’t seem to happen every night, I’ve just hoped it was something I’d get used to the not knowing when they’re going to happen is causing a lot of anxiety.
My suggestion would be to download OSCAR. It is a freeware program that will display your minute to minute data from the AirSense 10 SD card. Then you should be able to identify the type of event that is waking you up. OSCAR requires a SD card reader and PC or Mac.
Thank you, I’ve read about Oscar but when I looked at sample reports it was all Greek to me. Hopefully I can get some reports and maybe people on this forum can help me understand what I’m looking at. I also don’t know how to get my machine to record on the data card. This machine transmits my data over WiFi to my doctor.
As long as your machine is an AirSense 10 Elite or AutoSet it will record data on the SD card as long as it is inserted in the slot on the left side of the machine. Yes, OSCAR is essentially the same as SleepyHead. It flags all the events you have on a bar so you can see the time when the events occur. You can post them here to get some help reading them.
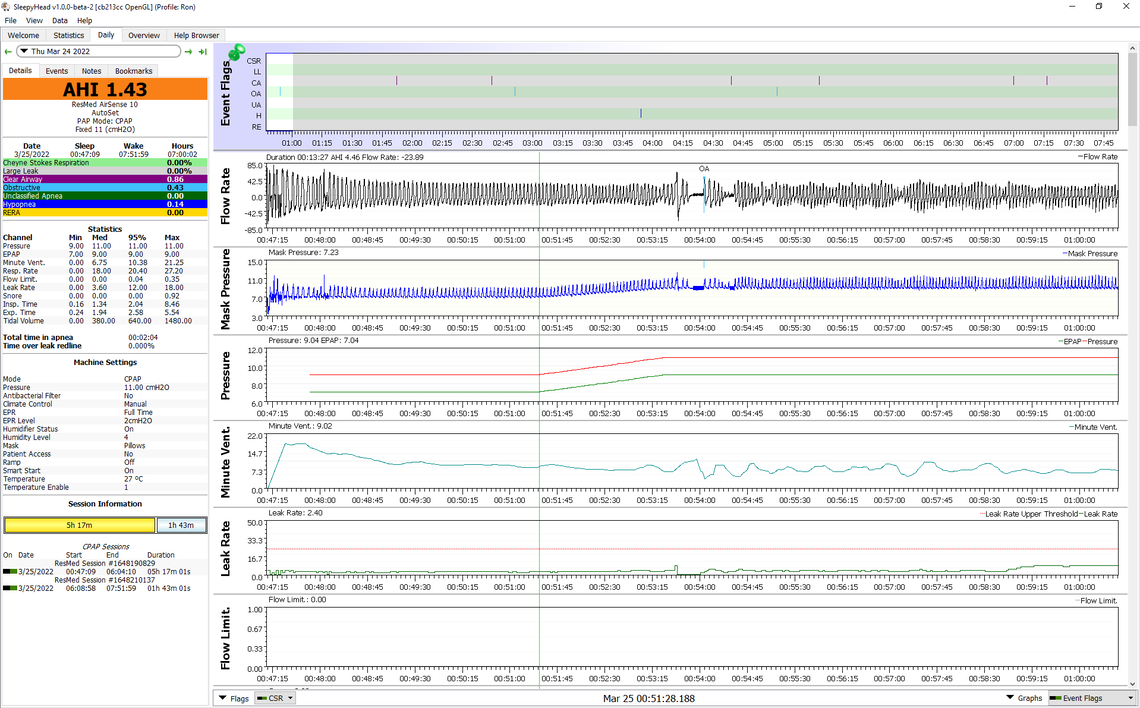
Here is an example of what an OSCAR (SleepyHead) looks like. This is one where I had an event shortly after going to sleep. If you left click repeatedly in the area of interest you can expand out the horizontal time scale. Where the green line is located is when the A10 decided I was asleep (ramp set to Auto for time) and then there is a ramp up in pressure. Very shortly after that I had a obstructive (OA) event, followed by one that did not last the 10 seconds to be flagged. This was a few days ago, and I have no recollection of waking up. But, it obviously disrupted my breathing pattern.
I can't thank you enough for taking the time to respond. I have results that I can share for last night, is there a way in OSCAR to share the image like you did above or or are you just taking a screen grab and posting? I would guess that the stopped breathing/body jolted awake gasping lasted around the first 40 min of me trying to sleep. I woke up occasionally to roll over, nudge a snoring partner, etc. but did not have those 'gasping' moments so it should show something useful on the reports.
Yes, that is a helpful chart. I find it easiest to just press the F12 key (on a PC) to save the screenshot. Watch the bottom right of the screen to see where it gets saved. Then you just use File Explorer to left click and drag the image file to a post. It is best to start a new full width window for the post by using the orange Write a Reply button in the bottom left. Otherwise it gets too small to read.
Have you tried the AutoSet mode instead of the fixed pressure CPAP mode? It seems like the fixed pressure you have is not high enough to prevent most of the obstructive apnea. I also like to set the "Ramp Time" to Auto, and then set the "Start Pressure" higher. I would suggest a minimum of 7 cm, but I use 9 cm. Using the Auto for time the machine will hold at that Start Pressure value until it senses you have gone to sleep. That may help avoid apnea events that could be occurring during the ramp period. The machine does not report events until after the ramp is over.
Those would be my initial thoughts. But, if you have some other days to post with the pressure set higher or in the AutoSet Mode. All your previous nights should be saved on the SD card.
Thanks, yes I have tried the AutoSet mode, I only changed it to the CPAP mode the other night thinking that was part of the problem, that perhaps the minimum was what was causing the issues. I'll try again though to be able to compare the reports. I cant remember if I had the ramp time in auto. It may have been originally and thought that was part of the problem.
The AutoSet mode is useful in determining how much pressure is necessary to control the obstructive apnea. The fixed pressure of 13 cm looks like it may be a little too low. Later when you know how much pressure you need, there can be advantages in using the fixed pressure CPAP mode. That is what I do. If you can post a daily screen when it was in AutoSet I may be able to suggest how much pressure is needed, especially if the maximum pressure was set higher than 13 cm.
You can tell when the Ramp is in Auto mode as the pressure will be flat until it ramps up when you go to sleep. With your issue of waking up gasping when you go to sleep there should be an advantage to having the pressure higher during ramp. The chart you posted looks like the ramp is starting very low at 4 cm pressure. That can be uncomfortable, and has limited impact on controlling apnea while you are going to sleep. If you look at the chart I posted you can see the flat pressure of 9 cm until it ramps up slightly to 11 cm. You may want to expand out that portion of your sleep to look at the flow in more detail to see if there are apnea events occurring during the ramp. They won't be flagged, but they may be there.
I tried the AutoSet last night, when I first got the AirSense, they had set the AutoSet at 4 - 14 which was way too low. I had changed it myself to 11 - 15, but when this waking/gasping/not breathing thing started again this past week is when I changed to CPAP 13 to hopefully mimic the system one that I never had problems with. Based on suggestions, last night I did AutoSet 12.8 - 18. I do not remember waking with that gasping problem, but I do remember waking up occasionally (not abnormal). I notice just as I'm falling asleep, both nights recorded show RERA event pretty early on and I'm wondering if that's the problem. Looking at my pressure range its clear I really need to leave it at least 13 - 18 if not higher. Still trying to learn OSCAR and make sense of what I'm looking at.
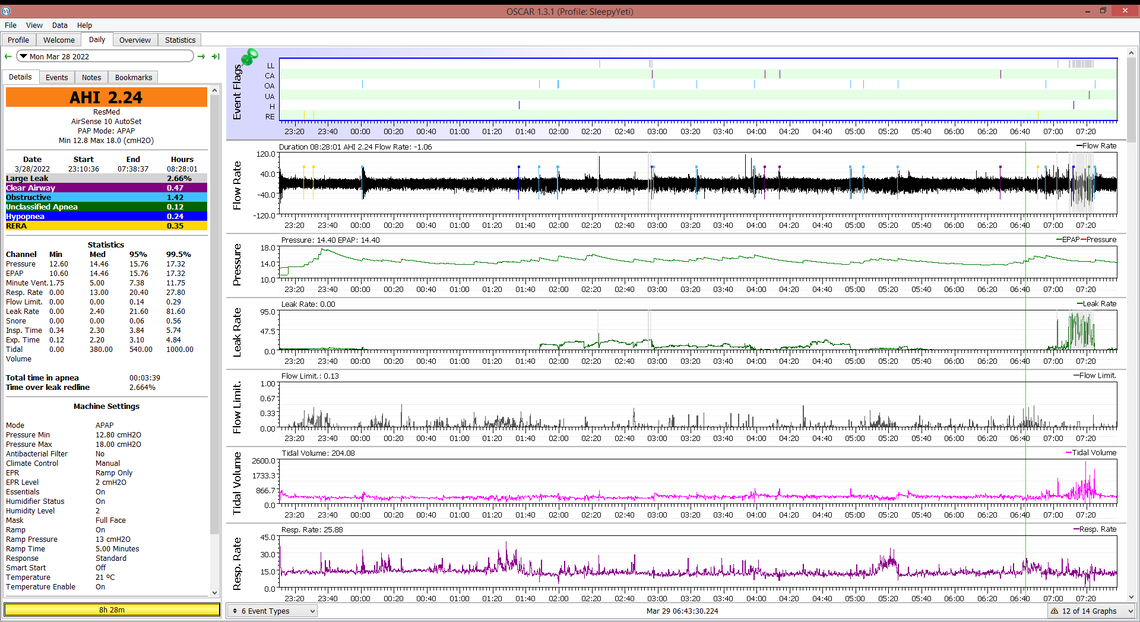
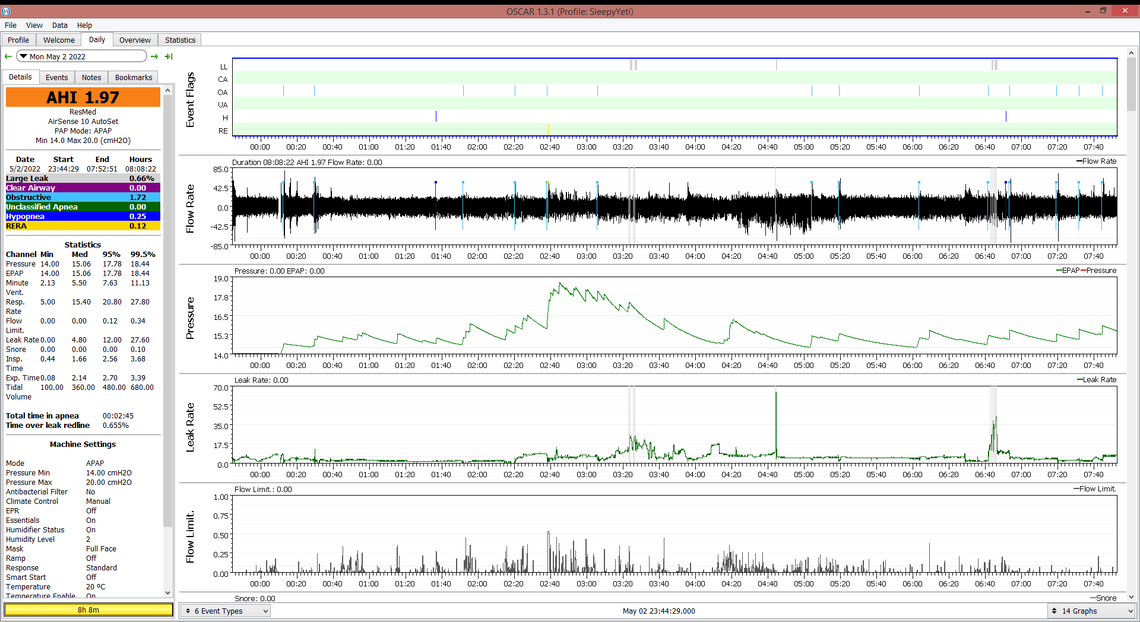
Based on this one night you do not seem to be hitting the max of 18 cm, so that max setting should be fine in AutoSet mode. Minimum pressure could be increased to 14 or 15. There is a rule of thumb that says if you want to go from auto mode to fixed CPAP mode the initial pressure setting should be the 95% pressure. So for you, based on one night that would suggest 15.8 cm. However, you may want to collect more data in Auto before you make that switch. Moving the start ramp up to 13 is good. If you move your minimum up I would also move the Ramp Start up too if you find it comfortable. I don't believe you can set the ramp start higher than the minimum though. But that said, I have not tried it. In any case it is not a good idea as you don't want the pressure to drop at the end of the ramp.
The idea of moving the ramp start pressure up is to prevent apnea events during the ramp period. The idea of moving the minimum pressure up is to prevent apnea events when the auto function ramps it down during the night. It also avoids the initial events needed to ramp up the pressure early in the night.
I see there are some CA or central events. It is hard to read the graphs accurately, but this may be due to the higher pressures. Once you get more data in Auto one possible advantage of switching to fixed CPAP mode is that it can limit the maximum pressure and possibly avoid some of the CA events.
I hope that helps some. l suggest you post more daily reports as you gain experience with the AutoSet mode. There is nothing totally consistent about CPAP treatment. It can be very misleading to make setting changes based on one night only. It is better to get a few and average them.
Since I posted last, I could use some help deciphering if anything is showing up in my Oscar reports. Based on another suggestion I tried raising my min to 15 and EPR 2, but I felt like that was making it worse so I stopped and change it to min 14, no Ramp and no EPR. Last night this 'sensation' happened again and I'm trying to get in the habit of turning off the machine when it happens so I can see if OSCAR shows anything helpful the next day. For last night I tried to really zero in on just when I turned off the machine. Anything stick out from the Flow? I have an appointment with a neurologist about this in case it is something related to hypnic jerks or something else but was hoping to really rule out that this isn't something sleep apnea settings related or machine related (this seemed to start when i started using the AirSense 10).
Any insight would be greatly appreciated. Still trying to learn OSCAR.
I'm looking at my results from last night and the night before and if I'm reading this right, looking at how much time my pressure goes above 13. I'm kind of perplexed why my doctor had my CPAP originally set at 13 and then with the new machine have a range of 4 - 14. I know my apnea could have gotten worse over the last 8+ years, I've definitely gained weight, but this seems like a big difference.
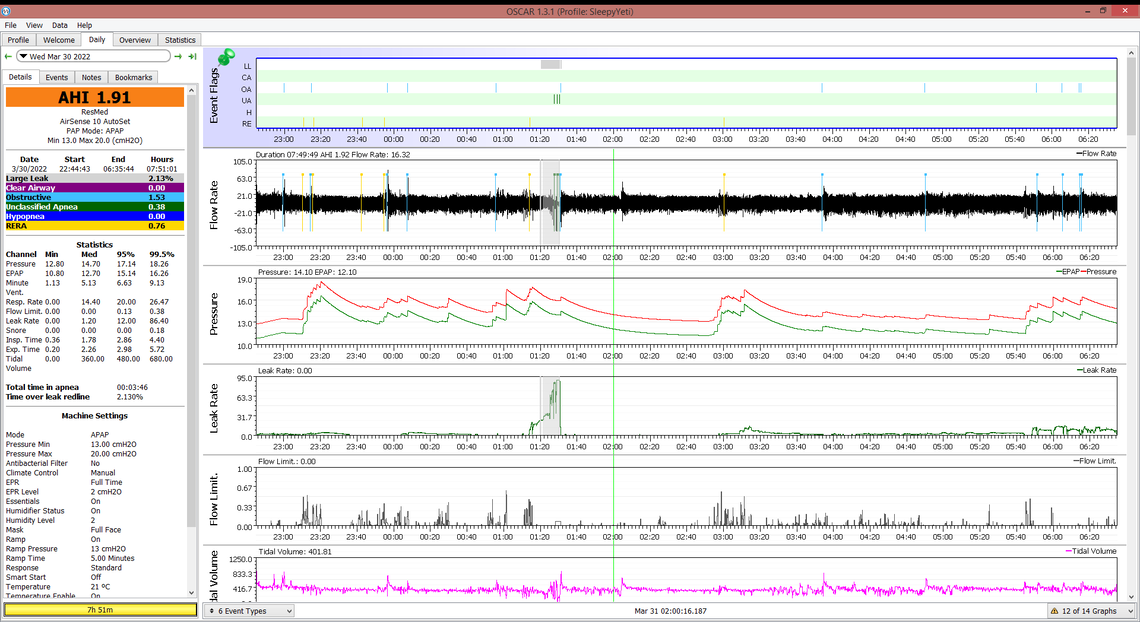
Sometimes you can get away with a lower pressure when it is fixed instead of in Auto. I think you would be better to leave it in Auto for a while to collect some more data before trying to go back to a fixed pressure. From what I can see you had the EPR in Ramp Only mode for your previous report, and now it is full time. In some people having the ramp on full time can increase the frequency of apnea events, and force the pressure to go higher. Because the pressure is reduced on exhale you can be getting an apnea event on exhale. Unless you are having a high frequency of hypopnea events I would switch your EPR back to Ramp Only to see if that reduces the pressure needed. I also see that your ramp time is set at 5 minutes. You may get better results with the ramp time set to "Auto". And it may also be of benefit to increase both the minimum pressure to 14, and the Ramp Start pressure to 14 cm as well.
That would be my thoughts for now.
Since I posted last, I tried making some changes, the other night I tried raising minimum to 15 with EPR full time 2 but that felt worse. Now my minimum pressure is 14, no Ramp, no EPR. I had a solid week and a half were it never happened. I have an appointment on the books with a neurologist in July but really hoping to just eliminate that this is being caused by apnea or the machine itself. I haven't been very successful. I'm trying to learn OSCAR but its still all greek to me. Based on a suggestion I tried turning off my machine when it happened last night so that I could really see what OSCAR is recording when it happens instead of trying to guess based on the time.
If anything is jumping out or other suggestions so that I can at least rule out its apnea/machine related.
Comments:
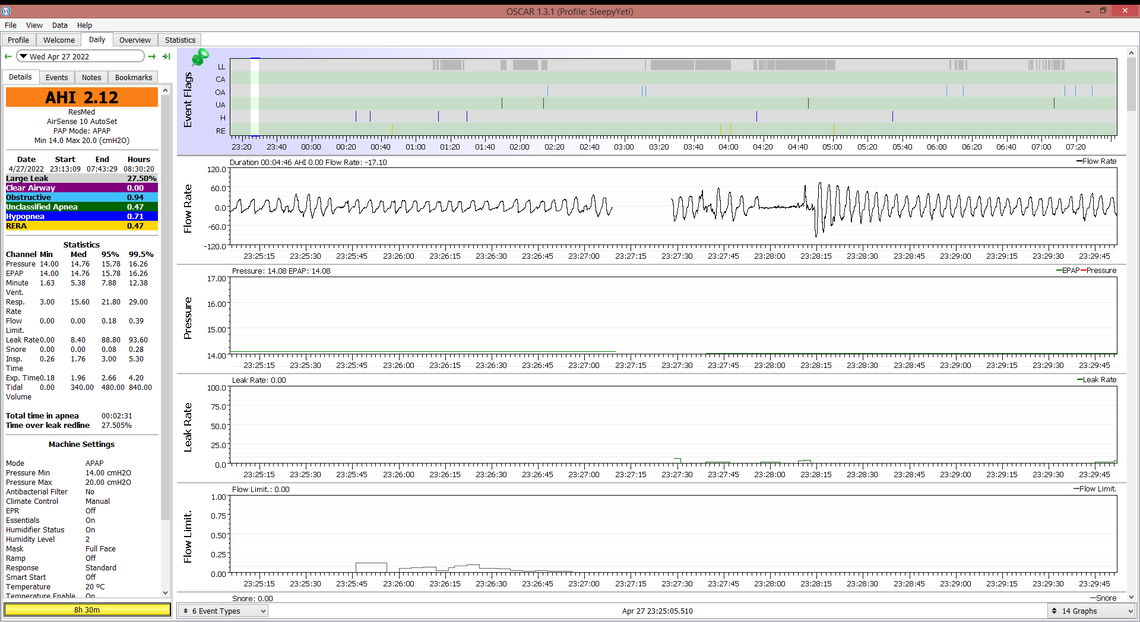
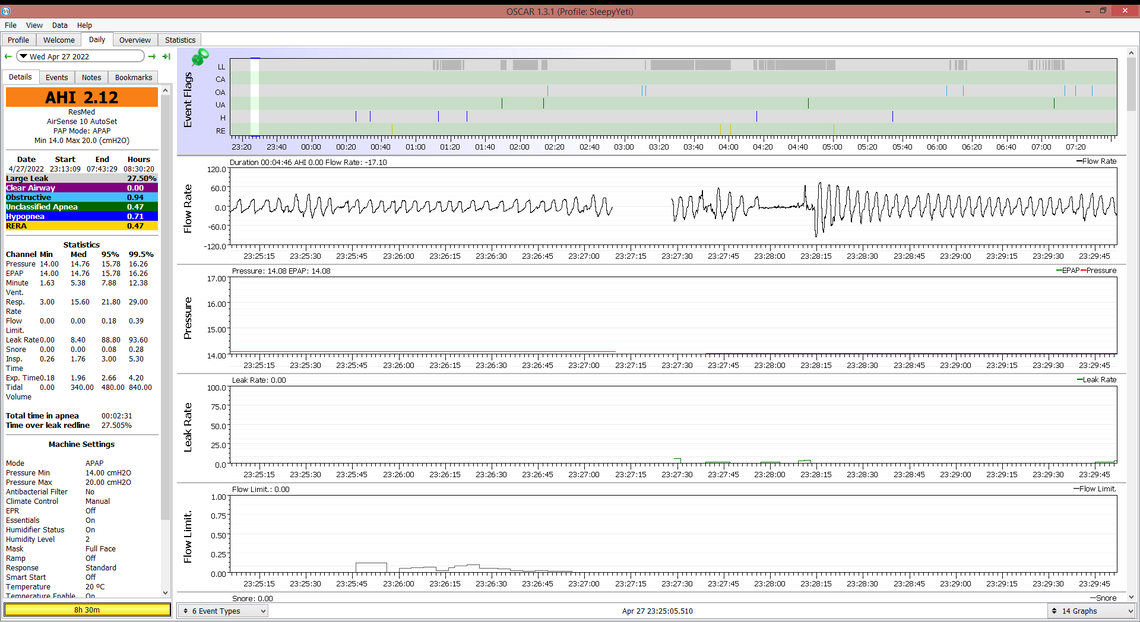
April 27, top screen shot: In the time before it appears the machine was shut off, there are no significant apnea events. However, I think I can see some flat spots on the top of the inhale peak flow. That can indicate a flow restriction, and I see there is an indication of Flow Limitation but it is not all that high. After the machine is back on again, I do see a significant no flow period and it looks long enough that it should have been flagged as an apena event. Although the left panel says the Ramp is off, I wonder if it really is. Sometimes SleepyHead did not report the status correctly. I don't know if that has been fixed in OSCAR.
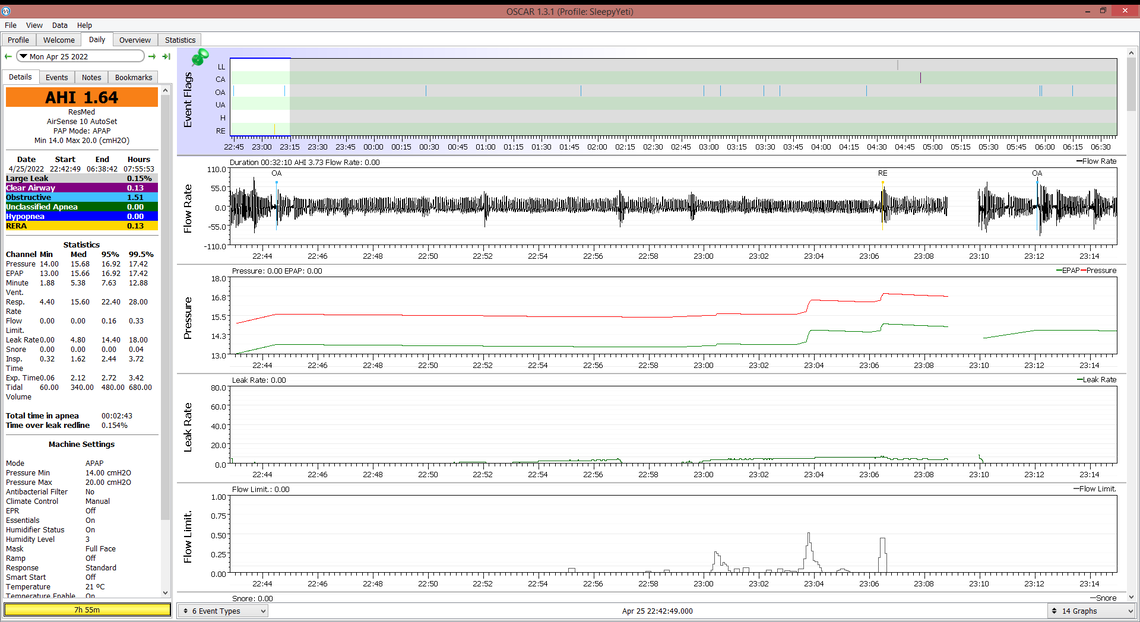
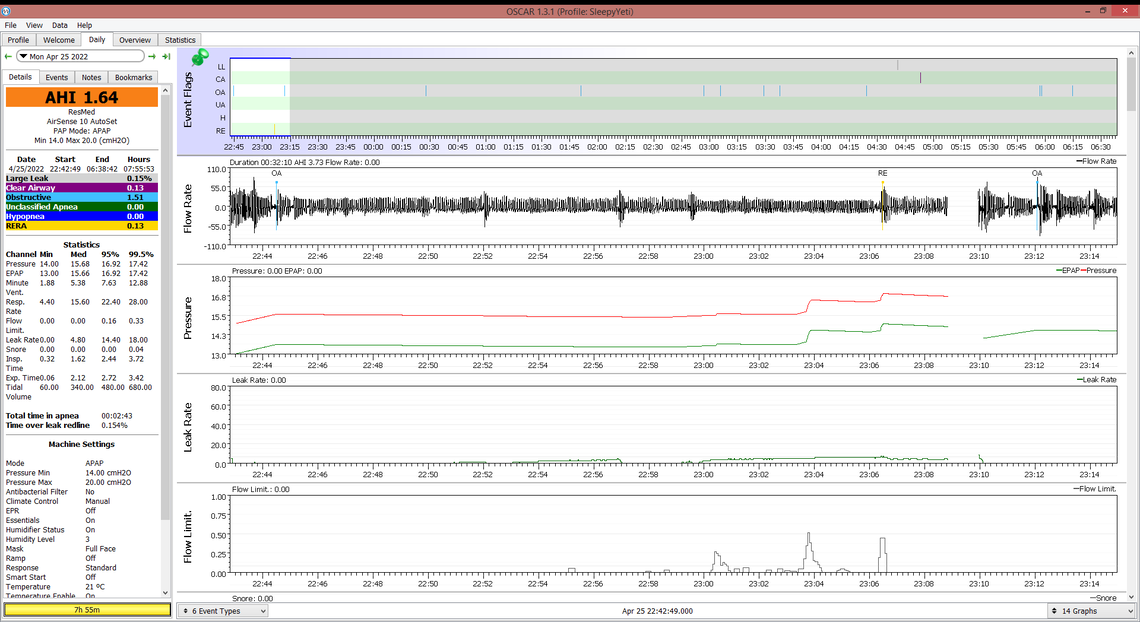
April 25: The pressure chart is showing a slight ramp, but it is not much. I see an event is flagged about 2 minutes in about 22:44:30. There is no obvious apnea event before the machine is shut off at 23:09. There is a RERA and some Flow Limitations displayed though. You would have to expand that area out some to see if there were any flow stoppages. EPR is on in this chart. It may be advantageous to turn it off. Having EPR on could help with flow limitations, but it may make the frequency of OA events worse. With EPR you need to try it both ways to see if it helps or hurts.
There is nothing jumping out at me that the machine is not working properly. It all looks reasonable what it is doing.
Thanks Sierra. Yes on the 27th I had turned off Ramp and EPR. Is Flow limitation the same thing as an apnea? 8 years ago I was diagnosed with obstructive but some things I read almost sound like what I'm experiencing is centrals. Would central apneas show up on this report? I'm going to post a screenshot from last night at the bottom of this thread.
Last night I know when I experienced the waking up 'jolt', heart racing, etc. I turned off my machine so I could take a look today if there was anything out of the ordinary but now looking I can't see when I turned off the machine so that I can see what happened just before. Am I missing something? I know it was within the first 15 - 30 min of turning the machine on.
I think I see a small gap in data at about 00:10. You would have to expand out that time period to see the detail of what was going on before you turned the machine off. Also on the left panel, below what you captured on the screen shot there should be start and stop times for each session over the night. That would give you the exact time.
oh yes, I do see that gap. Here it is expanded.
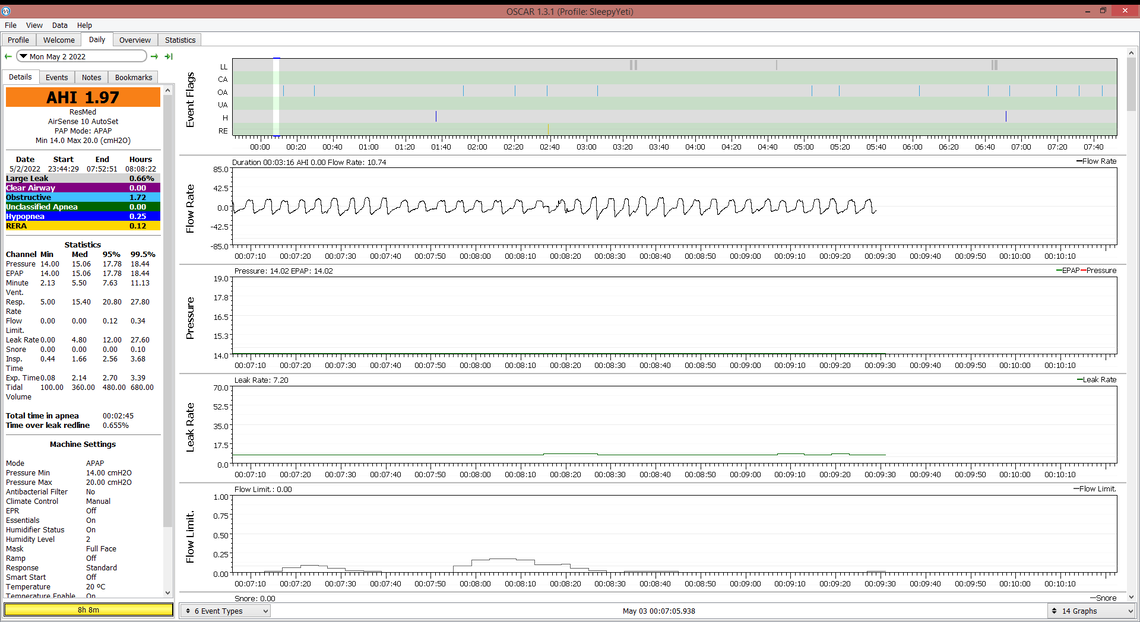
In that small window I do not see anything that looks like a OA event. But the flow rate inhale has flat tops that could be seen on some of your other charts. This suggests flow limitation issues. I would look back over this whole period (use left and right arrow keys) to see if there are any OA events. If not, it may be worth trying EPR on again, and set to 3 cm. It may help with the flow limitation. You also may want to discuss these patterns with your sleep clinic if they have someone qualified to look at it.
I had the racing heart issue on occasion for the last five years when I started using CPAP. It happened more several months back. For about three months I have been taping my mouth and that alone stopped the racing heart. My sleep is also better, not perfect, but a lot better than what I was having. I wear a full mask and for years prior, I was always a mouth breather. I started off slow with the taping. Patches are sold online. I also place the white tape over it so it does not fall off.