I've been on Cpap for 5yrs. Pressure @ 15 *Went for last study in June(?). They said i "woke up a lot" w/very little REM. Pressure then was 14. *Reason for study @ 4.5yrs was on 10/21 I was found to have an Olfactory Groove Mengioma, Dr recommended study saying "things may have changed". Successful operation 11/21. Tumor was found incidentally on CT while at ENT (ENT said I need sinus surgery, throat surgery (narrow) & Allergy drops) *Been wrestling with feeling fresh thru the day, but a 20-30m power nap will fix me up. *Reason for Bipap recommendation is because of higher pressure being recommended, & possibly less pressure on exhale, hence Bipap. *After 5yrs my Insurance allows new Cpap/Bipap *Dr recommending an Ambien because I woke up a lot at last study and didn't get REM. *Last 10 days = average 10 events an hour per myAir. *Mask Seal = 15 using AirTouch F20 **Only discovered myAir 2 weeks ago and just heard about Oscar today on this forum. *Only feedback that I was getting on Cpap #'s (leaks, events) were from Dr or PA. Very dissapointed they at least didn't tell me at least about myAir. *58yrs young and fit. 5'8" @ 165lb. Work out 7hrs a week cycling (main activity). *Any disadvantage going Bipap route? *Never took Ambien before? Ok before study? Your insights and experiences are welcome
It sounds like you have been through quite a bit... But, it sounds like things are under control. Welcome to the forum.
BiPAP - There is no significant disadvantage to using one, but it may not be necessary. They supply pressures up to 25 cm instead if the usual 20 cm with a CPAP. The BiPAP also allows for a differential of up to 10 cm between inhale and exhale. The APAP or CPAP usually only allows a 3 cm differential. Normally a BiPAP is not used unless you need pressures higher than 20 cm, or if you need some breathing assistance by the higher differential. Normally that would show up as a higher hypopnea incidence, high flow restriction, or RERA. With an AHI of 10 that is an indication there is room for improvement. The standard treatment goal is to be under 5 for AHI, and more ideally under 2.
I don't think there is a problem with Ambien during the study, especially if you are not having any significant central apnea events. What is your breakdown of the type of Apnea events being reported? On an ongoing basis I don't think using a sleeping aid is the way to go. There are other sleep hygiene methods that may work better with less risk. See this link for more information. The site was started by a pharmacist that was concerned about the over use of sleeping pills in seniors.
Have you downloaded OSCAR? If you have and want to post a daily report screenshot I can give you my thoughts on why the AHI may be high at 10 events per hour. Do you have a fixed pressure CPAP or AutoSet machine. I recall the most basic CPAP does not have a SD card to capture data. OSCAR is the best way to find out what is going on. MyAir really only provides summary data and is more intended as a compliance tool to see how much you are using the machine.
Hope that helps some,
Thanks for your response! Cpap = ResMed AirSense 10 "AutoSet",,,looks like I just need to get an SD card. I will download Oscar today. I will post screenshot tomorrow. Any other settings important to go along with my next post/screenshot?
If you machine has not had a SD card in it, all the detailed data to date will be not recorded. After you put the SD card (normally a 4 GB, but up to 32 GB will work) in, it will start recording data for each night. When you have some data to display then post it here. With a PC you just need to get the Daily Report displayed, and then press F12 to save it as an image file. A note will come up briefly in the bottom right of the screen showing where the file is saved. Use File Explorer to find it and then left click and drag the image to an open post here. Use the orange Write a reply button at the bottom to get a full width window. I will post a sample of how I like to see the Daily Report page set up for the best use. Oscar will display your machine settings if you have the page set up.
Here is a sample of how I have my SleepyHead set up. OSCAR is very similar, and I have not bothered to upgrade to it yet.. This is an example of a night when I had a high number of leak events. I also use a fixed pressure with my AutoSet machine, so the pressure is constant all night.
Thanks for your detailed response! Leakage was due to loosening the straps, because my new (10 day old) AirTouch F20 causing nose redness. Tightened straps throughout night to overcome leakeage. **If you think, Would like to try adjust some settings (differential, etc) to see if that helps. Sleep Clinic I have been dealing with has left me in the dark as far as data.

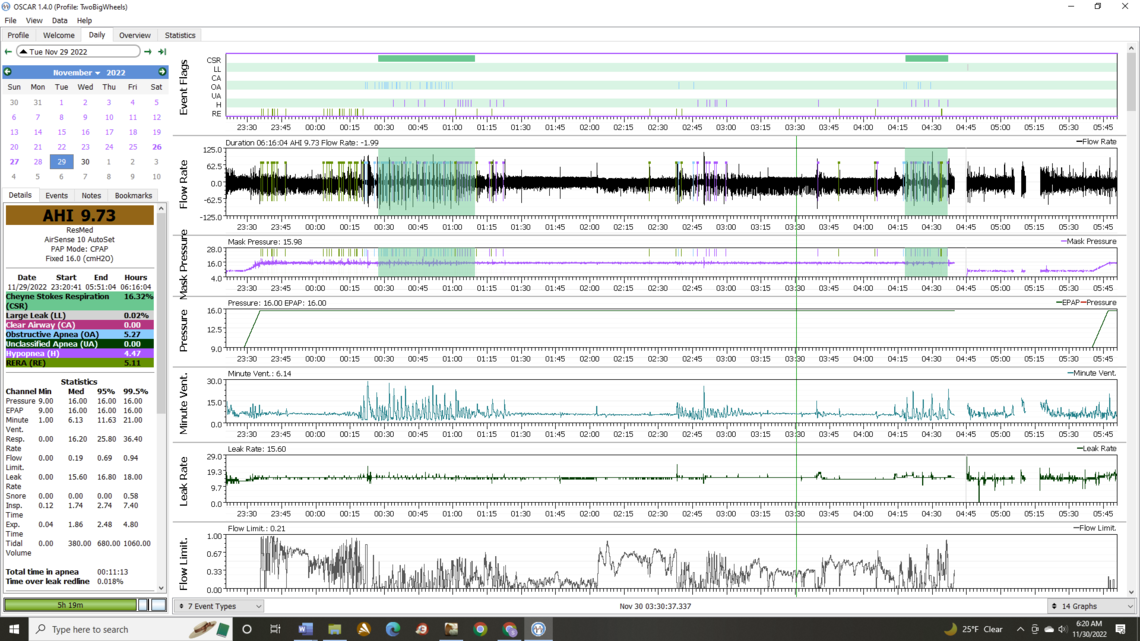
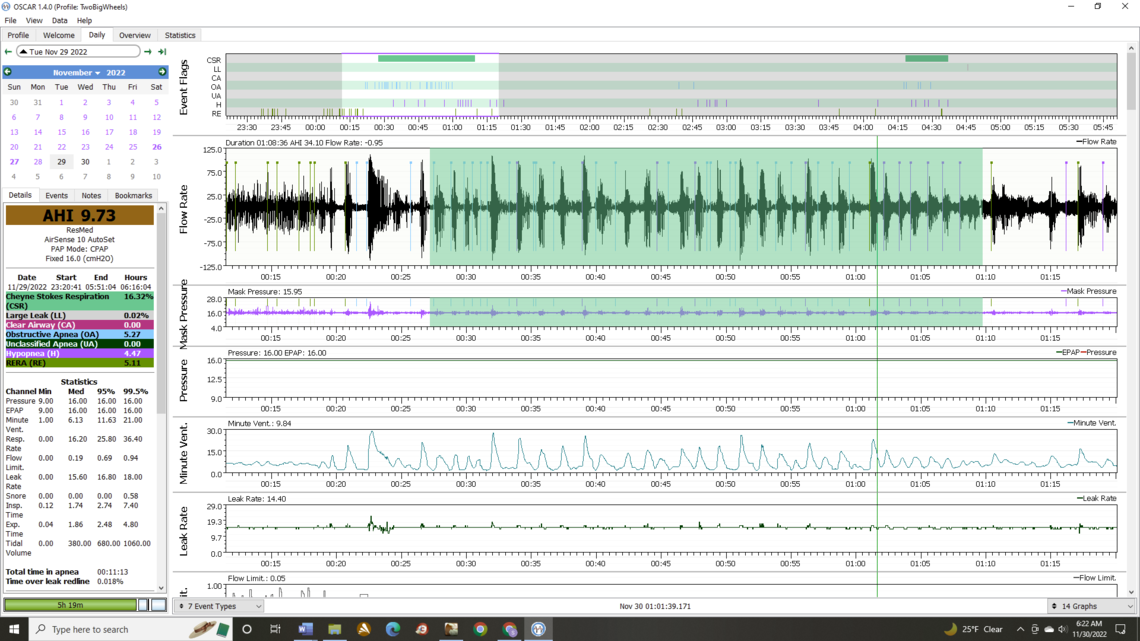
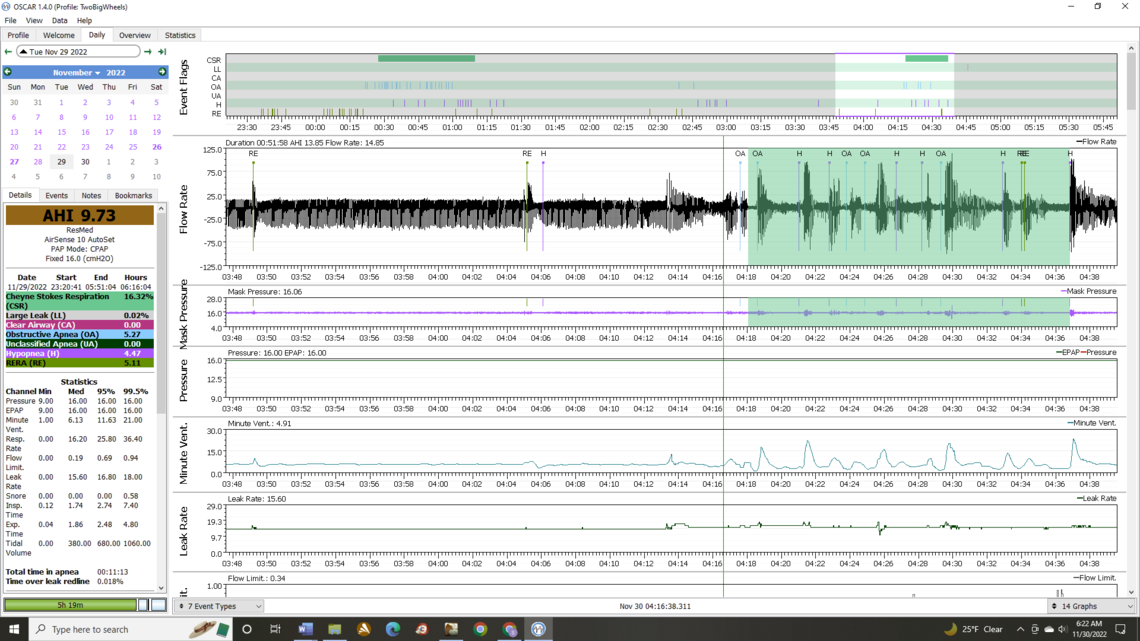
Those are very interesting results, and something I can't say I have seen before. I would be interested in seeing the CSR highlighted green area, but expanded out so the flow detail is shown. You can do this by left clicking on the area to zero in and expand it. The up down and left right arrows are also useful selecting the right area and zoom detail. Normally CSR is associated with central apnea events - CA's, not obstructive events like you have. I see you have no CA events reported. That is good because CA events are hard to deal with.
The other aspect is that you show quite high flow limitations and RERA. This would suggest you could benefit from turning on the EPR feature, setting it at 3 cm for level, and also for full time. If you try that post your outcome again after a night or two to see if there is some improvement. It may reduce your Hypopnea frequency and RERA. However, the 3 cm may not be enough to make a big improvement, and that is where a BiPAP with up to 10 cm pressure differential may be needed.
The other thought is that some people can have those high frequency OA events when they are kinking their neck while sleeping. Those that do sometimes report relief by using a soft cervical collar to sleep with to keep the neck straighter. They are quite inexpensive at places like Walmart. I have never needed or used one however, so I am just reporting on what others have said.
And as you may have figured out you should only post one image at a time so the post does not get hung up in the spam filter here. Once you have accumulated a few posts, then you may get away with more than one image.
Concerning collar, I sleep in a recliner if that makes a difference. I will pick one up and try. *Is the manual readily available online for making changes you mentioned? *I'll post last nights results when I get home.
Here is a link to a manual that will help you with the machine settings:
And here is a clinical guide to the ResMed BiPAP if you want to compare them. The BiPAP is more complicated to set up.
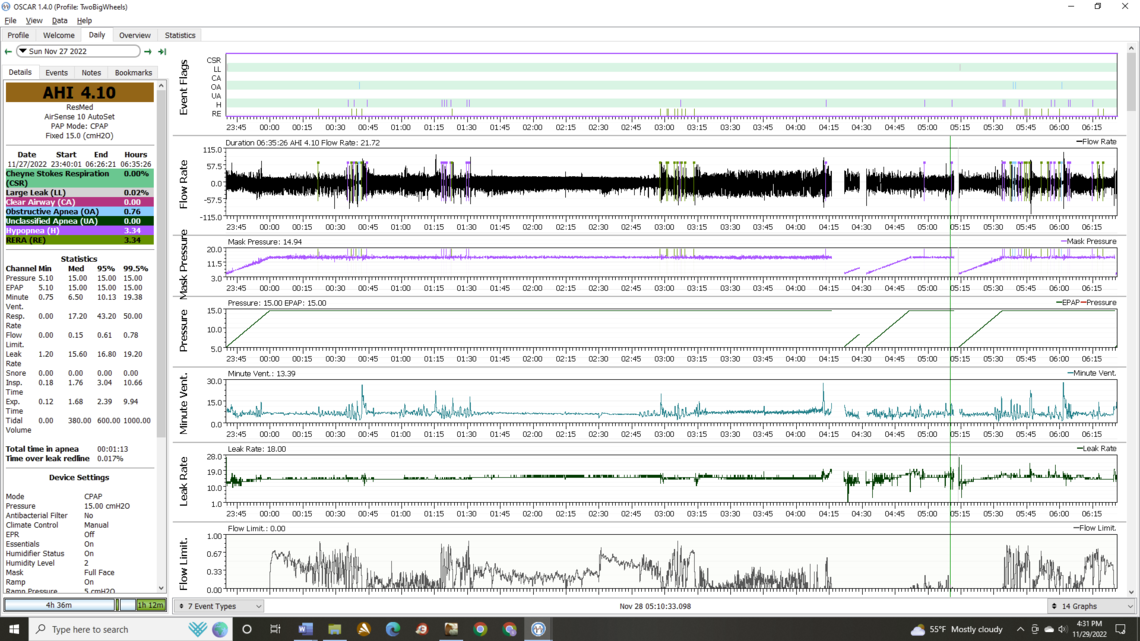
CSR Flow Rate expanded from 11/27. I'll post daily from 11/28 later this evening (There were No CSR events, but I woke up hard @ 3am and had hard time falling back asleep)
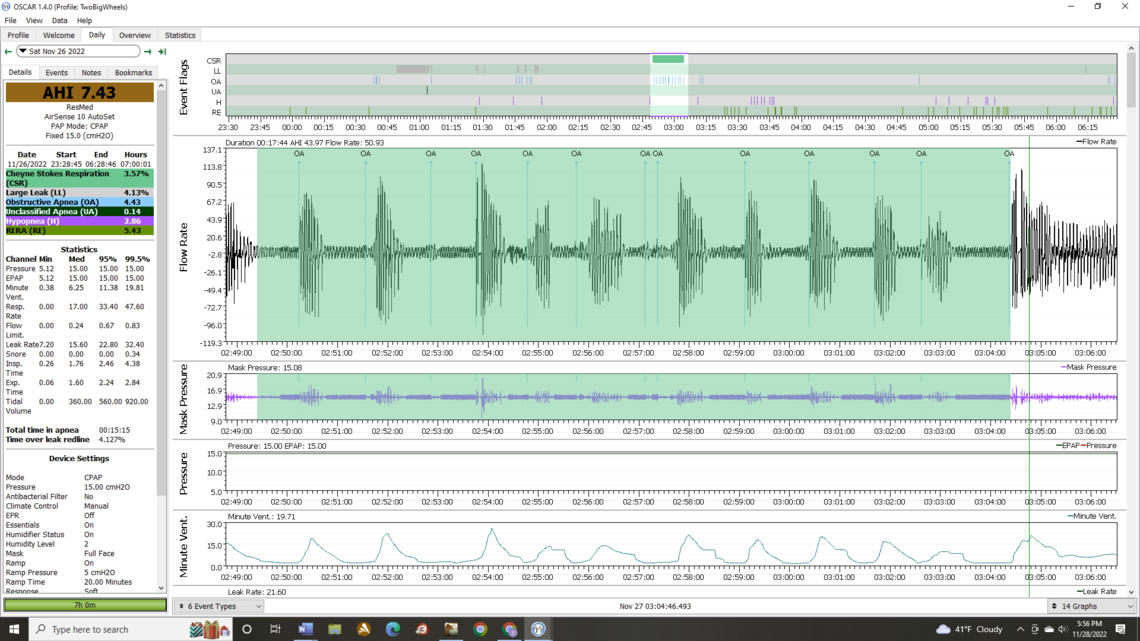
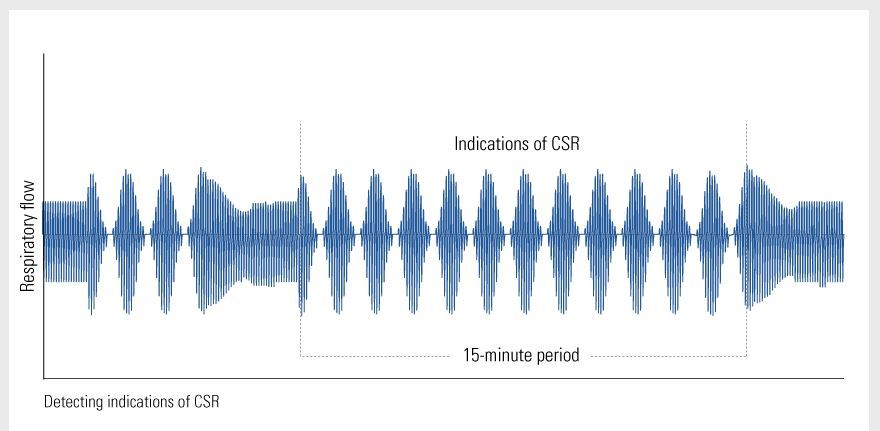
That is very unusual and does not look like typical Cheyne Stokes Respiration. Here is a theoretical representation of CSR.
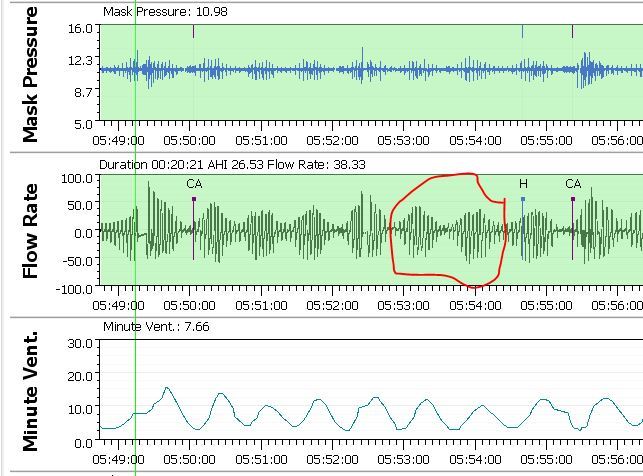
And here is an example from my records. I think it is much more typical CSR.
If you go for a sleep specialist consult I would bring a copy of that area and ask for comments about what the cause may be. You also should bring your SD card and ask them to take a look at the results. They should have a program called ResScan to look at the data.
For now I think the best thing you can do is turn on EPR full time at 3 cm level.
Thanks. Last night's data shows no CSR: I woke up 3am and had a hard time falling back asleep. Will try the EPR FT @ 3 cm
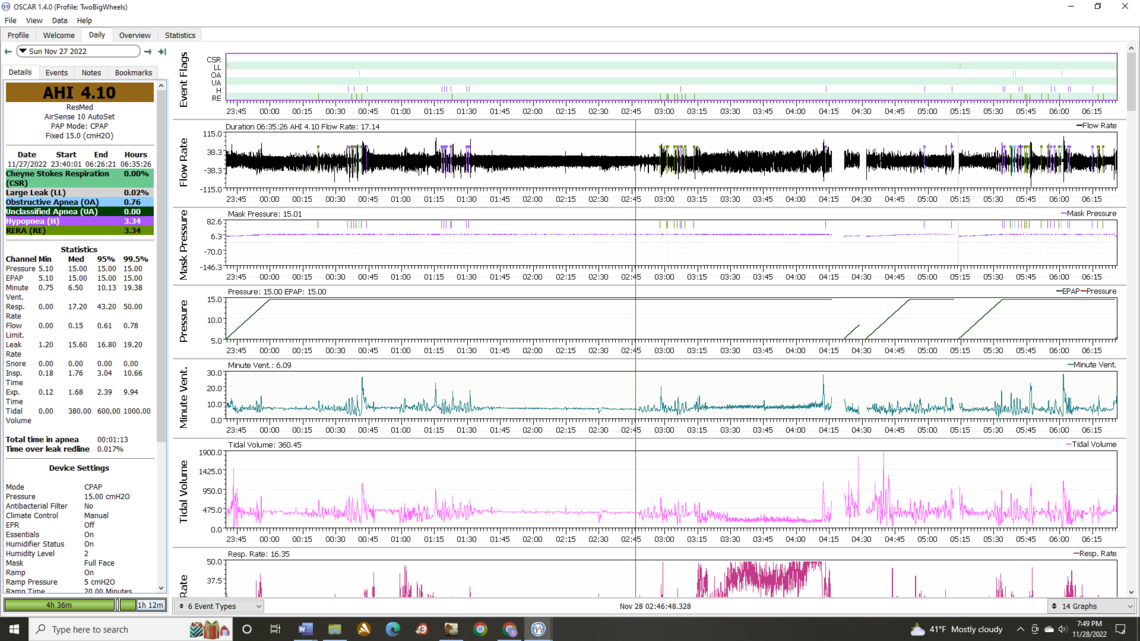
It is not going to help your event frequency, but one of the easy things to consider doing for comfort is setting your Ramp Time to Auto. And also your Ramp Start pressure to about 9 cm instead of 5 cm. When set this way it will start you out at 9 cm of pressure which should be more comfortable, and it will hold at that pressure until the machine decides you are asleep (up to a maximum hold of 30 minutes). Then it will ramp up to your set pressure of 15.
That respiratory rate seems a bit odd too. Your flow rate seems high, but perhaps you are taking quick short breaths. Expanding the scale out should provide more info. Compare it to when you are breathing at a more normal rate. Minute ventilation is low and fairly constant as well as Tidal Volume. Seems like you are breathing fast but not accomplishing much air transfer. Again you should ask the sleep specialist about this as well.
EPR ON Level 3 Full Time Ramp Time Auto Changed Ramp Start to 9 from 5
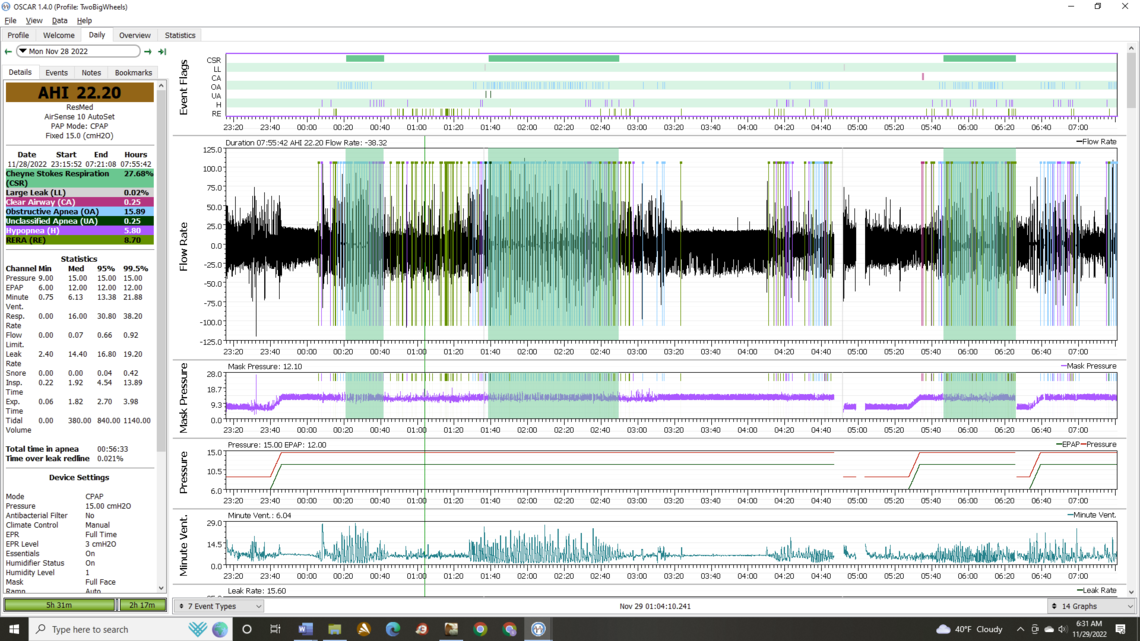
OK! I was not expecting that. Can you squeeze down the Flow Rate graph height and show the Flow Limitation to see if that changed? Have you tried the soft cervical collar yet?
Have you always been on a fixed pressure? If not then did the Auto mode not work for you? And, how about at a higher pressure. Is 15 cm the most you have used?
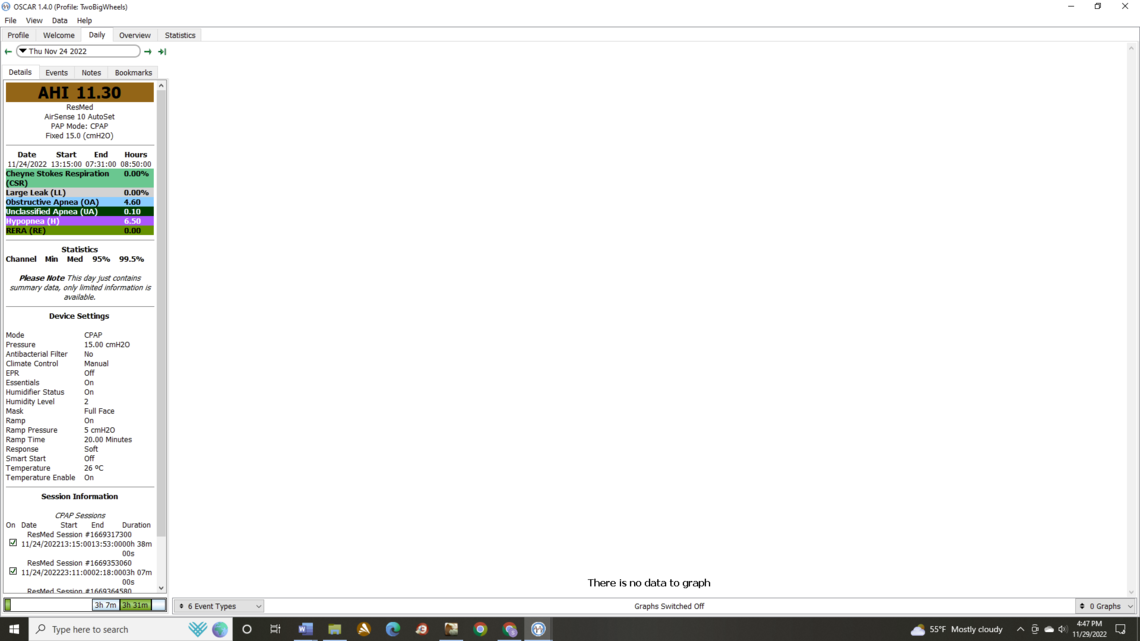
Will send flow info later. *I "think" i was on a auto before, but I never seen my data before to know what it was or compare. I'd have to go day by day on Oscar, looked like it showed settings & data on LS, but no graphs. *Cervical Collar not available locally, should be at my door Wed. *It was mentioned in last phone consult with PA that Dr thought I needed higher pressure since at last study I kept waking up (I thought I slept, they said I didn't or rarely entered REM). *The more I'm learning, the more I'm disappointed with my Sleep Center. No Cpap OP Manual, No SD card, not being told about even basic Resmed MyAir data,,,*If Bipap was to be considered, why not do a test run @ EPR 3 before getting sold a study,,,last conversation a week ago with PA was that we were making a change from Fixed 14 to Fixed 15,,,knowing what I know now, doesn't make sense... *I'll check my Oscar for max psi & Auto Settings if accessible
I've only had Oscar for a few days now. Maybe chart since 1st of year will help looking at pressures vs AHI's. Except for the last couple of days or so, Oscar only shows details on left side of page (as attached sample). If interested in any days in particular, let me know, I could try to tie in with Dr visit (5/3/22, etc)
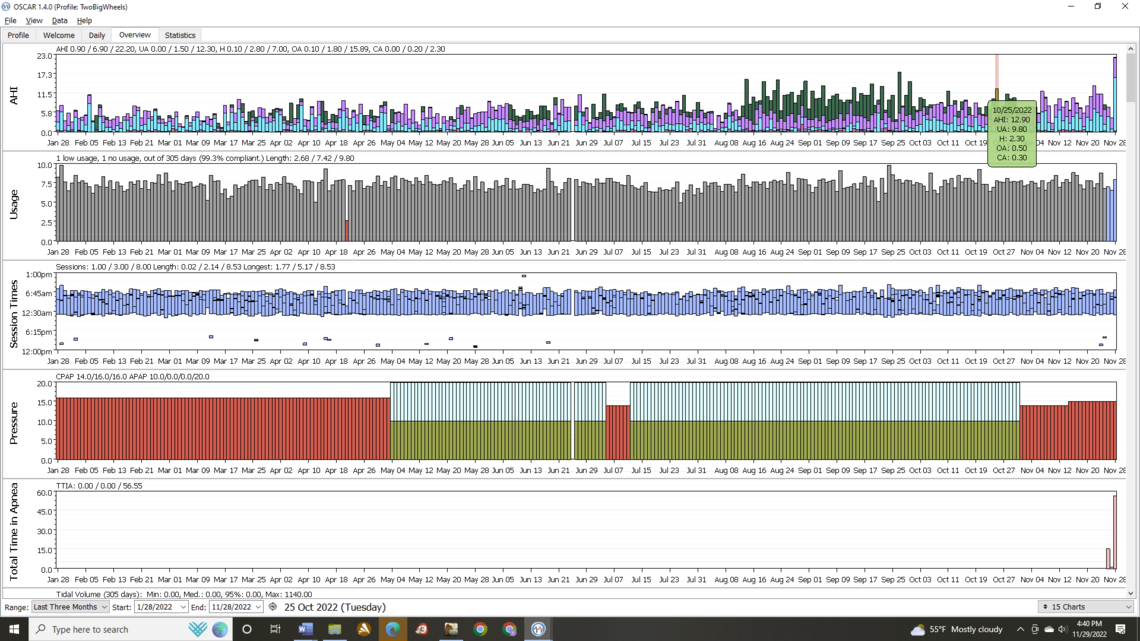
Glancing at Annual AHI's, it looks like i was doing better @ 16psi at beginning of year, not sure about mask seal, etc though. BTW: I seen that u mentioned on a post that your wife does Yoga breathing @ times. I'll do the same as i settle down w/CPAP started and also some breaths if I need to after waking up @ night (w/Cpap started). 5-7s in thru nose, hold for 5, 5-7s out thru mouth.
Any recommendations for tonight would be appreciated
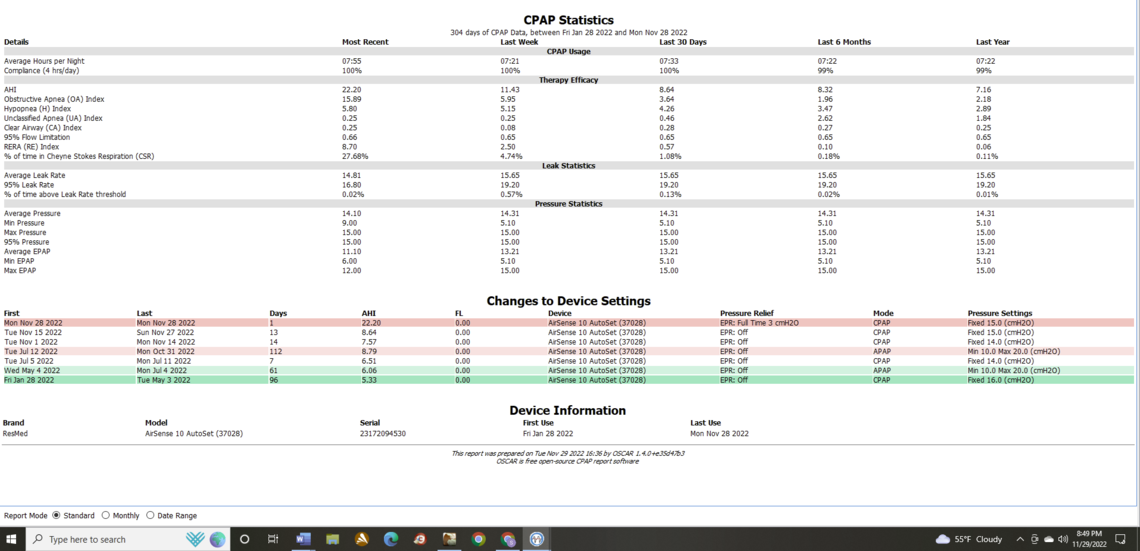
Yes, I see what you were talking about with getting the best results with a higher pressure of 16. And I see you have tried APAP mode a couple of times with not great results. For now I think I would try the EPR at 3 cm for another night. One of the issues with adjusting a CPAP it takes some time to see what the result really is. Perhaps the first night with EPR was an outlier.
But, if that does not work, then I would suggest increasing the pressure to 16 cm like you had before and give that a try. The other option would be to put it back into auto with a range of say 13 minimum to 18 max. The advantage of doing the Auto range now that you have OSCAR is that you can see the impact of pressure changes each night. That may help identify the best pressure to use, and then you could switch back to that as a fixed pressure.
I will give you some more detailed thoughts tomorrow. I have probably missed your bedtime for tonight anyway.
Missed your reply last night. Set @ fixed 16 last night. *Clicking thru daily history (only showing Summary data, No Data Charts), I can find no Daily Summary with the suspect CSR's. I changed mask to AirTouch F20 on 11/15. **I have weaned myself off of a Time Release Melatonin (3mg then 1.5 now 0). I was taking TRM to help with 3am wakeups and to help myself to try to fall back asleep. Weaned off after PA was questioning me taking it... **I'm not opposed to staying with a setting for X amount of time...I have a Sleep Study scheduled for 12/21. Hoping to make progress by then and hopefully just cancel it. **I actually felt pretty good thru the day after using EPR 3 even though the data said otherwise...
To speed things up so you can get as much information before your appointment on Dec 21, I would suggest going back to the APAP Auto mode. With a minimum pressure of 15 cm and maximum of 20. This is a higher minimum than you were using before and may give better results. When you have a low minimum you can get a lot of events happening before the machine decides to raise the pressure. With Oscar you will be able to see the impact of higher pressures, and determine what you may need.
One issue with EPR is that it lowers your pressure on exhale, and if you are susceptible to having obstructive apnea events on the exhale part off the breathing cycle, it can increase them. I went with EPR on the Ramp Only (which is an option) for a long time and was averaging about 2.8 for AHI. When I went to full time it dropped to my current average AHI which is 0.8. The big change was a reduction in apneas. It seems that adding EPR for me did not increase OA events, but everyone is different. I think for now it is probably best to focus on pressure as a solution and then come back to using EPR as a test when pressure is optimized. There is some logic to using the Auto mode to determine the best pressure and then go back to fixed CPAP mode once you settle on a pressure. That is basically what I did.
In your post you make reference to a "PA". Is that a doctor, and if so what specialty?
Ok will go to Auto 15-20. PA I was referring to is a Nurse Practitioner. Only talked to her on phone & couple of Telemed conversations. *The Dr is Internal Medicine w/subspecialty of Sleep Medicine. *They are part of a well marketed Sleep Center in Chicago area. *I'm disappointed with how I've never seen any of my data, like it was Top Secret. *Is it normal to not share hard data or does it depend on Dr/practice? *1 of the last things the PA mentioned was that if they couldn't find out why i was waking up at night, they wanted me to see their Sleep Phsycologist/Therapist,,,knowing what I know now, it sure looks like apnea events are waking me up... *With that being said, I'm going to look at another clinic. *Any idea (besides Dr sharing data) what Main Practice is best? Neuro? Pulmonologist? My sinuses were never 100% & have no sense of smell Post Surgery.