Hello everyone, I have been using my CPAP for about 7 months now, after being diagnosed with mild sleep apnea (9.6 AHI) from a sleep study test. Despite having improvements on paper (reported improvements in AHI and an average of 6-7 hours of sleep per night consistently) have yet to feel any better, am still plagued by fatigue, headaches, waking up exhausted, and having trouble concentrating, thinking, and processing information. I have brought up other sleep disorders like Central Apena sleep doctor, but he said not possible based on Sleep study results. Does anyone know any other potential causes? I’ve tried researching but I’m not finding anything useful. I have also used every mask type, but nothing seems to work. I have read weight loss helps, but I need this CPAP treatment to work or at least alleviate the symptoms until I lose some weight.
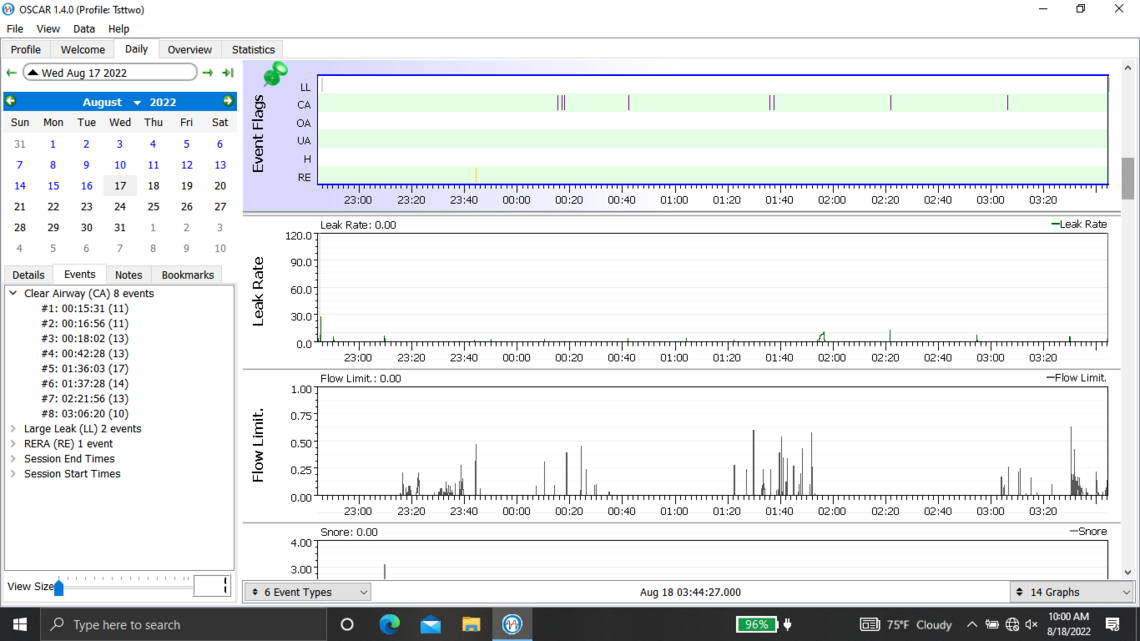
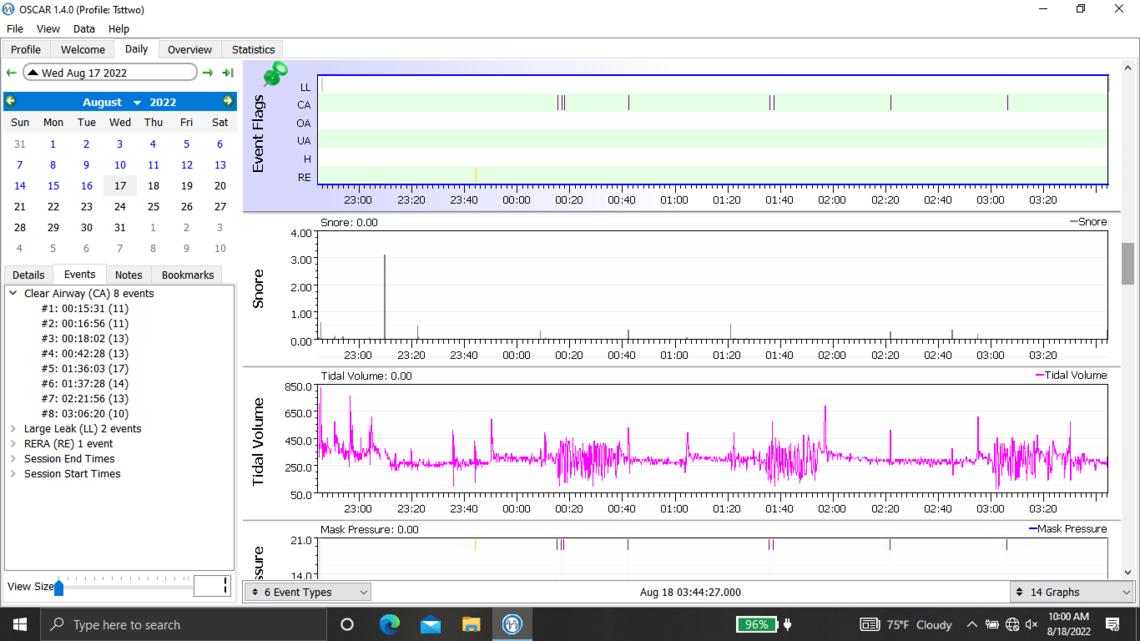
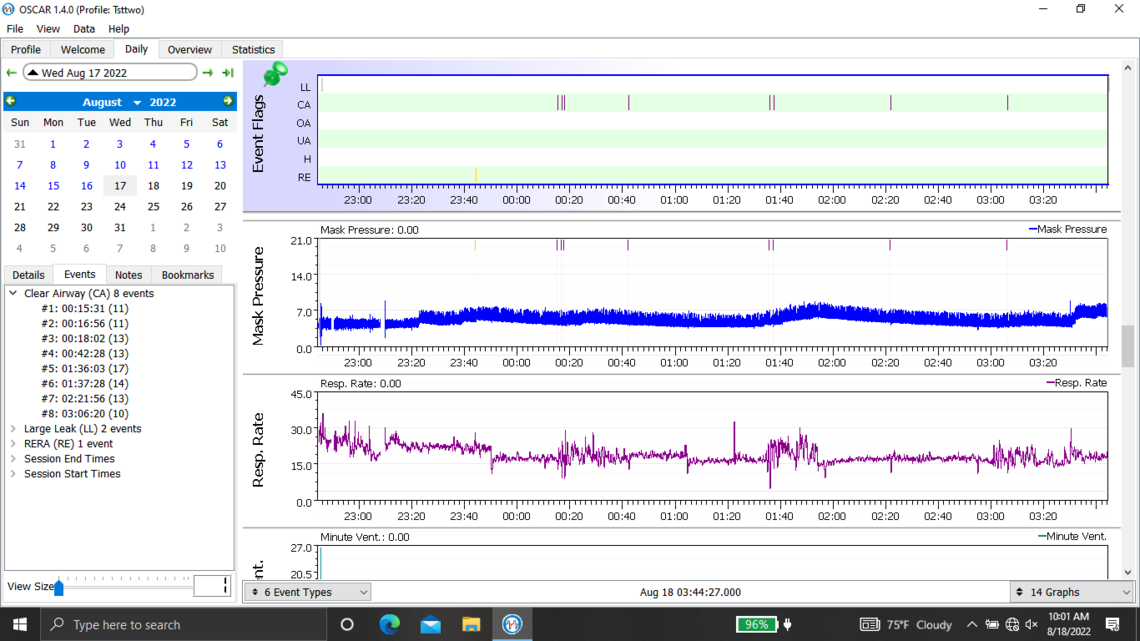
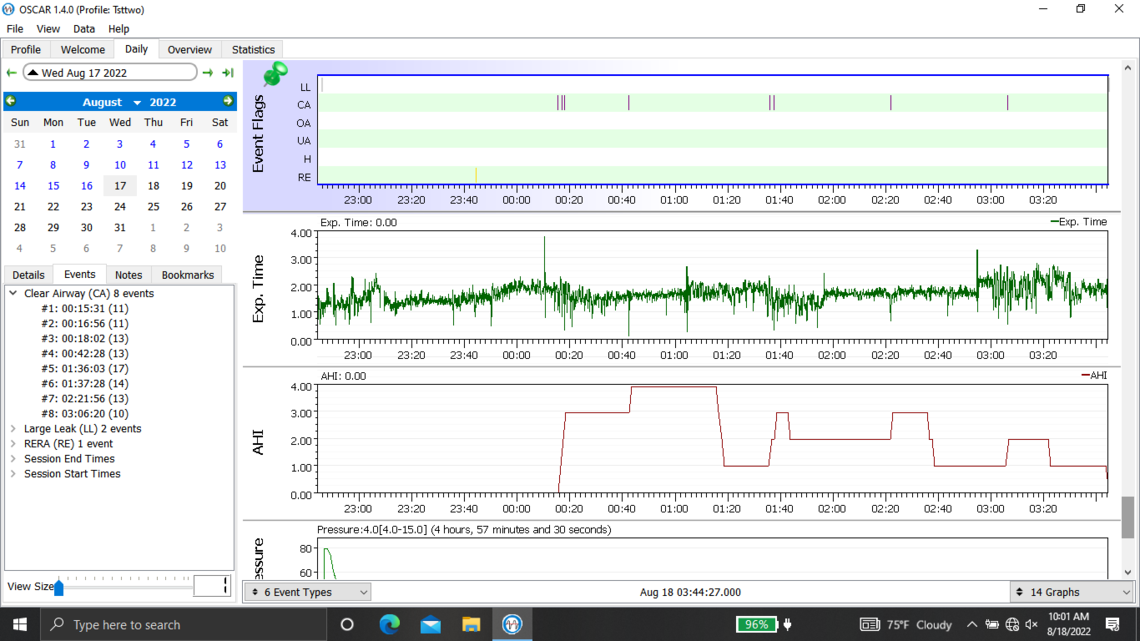
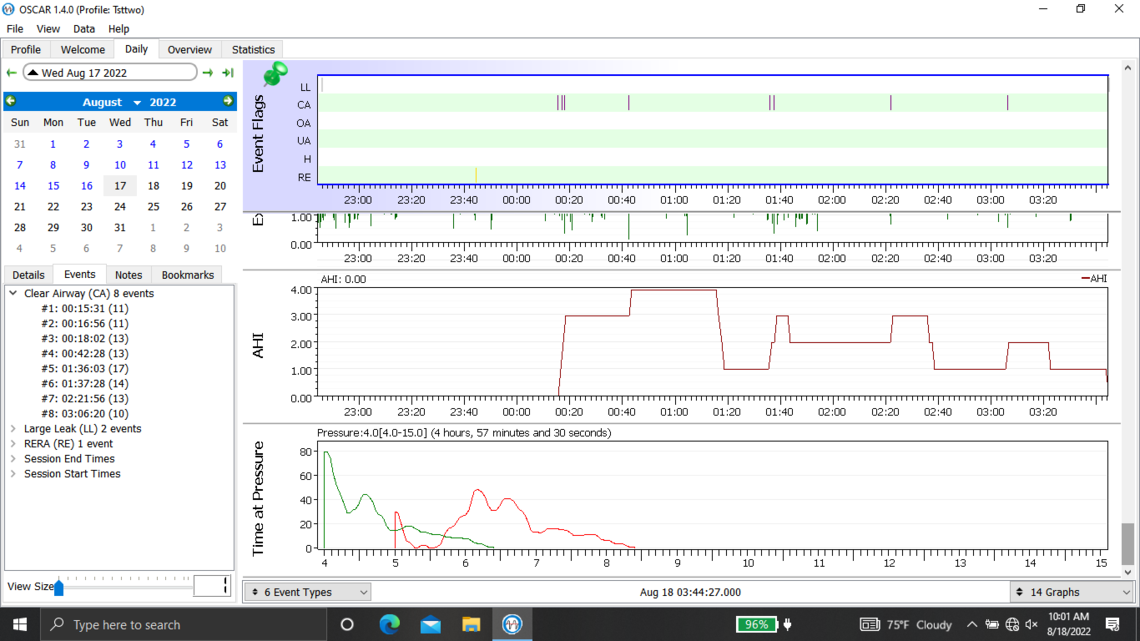
Below are my oscar results from last night. I ended up taking the mask off after 4 hours when I suddenly woke up. I also have issues going back to sleep with my sleep apnea after taking it off in the middle of the night.
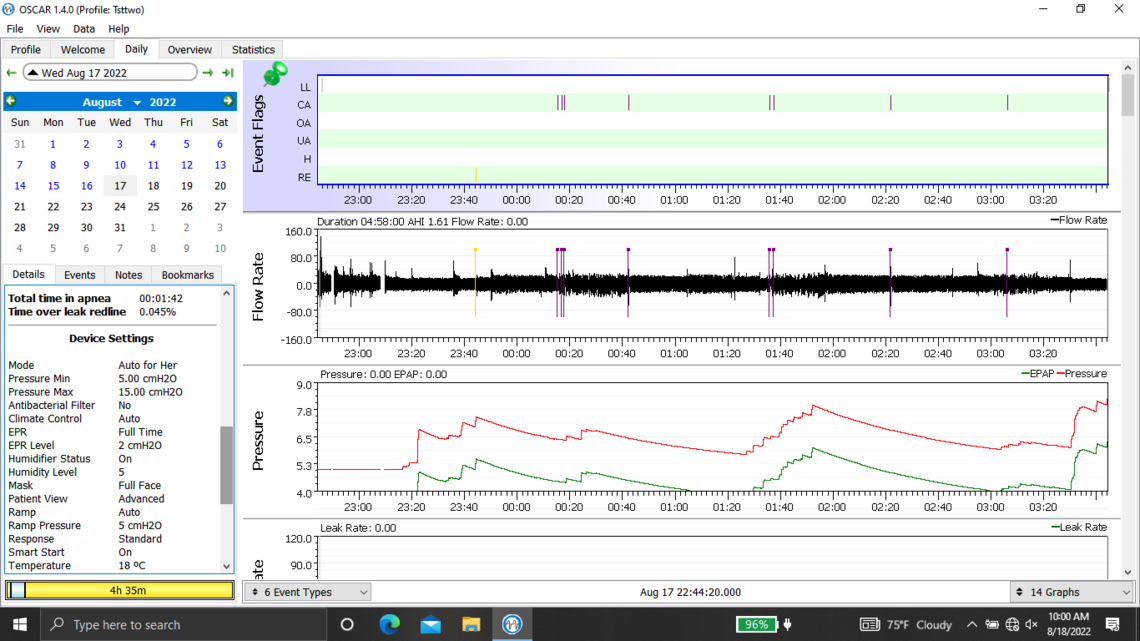
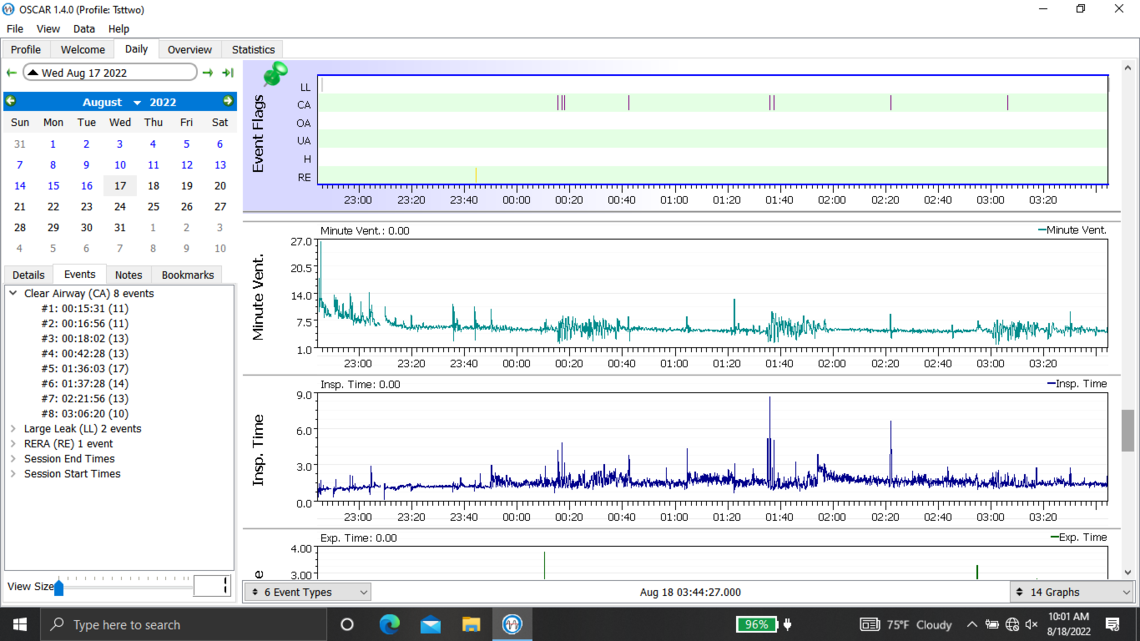
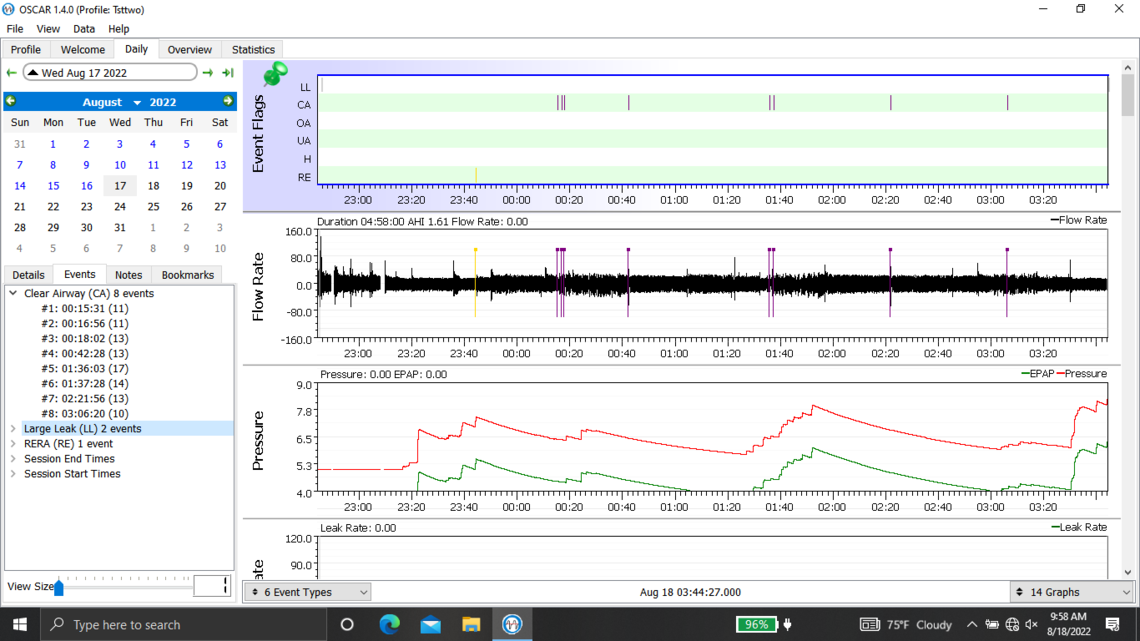
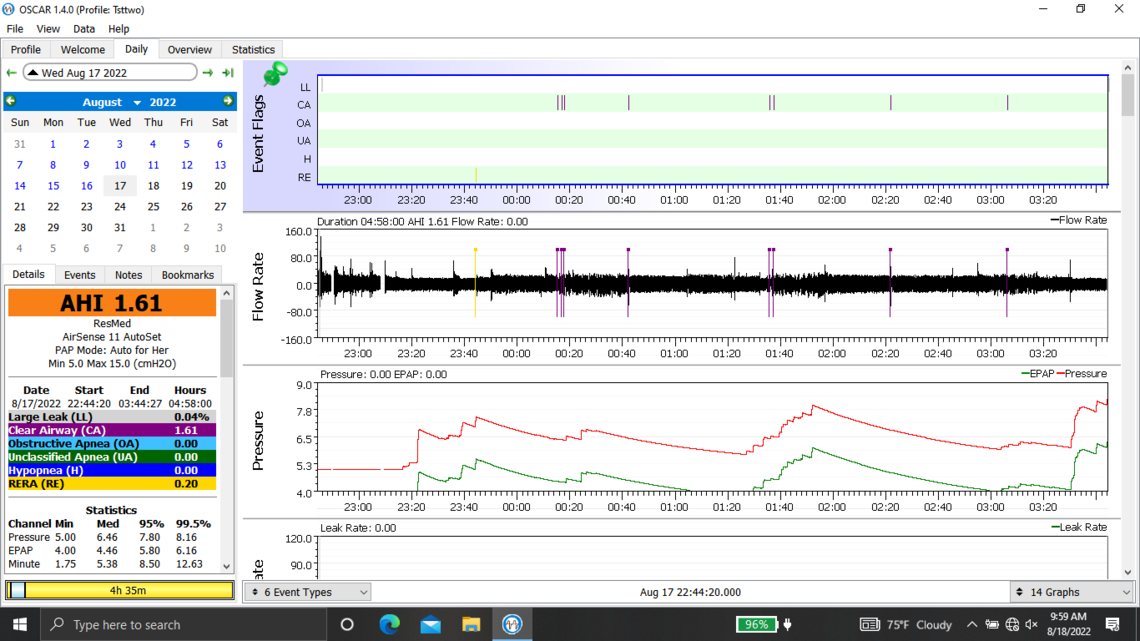
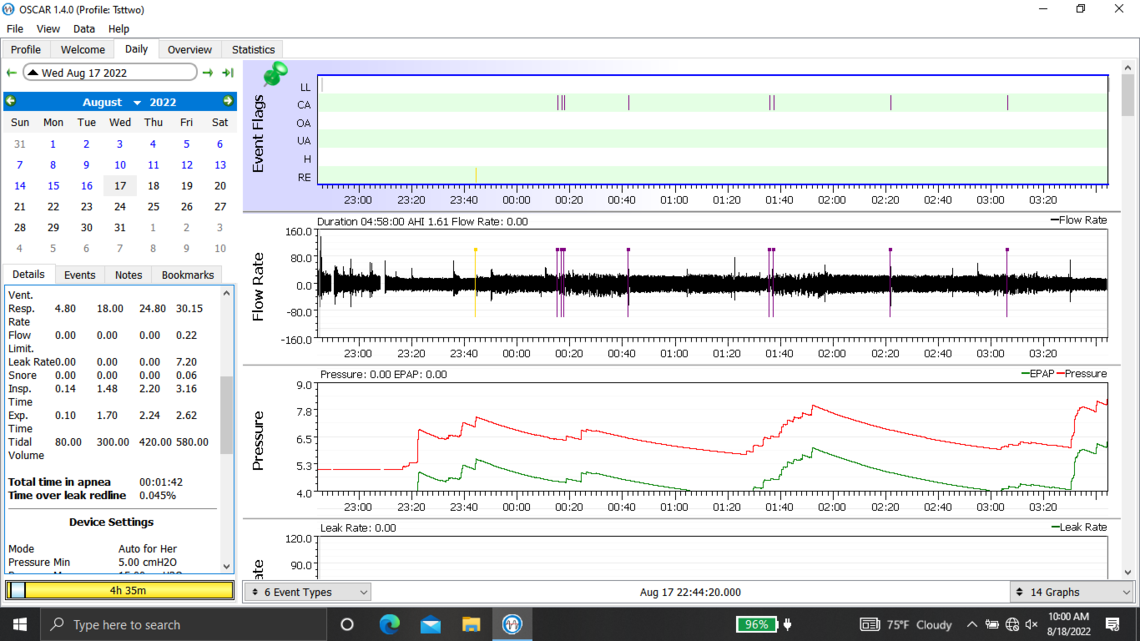
Welcome to the forum. There is no need to post all of those graphs as it tends to delay the post from showing up. The second last one you posted is the best. But you should click on that triangle beside the date to suppress the monthly calendar so more details show on the left.
Yes, you do have some issues with central apnea if this night is typical. With an APAP pressure does not work to resolve CA events and unfortunately can make them worse. My thoughts based on your graph would be to increase your minimum pressure to 6 cm, and reduce your maximum to 7 cm. This will limit the pressure that the machine will use. The Ramp start pressure should be increased to 6 cm to make it easier to breathe if you wake up in the night.
Those are my initial thoughts. The other approach would be to switch to a fixed pressure CPAP mode and set the pressure at 6 cm. If you continue to have CA events you could slowly reduce that pressure in say 0.6 cm steps to see how low you can go.
Do you know from your sleep study how much of what type of sleep apnea was recorded?
Thanks for the reply and tips. Here are my sleep study results:
SLEEP STUDY INTERPRETATION
The total time in bed was 485 minutes of which 420 minutes were spent asleep, yielding a sleep efficiency of 86%. The latencies to sleep and stage N2 were both markedly prolonged, likely contributing to the borderline REM latency of 60 minutes. There were 33 arousals, resulting in an arousal index of 4. Stage N1 sleep time was prolonged, comprising 34 minutes or 8% of total sleep time. Soft snoring was heard when the patient slept in both the lateral and supine positions. Four non-arousing myoclonic events were noted, the frequency of which did not reach clinical significance. No electrocardiographic abnormalities were observed associated with an average heart rate of 74 BPM. There were 5 obstructive apneas and 59 hypopneas, the frequency of which increased when the patient slept supine. The apnea/hypopnea index was 9 and the supine AHI was 22. The average oxygen saturation was 95% and there were REM related repetitive, sawtooth pattern desaturations to as low as 81%.
IMPRESSION: There is evidence of a mild obstructive sleep apnea syndrome, the severity of which worsens when the patient sleeps supine, associated with soft snoring, frequent arousals and REM related repetitive oxygen desaturation. CPAP was not applied due to the underlying relatively low AHI. This patient may, however, benefit from CPAP application or alternative therapy. Clinical correlation is advised.
The good news here is that there were no CA events detected during the sleep study. You therefore must have "treatment emergent" central apnea, or in other words created by the treatment pressure. In most cases these go away after 8 weeks or so of treatment. But, if they don't you probably want to focus on getting the pressure down to avoid them. The best way may be going to a fixed CPAP mode and fixed pressure.
One more question: If I am going on a fixed CPAP pressure mode, should I turn off EPR?
Whether EPR helps or hurts seems to be dependent on the individual. I have found that if I set my EPR to be Ramp Only (it shuts off at the end of the ramp) my hypopnea event frequency is higher. If I have it set to Full Time and at 2 cm, my apnea events nearly go to zero. I noticed that in your sleep test you had high hypopnea event frequency, and now in the one night you posted you don't have any with EPR on. That would suggest EPR is helping you. But, it can be worth while to try it on, and off to see what works best for you. Having it on during the Ramp can be more comfortable.
I also suffer from high CA event frequency, but my apnea is mixed which means I have both CA and OA. That can be difficult to treat as more pressure helps with OA but makes CA worse. Once you go to a fixed pressure about all you can do is try different pressures to see what works best for you. I would try changes of 0.6 cm at first to see what is best and then when you get it narrowed down, fine tune it with 0.2 cm steps.