I had a closer look at your OSCAR data and have done a little bit more google research. The first thing I need to say is that I am a retired mechanical engineer and not any kind of medical professional. I draw my experience from reviewing my and my wife's data, and many others from this forum and others. With that context these are my thoughts, in no particular order.
That period of time where you had the very high respiratory rate is likely called Tachypnea or Nocturnal Tachypnea if you were asleep when it happened. It seems to be fairly rare but has been seen in people being treated with a CPAP. Possibly it happens in others, but without a CPAP or titration test equipment, it is never recorded. You can google it, but I am not sure in your case that it has an obvious cause. If you were awake, it could be simple anxiety, and I am not sure one can get anxious when asleep. If it is anxiety there are a number of drugs that can be used, but one should question if they should be used. I have taken an Ativan single pill before cataract surgery to deal with anxiety, but I think using it on an ongoing basis can be addictive. You mentioned Ambien, and that would likely be less addictive, but may have other side effects. I take a beta blocker, bisoprolol, for blood pressure control, but I understand it can be used, off label, to control anxiety as well. If you feel it is anxiety these are things to discuss with your doctor.
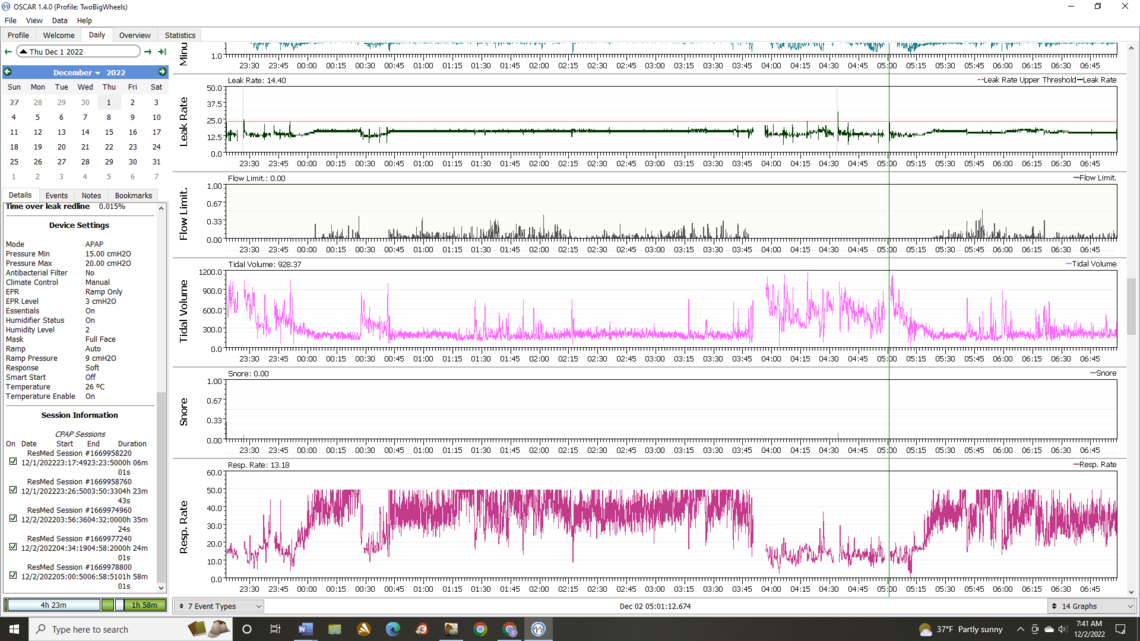
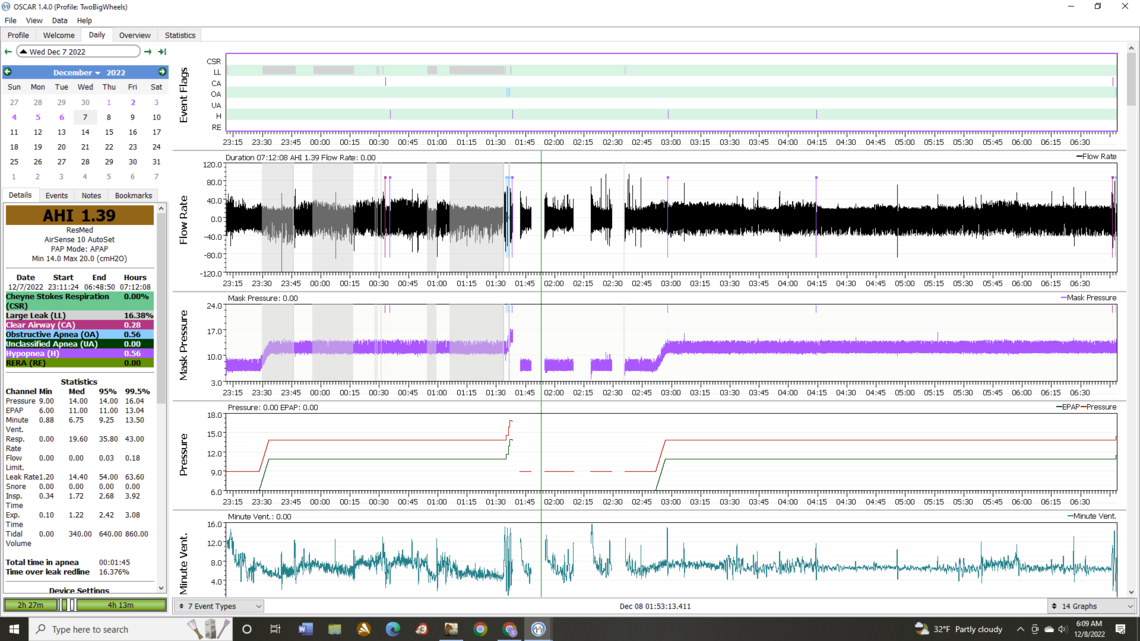
The areas flagged by your CPAP as CSR or Cheyne-Stokes Respiration, are more of a concern. I suspect those are quite disruptive to your sleep, and they may be resulting in low blood oxygen levels. You could consider getting an oximeter that clamps on your finger and gives a record of O2 levels during the night. SleepyHead and I believe OSCAR can accept the data from some of these meters so you can correlate events like the CSR flagged times to O2 levels. I believe OSCAR should give you some information on which meters it can accept data from.
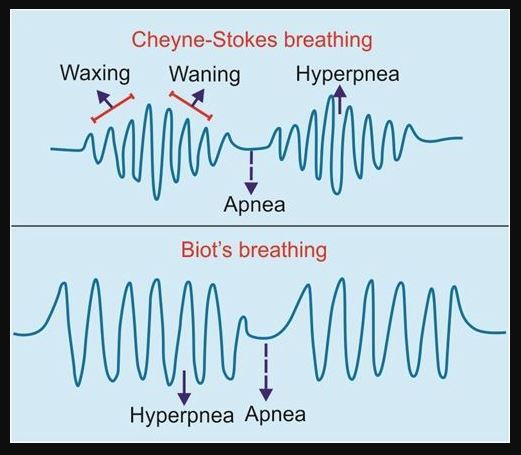
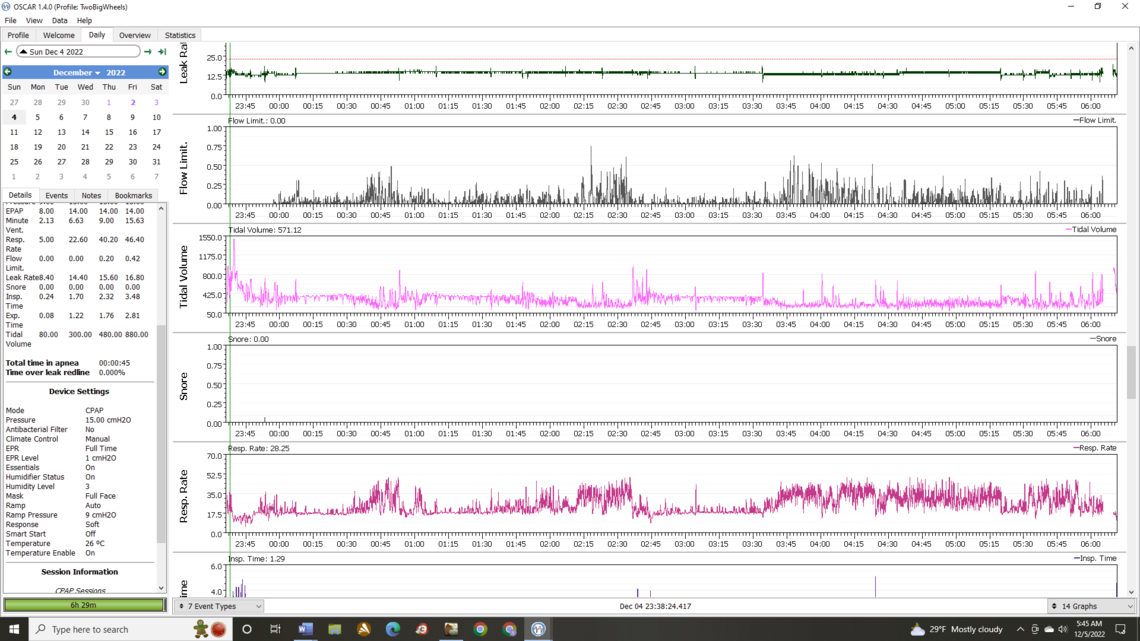
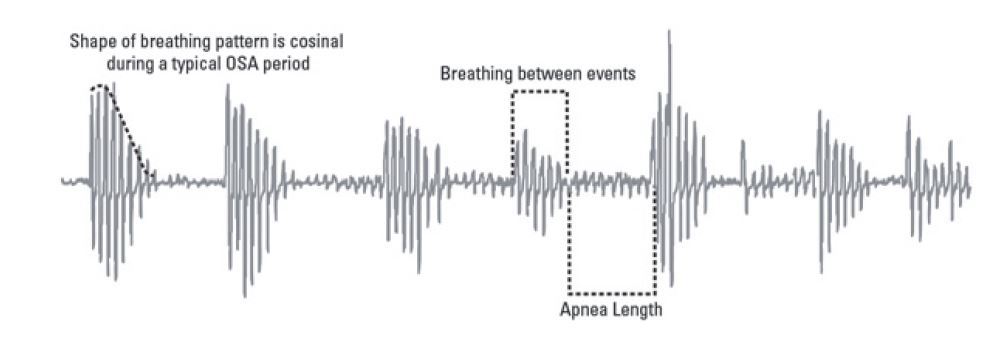
With respect to it actually being true Cheyne-Stokes Respiration I am not so sure. Have a look at this simplified illustration comparing CSR to another condition called Biot's. True CSR has a smooth waxing and waning pattern, while Biot's does not. I do not see that in your example. It is more of a sudden increase and then some waning back to nothing.
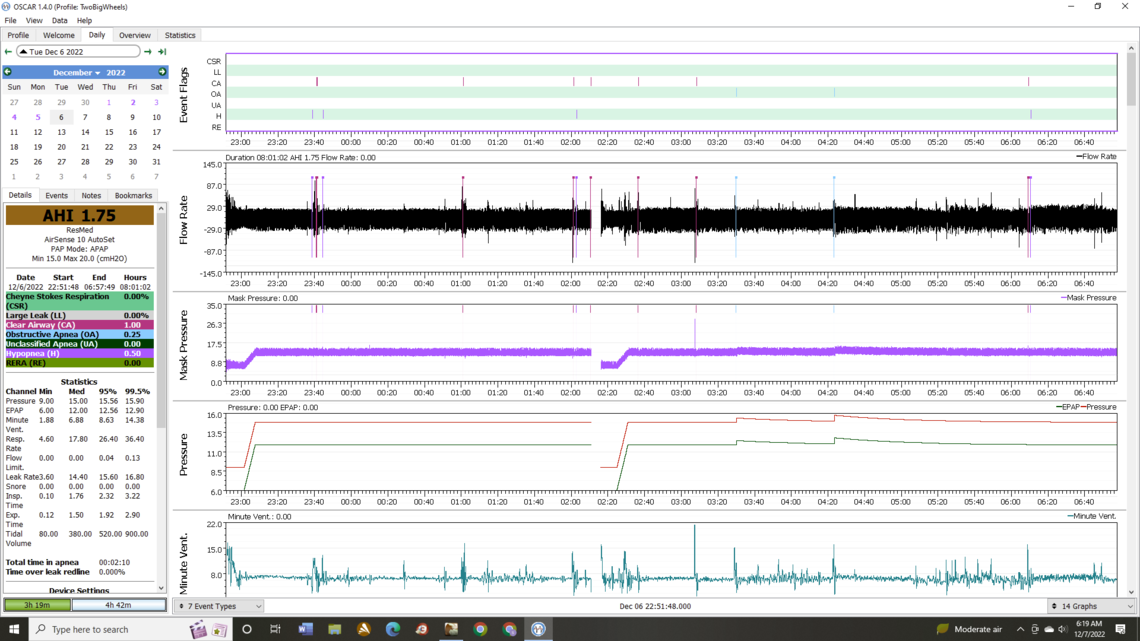
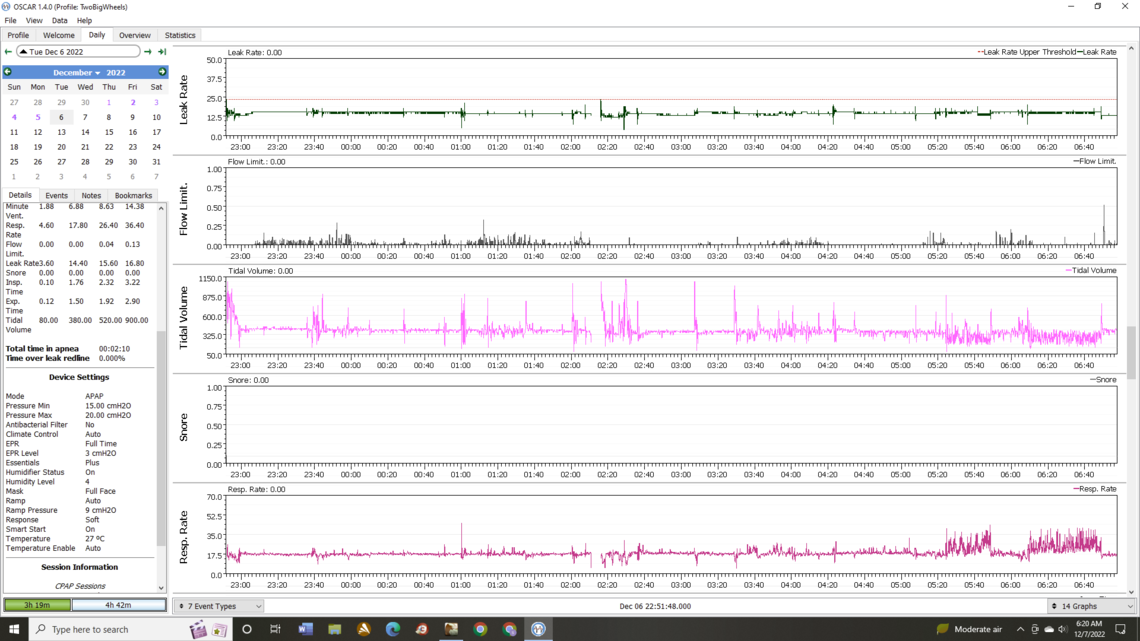
Here is an example of what I think is true CSR from my personal data back in 2018 when I was having issues with it and central apnea.
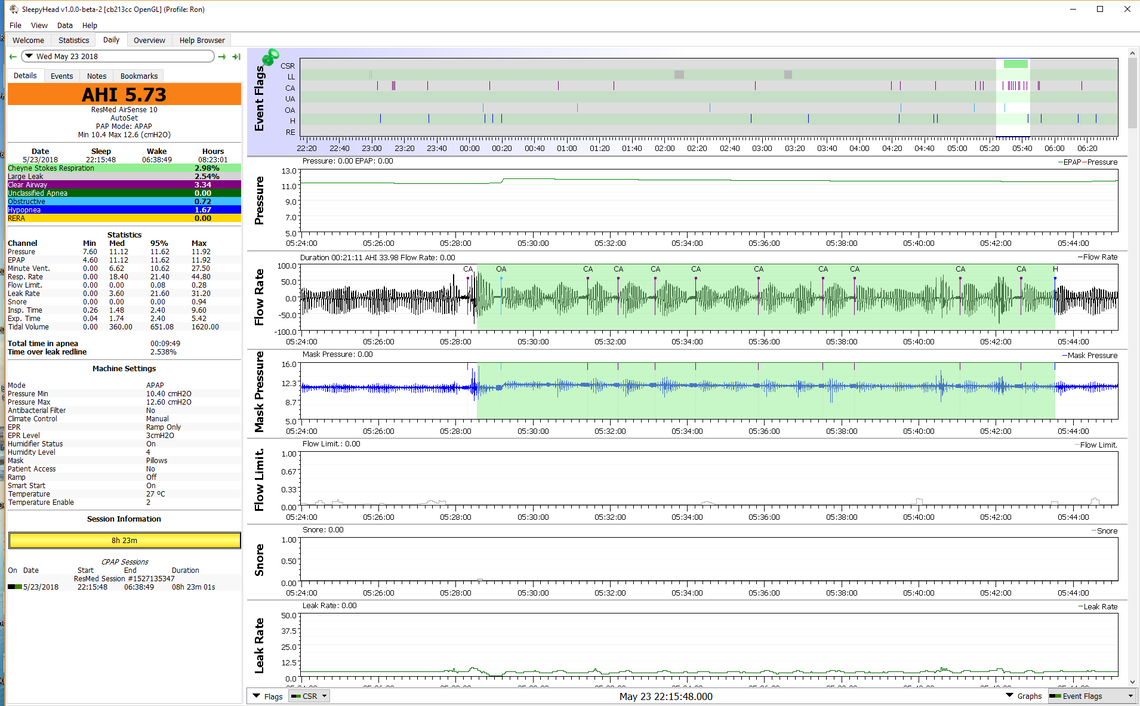
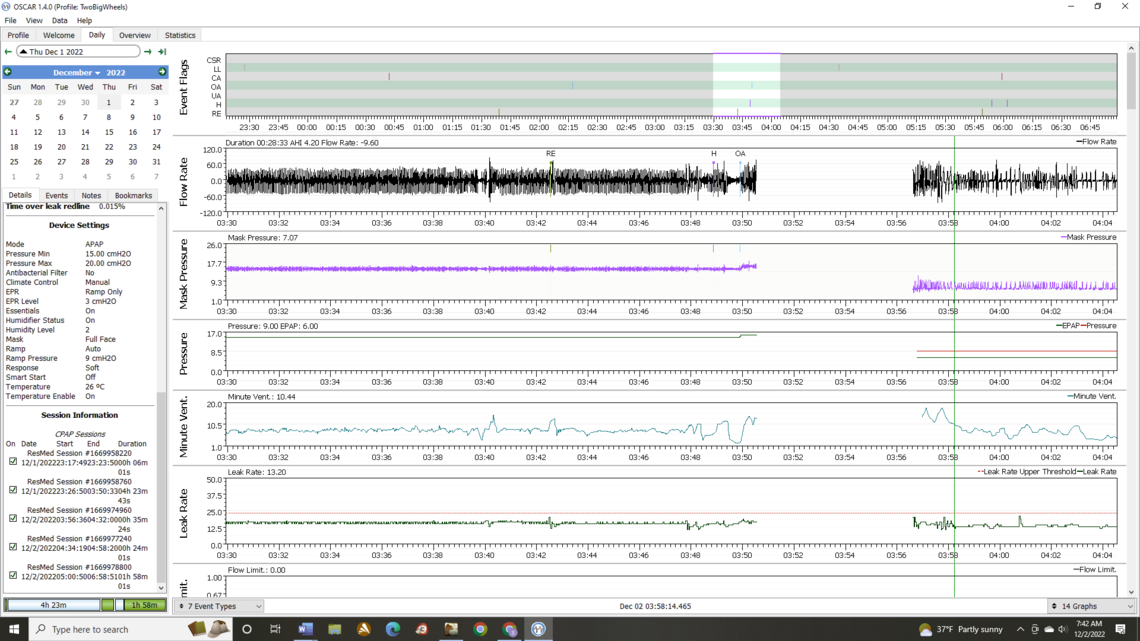
Notice the smooth waxing and waning which starts even before the CSR green areas. The other big difference is that you are having obstructive apnea events between each while I am having central apnea events, which is no obstruction, just me not wanting to breath. I don't know much about Biot's other than it is rare, and your pattern does not fit it exactly either. Not sure if it is associated with OA or CA events. I think there is a good possibility that what you have is simply obstructive events with gasping periods for air between each one, and not Biot's either. That would be very disturbing to your sleep.
So this all said, I think for the short term, I would focus on more pressure in auto mode to see if the obstructive events can be prevented with more pressure. If my theory about you gasping for air between each obstruction should stop too, if the obstruction is prevented.
The part about doctors is complicated. I am in Canada and I am sure the overall system is different here. I have just gone to a sleep clinic where they give you a home test kit to take home. They send the results out to some cyber doctor somewhere that is supposed to be qualified to read them. Then they want you to buy a machine for $2400. Since I have no insurance for CPAP, I just bought my machine on line for about $800 and have done everything myself since then.
If you are in a situation where your insurance will cover it, I would try to find a pulmonologist that has sleep apnea experience and show them the results you are getting. If increased pressure does not solve things you need to get to the bottom of what is happening. At some point you may need to get a cardiologist involved too.
But for now give the 15/20 auto pressure setting a try. If it helps but still jams out at 20 cm, then you probably will have to pursue the BiPAP alternative with the hope a bit more than 20 will help. They go up to 25 cm. The extra pressure support from the BiPAP is not looking promising as you did not get a significant improvement with the EPR at 3 cm.
Your test in Auto at 15 min and 20 max should be very informative as to what possibilities there are. The cervical collar is still worth trying too. It may provide relief from the rapid sequencing of obstructive events.
Thanks again for your help! Not doing Happy Dance yet, but looks like something to cervical collar. Was settled in last night, then remembered collar (CC) came from Amazon... At my wake up,,,I had a Large Leak (along with an event) that I was aware of as I woke up (leak, not event). Not sure why leak, i think leak by end of Nose Gel Strip at cheek end. *Pre Wake Up i was in recliner, after putting CC on noted that headrest on recliner canted my head forward. CC fought this and kept my mouth shut (I think). *After wake up, i did take a Sleep Aid supplement with 2.5mg of Melatonin. *After wake up, Laid down flat on couch "on my side",,,met friend over weekend who told me they only had Apnea on their back, No Apnea on their side, figured give it a try.
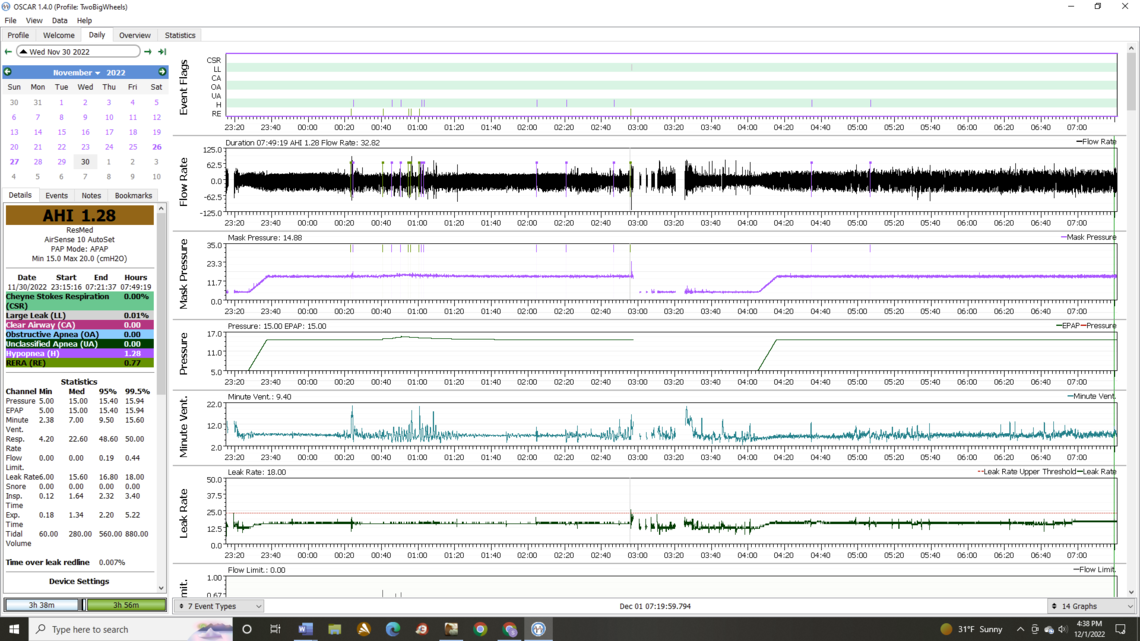
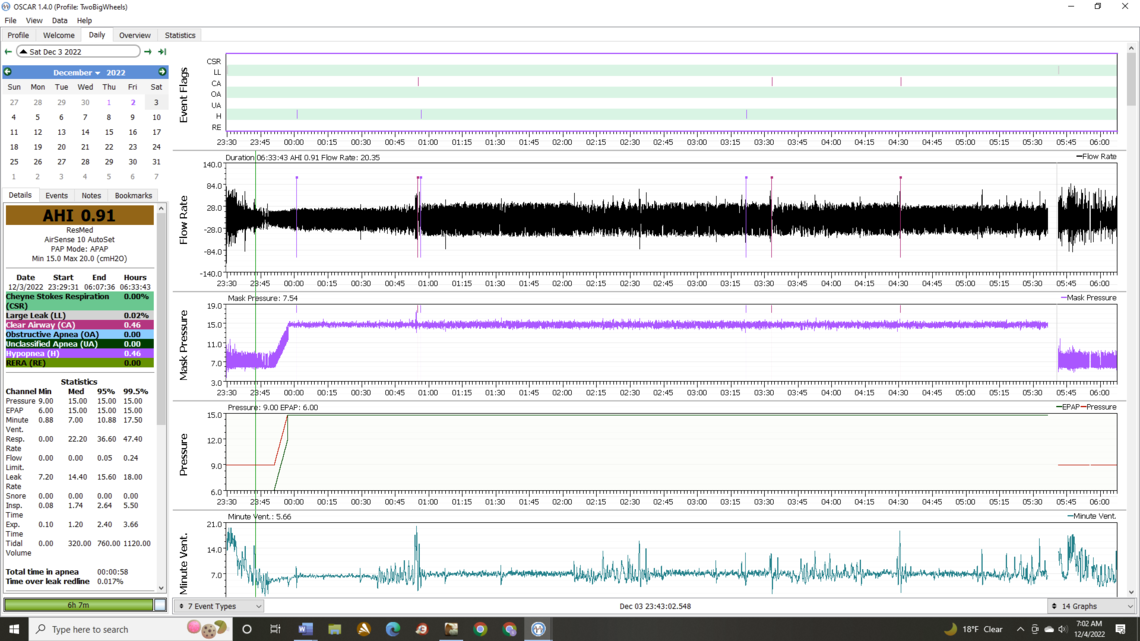
Well, that is looking more encouraging! I see your pressure increased slightly and seems to be mainly driven by Flow Limitations. The rapid frequency of OA events is gone, and that is good news, but one night does not prove much yet. The collar may be helping. More nights and time will tell. Yes, most people are more prone to obstructive events when sleeping on their back. I do not try to avoid sleeping on my back, but I have back issues and my back certainly encourages me to sleep on my side more. Some people go to the extreme of sewing a tennis ball into the middle of the back of their PJ's. It sounds cruel to me, but that probably would encourage sleeping on a side rather than their back! I recall from my sleep study that the apnea frequency was slightly higher when sleeping in the back position.
I noticed that your start pressure on the ramp has gone back to 5 cm. If you find that more comfortable that is fine, but most, and especially when there is flow limitation issues, find a higher pressure like 7 to 9 cm can make breathing easier. What I do is take really quick deep breaths and see if I can feel any flow restriction. I increase the start pressure until I can't feel any restriction at all to the quick deep breaths. In my case I found 9 cm to be just right. I don't like that feeling that the machine or mask is restricting the flow of air into my lungs. Kind of gives me a suffocating feeling. The other thing you can do for comfort is set the EPR to 3 cm, but also set it to Ramp Only. Then you will get the help exhaling with the EPR exhale pressure reduction up until the time you go to sleep. Then it will turn off.
Your main AHI score for this night is coming from hypopnea. EPR full time may help that, but I would not try that until you have established a baseline with the machine in Auto, and with the cervical collar.
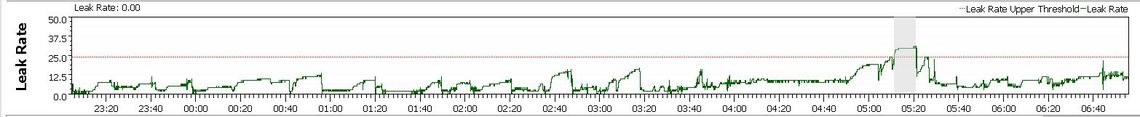
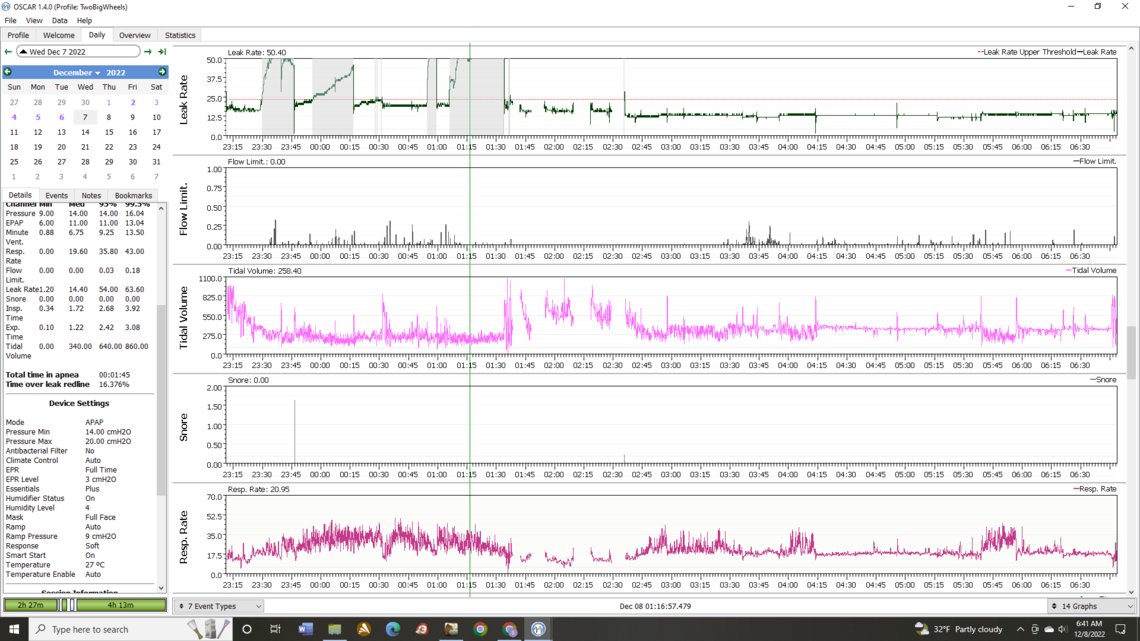
On the Leak Rate graph I find it helpful to set the leak rate red line. To do that you mouse over the Y-Axis scale and right click to bring p the options, and then click on Dotted Lines. Then check off the Leak Rate Upper Threshold box. That will display the red line on the graph. I don't worry much about the leak rate as long as it is under that line. Under these options I also set the Y Axis to Override with a min of 0 and max of 50. This keeps the relative proportions the same from day to day. Auto Scaling can make things look worse than they really are.
Not sure why start up pressure changed...I was in a hurry last night making 15/20 Auto changes. I'll Double Check tonight and apply your start up recommendation. *Implemented Leak Rate Graph recommendation you made (shown below). *Keep pressure at 15/20 Auto? *What if 15 on low end is to high?
The leak rate chart looks good now. On the start pressure, it may be possible that the 5 cm setting was linked to the Auto PAP mode, and it went back to 5cm when you switched to Auto.
I don't think the 15 cm minimum is too high at least for now. In fixed pressure mode you were using 15, and not getting great outcomes. However, if you can get good AHI numbers with it set at 15 and it never goes up much in Auto, then you could consider lowering it. The advantage of a higher minimum pressure is that it stops events from happening, instead of having events trigger an increase in pressure. When you were running Auto earlier the minimum was 10 cm, and that may have been a reason for Auto not working so well.
One good thing about your readings is that central events don't seem to be an issue. They can make things difficult as more pressure can cause CA events to increase. So you can get into a situation called Complex Apnea where more pressure is needed to stop obstructive events, but at the same time more pressure increases the CA events. In that situation one has to thread the needle and try to find a pressure high enough to stop OAs but not cause excessive CA events. With that issue using fixed pressure CPAP mode can be the best way out. But, you are lucky to not have that issue. The pressure is more of a comfort/leaks thing for you. But, I would leave that for fine tuning a bit later.
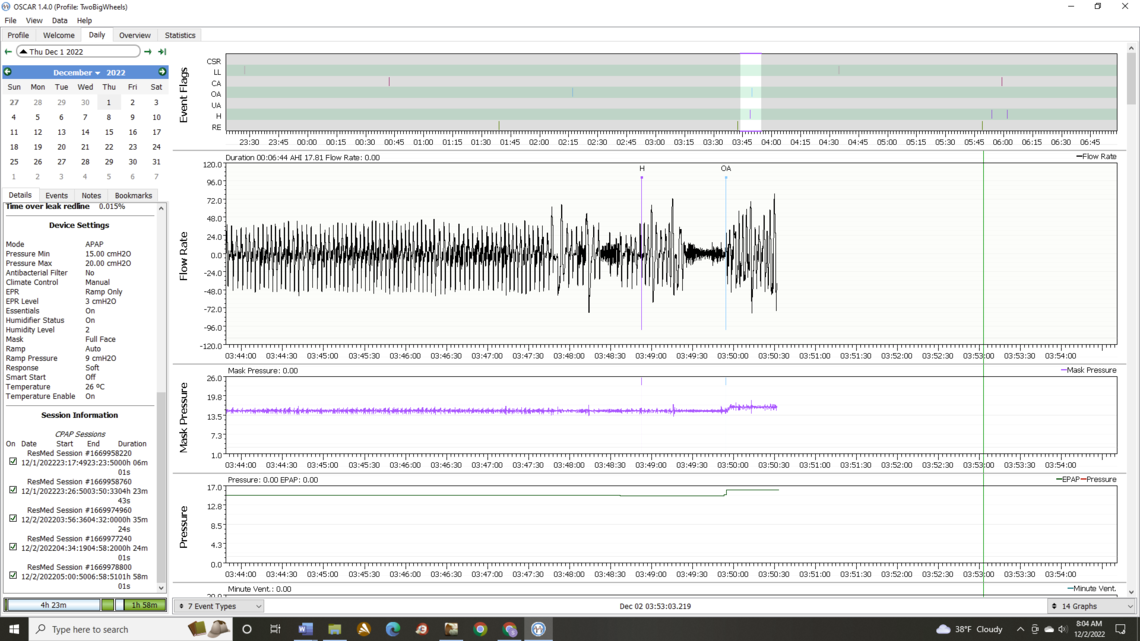
I had a hard time falling asleep last night (I usually don't), I took a nap in the afternoon which I probably didn't need after getting low AHI's. the night before. Layed on one side or the other the whole night w/collar. *I zoomed in on event that woke me at 03:50 Any idea why my Resp Rate is "clipped" at the top? I changed Y to 60, I think it was at 50. *The time is off by an hour, do you know how to correct it?
On falling asleep one of the very minor things I do is set my machine to warm up. I then starts heating up the humidifier reservoir. It is a menu item on the User menu. I also try to avoid napping during the day to build up sleep demand, and also try to avoid averaging more than 7-8 hours a night sleep, with 7.5 being about ideal for me.
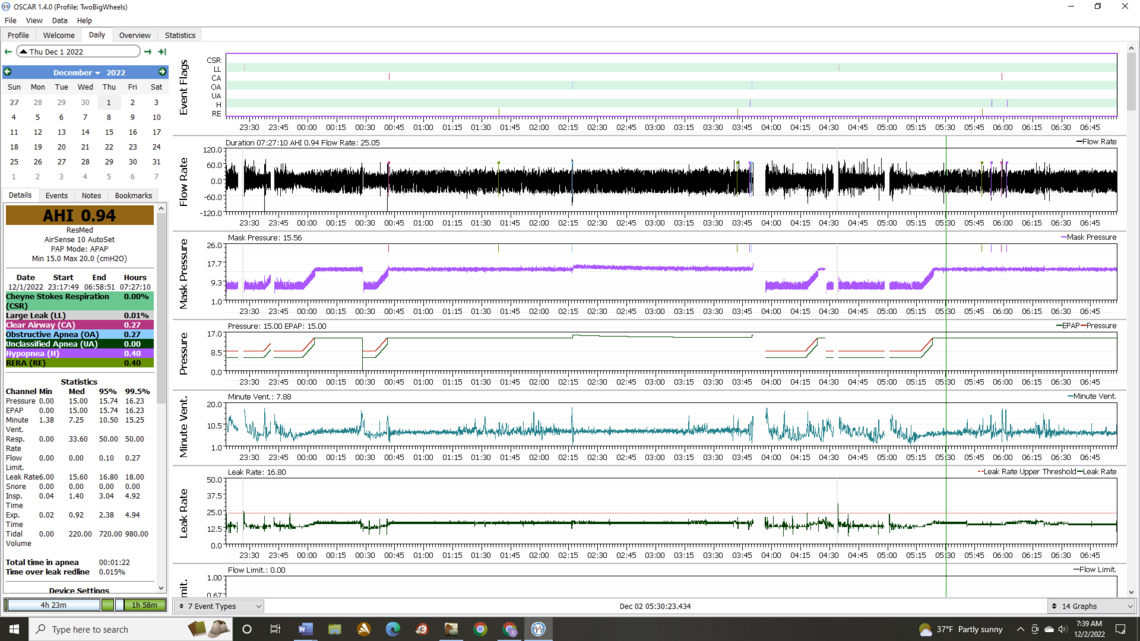
On the event that woke you up, it looks like a standard obstructive apnea and was preceded by a hypopnea event. Your Flow Limitation was not all that high at the time. Your machine responded with an increase in pressure, but of course by the time the event happens it is too late to prevent it. That is a good illustration of why a higher minimum pressure is helpful. Perhaps if you minimum was set at 16 cm, the event would have been avoided. But it is a little early for that conclusion yet.
Not sure what is happening with the respiratory rate being clipped. Perhaps the A10 does not report anything higher than 50, or OSCAR has a bug in reporting it. The real concern is that you are having the Tachypnea type breathing which is rapid and shallow. Notice that your tidal volume goes down when the breathing rate goes up. Definitely something to discuss with your doctor. The good news is that it is about the only abnormality left on your sleep report. It may be possible that use of EPR full time could reduce this type of breathing, but it is a bit early to try that. If things settle out with these low AHI numbers, you may want to try EPR at 1 cm to see if that helps, and then 2 cm. I only use 2 cm, but it seems to help me a lot in reducing hypopnea.
If these low AHI numbers hold up with more nights like this, it would appear there is no justification for a BiPAP machine. If you add back the EPR, pressure may need to be increased some, but probably not as high as 20.
The time thing I believe is a design problem with the ResMed AirSense machines. I have found you can advance the time, but you can't set it back. Right now I am running 1 hour ahead, because I can't set it back. I have researched it a few times, and if you find a solution let me know. But, I think the only way may be to do a full factory reset, which means you lose all your data stored in the machine, and you have to do a full set up of all your pressure settings etc... While you will not lose your data that is stored in OSCAR you will lose whatever is in the machine memory. I have never thought it was worth it, so I live with the time error. ResMed have released an AirSense 11 machine, and I would hope they would have fixed this time issue. There should be an easy way to switch between daylight savings and standard time, or even do it automatically. They are way behind the time on this issue!
Keep all settings the same tonight. Right?
Changing Resp Rate Y to 70 (see if graph looks different)
Concerning Warm Up, do you start it X amount of minutes before you lay down?
***Any thoughts on Time Release Melatonin? I weaned myself off the last couple of weeks. I "usually" woke up, but fell asleep a "lot" easier, none of this being up for an hour+ stuff
Yes, I would keep settings the same for a few days if you keep getting good results. I think the next step may be to try adding some EPR starting at 1 cm and possibly working up. But, it would be best to determine if your AHI results are stable first.
The warmup is fully automatic. You just turn it on. The screen will flash a message saying it is warmed up, and I think it takes about 15 minutes. Once it reaches the warm up target it will hold it there for some time - I think perhaps 30 minutes. I don't worry about that much, and just turn it on when I go up to the bedroom (if I remember) and what I get is what I get. Most nights it is around 10-15 minutes.
My wife used to take melatonin but I am not sure she does any longer. I don't think it does any harm, but I am also not sure how effective it is. My strategy for sleeping is basically to try to avoid naps during the day, and not try to oversleep. As I mentioned before my target is about 7.5 hours per night. I think one source of credible sleep information is this link below. It was started by a pharmacist and university professor that was concerned about seniors using sleeping pills and falling, with a high incidence of broken hips etc. There are some pretty good resources at the site with some tips on sleep hygiene and use of CBTi.
It is not a big deal, but one of the things I have noticed in your leak rate graph is that it seems to never go down to zero, but instead never goes below about 12 or so. I can think of a couple of reasons for this.
One is that the mask type is set wrong in your machine. Your first post indicated you were using an AirTouch F20 full face mask. OSCAR is reporting that you have the machine set to Full Face which is correct. However, I have found that SleepyHead and possibly OSCAR do not always report the equipment status correctly. So you may want to check in your Clinical Menu that the mask type is really set to Full Face. If it is set to a nasal pillow type mask this could be a source of leak rate error. The reason for making this setting is that the mask type determines how much of a purge leakage there will normally be for the mask. The purge flow on a full face is higher than for a nasal pillow because of the difference in volume of the mask.
If this is not the problem then about the only other alternative is that you have a fairly significant fixed amount of leakage. If you can find it, then that would be good. But, as long as your leakage stays under the redline, it should not impact the machine's ability to control apnea. It may be a source of irritation though, that may make sleeping more difficult.
Concerning leakage: I can find no obvious leak with ear or feel test. I am a mechanic, and used to listening and feeling for air leaks. I tried a Dead Head test (thumb over end of hose) but OSCAR didn't register anything. Could try old mask when I have a chance (Vitera gel). Vitera has a dozen or so holes in front with obvious flow coming out. I don't feel anything coming out near swivel with AirTouch F20 on.
Friday night forgot to put SD in: In recliner w/collar and took TR Melatonin and 25mg Benadryl to relieve sinus pressure. Yes, I have taken Benadryl in past to help with sleep. Slept thru night.
Sat Night laid on one side or the other w/collar and took TR Melatonin and 25mg Benadryl to relieve sinus pressure . Woke up and ended taking mask off and falling back asleep for an hour or so in recliner (no data). *Resp Rate: after scrolling over, never went over 50. Last OSCAR graph for Thurs Night, gave it the illusion that it was "clipped" @ 50. *My CA's were 15, 25 & 18s
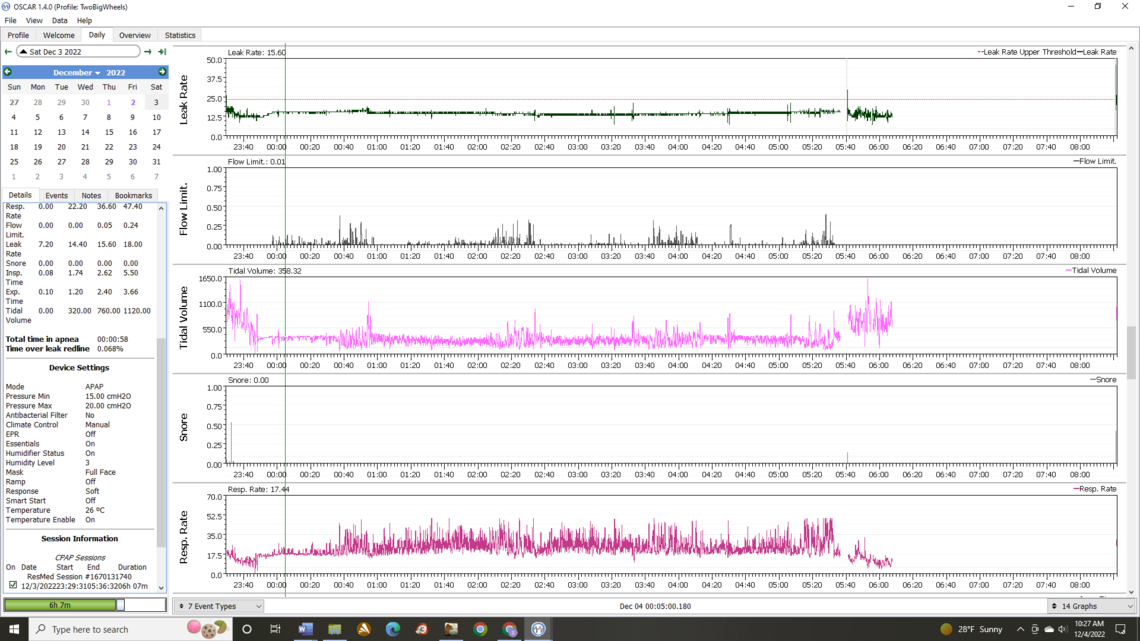
Too bad about leaving the SD card out. I do that every once in a while too. Not sure what to make of the leak rate not going to zero. Are you sure in the machine menu that the mask type is set to full face? If it is an actual leak it would almost have to be damage to the mask somehow. I see that ResMed recommends replacement of the memory foam seal once a month. That would be expensive as I recall they want a good price for it. I only replace the silicone seal on my P10 mask once every couple of years. The other possibility is some damage to the vent system on the pivot point, or misalignment of the parts... But, as I say the leak is not high enough to interfere with effectiveness of the machine. Here is an example of what the leak chart looks like on my machine.
If you think things are fairly stable at these settings it may be time to try adding back in some EPR. I would suggest an EPR setting of 1 cm to start with. And, you will have to switch the type back to full time. The hope would be that it may reduce hypopnea some without causing the OA frequency to go up. It reduces pressure on exhale, so you will get 15 cm on inhale and 14 cm on exhale.
Out of the 3 options (Pillows, Full Face & Nasal), Full Face is checked. Mask is 20 days old and seems in excellent shape. If it leaks, I'd think I'd be aware of it. I always had a hard time getting my Vitera Gel mask to seal (squealing, etc). For what its worth: MyAir shows 20/20 for seal and Smiley on my AirSense.
I tried a DreamWear full face (under nose, over mouth), couldn't get it to seal. P10 is strictly nose? You have no issues with your mouth opening? I think my mouth opens at times and my sinuses aren't 100%.
Fighting redness on the bridge of my nose from the F20
So your recommending 15 cm and EPR 1 cm Full time?
Your mask type is selected correctly, so I am not sure what would be going on. Yes, the P10 is a nasal pillow mask, and does not cover the mouth. I do have issues with opening the mouth. It tried a few different chin straps but finally settled on taping my mouth shut each night. It is not for everyone, but I find it quite comfortable. See this video: How to Mouth Tape for a Better Sleep.
Do you have a heated ClimateAir tube? If you do there is an Auto mode you can use to set the humidity and temperature. It still uses lots of water. I suspect my maximum limit for a night without running out of water is about 9 to 9.5 hours.
Yes, if you think things are relatively stable I would try 15 cm minimum, with EPR at 1 cm full time.
Settings = 15 cm minimum, with EPR at 1 cm full time
I'll contact the sleep center I have a relationship with now and see if they'll give me a P10 to try. I need to give my nose a break. They gave me the F20 setup for free to try (well actually nothing is free). CPAP setting stay the same, except for mask type?
Yes, ClimateAir tube. It was set to Manual w/Tube Temp 78 deg, Hum Level 3. Starting point for Auto? Right now humidity in house 36 after adding humidifier.
I am "pretty sure" I woke up last night 2.5hrs in (1pm CST). No obvious signs on charts. Stayed laid down on side the whole night.
The qty 1 CA I had was 16s
These results look pretty good. Since the EPR of 1 cm did not do bad things and your hypopnea seems lower, I would try EPR at 2 tonight. Leave everything else the same.
If you switch to the P10 the only thing you need to change is the mask setting to Pillows.
If you go into the Clinical Menu and scroll down you will come to a section called Options. Under that if you set the Essentials to Plus instead of just On, the User menu available without going in the Clinical Menu will be enhanced. In the enhanced User Menu you can set both the Humidity and Temperature to Auto. And while you are in the Options section you may want to turn the SmartStart On. I use that so my machine starts automatically when I put the mask on. It is just a convenience feature.
And when I was checking the Clinical Manual I found this illustration. It shows pretty much exactly what you were getting and was being flagged as CSR. I knew I had seen this pattern of breathing somewhere but couldn't find it. Here is the illustration. The important part is that you were not having true CSR, but just rapid frequency OA events. This now appears to have been solved with the cervical collar...
Sleep Clinics reply to how Leak Chart looked on their end after switching to new mask 10 days ago: "Everything is looking good on our end. Typically the leak number will never be at zero. The goal is to be in the recommended range, which you are"
No comments about my improved AHI, etc....
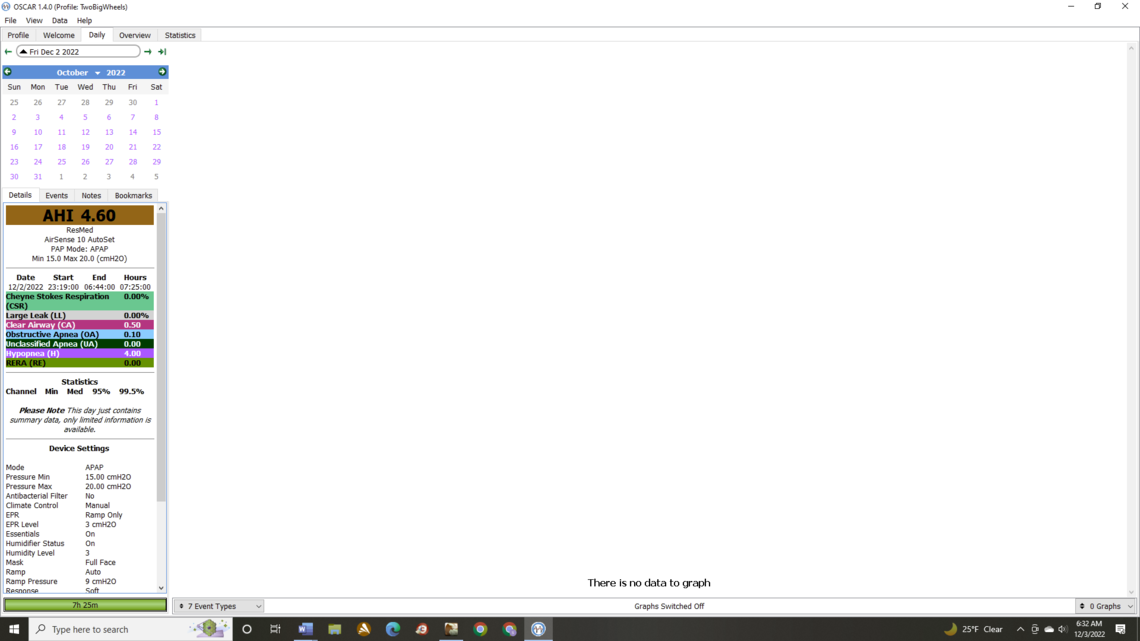
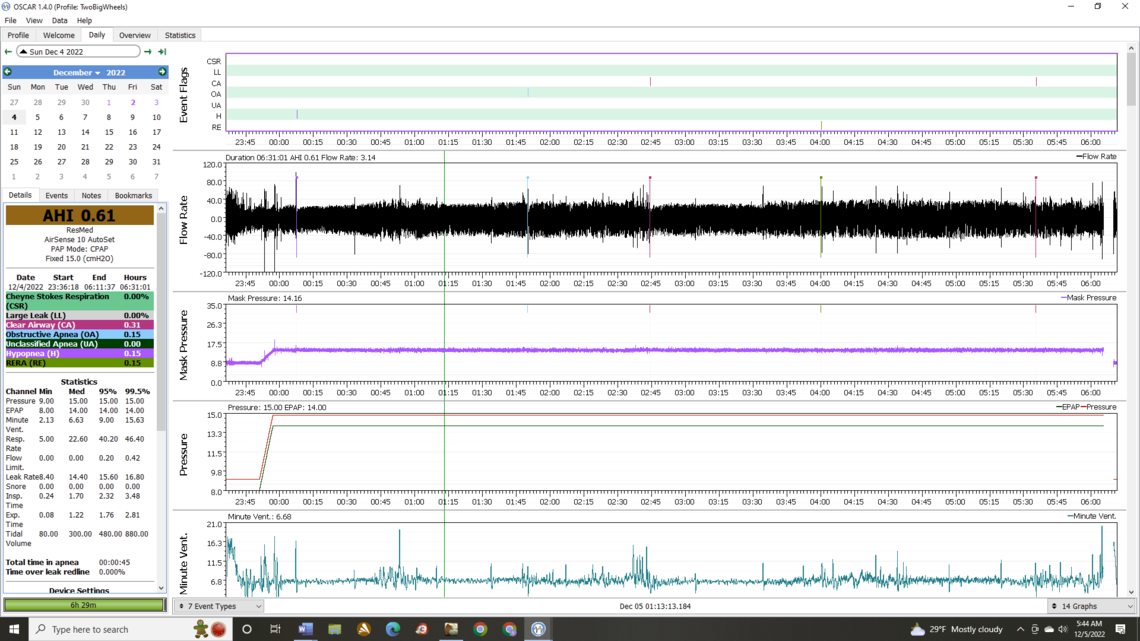
While your AHI has gone up a bit, the overall results look pretty good. Your hypopnea is low, which has been high before and the flow limitations look closer to normal. RERA is gone. CA events are up some, but sometimes when waking up that can happen. Some call it Sleep Wake Junk.
I noticed that since Dec 3 the pressure has been switched back to fixed CPAP mode. This is OK and does not seem to be having a big impact on apnea events as your OA component is zero. However, having it in Auto mode gives more information when trying new machine settings. You can see when the machine thinks you need more pressure. When you get flow limitations it may increase pressure some to reduce them. Being in Auto is a good flag to determine whether or not the pressure is set high enough. While it may be of benefit going to fixed for the long term, for now it would be better to leave it in Auto. To some degree having a machine in Auto is like getting a sleep lab titration test each night if you look at the OSCAR data each day. My long term setting is a fixed pressure, but my wife is using a fairly narrow band between min and max in Auto.
On masks the P10 is a very minimalist nasal pillow type. The weakness has been the flimsy headgear, but I see that ResMed claims to have improved it and the method used to adjust it. My wife uses a slightly less minimalist nasal pillow mask called the Fisher & Paykel Brevida. It has a little better headgear, but it is kind of personal preference between these two. Have a look at them both if the clinic has them.
Going forward I would suggest putting the machine back in Auto with a minimum of 15 cm and max of 20. And I would increase the EPR to 3 cm. I know that didn't work out before, but I think the cervical collar is making a big difference and EPR at 3 may not have been the cause of the poor results. So I would try it. If this works then I think the next step is to start reducing the minimum pressure in 1 cm steps to see at what point OA events start to become a problem again. The 15 cm may be higher than necessary, but it is a good safety net until the EPR setting is finalized. Reducing pressure may also reduce the CA event frequency.
The way things are looking now I don't think you need a sleep lab titration test nor a BiPAP machine. However, if the Tachypnea does not not go away with the increased EPR then I think you should see a specialist doctor about it. Probably start with a pulmonologist.
APAP Pressure Min15.00 cmH2OPressure Max20.00 cmH2O: EPR 3 Used Collar and Slept on side whole night
AHI is up but it is mainly due to an increase in CA events. OA and H are fairly low, and Flow Limitation looks good. I think it is time to try a lower pressure to see if it will reduce the CA events. I would suggest reducing your minimum to 14 cm and leave everything else the same to see what happens. I suspect the pressure is not far off what it needs to be, but you can only find out by trying it. If CA events are going to be an ongoing issue the basic objective would be to find a pressure where both CA and OA are lower and about the same. Hopefully the total will be lower.
Ok. Hopefully will be trying a Nasal Pillow Mask tonight.
That is fine. It should not impact pressure and other settings. Just remember to switch the mask type to Pillows. It will be interesting to see what it does for leaks. I would check carefully all the hose connections to see if there could be a leak, and also inspect the tubing to see if there could be a hole in it somewhere. That leak graph you are getting is suspicious as it never goes to zero. The machine measures the total air flow and subtracts the design vent flow (compensating for pressure) and that is what is displayed as the Leak Rate.
Ok. I know hose isn't that old (still could have a hole). I'll be ordering all new supplies today (hose, reservoir, etc). I will do a bubble test with soapy water.
Another place to look for leaks is the two connections from the machine to the humidifier. There are a couple of silicone seals in there that can possibly leak. I find that when the humidifier is not firmly inserted into the machine, these seals seem to flab back and forth with each breath causing a clicking sound. In any case a place to check for leaks.
My machine is 5yrs old. Not sure on reservoir. Are silicone seal replaceable? Seals part of machine or reservoir (I'm not at home...). How would u check leaks there? Just by hearing?
Check page 24, and further, of the Clinical Manual for some information on these seals. You probably can only visibly inspect and clean them. Another possibility would be the seal between the reservoir and lid of the humidifier. Again probably all you can do is inspect for damage and clean. Parts might be hard to find. I see this one part at CPAP.com for sale. Your clinic may have parts also.
https://www.cpap.com/productpage/resmed-airsense-aircurve-10-humidifier-air-outlet
I have had to replace the whole humidifier reservoir on mine as the plastic catches broke.
If your machine is 5 years old you may want to think about a new one once you have settled on whether or not you need a BiPAP. The normal replacement cycle is about 5 years. ResMed now have the AirSense 11, but it really does not have much for improvements. I believe OSCAR supports it. And I believe it supports 4G for the MyAir system.
A tip when getting the mask fitted. The P10 cushion comes in three sizes. Try to get the largest one that still seals properly. If the mask prongs are too small it will go too far into the nose and cause more irritation. You want to cushion to sit more on the nose rather than in the nose. But, it still has to seal. When you buy this mask on line it usually comes as a "Fit Pack" which includes the cushions for all three sizes so you can try them all. Not sure they will offer you all the cushions to take home. If not, try as above to get the best fit.
Started the night with the AirFit P30i Nasal Pillow Mask with Med cushion (small & med included in Starter Pack with Small Frame) & mouth taped. Med cushion appeared to fit ok in nose. Technician said to keep head gear on "loose side", that pressure would tighten it up. Obvious leak issues and woke up "hard" & glancing at my AirSense 10, it shown Red Face & AHI of 2+. Tightened Head Gear & had a hard time falling asleep, couldn't really put my finger on what felt odd, in hindsight maybe like nasal mask wasn't giving enough air before sleep mode. Went back to what I knew, changed mask setting and put F20 back on.
***Just discovered I didn't set machine to right setting.... I had it set to Nasal, while User Guide says set to Pillows....from what I got out of tech, this was to be Nasal while others I got were Mask. I wrote down Nasal Pillow for P30i and Nasal Mask for others...
Technician was helpful with giving me 5 masks to try,,,only 1 nose only. The other 4 covered mouth and went under nose.
I didn't have time to do leak test, but did order new hose & reservoir (comes with seals).
Tech didn't seem confident the Nasal would work for me (or they didn't have a lot of Nasal's in stock). Tech agreed that there may be leak somewhere, saying that Full Face allows for different leak rate than nasal.
Getting the right mask tends to be personal to each individual. It can take some time, as it is basically trial and error. If they will give you masks to try that makes it more affordable, as some places will not let you return a mask. In any case here is a link to ResMed document which shows how each mask should be set up in the CPAP. As far as I know this setting only impacts the leakage rate calculation. I believe it only shows ResMed masks so if you have something else you have to choose the mask that is closest in design.
Mask/Device Compatibility List
Your results last night were not bad considering you were having mask issues. It looks like you had one or two OA events right before you woke up and that may be sleep wake junk. You can expand the scale and see what the breathing pattern was like when it happened. If it is sleep wake junk it tends to have no defined pattern and a lot of noise.
So you have a choice. You could leave minimum at 14 and work on mask testing, or you could try 13 cm to see if that is low enough to start seeing significant numbers of OA events again. The general idea is to keep lowering it until you are seeing significant numbers of OA events, and then bring it back up just enough to get rid of them.
One other issue that I have noticed is that "Response" is set to "Soft". This will result in a more sluggish pressure response to Flow Limitations and OA events. My wife's machine is set at "Standard", and since I am in fixed CPAP mode this option is disabled for me. I noticed that your machine was showing a much more sluggish response to flow limitations than my wife's machine. So before you lower the pressure to 13, you may want to leave it at 14 cm and change your Response to Standard. When you are closer to the minimum pressure needed a quicker response may get pressure up faster to avoid some of the events. Something to try to see what happens. Just make that change only if you do it, so the outcome is not confused with a pressure change.
If you feel you are not getting enough air with a certain mask the best way to deal with that is by increasing your ramp start pressure. I believe you are at 9 cm now, but it can be set as high as your pressure minimum. What I do is put the mask on and take repeated quick deep breaths. I increase the pressure to the point where I can feel no air restriction from the mask when doing this. It should feel like you are breathing normally with no mask on.