Hi, I did a home sleep study as I've been feeling pretty tired, wife reports snoring that was improving when I lost some weight but has got worse even when I went back up 3-4 kg. Home test was a nasal canula and O2 sensor only, no chest strap. Nothing fell off and it gave a result of : AHI 15.4 hour ODI 16.5 hour Lowest o2 was 73% I would say I only had deep sleep for maybe an hour or so which was probably when the o2 sat went down and heart rate went up on the report. Rest of the time was light sleep and disturbed sleep. How accurate do you think the AHI is on these studies (I am a mouth breather by the way)
I kinda panicked and rented an Auto CPAP from the same place who supplied the home test and have one more week of that. It's proving hard to cope with to be honest.
Got to wait about 1 month for a hospital sleep study, so I'm trying to work out whether to rent a machine for another month or just wait for the hospital sleep study. The o2 sat is bothering me if accurate especially.
Thanks everyone!
With that little equipment the result is not terribly reliable. I'm glad you have an in-lab study booked. With just those 2 sensors, they would not have been able to tell when you were asleep, leave alone which stage of sleep you were in. They can't report a real AHI because those 2 sensors don't return the data required to determine an apnoea or hypopnoea according to the rules. Some brain activity data at least is also required. In fact, that is the most cut down set of sleep study gear I've ever heard of. It sounds rather suspicious that after performing such a flimsy test they were so quick to offer you to spend money on treatment. You may well have OSA, but it would be worth waiting on the lab study to get a clearer picture.
Thanks for both replies. I discovered it's actually a Japanese home sensor (I'm out in Asia) so seems to be legit but I know a chest strap would obviously be better. The machine I have on loan now is also Japanese so I can't view the data on it until I take it back but to be honest I'm not a heavy sleeper anyway so am struggling with using it, seem to fall asleep after a while but then when the air kicks up a notch it wakes me up then I have unsettled sleep the rest of the night. Guess I'm in two minds now whether to rent the machine for another month til I get the sleep study done at obviously quite a cost, but the low o2 worries me or just to wait.
Let me start by stating that I am highly dubious about the entire industry.
When money is a real issue I believe that in many countries you can rent testing equipment overnight (I rented one for less than $100 from my local chemist) that will give much more detailed info than you have described. This data is then sent to an 'expert' and you receive the results some days later. (This service was included in the original cost)
There is the added advantage that you get to sleep in your own bed. :)
I took my results to the sleep specialist at our local public hospital and was immediately issued with a CPAP machine without any further testing or studies.
It can be that simple. Obviously individuals, circumstances, practices and countries differ.
Since then I have personally known of many who have gone through the "proper" processes at considerable expense in both money and time with very little in the way of discernible benefits.
I am not seeking to counter the information and advice above, just broaden the horizon.
The rules in Australia vary from state to state, but if you hold a Pension Card or a Health Care Card you can often access treatment for free (or close to) depending on the severity of your OSA. The private sector often takes advantage of OSA sufferers in various ways, with unnecessary tests, overpriced equipment and so on. One extra problem which we have in Australia is that auto CPAPs cost AU$1000 - AU$2000 more than fixed pressure machines, which is not the case in the US. It is often possible to order a machine online for much less than you would pay for one in a shop. Most patients are, not unreasonably, reliant on their doctors and other medical professionals to give them sound advice which is in their best interests. Unfortunately, too many medical professionals are lured by the easy money which treating OSA can offer.
I think 100% there is a motivation to use a simple home test to push a machine sale. Where I obtained my home based one from (In a developed Asian country) I did that because I knew I wouldn't sleep well in a hospital but when I got the results, although I think the O2 alone is concerning, I was told that they were good enough to prescribe a Cpap and wouldn't need to see a doctor. I'm not exactly criticising the shop as that is the way from what a newbie has read even US insurance companies are going with a home based test leading to an Auto CPAP machine, but when I followed up with a hospital doctor he said it's a good indication but a test in ahospital shows up so much more and should be done prior to deciding treatment. He wasn't against me trying a machine in the meantime as I was concerned.
So I suppose I am saying, that I put off testing for years because a) I thought I couldn't have it and b) it was too difficult to do, so there is a place for home based tests, but being in the middle of this now and about to pay more for a hospital test I would say that you need to follow up a home based one with a proper hospital test even if it costs you more.
Finally, it seems to me as well that you want to be as informed as possible when it comes to treatment, from what I've read even the effects of mild OSA on the cardiovascular system can be helped with CPAP but there are other treatments like mouth guards etc which you aren't going to be able to work out what is most suitable unless you have the full testing knowledge.
So from someone who is figuring all this out, spend the money on the tests, read and then make an informed decision and take advice from doctors but don't treat is as gospel.
Some comments. A sleep clinic test is not going to help you decide between CPAP and dental appliance treatment. If your APAP is collecting detailed data an analysis of that is going to tell you a lot. Probably more than an in clinic sleep test. Even without a detailed analysis, what is your reported AHI? Has it improved?
A CPAP machine, no matter how smart, cannot rival a monitored sleep study in terms of the level of data it returns. A CPAP has 1 sensor to generate all that information. This is one reason why data from a PAP machine has to be taken with a grain of salt. As an example, the sleep study I am recording right now has 21 different channels of data. This is one of the reasons why a proper BiPAP titration can only be done in a lab because there is no other way to get all of the required data (CO2 levels for example).
As with all things medical, there is no substitute for trustworthy, reliable medical advice. A good doctor will work with you and educate you to achieve the best outcomes. A not-so-good doctor will glance at the results, rubber stamp your treatment (or other course of action) and barely acknowledge your presence.
The home test is the cheapest option and the least favoured for obvious reasons. The main push here is for sleep studies which cost a great deal more.
Do you doubt the CPAP gospel? Such heresy cannot be tolerated! :)
I have come to view Apnea as a single link in a short chain that acts as a binding shackle for many sufferers.
Some of the other links in that chain are age, weight, depression, hormone imbalance, inactivity and of course tiredness.
They all cycle around and compound each other. "Fixing" one problem without addressing the others won't solve the larger issues and some of the problems can't be fixed.
That is the gospel according to Biguglygremlin! :P
I am not so convinced that the home test is all that bad a choice. First some are not willing to do the in clinic test, and for them it is the best option. The OP's test was very basic as it did not measure breathing effort. That would only mean air flow, so there is no way to distinguish between central and obstructive. But, if that is followed by a trial with an APAP that does identify the difference, then the whole package, test + APAP gets the job done. The key is to get at the APAP data to see in detail what is happening. At the end of the day the proof in the pudding. The availability of sophisticated APAP machines has changed the whole game.
One problem with home based studies is that they often have very few sensors. It is possible to get one (such as the one I use) which has the same array of sensors as an in-lab study, but almost all of them have far less. This is generally for 2 reasons. 1) this makes the equipment much cheaper to buy and easier to use. 2) The fewer sensors, the greater the chance of a false positive and therefore the more chance of selling a CPAP machine. There was a big fuss a few years ago when it was revealed that a lot of home studies were being performed, and treatment sold to patients, without a doctor being involved at any stage.
Home studies absolutely have their place in the landscape of management of sleep disorders but, as with all things, they need to be used intelligently, responsibly, and with a focus on good patient outcomes rather than making money.
Thanks for all the replies ladies and gents
So just wanted to update you, one question if anyone has some help...
I'm trying to perservere and get the right mask to see if I can actually sleep 6-8 hours with one and it helps, right now I'm feeling worse due to cpap for the last two weeks but I don't give up easy :-)
The main prob seems to have been the mask noise. The p10 I know is quiet in terms of machine and hose noise but what I found was that I could hear my in and out breath, especially in breath very loudly, I suspect due to the smaller nasal fitting and vents. The Swift FX seems to be better for this. Does anyone have any advice on the best minimal mask (Nasal pillow) for the quietest breathing noises? Anything better than the Swift?
Thanks as always, your help is invaluable.
If the machine is getting you down to 1-2 it is highly unlikely you have any significant central apnea issues. Getting the right mask is often the most difficult part. I started with the P10, and then tried the Mirage Quattro, and F20 full face masks to solve the mouth open air loss. I couldn't get them to seal and rejected both. I then tried a mirage nasal mask and did,'nt like it either. Next I tried the F&P Brevida. It was OK but seemed to irritate my nose more than the P10. So now I am back to the P10, and use a Breathewear Halo chin strap, and also tape my mouth (horizontal). I find the P10 very quiet. I believe it is rated at 21 dB, while the Swift is 24. You may be using an insert that is too small. If you buy a new one they are usually sold as a fit pack, which means you get three sizes of inserts. I believe it makes the most sense to use the largest one that will still seal.
On machines I would recommend the Australian ResMed AirSense 10 AutoSet For Her. The For Her model offers an extra algorithm and is the same price. My second choice would be the US Dreamstation. Both are compatable with Sleepyhead.
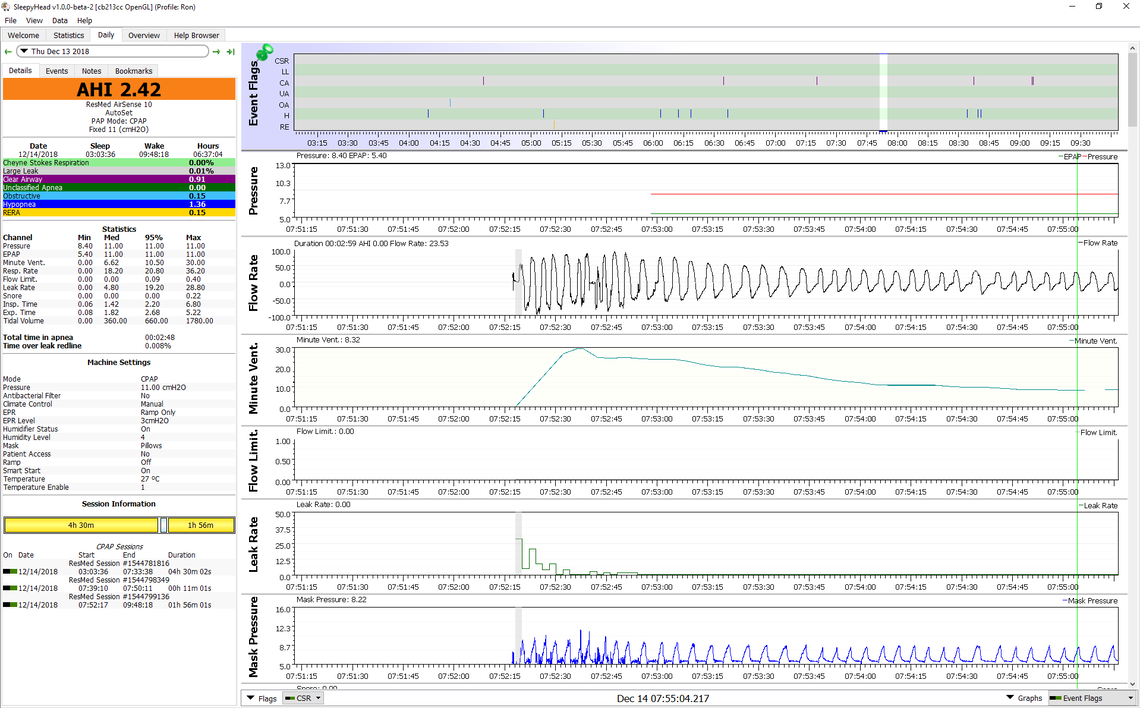
With your mask noise on the ResMed AirFit P10 the problem may be a combination of items. When you first go to bed it is normal to breathe more air in and out until you relax. And in addition with a new user of a CPAP one tends to be anxious and breathe even more. This can be aggravated by a start pressure that is too low, so you feel like you have to breathe more heavily. The higher flow rate increases velocity of the air, and makes some noise. If the mask insert is too small that velocity increases even more. So to avoid it, make sure your start pressure is not too low. I would suggest not less than 7 cm ideally, and I actually use 8.4 cm in my machine. I also use the large insert size, even though the medium seals better. Here is an example from SleepyHead of what air flow looks like in SleepyHead when I was going to sleep after getting up in the night, going downstairs, and then back to bed. I probably was a bit out of breath. You can see that the flow volume (Minute Ventilation) started out at 30 and dropped to about 8 after I relaxed and got my breath. When breathing heavy like this I do hear some noise, but I find it goes to nothing after I stop breathing hard.