Hello everyone.
I am new to this forum so I will introduce myself. :-)
WHO I AM
My real name is Daniel and I tell everyone to call me Dan. I am a 71 year old retired engineer bilingual French-English. I live in Canada, province of Quebec, city Shawinigan. Unfortunately, I am a smoker.
MY SLEEP STUDY
I was diagnosed with apnea and part of the results of my sleep study were:
Central apneas : 1.3
Obstructive apneas : 23.3
Mixed apneas : 1.7
Hypopnea : 7.7
Apneas + Hypopnea : 33
RERAs : 2.3
That study was done in February 2021.
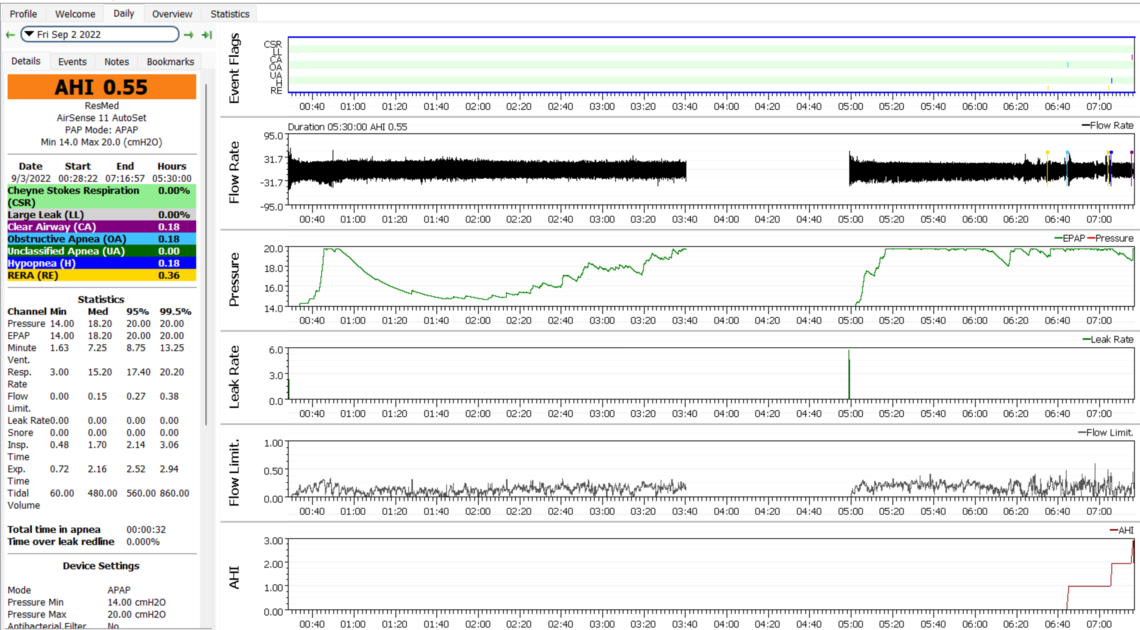
MY CPAP
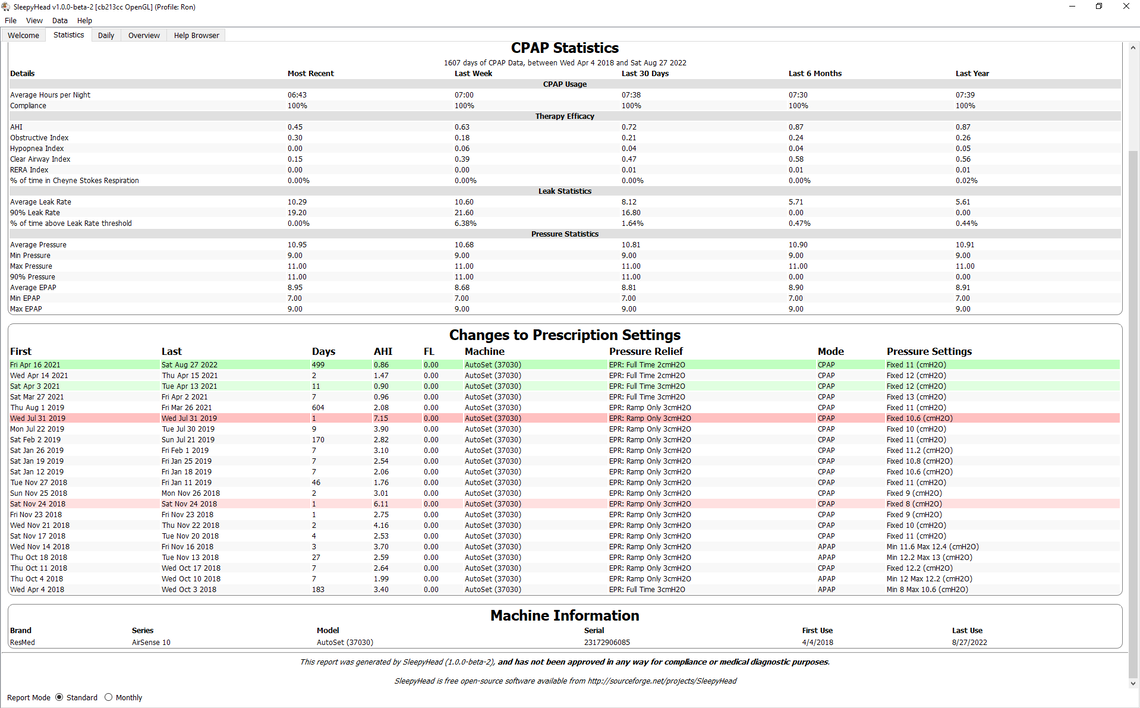
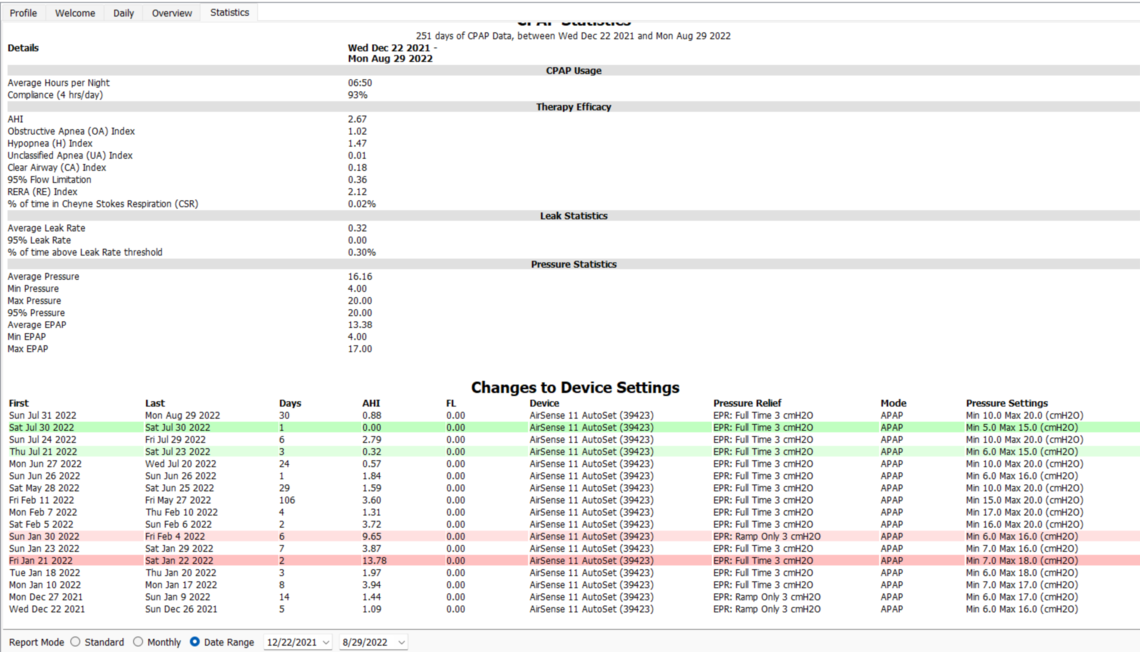
I got Philips machine first but problems with the sleep clinic (not the Philips recall) forced me to change the machine. I then got à Resmed Airsense 11 and started using it December 22, 2021.
MY THERAPY
Untill June 2022:
I struggle to get my numbers down. I got different advice for the pressure settings and played with those with no real improvement. The final pressure settings are now 10/20 which is the maximum for the high pressure. It was also suggested I wear a cervical collar because of probable "positional apnea". I tried two collars with the second one showing some improvement. I call it a semi-rigid collar. My results were still up and down and not really good.
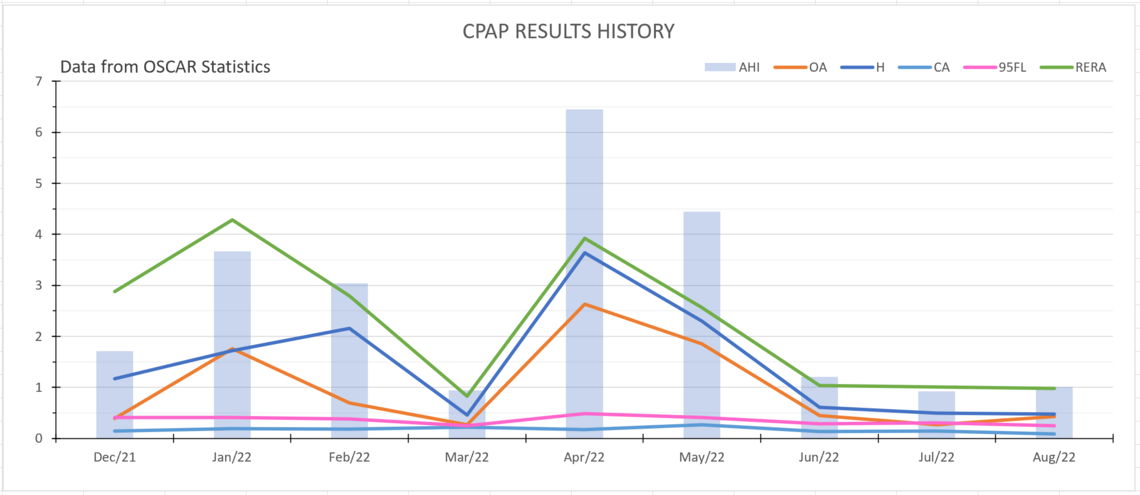
After June 6, 2022:
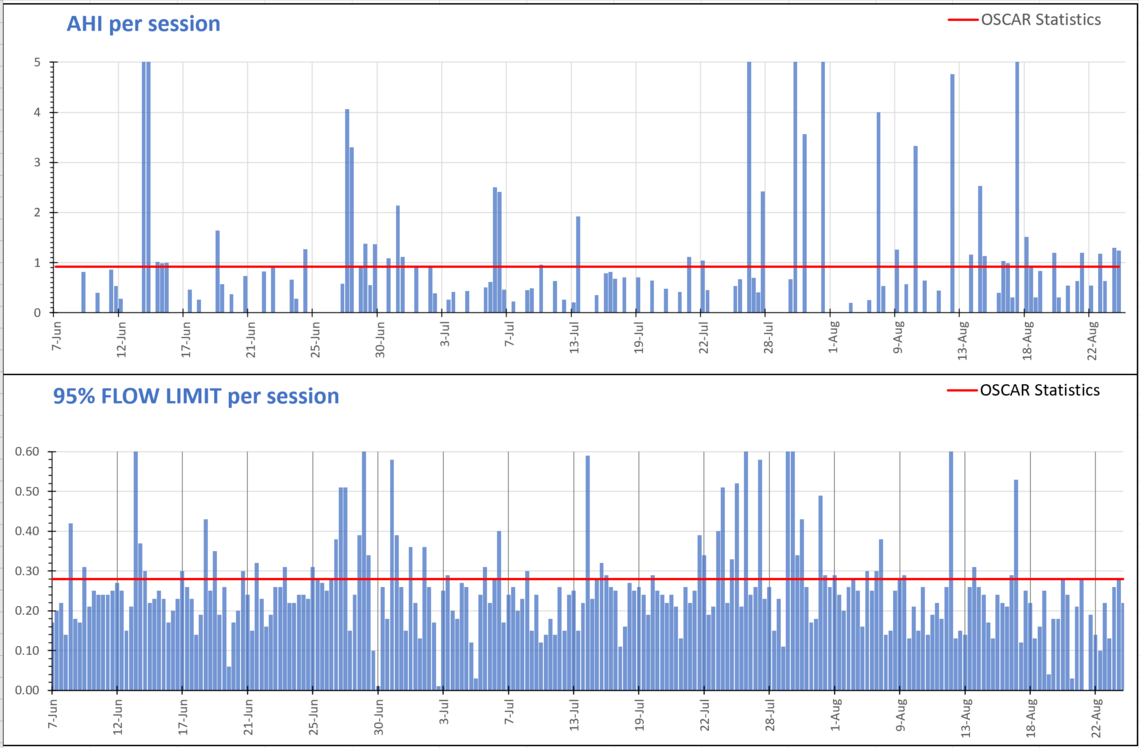
As I was searching internet for information about apnea and treatments, I stumble on an article about a MAD (mandibular advancement device) that would be a help for some people. So I got one device from Amazon to try. It is not something I should keep wearing for long because it can have a bad impact on the mouth and teeth (so says my dentist). From the first night I tried the MAD, I saw my numbers drastically improve as shown in the table below.
If those results stay as good as they are now, I will get a MAD made by a professional.
MY QUESTIONS
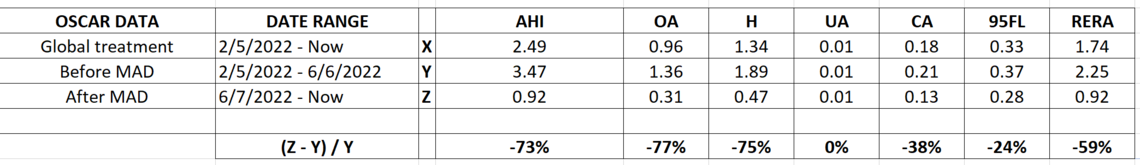
My big question is when you look at my numbers (images below), is it possible to improve on that or should I be happy with what they are?
I started yesterday to stop drinking coffee with the hope I will cut down the fragmented sleep which is my usual night. For now I do not seem to experience caffeine withdrawal problems.
Finally, can you think of anything else I could do for improvements?
I have more information available should you want it. Thank you for any comment you would submit.
Your post was probably delayed due to the graphics. I just saw it today.
On your sleep test are those numbers events per hour? If so an AHI of 33 is moderate apnea and should be treated. I am a bit surprised that the pressure you are using is as high as it is (95% at about 18 cm). My AHI at diagnosis was 37 and I use 11 cm of pressure.
I find your results from the MAD device very interesting and are worth exploring. They are expensive but it would be worthwhile getting one made by a dentist.
You are using EPR at 3 cm and full time. People respond differently to EPR. I went a long time with EPR at 3 cm but on ramp only. When I switched to full time at 2 cm my hypopnea events went down significantly and my AHI improved from about 2 to less than 1. It is hard to predict the value of EPR and the best way is to try with it on and without it to see what works best for you. For some having EPR off can reduce the frequency of obstructive events and as a result reduce required pressure. Trial and error seems to be the only way to figure out what works best for each individual.
I have had issues with central apnea which you do not seem to have. The other big improvement I got and especially with respect to CA events was to switch from auto mode to fixed pressure CPAP. In auto it seems that the machine can sometimes start to chase its tail and raise pressure too much. I also think it can raise pressure too much based on hypopnea events which may be central (open airway flow reduction) in nature rather than obstructive. The machine is smart enough to not raise pressure in response to central events, but it seems to not be able to distinguish between central hypopnea and obstructive hypopnea. In any case I was running pressures in auto up to 15 cm, and now I am using a fixed 11 cm of pressure with full time EPR at 2 cm. It may be worth a try to see if it works for you. It is a trial and error process and based on your one night you may want to try 15 cm to start. And at least in the beginning make 1 cm changes in each direction to zero in on the optimum fixed pressure for you. Once you get close then you can fine tune with smaller steps. See my history below to get some idea how I did. Not very scientific, just patient trial and error!
On coffee I drink lots of it, but never after 12:00 noon, or any other caffeinated drinks in the PM or evening. There is some good sleep info at this link. It was set up by a professor of pharmacy in Nova Scotia I believe. His objective was to try and get seniors off sleeping pills.
Thank you Sierra, your comments are greatly appreciated :-)
On your sleep test are those numbers events per hour?
Yes, they are.
the pressure you are using is as high as it is (95% at about 18 cm)
At the beginning the pressure settings were Min. 6.0 Max 16.0 (cmH2O). The results were not very satisfactory so I tested different settings. I got the best results at the settings Min. 10.0 Max. 20.0 (cmH2O). One thing I just realized is that all the tests I made was before I started using the MAD. I will retest with different pressures and see if there are positive effects.
You are using EPR at 3 cm and full time.
I do not have a clear understanding of what the EPR is or do. Based on your results, I will try different settings and check for improvements. I think I should do those tests after the ones with the pressure.
I read somewhere that the caffeine effects could last for 1 to 2 weeks. Since I have no problem cutting it, I am waiting for a couple of weeks before concluding on its effect on me. I used to drink coffee throughout the day and even at night when I woke up.
What is hard for me is getting the patience required. I am not naturally very patient.
P.S. Is there a place instructing how to post. I got this one by chance I think.
EPR or Expiratory Relief Pressure is mainly a comfort feature. It is a reduction when you expire to make it easier to breathe against the CPAP pressure. The knock on it is that if you are having an obstructive event during or at the start of the exhale it can make OA events more frequent. The machine in turn then increases pressure to prevent them. So for some using EPR can result in higher pressures. For a long time I set my machine to use EPR during the ramp period only. Then more recently I turned it back to full time when I was in fixed CPAP pressure mode. My OA events did not go up, and my hypopnea events went down. I suspect it is something that varies from person to person as to having it or not working well. Only trial and error resolves it.
While EPR is a comfort feature on a CPAP, it works in a similar way to pressure support in a BiPAP machine. However they can go much higher than 3 cm that the CPAP provides. For those with flow resistance EPR can be a benefit, and if they need more, they may also benefit from using a BiPAP. Keep that in mind if you do not achieve what you want with a CPAP. I would exhaust all possible options with a CPAP first. Early on in my journey, I thought I needed a BiPAP or even an ASV machine. I am now under 1 with a CPAP in basic fixed pressure mode.
The site uses a spam filter. If you are a new participant and post graphics and especially more than one, your post can get hung up in the spam filter.
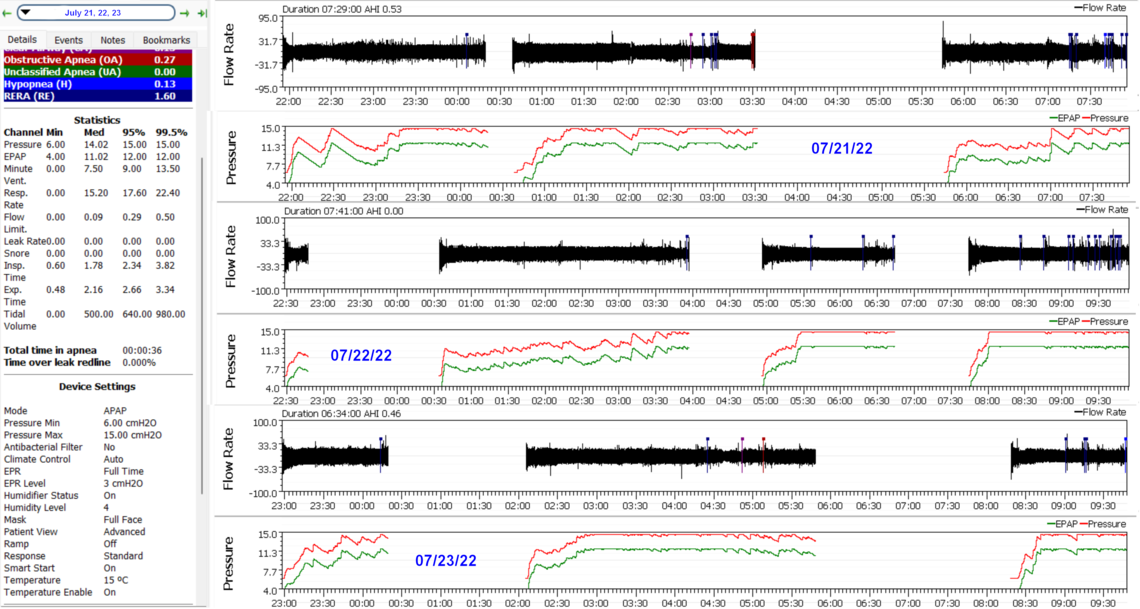
I started my tests with pressure. After one night with 4 sessions, the results are not conclusive. I will continue those tests for a few more nights.
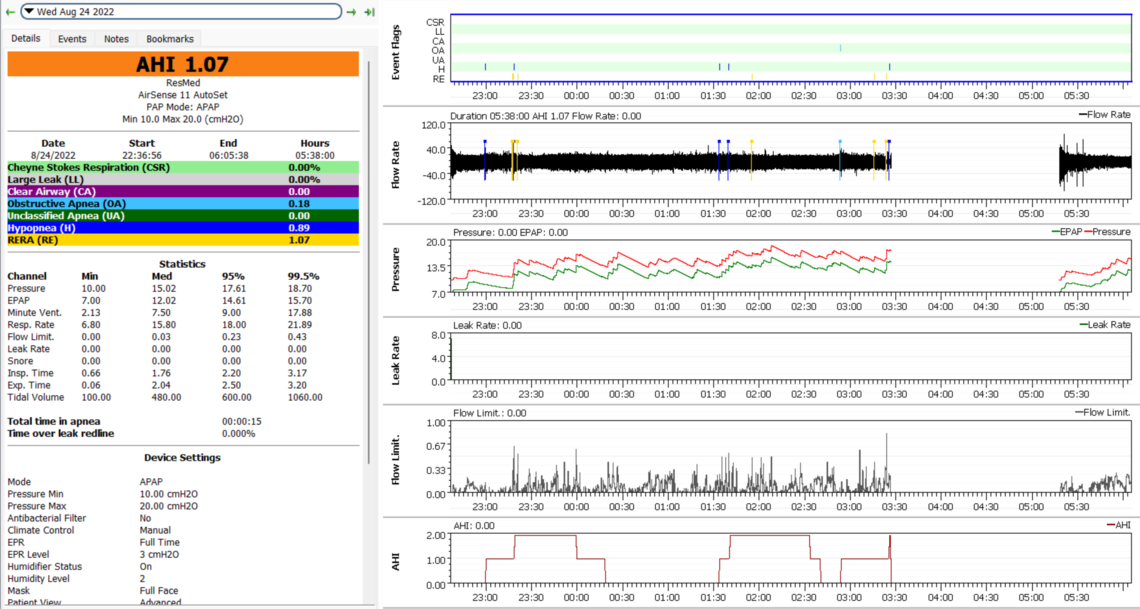
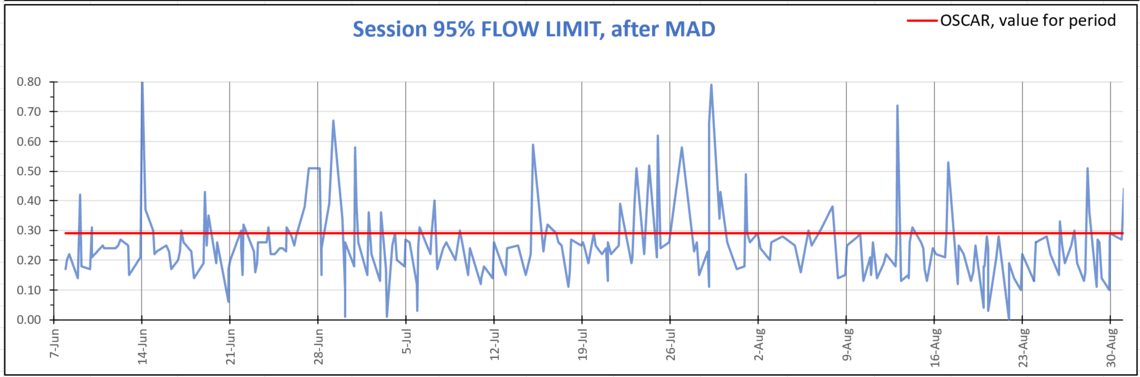
I read somewhere that the 95% Flow Limitation should ideally be below 0.1. My average for the last 3 months is more 0.3. Is it something I should try to bring down and if so, how can I do that? Is this a case that would benefit from a BiPAP?
Did you export the data to produce that graph? I don't seem to have anything quite like it in SleepyHead. Or, is it a feature of OSCAR?
I have looked at several days of my wife's graph for Flow Limitation and for my own. She has more of an issue with it than I do. From what I see, it sits mainly in the less than 0.3 range and peaks at about 0.5 occasionally. I set SleepHead to show the 95% dotted line, but I can't see any. Perhaps a bug in SleepyHead...
My machine is in fixed pressure CPAP mode by my wife's is still in Auto, but with a quite narrow range; Min 13.6, Max 14.4, and EPR at 2 cm. I should probably try hers at 3 cm to see if that helps or hurts. She just got a new A10 For Her and I thought I should let things settle a bit before trying any changes. Her average AHI is 0.45, so not pressing to make any changes. She used a S9 before that with the same settings, and a slightly higher average AHI of 0.52. This all said her pressures seem to get driven by flow limitations and less by OA or hypopnea events. I have never really tried to track our flow limitation values in any detail. My issues are high CA events, and hers is more OA events and trying to keep them down without going too high in pressure.
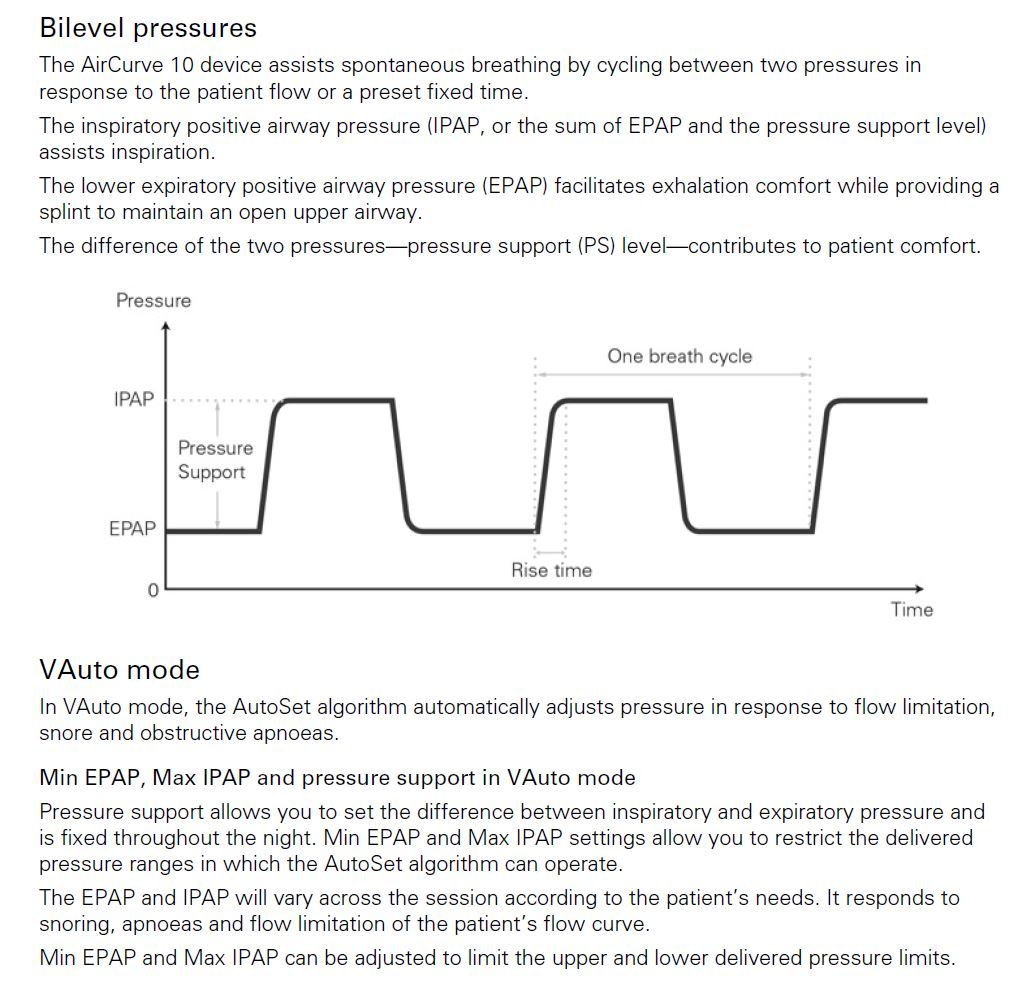
So, I am not sure if a BiPAP would help to reduce flow limitation values. It may. I believe they can go up to about 10 cm of "pressure support" which is essentially the same as EPR on our machines, but EPR of course is limited to 3 cm of pressure assist on inhale. For whatever reason BiPAPs refer to it as a pressure increase on inhale, while CPAPs call it a pressure reduction on exhale. Really the same thing, at least on ResMed machines.
I think the first thing I would try on your machine is tightening up the pressure range by increasing the minimum pressure. This may reduce flow limitations before they happen rather than waiting for them to occur and have the machine respond to them with more pressure. I would suggest 14 cm as a minimum, which is closer to where my wife's machine is. You could also probably reduce the maximum some, after you see what the increase in minimum does. Once you narrow down what pressure you really need, a trial at a fixed pressure (CPAP) may be worth a try. 15 cm fixed may work well for you or something around that.
The other possibility is a switch to the For Her mode. I believe the A11 machine includes that as an option. The For Her mode is supposed to increase pressure earlier to flow limitation and RERA. I have not tried it on my wife's machine as I recall that the For Her mode only uses up to 12 cm of pressure and that would not be enough for her (or you by the look of it). But you may want to look into it to see if 12 cm is really the max it uses.
Edit: Not sure from your graph that you are using the Auto Ramp feature or not. 14 cm is a bit high to go to sleep with, so if you adjust the minimum up to that, you should set the Ramp Time to Auto, and also set a Start Ramp Pressure to about 9 cm. That will be more comfortable in going to sleep. When the machine decides you are asleep it will ramp the pressure up to the minimum pressure.
Did you export the data to produce that graph?
I export the data to CSV files and then use them with Excel to get different graphs.
The other possibility is a switch to the For Her mode. I believe the A11 machine includes that as an option.
I don't see that option on my A11.
BiPAP I believe they can go up to about 10 cm
The AirCurve Vauto specifications say 25 [cm H2O (hPa)]
I think the first thing I would try on your machine is tightening up the pressure range by increasing the minimum pressure. I would suggest 14 cm as a minimum
My test last night was with pressure settings at 15 cm and 20 cm for the first 45 minutes and then I reset the pressure to 12-20 cm because there were leaks at the mask when I exhaled. I will give it a shot at 14 cm.
a trial at a fixed pressure (CPAP) may be worth a try
I will have to check on my A11 to see how to set such fixed pressure. As for the ramp, I don't really need it. I fall to sleep very rapidly, within a few minutes. I was thinking to check if I could just eliminate the ramp and see what it would do.
Since there are many things to set to finally have a clear picture if that is possible, I am going step by step with those tests. A few more nights to try and finalise the pressure settings.
To set the mode you have to go into the Clinical Menu by pressing and holding the round set button and the rectangular Home button at the same time for 5 seconds. With the A11 you should have a choice of the CPAP mode, AutoSet mode, and the For Her mode. You may have to use this menu to setup the ramp as well. Here is a link to a Clinical Manual that gives all these details for an A10 machine, Your A11 should be closest to the For Her A10. See pages 15 to 18.
Also when in the Clinical Menu scroll down to Options, Essentials, and set it to Plus mode (if it not there now). That will give you access to more settings from the User Menu, and a more detailed Sleep Report on the machine.
There is no real benefit to eliminating the ramp when it is in auto. I agree that the timed ramp is an annoyance, but when the time is set to Auto it is not a problem at all. It automatically switches out of ramp when you go to sleep, which will happen quite quickly by the sound of it. I find it works really well for me.
Yes, there are lots of options to change to optimize your results, but it takes time to try them all to see what works and what does not. The other advantage of using the Ramp set to Auto is that it does not respond to or count events detected. In the first few minutes of going to sleep most have what is called by some as "Sleep-Wake-Junk". These are false indications of OA and CA events. they can mess up your data with no real value added.
Yes, with the VAuto the maximum pressure can be set as high as 25 cm. However, the pressure support (difference between IPAP and EPAP) has a maximum of 10 cm compared to the 3 cm on the AutoSet devices. So, it can give a much larger differential between inhale and exhale to assist in breathing.
To set the mode you have to go into the Clinical Menu by pressing and holding the round set button and the rectangular Home button at the same time for 5 seconds.
On my A11, you just need to touch 2 fingers anywhere on the screen for 3 - 5 sec. and the Clinical Menu appears.
Also when in the Clinical Menu scroll down to Options, Essentials, and set it to Plus mode
No such Plus mode on my A11. But there are more settings available within the Clinical Menu.
There is no real benefit to eliminating the ramp when it is in auto.
I did not notice until now that I have the ramp off. I will keep it like that for the tests I am doing so I have comparable data.
Interesting that they have actually made some more changes in the A11 compared to the A10 than I was aware of. I had thought that the only significant change was the availability of the For Her mode in all machines.
I am in Alberta and wanted to buy an A11 for my wife, but it seems that the supply of CPAPs at the on line outlets is so reduced you have to put your name on a waiting list to even get an A10. I managed to find an AutoSet For Her A10 with only 96 hours on it, so we bought it instead.
I stumbled on this article in the blog section here that you might be interested in.
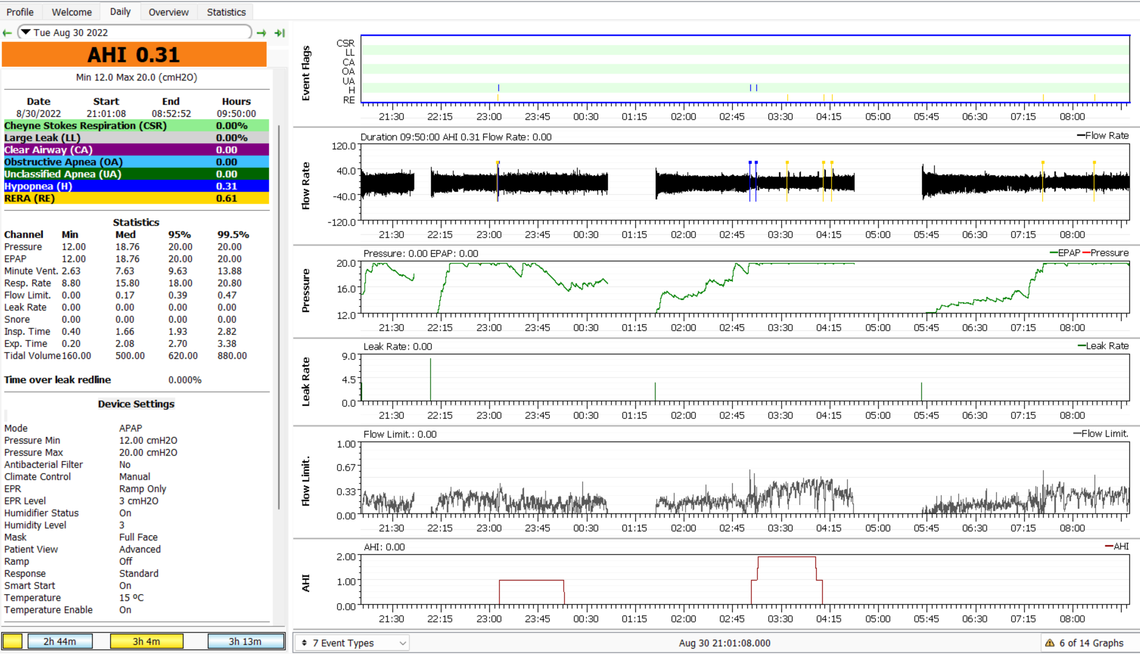
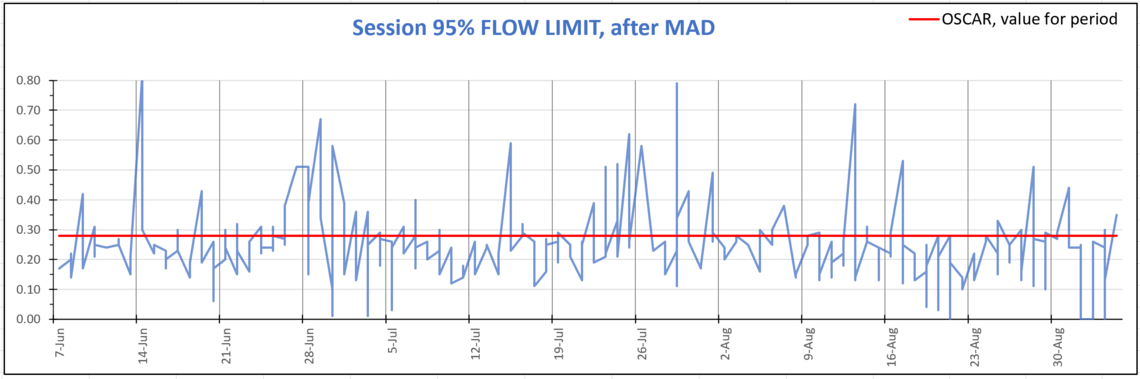
Does someone has ever seen something like my last night sleep?
That is for the same night. No change in anything. I got up and went back to bed into the same sleeping position. For both sessions I woke up in the same position.
Why is my second session different? Could there be clues in some other OSCAR graphics?
What I see unusual about the first session is that from 1:20 to 2:40 your EPAP is 16 or less, but there is no IPAP (red trace) showing. I assume your EPR is at 3 cm and your IPAP should have been at 19 cm or less. Perhaps an OSCAR display problem. Your second session is showing a requirement for even more pressure and some events. The number of events is not that concerning, but it looks like you may get some benefit from a BiPAP machine which can provide more than 3 cm of pressure support and IPAP can go up to 25 cm. Overall it looks like flow limitations are driving your pressure requirement up.
I switched on the EPR. My last night results:
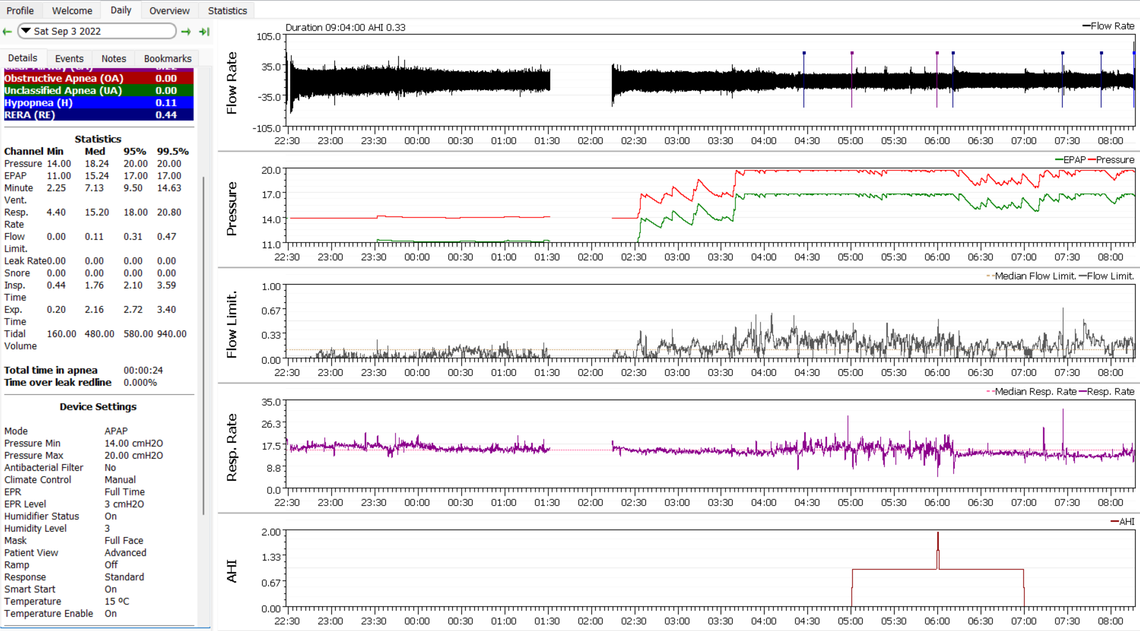
Following his part of my history with flow limitation:
Am I still a candidate for a BiPAP machine ?
Any other information or graph you would like to see ?
Unfortunately when your IPAP pins at the maximum pressure of 20 cm, that is an indication you may need to look at a BiPAP. Also the flow limitation issue can also indicate the need for more pressure support. The other option is to set an IPAP pressure limit of less than 20 cm and just accept the flow limitations. To a degree that is what my wife's preference is. She has issues with snore and flow limitation that could probably be solved with more pressure, but she says she would rather limit the pressure (14.4 cm), and suffer the consequences! I don't often actually hear her snore, but I also don't sleep with my hearing aids on.
As far as the graphs I always leave the event flag bar showing as it is more informative than the cumulative AHI graph.
One thing you may want to do is zoom in on the flow chart at those times when flow limitation are spiking higher and you are at the maximum pressure of 20 cm. You want to zoom in to the point where you can see each individual breath flow. My understanding is that flow limitation can be seen as a flat top on the inhale (upward) flow part of a breath cycle.
The other possibility is that if there are issues of asthma or COPD there may be medications (inhalers) which could help too. You would want to discuss with your doctor of course.
I understand from your last post that a BiPAP is the solution for the pressure and the flow limitation. More pressure would reduce my AHI and the flow limitation. If that is the case, then I should fight to get my lung doctor to change her prescription for a BiPAP. I am not certain I could convince a doctor to change its mind.
If I can't get a BiPAP, what would be the long term effects of flow limitation on my health?
To get considered for a BiPAP or BiLevel machine like the ResMed AirCurve VAuto you should show your doctor the graphs where pressure is hitting the maximum level of 20 cm of pressure, with flow limitations still spiking high. That is a strong indication that a PAP device with a maximum pressure of 20 is not enough for you.
And I am not sure that this pressure maximum is the the most important issue. It could also be that the 3 cm of pressure relief is not enough. You may need more than a 3 cm difference in pressure to adequately assist breathing and reduce flow limitations. The VAuto can go up to 10 cm of pressure support (differential between IPAP and EPAP). It is possible with a higher pressure support your maximum IPAP pressure could be reduced to a level lower than 20 cm. Just for example you may get away with a maximum pressure of 15 cm, but with a 10 cm pressure support. Then the machine pressure will alternate between 15 cm on inhale and 5 cm on exhale. This could be much more effective and more comfortable than what you are getting now, which is 20 cm on inhale and 17 cm on exhale.
Here is a short article BiLevel Positive Airway Pressure to look at.
In Canada the AirCurve 10 VAuto seels for about $2300 compared to the A10 or A10 AutoSet at $1300.
Just for example you may get away with a maximum pressure of 15 cm, but with a 10 cm pressure support. Then the machine pressure will alternate between 15 cm on inhale and 5 cm on exhale. This could be much more effective and more comfortable than what you are getting now, which is 20 cm on inhale and 17 cm on exhale.
I am confused. I can set my machine (AirSense 11) with a range of 4 to 20 cm. So I could set it to 5 - 15 cm. Is that what your saying? I had it set to 6 - 15 which is close.
It can be confusing as for some reason ResMed and others changed the vocabulary from the APAP machine to the BiPAP. Let me give a go at trying to explain each:
APAP - "Pressure" is assumed to be the IPAP (red on OSCAR). You set this pressure with a minimum and maximum. In your example 6 cm minimum, and 15 cm maximum. The machine will automatically increase and decrease the pressure (IPAP) within that range during the night. Independent from this you can set a pressure reduction on exhale EPR of up to 3 cm. So for example if the machine is asking for 10 cm of inhale pressure, and you have EPR set at 3 cm, it will give you 10 cm on inhale and 7 cm on exhale. On Oscar this is the red and green trace respectively.
BiPAP - For strange reasons that I don't understand they have assumed the convention that "Pressure" is now the exhale pressure or EPAP. This is likely for marketing and hype purposes. You can set a minimum and maximum range of that EPAP pressure just like in an APAP machine which it will adjust automatically during the night. Again separate from this you can set a "Support Pressure". This is like the EPR on an APAP, but is an increase instead of a decrease. This pressure support can be as much as 10 cm. If you have it set at 10 cm, and the machine wants an EPAP of say 8 cm, You will get 8 cm on exhale, and 18 cm on inhale.
The key difference is than on an APAP the maximum differential between EPAP and IPAP is 3 cm and is set with EPR. In a BiPAP the maximum differential is 10 CM and is set with the Pressure Support. Both EPR and Pressure Support create a differential between inhale and exhale which assists in breathing, but the Pressure Support on a BiPAP provides much more.
First, thank you Sierra for your patience with me. With age, my brain is getting slower than it used to be, I guess. :-(
Maybe I have it right now with your last explanation.
Please correct me if I am wrong.
With my APAP, when it requires higher inhale pressure, it will reduce that pressure on exhale by only 3 cm as fixed by the EPR setting being max 3 cm.
My exhale pressure being high would favor higher AHI and Flow Limitation.
The key to getting better results is then to get a lower exhale pressure than the limit of 3 cm below the inhale pressure.
With a BiPAP that would be possible, not with an APAP.
Keep in mind that I am not a medical professional. Like you I am a retired engineer with sleep apnea that is now pushing 73! Your summary is basically correct. My theory is that you need breathing assistance more than just higher pressure. Breathing assistance is gained with more pressure differential between IPAP and EPAP. My hope would be that with more differential, your IPAP would not need to be so high. The reason is that you don't seem to be having a high obstructive apnea frequency, and it is flow limitation that is causing your CPAP to raise pressure, when what you really need is more differential.
Engineers like graphs. This section of the VAuto Clinical Manual may help in understanding how they work.
Thank you again Sierra.
Now I need to build a good argument to convince my doctor to prescribe a BiPAP. You have provided much valuable information that will help. Thank you.
B.T.W.
My career background is with large hydro turbines and generators design, fabrication, field installation for 10 years and then client representation for large refurbishing and construction hydro generation projects for another 15 years.
Interesting. I spent about 35 years in electric power generation, starting with Ontario Hydro, and later in Alberta. My experience is primarily in thermal generation, and in the later years also some smaller hydro and run of river hydro.
Then you might know my former employer, Alsthom (before it was Marine Industries Ltd). My last project was getting the order for 3 turbine/pumps for the Corps of Engineer. Then I moved to Hydro-Quebec. Some of the projects I oversaw were refurbishing of Shawinigan 2 & 3 power house & dam, La Gabelle powerhouse & dam and finally the construction of dam and powerhouse Peribonka.
It is a small world :-)
Here I am once more with questions about flow limitation.
From advice on the subject, my case seemed to require a change of my AirSense 11 for a BiPAP (Resmed AirCurve vAuto).
I found that it is almost impossible to get such machine without a prescription which means I have to convince my lung doctor to change her initial prescription. So far I have not been successful.
I am thus trying to find more arguments to convince my doctor.
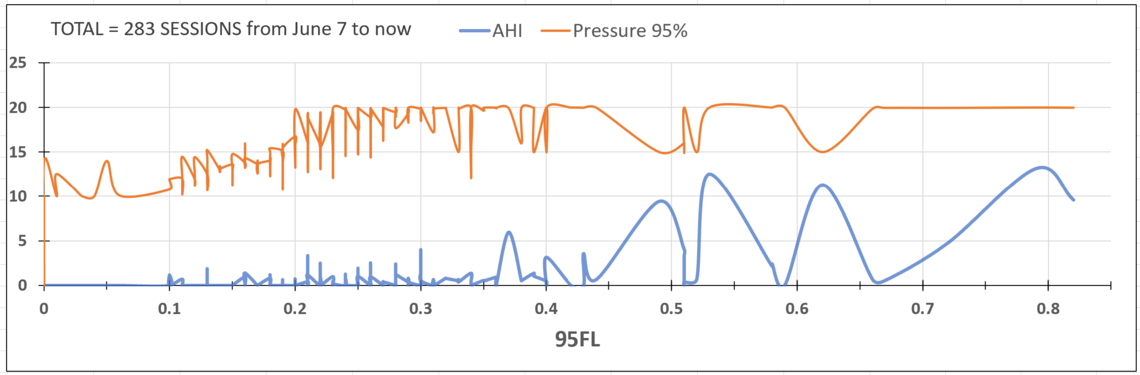
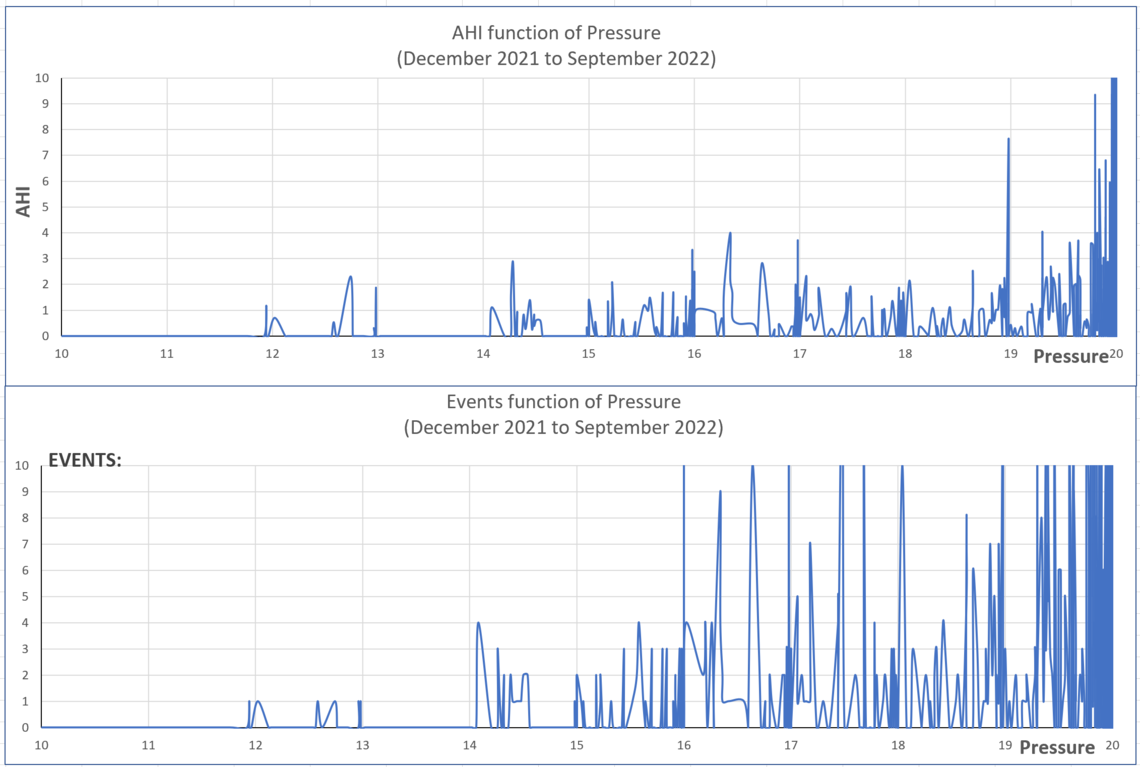
So, I took a different look at my results. Almost all graphs out there are time based. Showing different events per hour. I wanted to see if there is a relation between my AHI, my pressure and my flow limitation. Like you said, engineers like graphs :-)
The graph I produced confirmed pretty much one information I got that flow limitation under 0.1 is a good objective. You can see on the graph that below the 0.1 value for flow limitation, I have no events occurring. That is a clear indication for me.
Also shown on the graph is that higher the flow limitation is, higher the AHI also is.
From WiKi: .... Flow limitation may be inspiratory (during inhale) or expiratory (during exhale). It refers to any condition which impairs the flow rate of air through the respiratory tract.... Flow limitations can result from anatomical narrowing of the airway, airway obstruction, and positional obstruction where the airway is restricted due to an individual's sleep position resulting in occlusion of the airway (I am wearing a cervical collar). EFL may also result from intolerance to CPAP pressure during exhale. Both IFL and EFL seem to respond well to bilevel therapy where the exhale positive air pressure (EPAP) is a lower pressure than the inhale positive air pressure (IPAP).
So I do need to fight flow limitation which in my case sometimes goes up to 0.8.
I am thinking of presenting this argument to my lung doctor.
If you can improve/correct the above, please do so.
Thank you.
Yes, flow limitation and obstructive events are related. Flow limitation often precedes an obstructive event. I think your basic problem in getting a prescription for a BiLevel machine is that your current machine is getting your AHI below the standard 5 level which is considered acceptable treatment. It is struggling a lot to do it, and frequently is hitting the 20 cm limit of the APAP, but the average AHI is still reasonable from a medical treatment perspective. So, the AHI is the weak point of your argument for a BiLevel machine. Your strong points is the duration of time that the machine is at 20 cm of pressure. I would expect that is not all that comfortable and may impact your sleep, and she should be told that (if it is true). The big advantage of the BiLevel for you is not the maximum pressure increase, it is the Pressure Support of up to 10 cm that would be of value to you. She should know that Pressure Support is what is needed in the case of flow limitation issue. Again you would need to convince her that flow limitations are a problem affecting your sleep, and need to be reduced independently from reducing the frequency of obstructive events. It is a bit of speculation on my part, but I would expect your overall pressures would go down if you had more than 3 cm of pressure support. What you really need is breathing support from a bigger differential between IPAP and EPAP. This addresses flow limitation on both inhale and exhale.
The other evidence you could give here is a zoomed in shot of your flow rate during these times of flow limitation. Not sure what yours looks like, but my wife has higher flow limitation than I do, and here is an example when FL gets up to 0.5 or so. You can see that the tops (peak inhale flow) of the breaths are flat topped and irregular. If yours are similar, that would be something you could take an image of an show her.
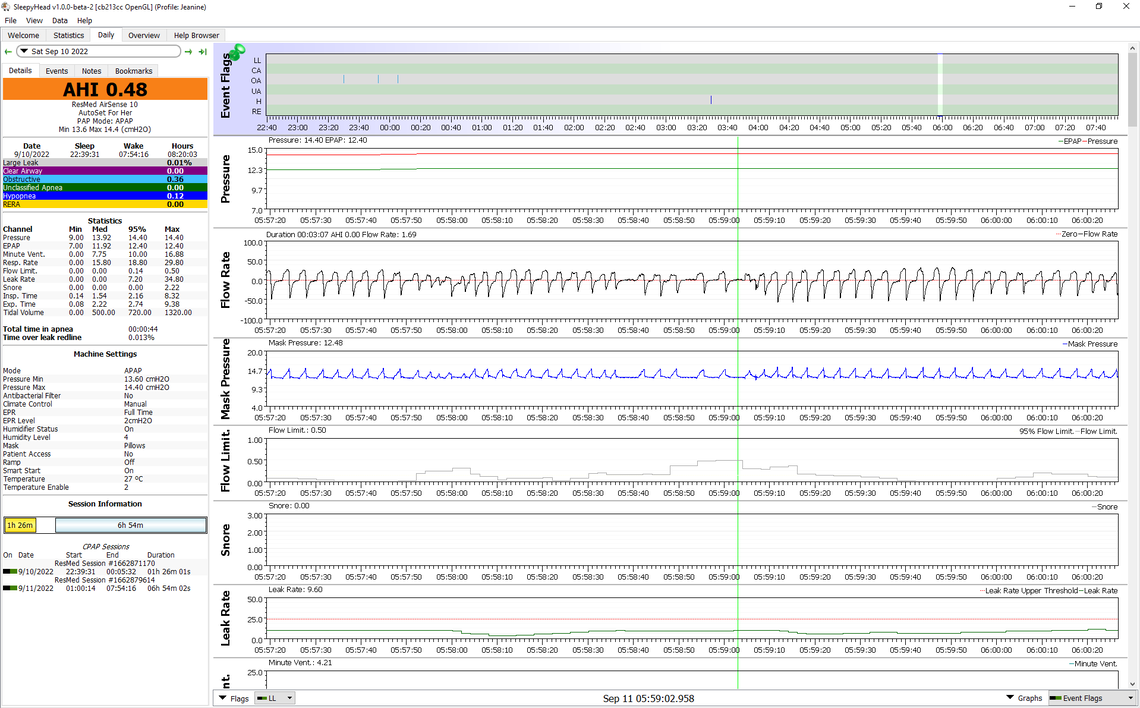
From the look of the flow chart it would appear my wife suffers more from flow limitation on inhale (up direction) compared to exhale.
Maybe it is because it is late and I can't get my fingers to hit the right keys, but this is my third attempt with this message.
To prepare my arguments for my doctor, I took a different look at the presentation of the data. Almost all graphs I have seen are time based and I thought of producing some based on the Flow Limitation.
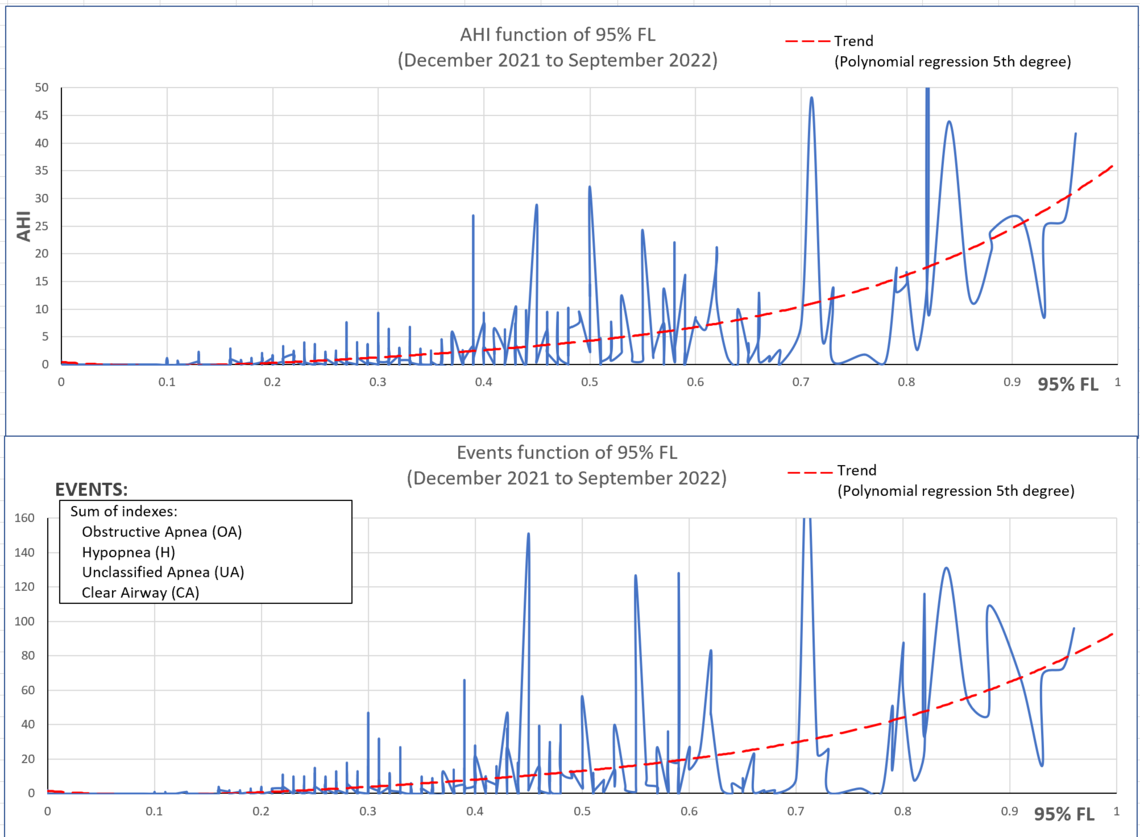
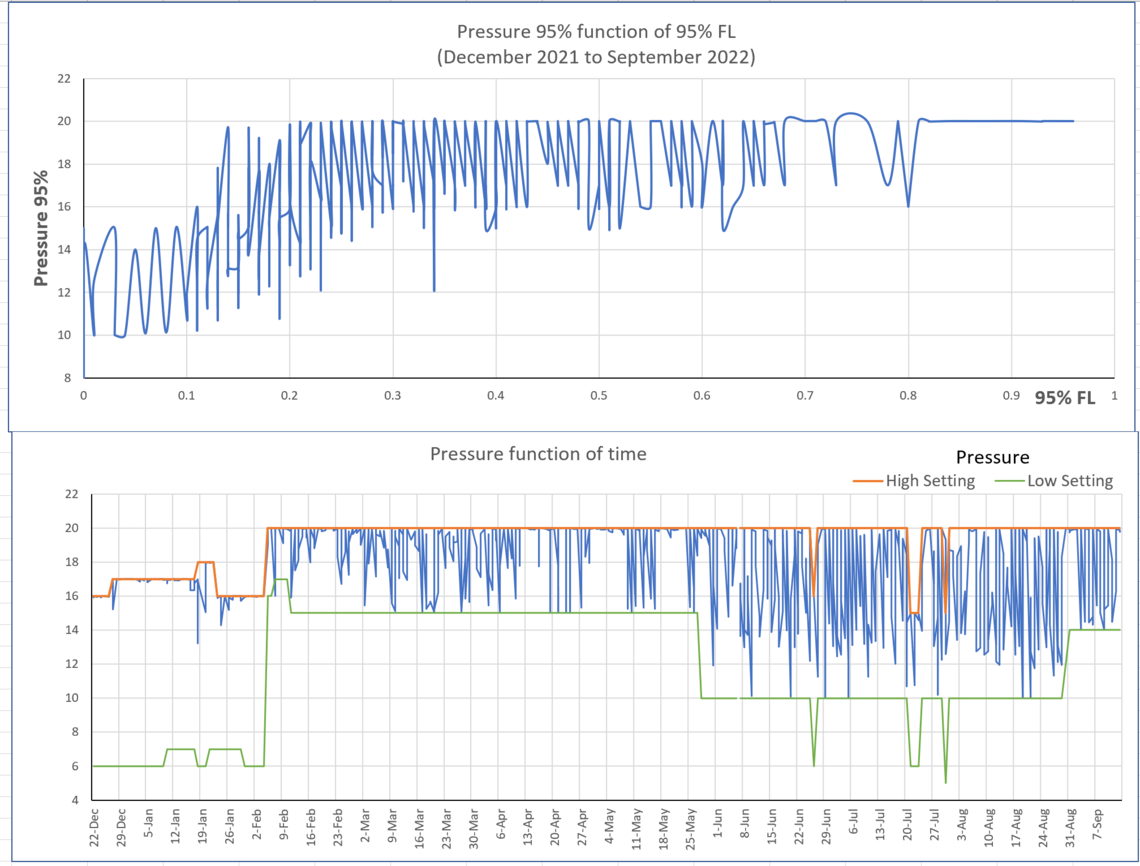
The 2 first ones demonstrate that if I can get my Flow Limitation down to 0.1 as I was advised, I should get much better results.
The 2 last ones show that the pressure is maxed out above 0.1 for Flow Limitation. Since it seems only a BiPAP (I think) can lower Flow Limitation, there is my argument.
I would again greatly appreciate any comments you would submit.
BTW, should you like to have similar graphs, I can make them for you if you are not too familiar with Excel. I would only need your CSV files for the period you would like covered. To keep private, you can send anything to my email address:
I hope this is also useful for you and many thanks again for you superd support :-)
Very nice graphs. There are two arguments for a BiPAP machine. One is that your APAP is maxxing out at 20 cm much of the time, and a BiPAP would be able to go as high as 25 cm in pressure. The second argument, which is a little harder to make is that your APAP can only provide 3 cm of pressure support (difference between IPAP and EPAP), while a BiPAP can provide up to 10 cm. I am not sure if you have any time where EPR was set at 0 cm or off? If there is and there is a difference in flow limitations between the zero setting and the 3 cm setting, it would support your case that more pressure support reduces your flow limitations. A pulmonologist should know that, but if you had some evidence to show that, it may be helpful. The other data you have is the shape of the flow chart which indicates flow restrictions on the inhale.
What is the situation in Quebec for coverage of machines? In Alberta our healthcare does not pay for any apnea machines. You either pay yourself or some may have private health insurance to pay for it. I recall someone saying that Quebec pays for an APAP. If that is the case the doctor may be under some obligations to show that a BiPAP is needed. I know in the US that when you deal with the DME system they have, there are criteria for each level of machine. You have to start with the basic machine and if that fails you can then move up a level.
One last thought is that if you are prepared to pay for a machine, there are no regulations that I am aware of preventing you from buying a used machine. My wife's S9 machine was on its last legs and there are no APAP machines to be purchased at one line stores. Our insurance does not cover them, so we pay out of pocket. All they seem to have now is a wait list which is months long. So, I started looking on Kijiji for a used machine. I found a virtually new A10 For Her machine where the seller was 10 minutes away. It had 94 hours on it. I bought it at half the price of a new one, thoroughly sanitized it, and my wife is very happy with it. I have read that about 1/3 of all apnea machines end up being not used and are sitting in a closet or drawer, essentially brand new. Many get them on insurance and are not out of pocket, so they don't care. That may have been the case in my wife's machine. All the seller said was that his wife could not tolerate it. So, of course, we have no warranty on the machine, and I am not sure ResMed would even take it in for repair. But, her S9 worked well for about 25,000 hours so I think the risk is low. The part about this option is that the relationship between you and your doctor may sour. They probably will not be willing to support you, and you would be on your own. We never had any support from a doctor, so that is a non issue for us.
I am not sure if you have any time where EPR was set at 0 cm or off? The EPR was off for 1.12% of the total time of treatment and is was set to Ramp Only for 7.49%. I don't think it is significative to see a difference since my stuff goes up and down all the time.
I have a private insurance that covers CPAP but they have a time period of 5 years wait before you can submit a new reclamation.
One last thought is that if you are prepared to pay for a machine, there are no regulations that I am aware of preventing you from buying a used machine.
I did search for used machine and found only dealers that still require a prescription to buy one.
The only one I found without the requirement is shown on Facebook. I sent the guy 3 requests for him to contact me. He never answered.
I did a few graphs based on pressure but I don't think they are very useful.
So I will now request an interview with my lung doctor and do the best I can to convince her to write a new prescription.