I've had mild to severe sleep apnea for the last 15 years. I have a mix of obstructive and central apneas. I have been treated by a sleep specialist, two neurologists, used an oral device, had numerous sleep studies, and one trial period with a cpap device. I did not meet compliance. My last two sleep studies indicated severe sleep apnea.
I am now in the 3rd week using a ResMed AirCurve 10. (BiPAP BIPAP-ST: EPAP=10 cm H2O via mask during sleep 99 mo) I think the higher number is 16. I’m doing pretty good so far. Compliance is an issue though because I have difficulty staying asleep, and keeping the device on at least four hours a night. What happens after a couple of hours is that the pressure pushes the mask off my face. This has been consistent with every sleep study, Cpap and now Bipap I have used.. It does not appear to be a problem with the pressure, mask or equipment. No matter how tight the straps are, I end up gasping for air and fighting the pressure. My theory is that after a few hours of sleep, I wake up abruptly and either start holding my breath, or try breathing at my own rate (time between, and length of breaths) competing with the machine making it almost impossible to keep the mask on. I end up becoming so uncomfortable, I become completely awake, the mask comes off, and I'm awake for the night. Only once was I able to relax enough to fall back to sleep. Since using the bipap, I have been in compliance 13 of the 16 nights. By the way, I normally only sleep 5 to 6 hours a night without a machine.
Since getting to sleep is also difficult even with a long ramp time, I am finding a benefit from trying NOT to inhale on my own, and letting the machine fill my lungs, and then concentrate on exhaling. When I do this, it doesn’t feel like I’m competing with the machine for a breathing rate, and I usually fall asleep fairly easy. I don’t know if this technique is appropriate for this machine, but it seems to work for me for at least getting to sleep. I have a follow up appointment with my doctor in six weeks. In the meantime I’d be interested in the opinions of the professionals and users in this forum. Thank You
The Bipap ST machine initiates your breathing as it records the number of breaths per minute you have taken. The number is a set parameter I think. I am on an Aircurve 10 in Bipap mode and don't believe this ST thing is actuated on my machine. To my thinking, the ST feature may be like stuffing air down your throat and would discuss if this is a benefit or a detriment since you are having problems with compliance. You may want to discuss turning off the ST function with your sleep doc to see if things improve. As far as length of sleep, I sleep between 4.5 and 6 hours generally and this has been the norm all my life. On therapy, I sleep much more deeply and don't feel tired within those times. Follow up on your visit with the sleep doc and hopefully some positive will come of it.
The analogy, stuffing air down my throat, is a interesting way of describing the ST function. It is somewhat accurate, but only seems to occur closer to my wake up time. And, because my AHI average is about 4 per hour and I've only been on the Bipap for about 3 weeks, I will continue to work with the current settings, and definitely discuss them with the doc in about 3 weeks.
easiest way is to go back to your DME, the ST isn't set up properly for you. The waking up short of breath is telling. You may finish up back at the doctor for a script change. If you have a physical problem, obesity, copd etc, then the ST is the right choice. If it's a brain signalling issue and there are a lot of central apnea. Then if your heart is ok, an ASV is more suited. Get a copy of your sleep report. You may need another sleep study to sort it out. If you are self funded, probably apneaboard forum could help you with self diagnosing.
ASV was created specifically for treatment of Cheyne-Stokes ventilation in a setting of hypercapnoea. It can occasionally work in some other cases but it is far from being a magic bullet. It certainly is not effective in situations were ventilation is required to increase oxygen saturation or lower CO2. It should ALWAYS be set up by a qualified, experienced technician (as with any Bi-level ventilation) because it is quite complicated and the way every patient responds to it is different.
Hi, regarding your issue during night i would recommend you to not follow the machine in the breathing and use your tempo on the breath cycling, you have to check the back rate at ST machine which may have been adjusted very high to avoid your sleep apnea, this could be an issue, because BiPAP ST machines generally isn't the correct device for the Central apneas, however sometimes doctors prefer BPAP's instead of ASV due of other cardio reasons. also if your EPAP pressure is on 10 which is high enough could make the compliance more difficult. and lastly one idea is to activate the Ramp time so this will help you fall asleep before the pressures reach the high level and eventually you will sleep little bit more.
Hi CPAPstore My machine is in the ST mode IPAP 16, EPAP 10 RESP RATE 12 TI MAX 1.5s
TI MIN .5s RISE TIME 250 TRIGGER LOW CYCLE MEDIUM
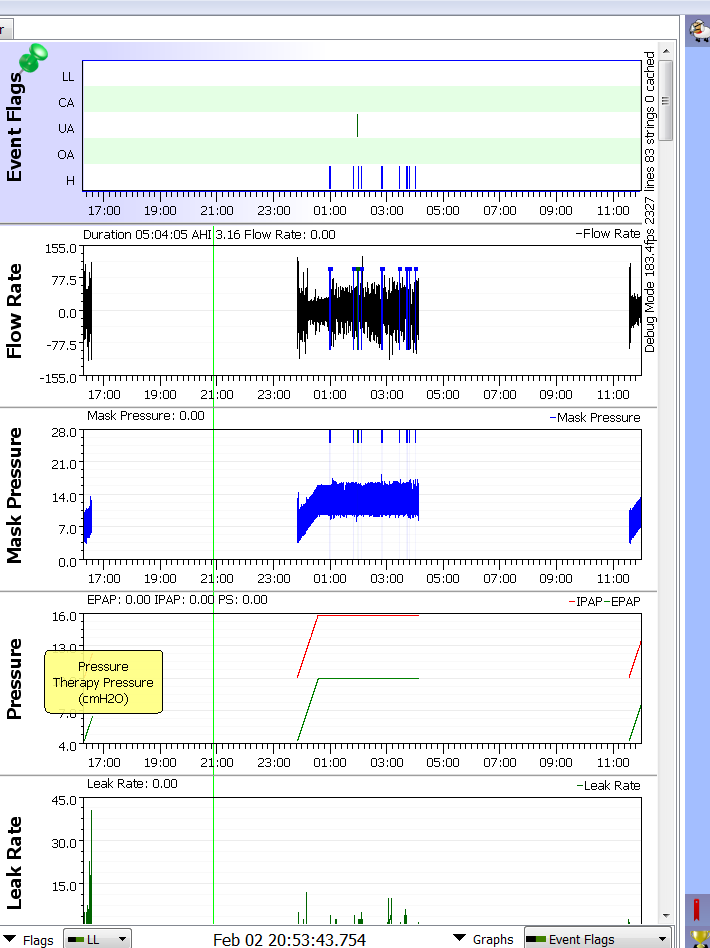
RAMP TIME 45 MINUTES According to SleepyHead, there has been 0 events recorded in the first 45 minutes of usage, events usually do record after pressure is at the max. The only cardio issue I have is high blood pressure well controlled with med. I'm not certain what you mean by back rate, unless you're referring to IPAP . In the current settings, I have been unable to use my own breath rate tempo. When I do try, the pressure starts pushing the mask off. I thought the machine was supposed to adjust to my breathing rate? It seems like I can sometimes slow the machine rate down a little bit by taking extremely long deep breaths, but it is a fight (and I usually lose!). Attached is the SleepyHead summary for my first 22 days on the machine, and one partial daily report. Any further info you can provide would be appreciated.
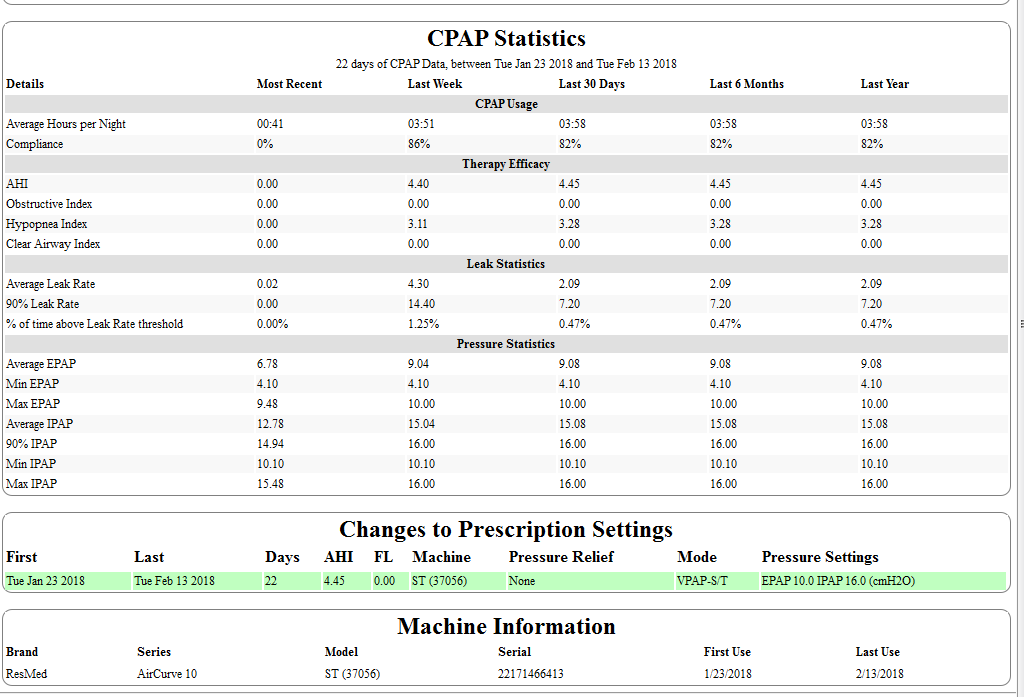
Hi, Back up rate is the 12 resp rate you have it is working as a backup this mean that you will not able to breath at your on breathing cycle under 12 resp rate because machine have been adjusted at 12BPM, the Ti min is at 0.5 means that if you would like to exhale before 0.5 of time the machine will not let you. However regarding your sleepyhead results you have treated you apnea. Have you ever try a autocpap machine before bipap for your treatment? Or even at sleep lab?
Thanks for the info. It confirms what I am experiencing. Basically, I have to allow the machine to breathe for me. Yes , I do see the AHI events are good or at least acceptable, but the issue continues to be the nights that I have been unable to use the machine, or wake up prematurely (about 4 hrs of sleep) as a result of fighting the breathing rate.
No, I have not been on a autocpap machine. After reviewing the way it works, it sound very interesting. My understanding is that my Bipap machine is being used in a rental type program, so if my doctor would agree, and my insurance allows it, I would not be opposed to trying any other machine. I took a quick look, but didn't see a machine that might be able to switch from BiPap to autocpap. An ASV machine was also suggested earlier in this thread as well as having the ST mode turned off on my current machine. I will discuss some of these things with my equipment provider and doctor in the near future. I am also considering getting a Fingertip Pulse Oximeter Oximetry Blood Oxygen Saturation Monitor. Do you have any further advice or ideas pertaining to my equipment or treatment? Thanks again for your input!
Hi,
I'm not sure where the people above are getting there information from but I have been treating people with CPAP, BiPAP, ASV etc for over a decade. BiPAP in ST mode certainly is good for treating central events. In fact it is the default treatment for central events. ASV, As I added above, is only for specific cases.
One of the resasons that ASV is less widely used than it used to be (which is a good thing as too may doctors would throw ASV at a patient without checking to see if it actually worked) is that there was a study which showed an increased risk of mortality if your left ejection fraction is less than 40%. To put it more simply, if your heart is dodgy (in a particular way) then ASV could kill you. This is yet another reason not to get carried away playing doctor with your own treatment.
BiPAPs are complex devices and setting them is equally complicated. Yours was set the way it is for a reason. Your doctor should know what that reason is, so make sure that they explain it to you. Ask question until you get answers and be very involved in your own therapy, but beware of changing stuff based on responses from a forum such as this or, indeed, anything but advice from a qualified medical practitioner.
Many of my patients who use BiPAP say, as you have, that they find it easier to fall asleep with BiPAP when they follow its rhythm. This is fine. It should be adjust to something quite similar to you normal breathing pattern in sleep so going with the flow should not be a big change.
Overall, BiPAP therapy of any kind is complicated and should not be mediated through an online forum, nor should you make random adjustments yourself. I have treated hundreds of people with BiPAP (possibly thousands, I lost count long ago) and it has to be done hands on with all of the data at your disposal. If all else fails, perhaps a different doctor would be better.
Sleeptech, a couple of things. It sounds like you have a lot of experience and knowledge in sleep apnea treatment and equipment, and annoyed with some of the previous answers to my questions. The information you offered to me is very valuable. Others have offered their opinion based on what they believe or what experience they have.
I’ve been at this for quite a while, and you can rest assured that the last thing I personally would do is make random adjustments to my equipment or play doctor with my own treatment. I can’t afford to, and I don’t mean that literally. Sleep Apnea is not my only issue. In another thread in this forum I wrote “> My personal expectation is that I have to work very hard to get the best treatment available to take advantage of the expertise of those in the medical field. My final sentence in my original post was, >> In the meantime I’d be interested in the opinions of the professionals and users in this forum. Thank You. I believe I have already benefited and learned from many posts in the short time I have been in this forum.
Based on the 2 visits with my present neurologist, and the 2 sleep studies that he prescribed resulting in him prescribing the bipap, I have the utmost confidence in him. I have a long way to go with my bipap before I see him. I’m feeling a little better and my AHI’s are dramatically improved, but I’m still only getting about 4 hrs of sleep on the bipap. I still have to master keeping the mask on for at least 5 to 6 hours or come up with an alternative. No fun fighting with the machine to keep the mask on, and being so sleepy and exhausted at 5pm.
I would not say that I am annoyed by any of the previous posts, rather concerned for you health. Random tinkering with machine settings (as some people certainly do) can cause all sorts of problems. It sounds like your approach is considered and systematic which is excellent. The complexity of Bi-level therapy requires a careful and thoughtful approach. I'm also really glad that you have a doctor you can trust - stick to them like glue. It may also be encouraging for you to know that, once on BiPAP, people with complex respiratory failure can improve, sometimes a lot. So hang in there, things can get better, and keep working on your treatment. It is a process, and sometimes a long one, but it will be to your great benefit in the long run.
Thanks for your help and concern sleeptech. It sounds like I certainly gave you the wrong impression by mentioning my other conditions and that one of my specialists was a pulmonologist. That doctor was a sleep specialist who also happened to be a pulmonologist. He was referred to me by my primary physician( they were apparently good friends). My current neurologist and sleep specialist is highly regarded in these areas and was the first doctor to order two consecutive sleep studies prior to prescribing the BiPap. He also is treating me for RLS, and (since I can't detail it better than the doc) here goes: Localization-related (focal) (partial) symptomatic epilepsy and epileptic syndromes with complex partial seizures, not intractable, without status epilepticus. Fortunately for me, these additional conditions are being well controlled with meds. I am very active working almost daily on my six acres (retirement property) and still biking on some moderate hills. With all that is going on, its interesting that right now sleep apnea and disturbances are having the biggest effect on quality of life.