Newbie here. Diagnosed with mild OSA. 2 months into PAP therapy (Resmed 11 on Auto 8-18 with full-time EPR=3), just trying to get used to it. SO much angst, so many questions, but let me start with some basics.
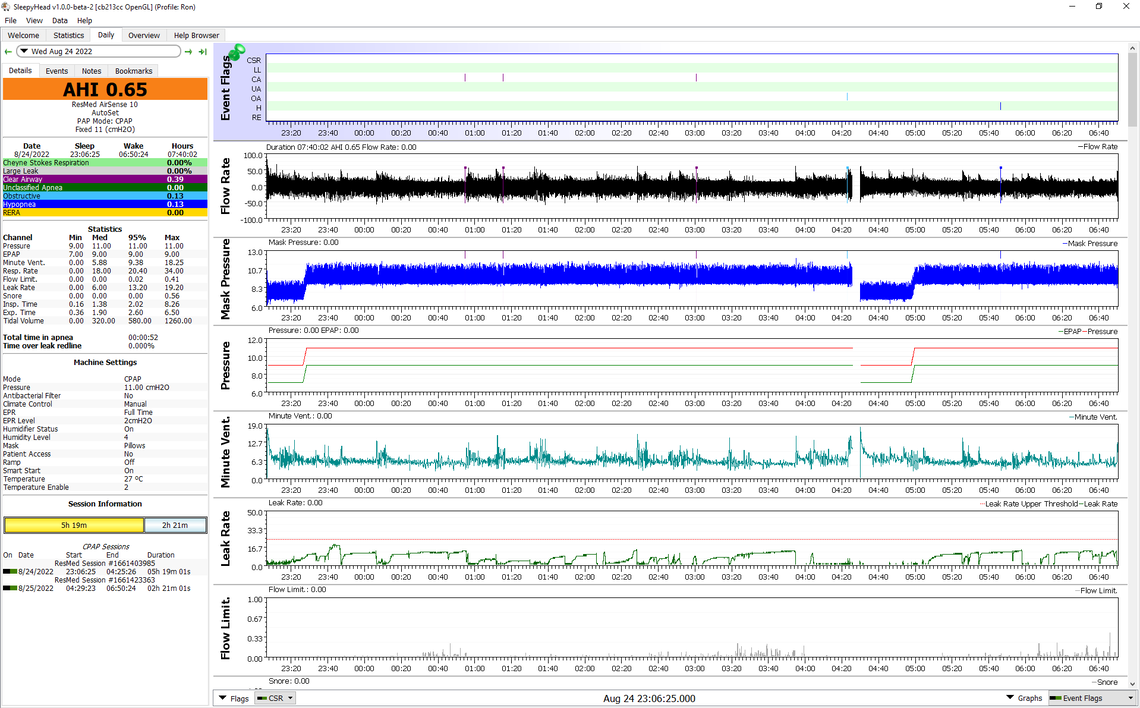
My sleep study was rough, but perhaps representative of my sleep: ~3.5hrs of sleep with OAI=0.0, CAI=2.1, HI=10.2, for AHI of 12.3. Although the Dr did not look at anything but the study summary results, he said absolutely I have Obstructive sleep apnea. Up to now, I feel that I have been in an adjustment phase, but I may be turning the corner in getting used to the PAP. I am retrieving and reviewing OSCAR data. So far, each night is pretty different.
My first question is, where is the best place to get more detailed review of OSCAR data?
Forums like this seem to be the only option I have found, and I am generally impressed with what I read. But, it seems as part of my medical treatment, someone should be interested in reviewing the data that is available. I do not see my Dr. doing it. I talked briefly with sleep techs, but they do not seem to be in a position to help. I though maybe the PAP (DME) supplier might help, but that is not the case.
My experience (and what I have read in forums) seems to indicate that the doctors are just like, you have X try a PAP and we will go from there. Is that how it really works? I now feeling like there is no general practice of reviewing the available data.
My second question is a bit more related to my specific condition, but I want to run a baseline with the PAP at minimal pressure to have something to compare to. Does sound reasonable?
My initial OSCAR data review has yet to show clear patterns. CA, OA, UA, and H events often appear very similar. I'm assume the pressure ramp/release has lots of coding control behind it, but does not seem to make much difference in events. Still getting used to this mess. Seems I get into too much leaking with the high pressures. I'll show 2 nights below, but not really expecting much analysis as feel I'm still in the adjustment phase.
Calm? night
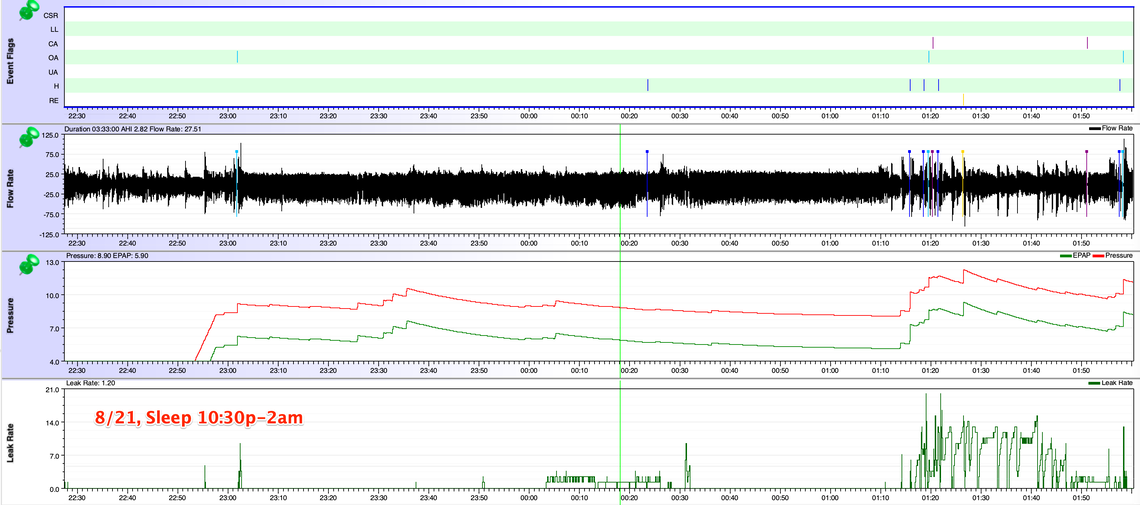
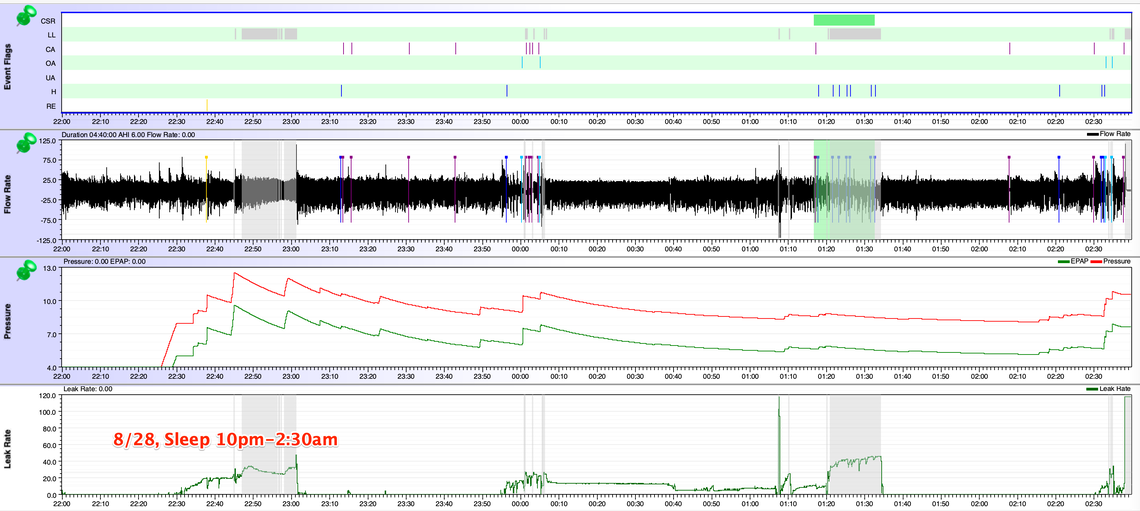
You may wonder why I only show 3-4 hours of sleep. This is my pattern. After this initial sleep phase. I do try to get back to sleep, and most often I can after 15minutes to 2hours. But this second sleep will be lots of tossing and turning. Upon the first wakening with the PAP, I'm often congested and fed up with the mask and do not even try wearing it. I'm hoping the 3-4 hours extends once I find the root cause and fix. I'm not convinced at this point that the fix will be the PAP device.
I am actually hoping the PAP will help, because I need help. My Dr said mild sleep apnea will not kill me. I told him my trending poor sleep and its consequences is absolutely UNSUSTAINABLE.
Welcome to the forum. Some thoughts:
A proper sleep clinic should have ResMed software called something like ResScan. It is similar to OSCAR which frankly is an unauthorized knock off product developed as OpenSource freeware. If you take your SD card into your clinic they really should be able to look at the data and give you their analysis. Unfortunately most just want to sell you a machine and not have you come back unless you want accessories or a new machine. If you post your Oscar charts here I and others can give you their opinions. This is the format I like to see it in, so I can be most helpful. On a PC when you have the screen set up just push F12 and observe where the file gets saved. You can then drag it into a post here. Use a new full with window so it is easer to read.
Running a baseline with a CPAP is really not possible as these machines will not reduce pressure below 4 cm of pressure. A sleep study is done with zero pressure. Your machine will always be providing some kind of treatment. The other issue is that only 4 cm of pressure can be suffocating to sleep with. I see you seem to be starting your sleep each night with only 4 cm of pressure. That is unlikely to be very comfortable. My suggestion based on your two OSCAR charts is to increase your minimum set pressure to 7 cm, and set your ramp time to auto, and to set the ramp start pressure to 7 cm. That should give you a better start to your sleep each night. To do these things you have to go into the clinical menu. See this link for a Clinical Manual.
You do seem to be having some issues with CA events and CSR. This sometimes can be something called "treatment emergent central apnea". The pressure of treatment can be causing the CA events. Pressure can stop OA events, but can make incidence of CA events worse. The good news is that in most this effect goes away after about 6-8 weeks. For me it did not. I had to go through all kinds of changes to try and bring it under control. I used to get CSR quite reliably about once a month, but it has gotten better.
Hope that helps some. Post your Daily screenshots for more comments. Only post one at a time or your post may get hung up in the spam filter here.
Sierra - Thanks so much for responding. I have been traveling and will be back home after the holidays. This all seems like a big mess. I beleive job one, is to get used to the PAP so I can get more consistent data. I may even continue with that on the prescribed setup until my sleep doctor revisit. At that point, I may decide to go on more self-directed (with help from forums).
Thanks again, more to come after I get home. Eric
I am told that you need to hold two fingers on the screen of an A11 for about 4 seconds to get to the clinical menu on it. A change from the A10. If you are going back to visit your sleep doctor be sure to take your SD card in and ask them to look at the data. For discussion it would also be good to print out some of your OSCAR charts where you are having frequent CA events and sections where CSR is flagged. It is good to zoom right in where there are lots of CA events and CSR to show the detail of your flow rate. Include a graph of your Minute Ventilation. That can be telling too. And you can post it here for comments too.
Congestion: One big current problem with PAP is that it seems to make me congested. When I tried a nasal-only mask, after a couple of hours, I could not even breathe through my nose, so it was kind of game over. With the full-face masks, it seems I have better luck, but it is still an issue. In fact, most times when I wake after my ~3hrs of PAP sleep, the auto has cranked the pressure way up, and I have had a series of various events and often large leaks. This makes me feel like the PAP is making things worse, not better.
I certainly have read about other PAP people having issues with congestion, unsure if I have seen much about the PAP being the cause. I few nights I tried using Breathe Right strips, which seemed to help, but then I felt like I was adding too many variables into my treatment and decided to just continue with drudgery as is.