Hey All,
I could use some advice on tuning my CPAP machine for a complete beginner.
I did a basic in home sleep study and had a 21.1 AHI. Blood oxygen dipped to 91% but generally stayed 95-99%
On my prescription:
Diagnosis - obstructive sleep apnea Min pressure - 4 Max pressure - 20
I have completed my forth night using an Airsense 11, heated tube, and nasal pillows.
Night 1 - started a pressure 4 which was way too low to breath, I believe I upped it immediately to 6. I woke up in the middle of the night and saw AHI similar to my sleep study, so I bumped up the pressure more assuming the existing pressure was ineffective (I believe to 8). When I awoke, my AHI was down to 10.4 so I assumed the change was effective.
Night 2-4 - adjusted pressure up to 9. AHI came way down (avg 1.93). Had issues with sealing of nasal pillows. Had major stomach pains, which I believe is from swallowing air basically. I ordered a chin strap and a full face mask to see if those would help.
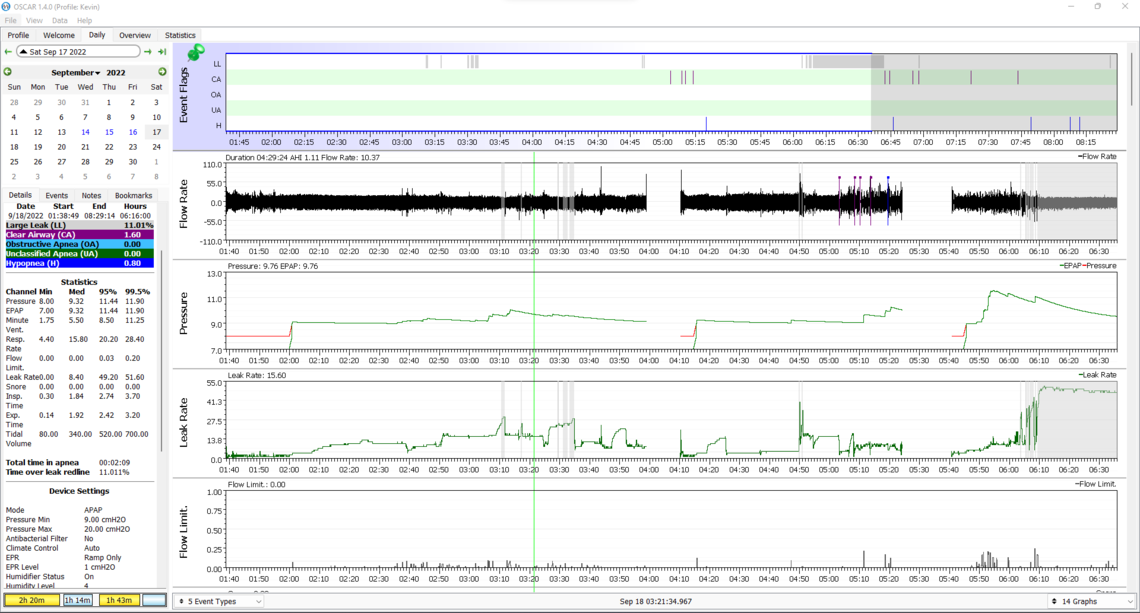
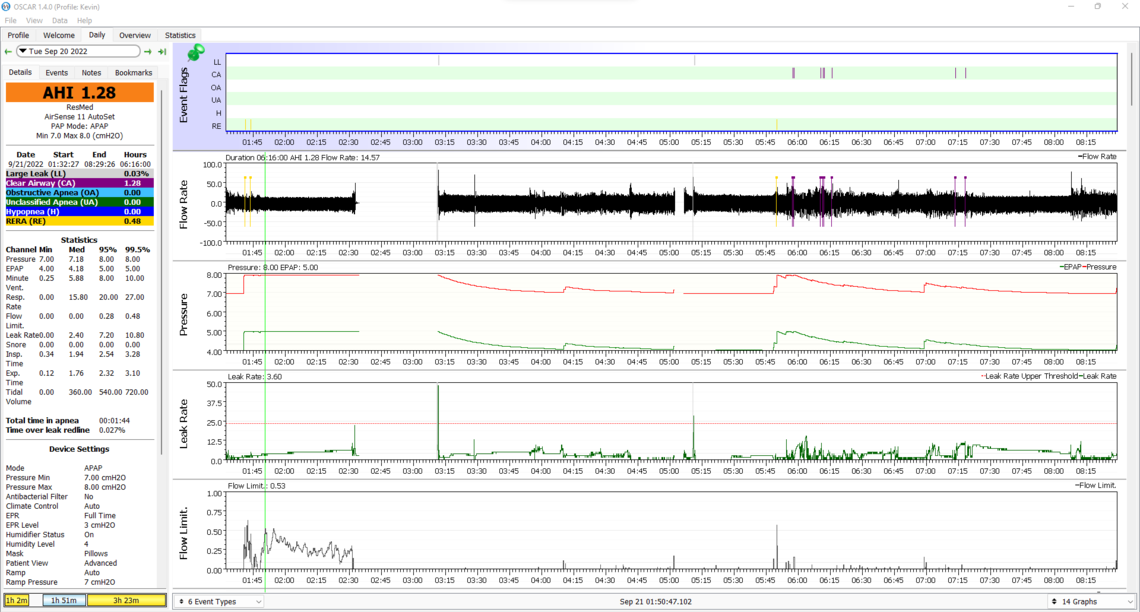
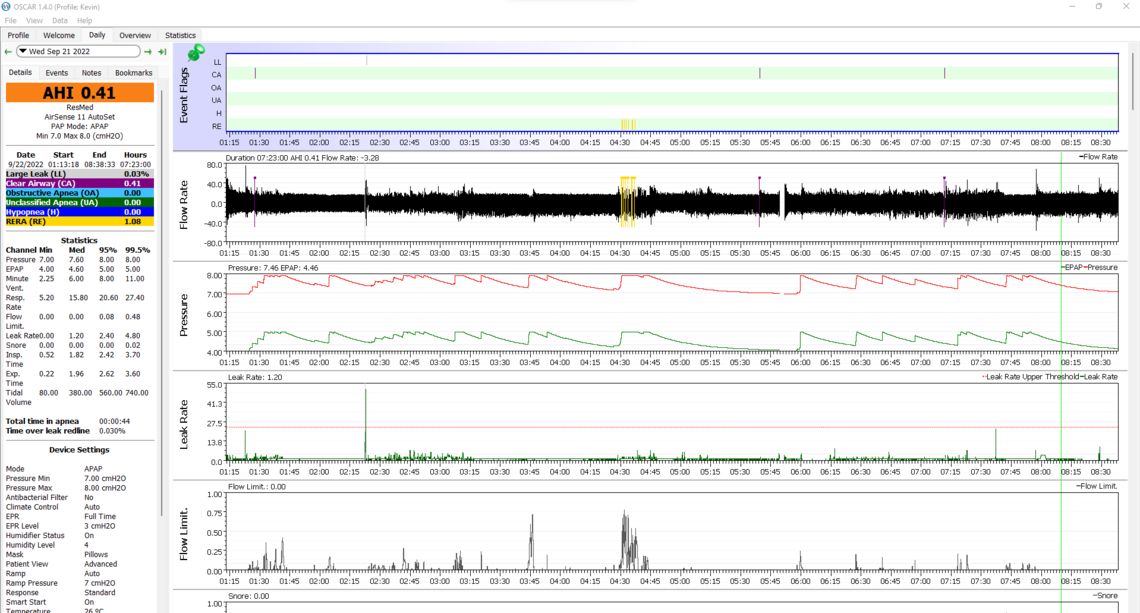
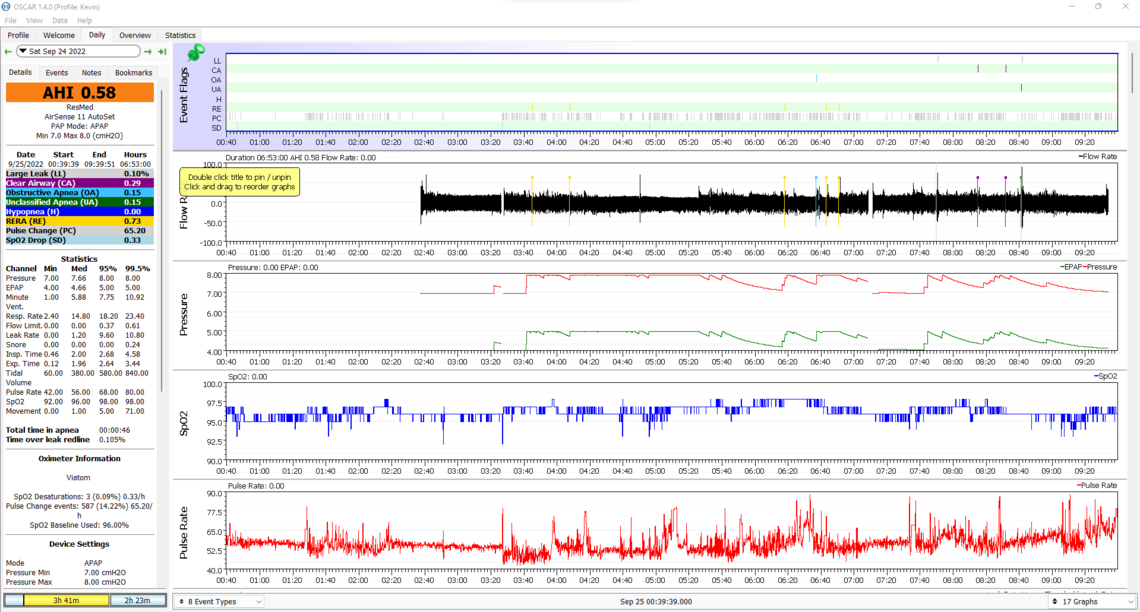
Night 4, I collected data for OSCAR. These were my results. Can anyone provide thoughts/feedback? I can zoom in on sections if needed. I plan to reduce pressure tonight by 1-2 and see how my AHI is impacted while I wait for the new equipment. My stomach has felt pretty terrible, and I expect that is the best approach for now.
Thanks in advance for any help you can provide!
Welcome to the forum. You are correct in that 4 cm is too low a pressure to be comfortable for most. It appears your machine was not really set up as from the factory it is set from 4 cm to 20 cm. A more reasonable setting to get started would be 7 cm min and 10 cm max. You might need a higher max later, but 10 looks like it would be fine for now, and may reduce the aerophagia (swallowing air). It looks like you are using the ramp set to Auto which is good. I would set the Ramp Start Pressure to 7 cm as well. It appears your EPR (expiratory pressure relief) is either turned off or set to Ramp Only. I would set it at 3 cm and for Full Time. EPR may also help with the aerophagia.
Your apnea events are all central apnea along with some hypopnea events. Turning the EPR on my help with the hypopnea. The central events are a bit more concerning. Central apnea (CA) events are not obstructive, and the airway is actually open. For that reason more pressure does not prevent them and can actually make the frequency worse. There is a condition called treatment emergent central apnea which you may be suffering from. It is your body's reaction to the pressure of cpap treatment. In most cases this goes away after 6-8 weeks of treatment. For now I would hope that is the case. Limiting the pressure may also help. There is no real need for a higher pressure as long as the obstructive apnea events do not go up. In any case I would try these new suggested settings first while you collect some more data.
Hope that helps some. Any questions, just ask. You can improve your OSCAR layout a bit by clicking on that black triangle beside the date to suppress the month calendar let some of the more important stuff show. The other thing you may find helpful is to right click on the Leak Rate scale, Dotted Lines, and then check off the box to show the Upper Leak Rate Threshold. It is a good guide as to when the leak rate is excessive.
Thank you so much for the advice! I'll definitely look into those changes - all super helpful.
I got another night of data last night with a slightly lower pressure (8-20) and had both lower CA and hypopnea events. With this adjustment in pressure, I did not seem to have the issue of air in my stomach, but I don't think I wore the equipment all night and didn't sleep for super long, so perhaps it wasn't a great test.
I did have some mask leak problems - I am not sure the nasal pillows are for me but I'm still experimenting. I will have a full face mask (f20 I believe) to try Wednesday.
If you or anyone else spots anything interesting or has more feedback, please let me know. This is all fascinating, and I'm looking forward to getting this all properly set. I have huge issues with memory and sleepiness, and I am hoping this will help improve that.
Thanks, again!
It seems that Flow Limitation is pushing your pressure up. This indicates you could benefit from changing EPR to full time, and increasing it to 3 cm. I would also suggest the same as my previous post with pressures; ramp start at 7 cm, minimum pressure at 7 cm, and max pressure at 10 cm.
Masks are hard. I have tried the AirFit F10 nasal pillow, Mirage FX nasal, Mirage Quattro full face, AirFit F20 full face, Swift FX nasal pillow, and now I am back to my first mask, the AirFit F10. If you can keep your mouth closed I think the F10 is a good mask.
Thanks for taking a look! I've made the suggested changes for tonight - fingers crossed for better results! I truly appreciate the recommendations and will get some fresh data and try to post results tomorrow evening when I am back at my computer.
I am hoping the chinstrap (also arriving Wednesday) and some practice still allows the nasal pillows to be doable, but at least I will have some options to test out!
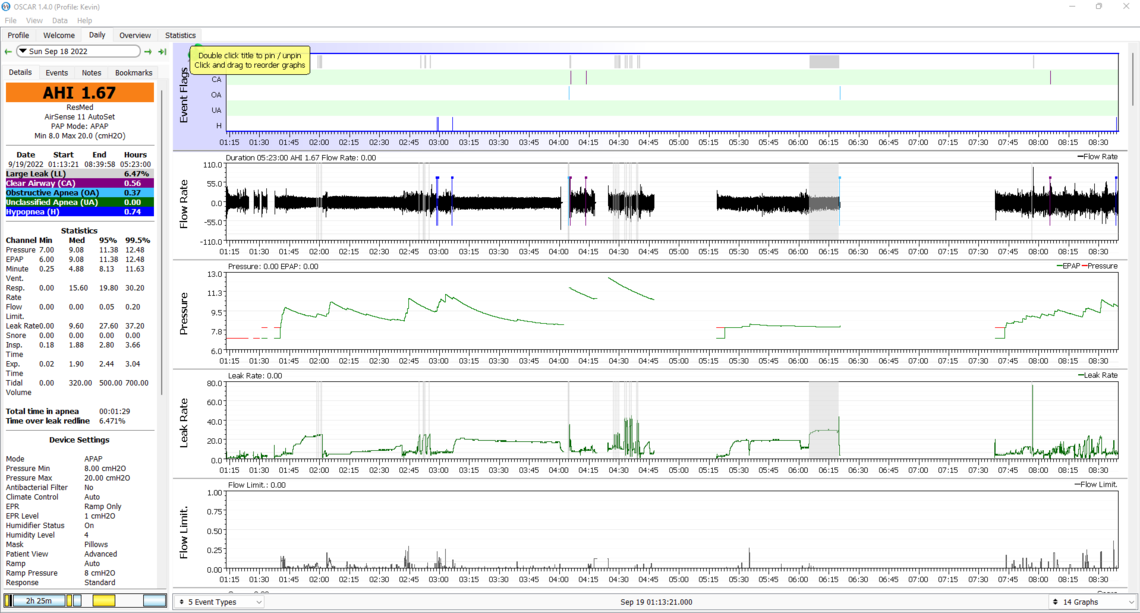
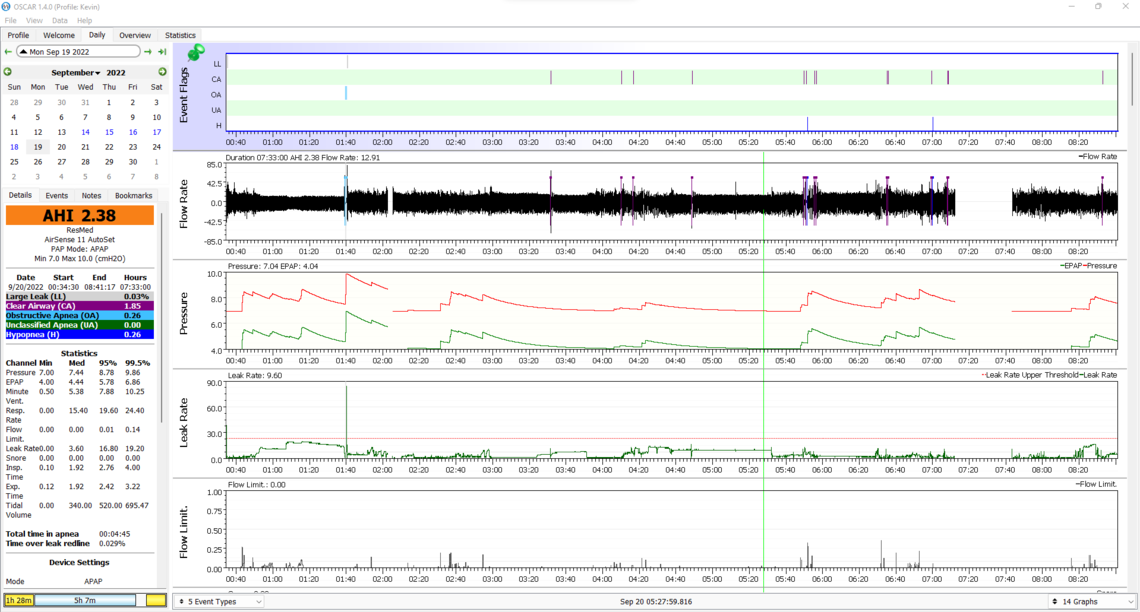
Here's my latest data after the suggested adjustments:
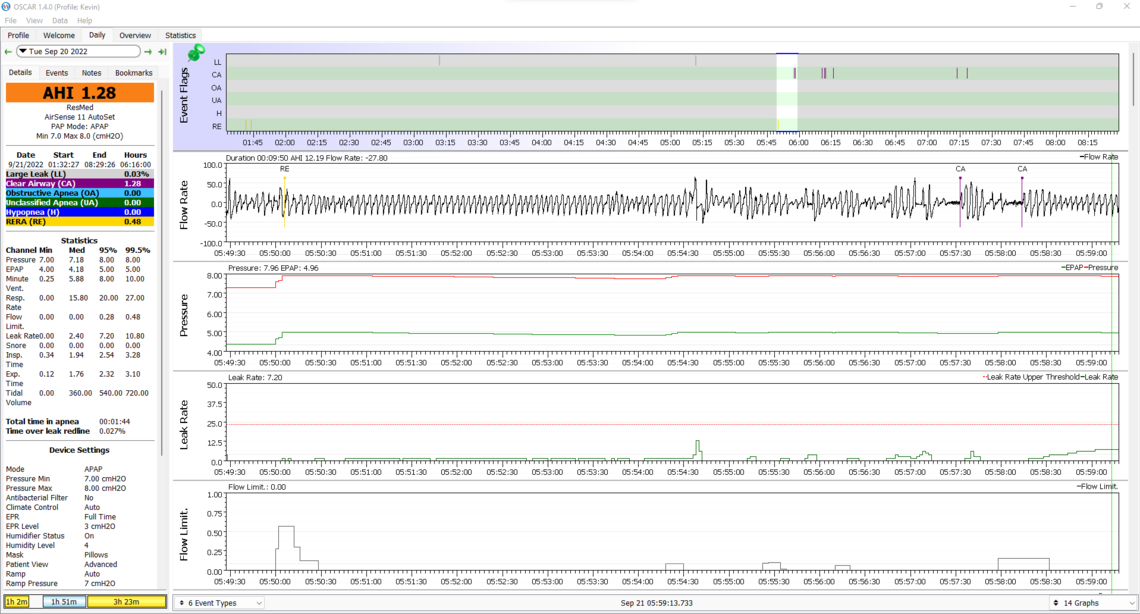
Well the good news is that hypopnea went down as well as flow limitations, and you only had 1 obstructive event. The obvious issue is the number of central apnea events, and more concerning is that with a few exceptions they don't seem to be happening when the pressure is higher. You have a couple of options, but I would suggest not doing them at the same time. First would be to reduce maximum pressure down to 8 cm. The other option would be to reduce the EPR from 3 cm to 2 cm. EPR seems to affect different people in different ways. One possibility is that the higher EPR has caused the central apnea events to increase. Central apnea can be caused when the CO2 and O2 oxygen control system is not stable. A higher EPR could decrease stability. I have central apnea issues and I have settled on an EPR of 2 cm, but I really did not do enough testing to determine if that is ideal or not. I do average under 1.0 now for AHI so I am not motivated to mess around with it more. How is your comfort level with the pressure? EPR should help with that.
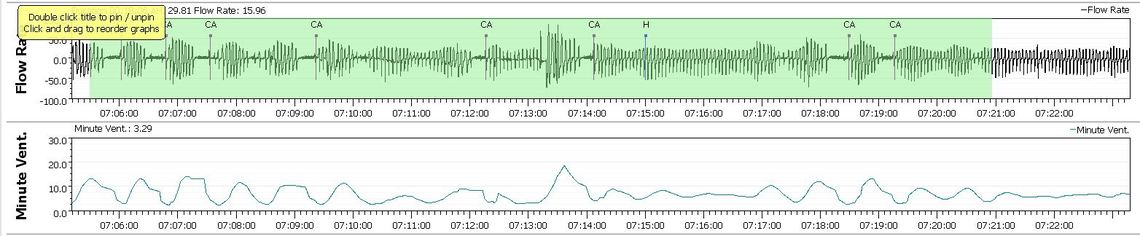
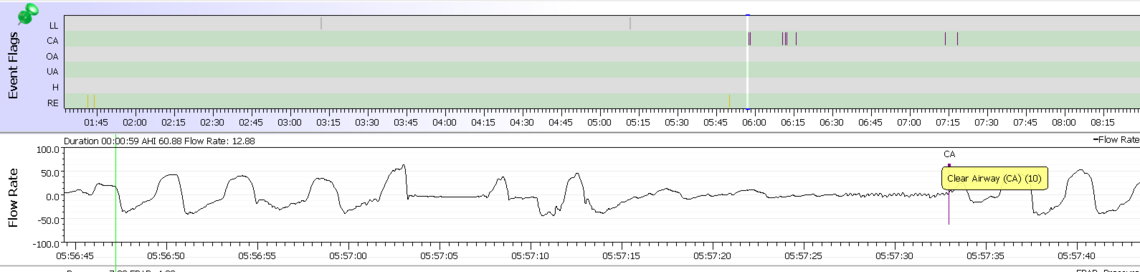
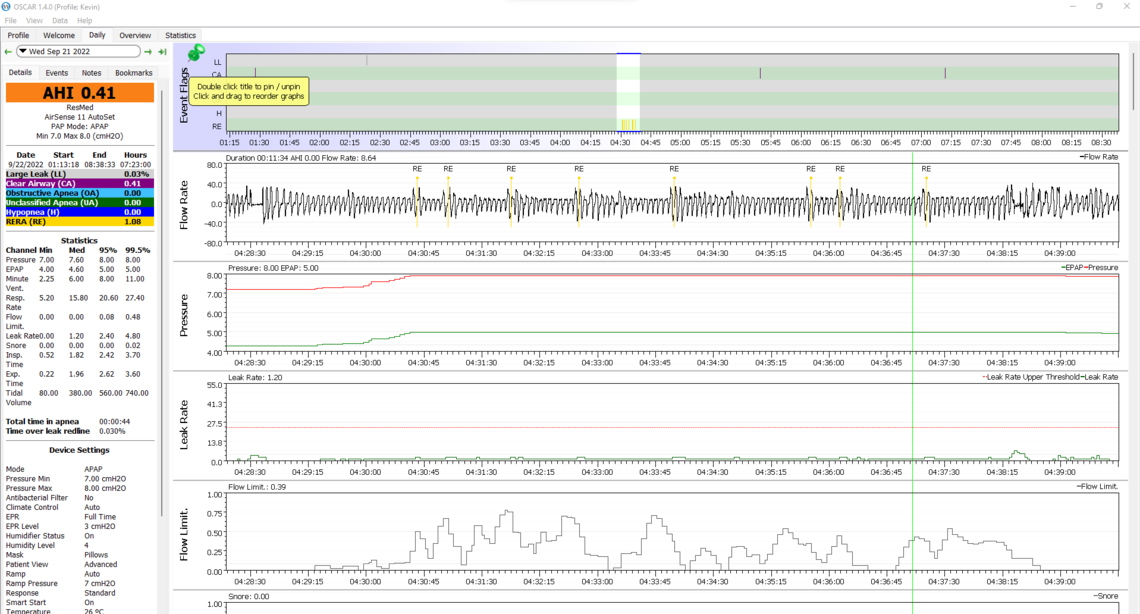
It might be informative to see what the breathing pattern looks like when you zoom in on those CA events. Sometimes they are just caused by waking and going back to sleep. Other times they are a regular pattern that ends in a CA event. Here is an example from my records of the latter. It also may be helpful if you could scrunch down the graphs to fit Minute Ventilation in as well. I limit my leak graph to 50 to save space. If you hit 50 it is bad and you don't need to see the detail... You can also click and drag on the horizontal grey bars to get more in as well. Minute Ventilation is a good indication as to how regular your breathing is. If it cycles up and down like shown below, it is not stable. Ideally it would be a flat line.
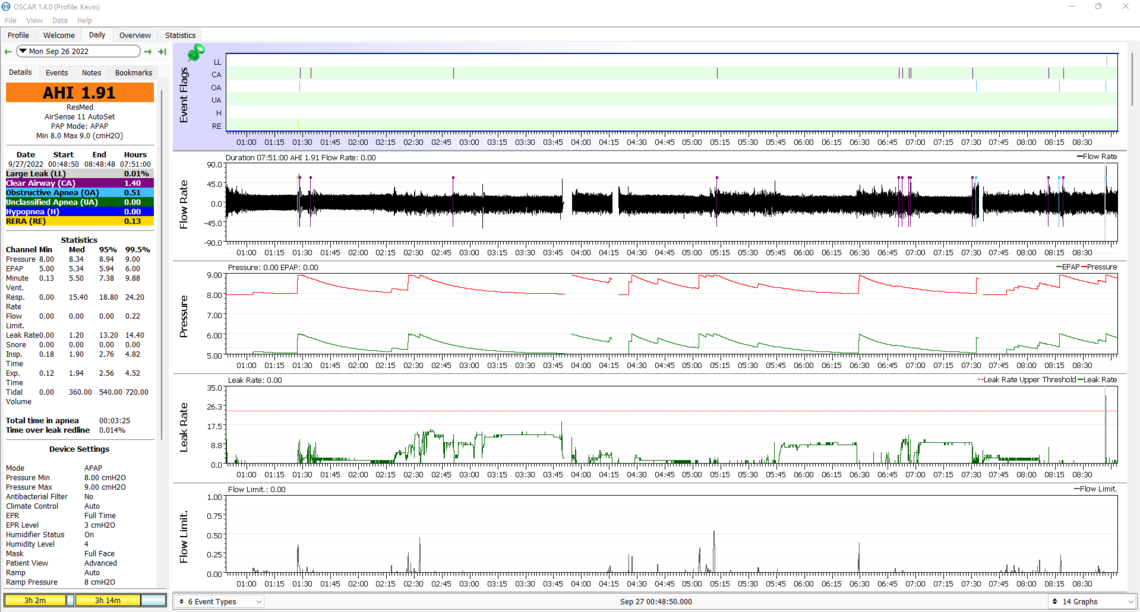
Here is last night's data with maximum pressure reduced to 8 and no other changes. My humidifier may have ran out of water at some point in the night. Today, I definitely noticed aerophagia which became apparent kind of midday, which I did not feel the previous night. I had a few drinks with a friend before bed, so I don't know if that impacted anything.
I do notice our flow rate curves look different. Not sure what that indicates.
Chin strap and full face mask are here today. I am tempted to try the full face mask tonight to see how that is.
Thanks Sierra for all the help!
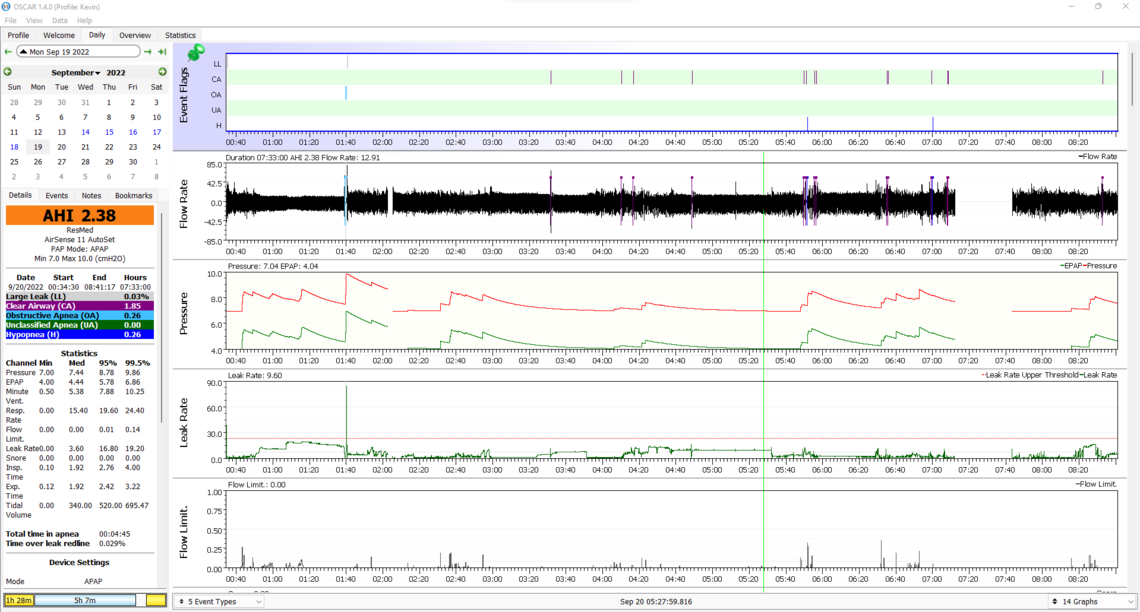
Again the good news is no OA or H events. Flow limitation is up when the pressure has been limited to 8 cm though. In your second clip I do see some indication of instability in breathing control. See the section circled with yellow highlighter. Notice how the breathing rate gets deeper and deeper and then more and more shallow until a CA event occurs.
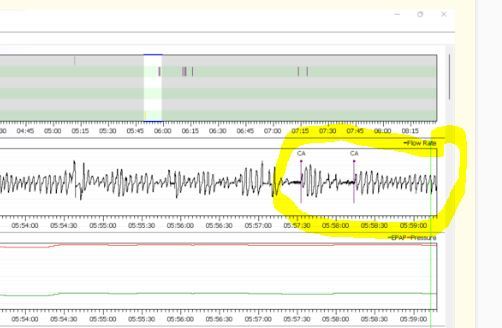
It still would be interesting to see the Flow Rate chart next to the Minute Ventilation graph for some more of those periods of time where there are multiple CA events. Minute Ventilation is a measure of how much air is being brought in and out of the lungs. It will cycle when the breathing rate control system is not stable.
The basic problem is that an APAP can't directly do anything to stop CA events. The pressure from the machine may in fact be the cause of the CA events. So, about all you can do is reduce pressure. But, there is obviously a limit to how much you can reduce pressure. What you may have to do is stick with it for some time to see if this is treatment emergent central apnea that will go away after 6-8 weeks or so.
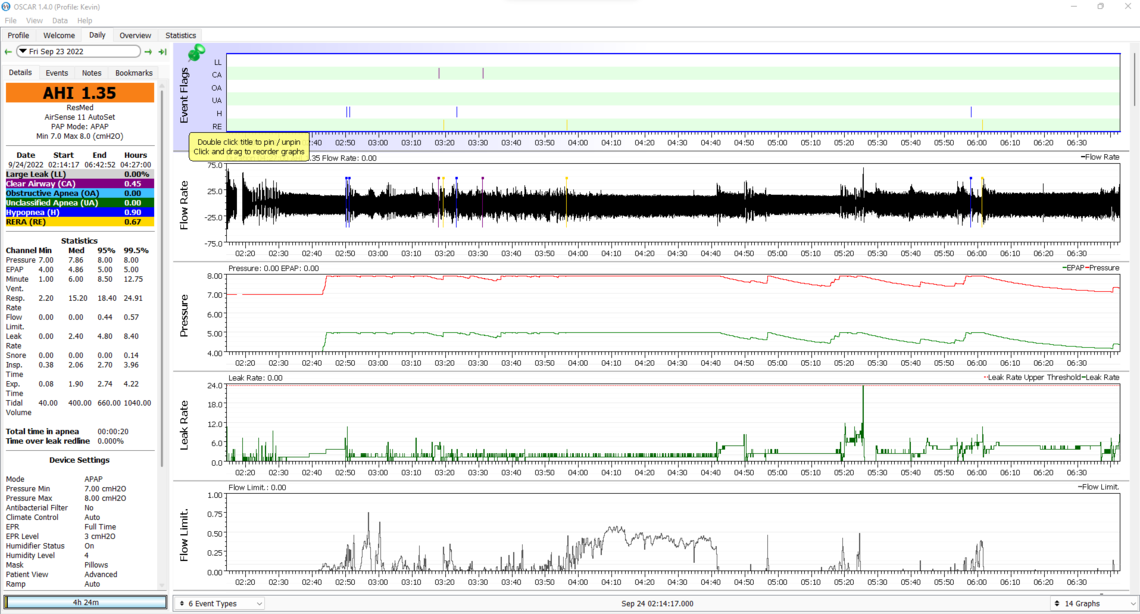
I can grab more data if needed, but I think last night's information is promising and worth reviewing first. I wore the chin strap that came in with the nasal pillows, and I think it made a significant difference:
If I'm interpreting this right, it looks rather encouraging. Do you agree?
Thanks!
Your leak rate certainly has improved. Did you sleep well? I find that the better I sleep the worse my mask leaks are. I almost take it as a sign that I was not really sleeping...
The overall score is certainly good. I have not seen consecutive RERA events like that before though. Flow limitations were high at the same time. This may be the price of limiting pressure to 8 cm.
Some have some success with wearing a soft cervical collar to keep the neck straight during sleep. They are inexpensive and can be found at Walmart. Not sure about the comfort though as I have never worn one.
I did sleep well - I only remember waking up once in the night instead of a bunch of times. However, in the morning, I felt more tired than I usually feel for some reason, so it was odd. Not how I was expecting to feel. I am wondering how tonight will go - I am planning to not modify anything and see how the data changes.
The RERA events do seem strange. I also had some data on Tuesday night that didn't look particularly good, but of course I don't really know what I'm talking about at this point. I didn't get a chance to highlight this the other day, so I'll include it now.
The chinstrap worn last night wasn't my favorite, but it didn't bother me all too much and seemed to make the nasal pillows fit a little better. I wasn't able to improve the seal to the same level with just the strap adjustments on the nasal pillow oddly. I'll stick it out with the stylish chin strap for now haha. My stomach also wasn't full of air when I woke up which might be reason alone to keep at it with the chinstrap. Hopefully I'm in for another night of solid, but more restful sleep!
It looks like my CA events have been somewhat on the decline, so perhaps my body is beginning to adjust to the CPAP machine. I believe I took the CPAP mask off prematurely on the night below though which would impact quantity of CA events.
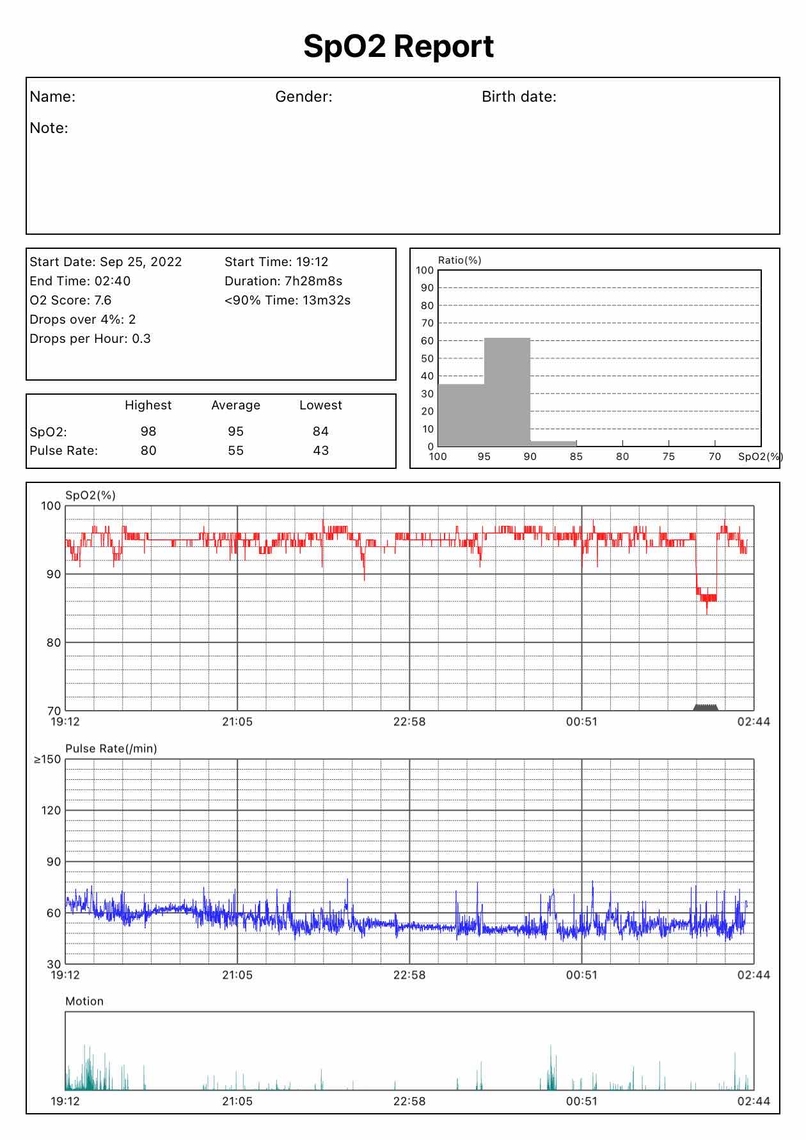
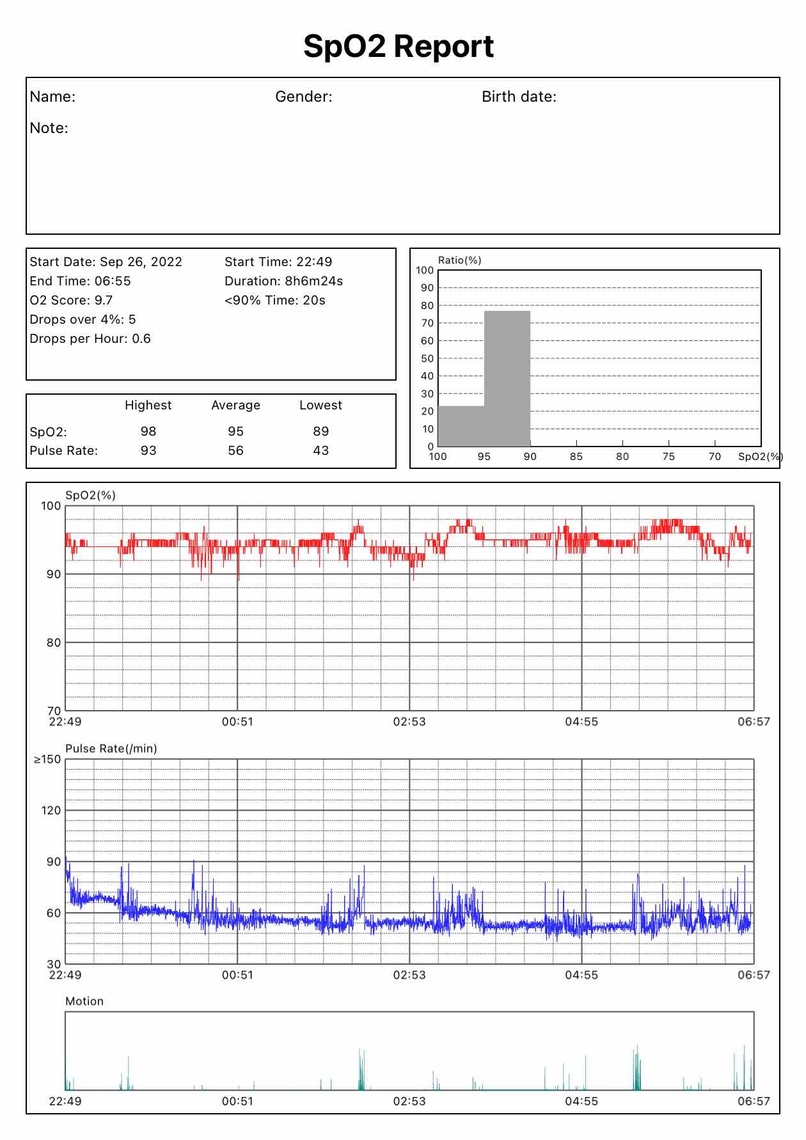
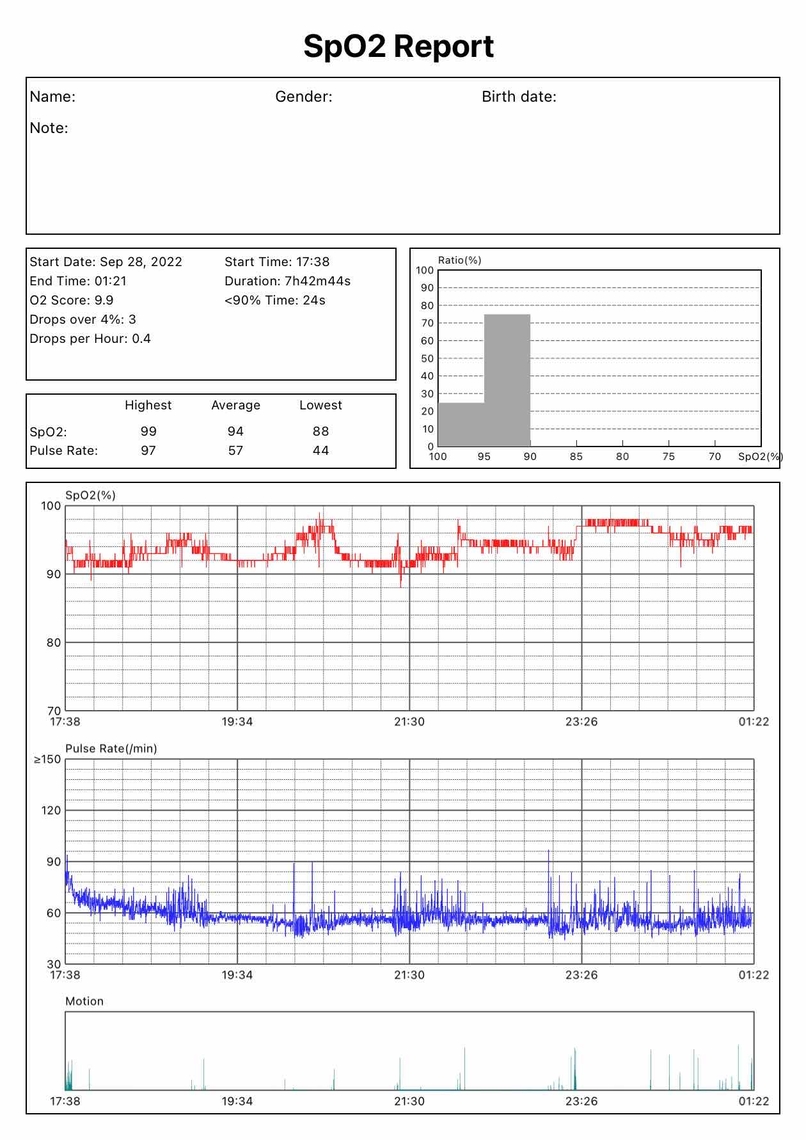
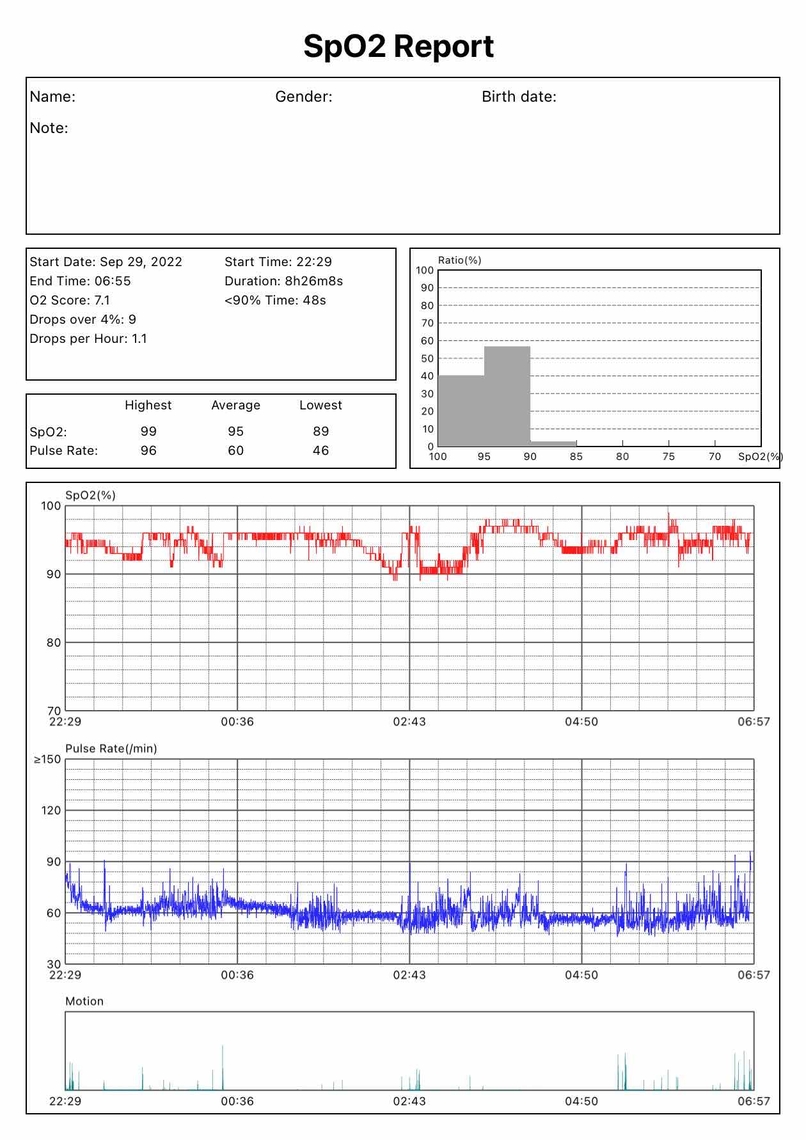
Last night, I introduced a Ring02 sensor to better monitor impacts on blood oxygen (not expecting significantly accurate data). Below is the updated chart. I began wearing the 02 sensor slightly before starting the CPAP machine, so that shows in the data. I'm not sure if there is a better way to order the graphs - I can adjust if needed.
I will say that sometimes when starting my CPAP machine, I maybe wish there was a hair more pressure (I can feel ever-so-slightly out of breath, nothing terrible) but I'm a little unsure if I should be tweaking anything at this point, as results don't seem too bad. I can't say that I feel much in the way of a positive effect from the CPAP yet though.
Since your CA events seem to have settled down a bit you could try increasing your minimum pressure to 8 cm, and also set your ramp start to 8 cm. The maximum pressure would have to be increased as well to do this, so I would suggest 9 cm max. This will allow the machine to increase pressure higher than it can now. You will be able to see if this helps with the breathing while going to sleep, and whether or not the increased maximum causes the CA events to go up. Depending on how this goes you may want to pick a pressure and go to the fixed pressure CPAP mode. As it looks now it would appear that 8 cm would be a good starting point. My thoughts would be to go to an 8 min and 9 max first to see if you can learn a bit more about what is impacted by pressure.
I have never used an O2 meter so can't really comment on your results from experience. However it looks like for the most part you are staying above 95% which is good.
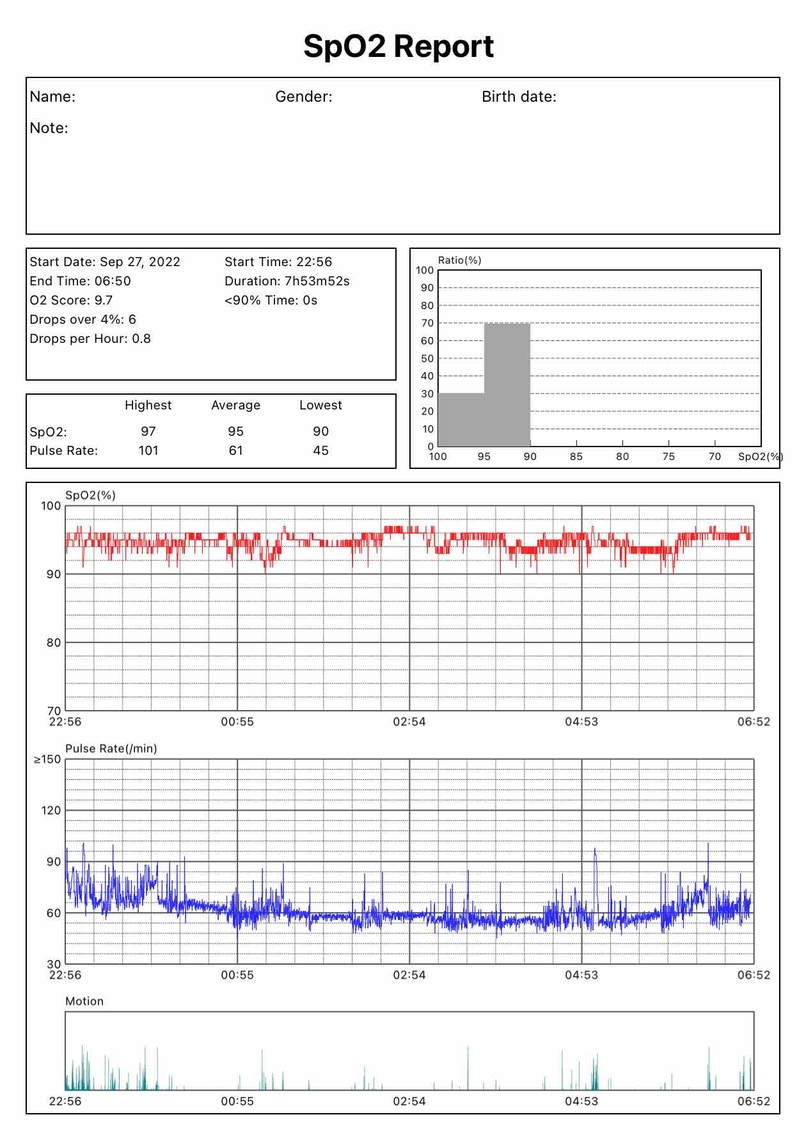
So I have been gathering data, and here are some results from the past five nights. Mostly settings have not been adjusted other than the 28th. Blood oxygen has been somewhat low sometimes - I am having syncing issues with Oscar and the 02 ring, so for now I have included the report exports. If you or anyone has thoughts, please let me know : )
25th
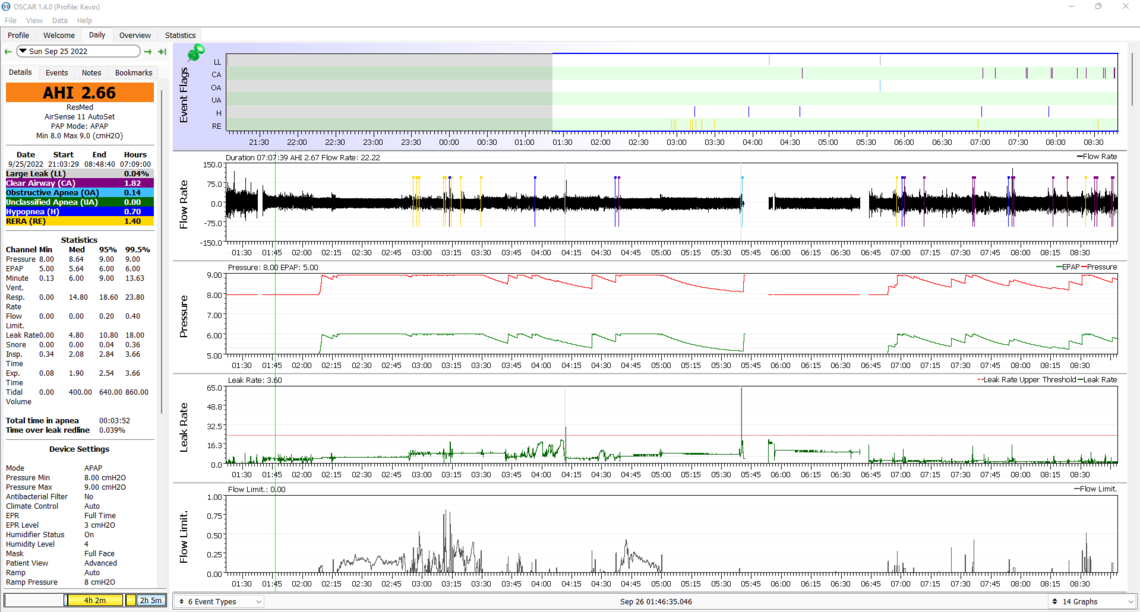
26th
27th
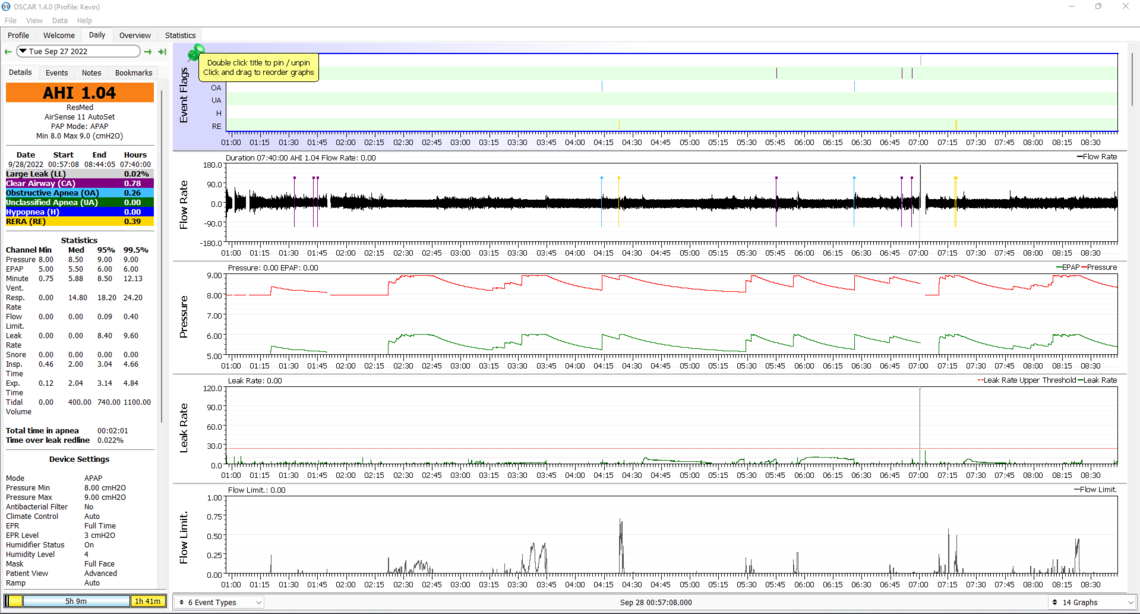
28th
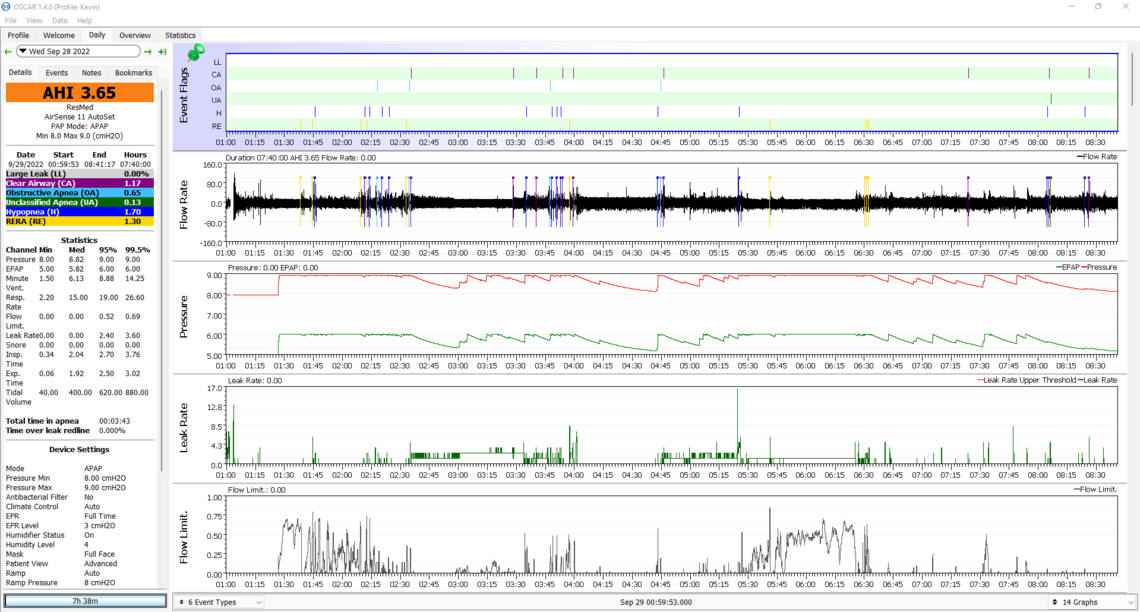
(the above day was using the full face mask due to nasal congestion)
29th
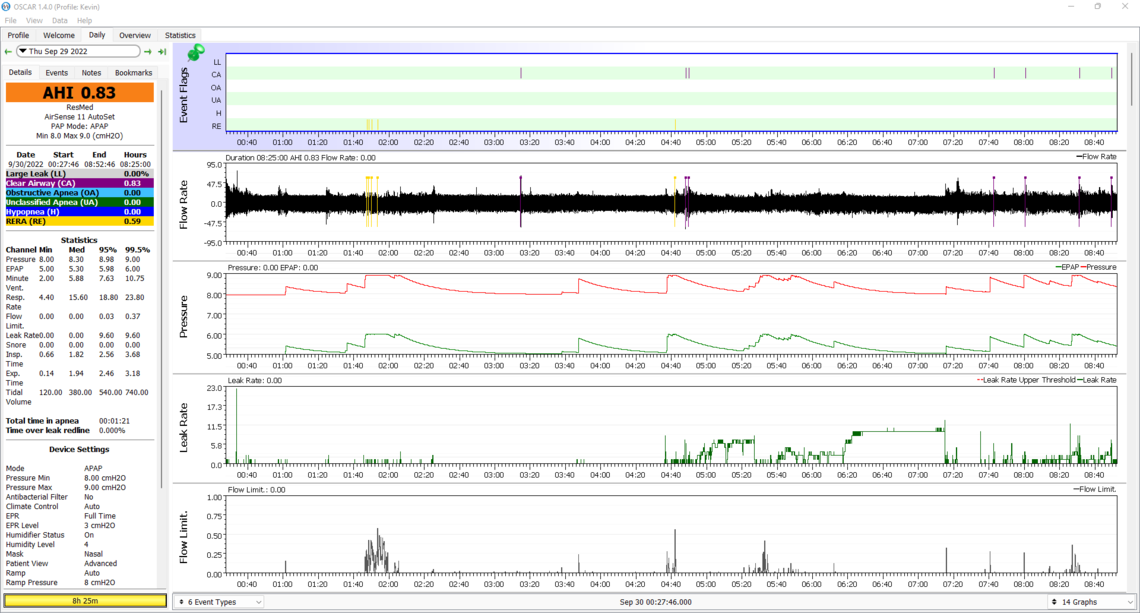
Those results are kind of all over the place, and I am not coming to any firm conclusions as to what is going on. I think at this point you may want to try simplifying things and switch your machine to fixed pressure CPAP mode with a setting of 8 cm. If OA events do not go up a lot, then you may even want to try CPAP mode with a fixed pressure of 7 cm.