I have a Resmed Air Sense10 Respond and Airfit p10 mask. I almost always have under 5 events per hour. I usually don't take my mask off more than twice. I usually sleep between 7 and 8 hours a night. The only thing that changes much on the dashboard is mask seal. It seems to vary a lot. Some days I am so tired I can barely function. Other days I'm perfectly well rested. Other days are between the two. So I started to check my dashboard later in the day to see if I could figure out why. I checked later in the day so that I wouldn't prejudice it by "becoming" tired after seeing my scores. I waited to see how tired or not tired I was before checking. I even kept a spread sheet for two weeks and added in things like how late I ate, when did I have caffeine, etc. The only thing I could find that really affected it was mask seal. My doctor and the guy at the cpap store said that my machine compensates for this and if my events per hour level was fine I should not be tired. Well, I am. When my mask seal score was very low, I was very tired. When it was high I felt great. This doesn't correlate to events per hour, which would make more sense. Any ideas?
I have an AirSense 10 AutoSet, but I do not use the MyAir app. I take it that a low Mask Seal score indicates high leakage rate? I will base my comments on that assumption.
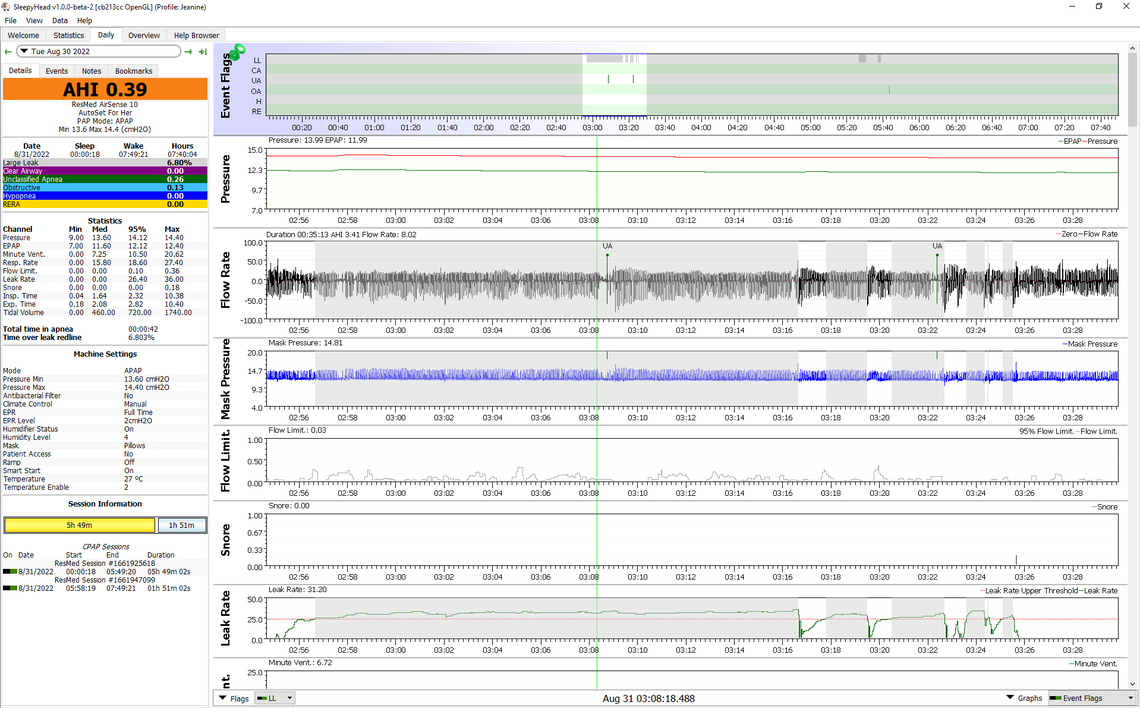
I agree with the CPAP store statement that the machine compensates for leakage in most cases, but it can affect the reporting of events. ResMed calls leakage up to 24 Liters per minute acceptable. But above this 24 L/min redline it still tries to deliver the set pressure, but it suppresses the reporting of events. When you look at this using OSCAR freeware, these high leakage times of the night are shown with a shade of gray. See a zoomed in report screen below for a period of time when leakage is above 24. You can see that events can still occur, but they get flagged as UA events (unidentified apnea). I don't think they get counted in the AHI score for the night, and I am not sure if MyAir tracks them. They are still apnea events though where air flow rate is interrupted. But this graph also shows that despite the long time with leakage high the pressure is maintained.
With respect to leaks the P10 mask is pretty good as long as it stays on your head and nose. But, one issue with a nasal mask is that you can open your mouth during the night. This causes a significant leak and in addition it can cause a dry mouth and discomfort. Your leaks may or may not be due to this happening. And, it may be affecting your sleep quality. Some people use a chin strap to prevent this from happening.
Thank you! That is excellent information. I will see if I can figure out OSCAR and report back. I am interested in those UA events. I will try a chin strap tonight. I actually have one, but I haven't used it! Meanwhile, my L/min averages about 24 for the past year with an average of 4.47 events per hour, according to the MyAir report. This month it has averaged almost 28 L/min with 2.99 events per hour average. I'm confused about what an acceptable L/min is. Also, I don't understand why having low events per hour with high L/min would leave me tired. It seems like low events means that the apnea is under control. Is that true, or am I missing something here?
For leakage I look for Time Over the Leak Redline to be zero or close to zero. My wife (which is where the example report above is from) averages about 2% of the time over the leak Redline and 4 L/min for average leakage rate. I average a little lower for % of time over leak redline at 1.25%, but my leak rate average is higher at about 7 L/min. Overall her long term average AHI is 0.46, and mine is higher at 0.83.
If you get OSCAR working you should find out a lot more about what is going on. You need a PC or Mac and a SD card reader to get the data from your machine into OSCAR. And, if you post some typical Daily Report screens here you can get some comments on what may be opportunities for improvement. While an AHI of less than 5 is the clinical guideline for effective treatment, I suspect most CPAP users do quite a bit better than that when their machine has been optimized.
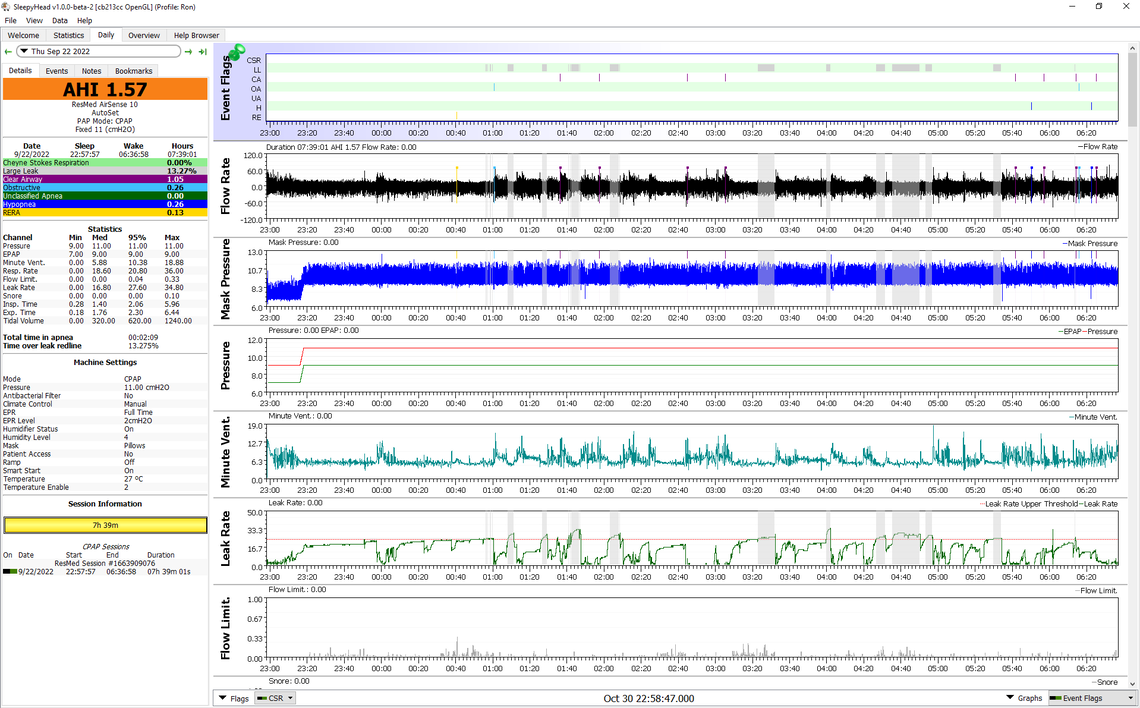
It is hard to get good results every night. While overall I think I am doing ok, some nights are very good, while others are not so good. Here is a night from last month where my time over the leak redline was over 13% and my AHI at 1.57.
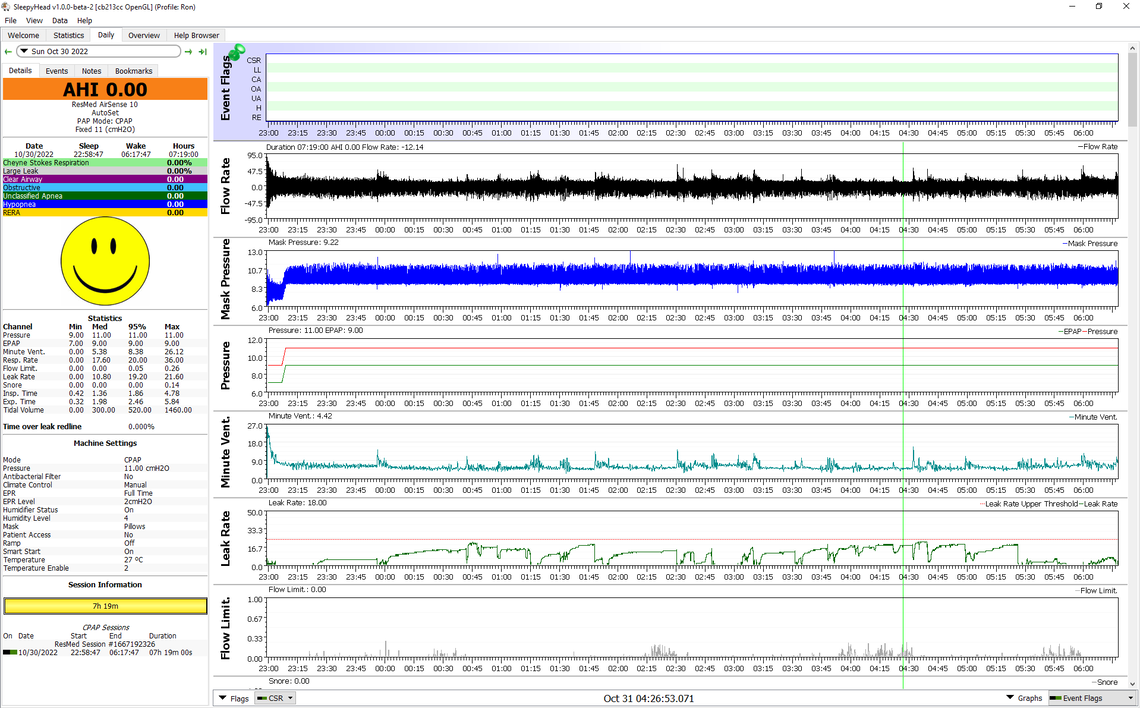
And here is last night which was as good as it gets for me. 0% of the time over the redline, and 0.0 for AHI. That does not happen very often...
Thanks, Sierra! I'm going to get some help from my husband or daughter to get OSCAR going. I will report what I find. It sounds like even when MyAir says my leaks are fine, they really aren't. I've been using CPAP for 20 years, but only just realized (since I've retired) that when I feel depressed, anxious or irritable it probably relates to bad nights with sleep, even though it seemed like I slept well. So I've been trying to figure out why. I think OSCAR may give me some answers. I really appreciate your help.
We just realized that there is no SD card in my machine. I called to see if maybe the cpap store took it out and forgot to give it to me, but the guy who helped me isn't in today. Or maybe my doctor took it out a year ago, or maybe it was never there. is it possible to get a new one?
Is your machine a ResMed AirSense 10 AutoSet? If so, ResMed claims they ship every machine with a 4 GB SD card. Unfortunately it seems to be the practice of some dealers to remove the card. I think this is a dirty trick, possibly to keep you from looking at your own data, and therefore increasing their after care business. The unfortunate part of this practice is that all the detailed data is lost when the card is not in place. MyAir only sends very high level summary data, but no detailed data. However, you can put a card in and start to collect data. Any 4 GB to 32 GB SDHC standard sized card will work. You may have a suitable card around the home that came from a camera or other device no longer being used. The machine formats the card the first time you put one in, and it will start collecting data that night forward.
Here is a link to a Clinical Manual for more detailed help on using the machine.