Hi all - pardon me if this topic has already been covered and I missed it. I had a sleep study several months back that lead to a diagnosis of OSA. The sleep doc left a lot to be desired, but that’s a story for another time. They determined through an overnight study that I should wear a full face mask with a pressure of 8.
It took weeks to get used to it, but I finally did and started seeing decent results on some nights. I changed to a better sleep clinic a couple months back. They noticed my results were sporadic and recommend I go on auto from 8-15. My numbers got worse. On my next visit they told me I’m showing way more Central Apnea, so they recommended an overnight study.
I argued against a second study citing the first study, the results of which they have, should have provided enough info and that I can’t afford the 30% co-insurance on a second study. We changed my pressure back to 8 in hopes I’ll get the sporadic good nights I was getting. They recommended a Sleep Shirt designed to keep me off my back (though I don’t really sleep on my back much).
I guess I’m looking for general advice. That being said, has anyone had experience with CA revealing itself following changes in prescribed air pressure?
I’m a little nervous that I’m not getting this under control. The night before we made the switch to a range of pressure I only had 4.3 events an hour (a personal best since staring with the ResMed AirSense 10). I’ve been out of whack since.
Thanks!
Central events can be a result of you pressure being too high, so it's not so surprising that when your pressure was effectively increased you developed some centrals. It sounds like you were steadily improving at 8 cmH2O, so sticking with that for a while may be a good bet. Be aware that it is not unusual for automatic machines to misinterpret central events as obstructive, increase the pressure in response and wind up making things worse. If things don't improve eventually, you may need to think about that second study.
Thanks for weighing in here, sleeptech. I adjusted my pressure up a few times to see if I could find a sweet spot. I had 13-17 AHI the last few nights until last night at 10.4cm I only had 10 AHI. I’m going to keep it there again tonight in hopes that I hit lower than 10 AHI.
That being said, I scheduled the second study for next week and hope it yields some clear data indicating exactly what’s going on with me. I think my apnea issue got really serious for a while when I was traveling in SEA last year. I had been struggling with insomnia for about a year at this point so was taking Ambien to sleep while traveling and was unaware of my apnea issue. My assumption is it was taking me even longer to start breathing following each Apnea event. I had a few resulting episodes while I was there - almost passed out in public, had to go back to my hotel and cool my core temp down with a cold towel and could barely move. I was worried I was having a stroke or something. I had an episode on a plane and on a bus. I went to Bangkok International Hospital Chiang Mai and a doctor told me I had hypertension. I thought I had vertigo as I was dizzy all the time. I was congested. I could go on.
I’ve had intense anxiety lately, which is not normal for me. I’m quite certain this all leads back some health event(s) I had while traveling - and Apnea could be a root cause. I’m on metoprolol for the hypertension and palpitations; it seems to be helping but it makes me short of breath. I’m really hoping to figure this all out and that this seemingly vicious cycle doesn’t continue to perpetuate itself.
Ugh.
I have to know what a "sleep shirt" entails! Sounds like it emerged from the Spanish Inquisition...
Haha. Indeed, wiredgeorge. My doc was trying to give me a more affordable next step since my co-insurance would have left me with $600 out of pocket for another study (which is a problem I’ve since remedied, allowing me to afford the study). The shirt just seems like a silly waste of money. I don’t sleep on my back much. My clinic suggests I do more than I think, which is possibly true, but I doubt it’s even 20% of the night. All I do is toss from one side to the other all night. I’ve slept like that for years.
Here’s a link to the shirt! https://www.antisnoreshirt.com/Rematee_AntiSnore_T_Shirt_p/ts.htm
Bwhahaha. I used to sleep on my side prior to therapy. When I started therapy, I was give a big and cumbersome full face mask and was forced to sleep on my back. I had never slept on my back prior. I played football about 100 years ago and have some fairly significant residual damage in two place in my spine and I would wake from horrible pain. I discovered if I propped up using a tv wedge shaped pillow with a regular pillow on top, I could sleep on my back. Later I changed to a mask that allows side sleeping but still sleep exclusively on my back. I also think that if someone is a habitual snoring machine they can snore on their side as well as back. That shirt has to be one of the strangest things I have seen. $90!!! I think I could sew some cans of peaches on the back of a $5 tee shirt and get the same effect.
My sentiments exactly on the shirt.
I’ve been using the Simplus full face mask and mostly don’t have a problem sleeping on my side. I may give the nasal pillows a try now that I’m used to the CPAP at large, though, I tend to open my mouth and would just have to use a chin strap anyway. Once I know if they’re going to switch me to a BiPap I’ll figure that stuff out.
Yeah, most devices to prevent you lying on your back don't work.
That was my intuition. I’m glad to read you feel the same.
I had my sleep study last night. I barely slept. I’m wondering how reliable the data they collected is. The tech seemed to think I need a Bi-PAP. Problem is, I kept waking up when he’d kick it on. He’d have to shut it off temporarily (put it back to CPAP mode) for me to fall back to sleep. I’m not looking forward to getting used to a new machine.
Ok, sleeptech and wiregeorge (and anyone else who's kind enough to weigh in)...
I met with my doc yesterday following last week's sleep study. As expected, I didn't get a good night of sleep and it was hard to tell if the study yielded clear info on how to move forward. He's going to continue me on the CPAP for now. The sleep tech at the lab was convinced I'd be moving to a Bi-PAP. The plan is to do constant pressure at 12cm and increase if needed. If the Central events continue, he wants to go to advanced modality therapy that is a bi-level with a backup rate structure. It's clear to me that docs basically guess and check. Meanwhile, I'm trying to pull myself together to feel normal on the day to day.
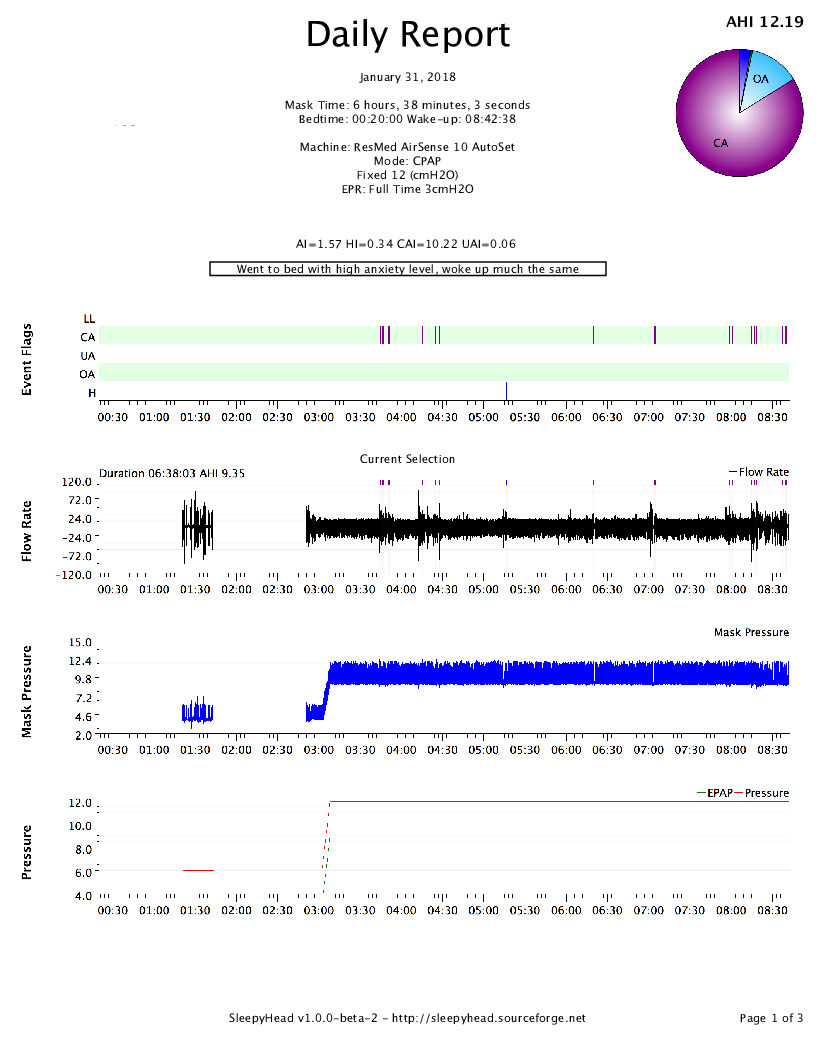
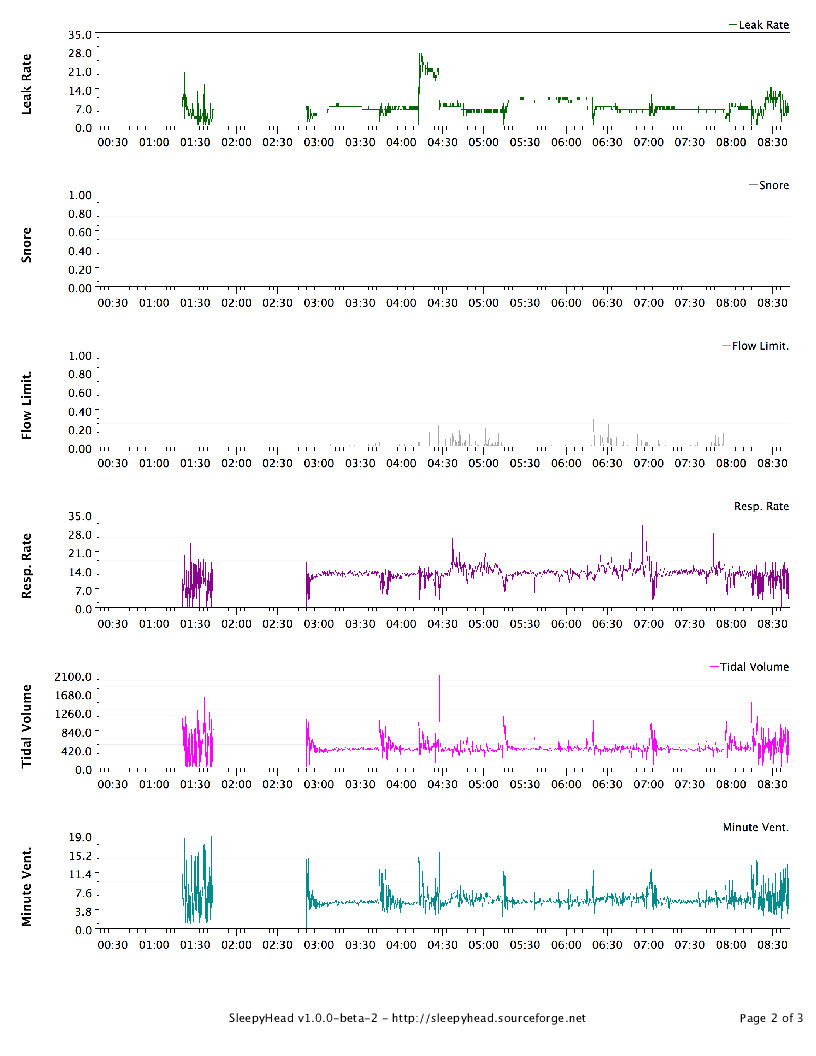
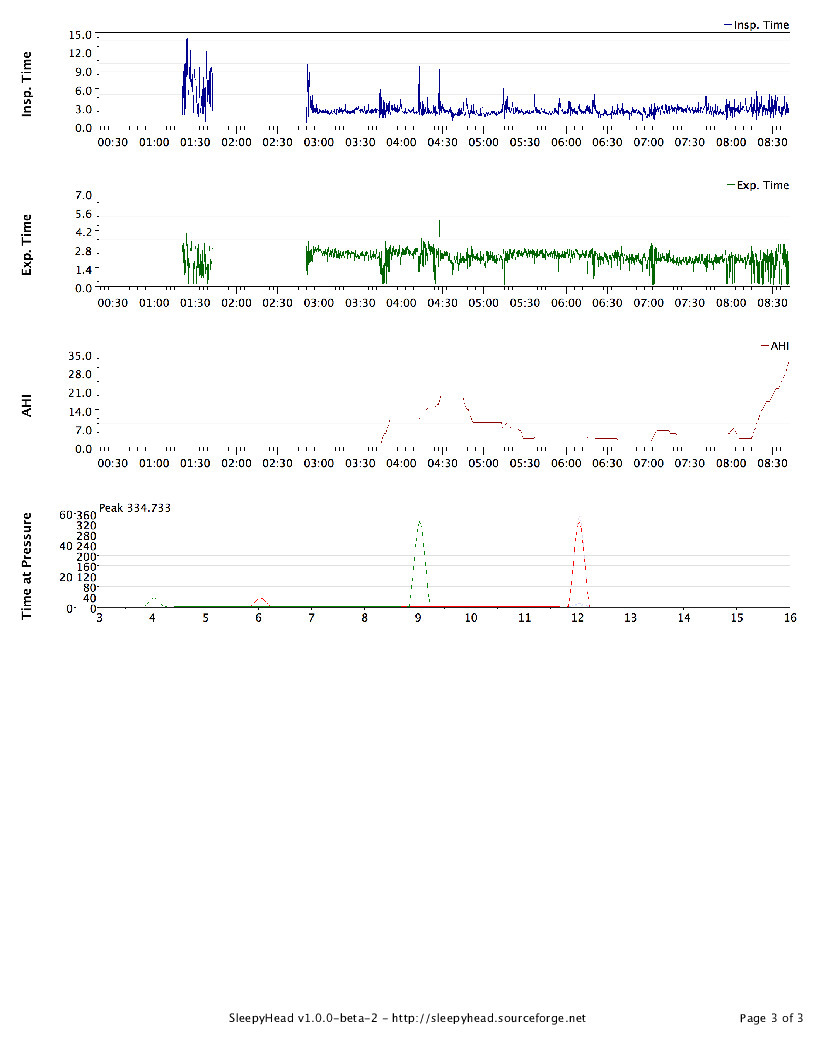
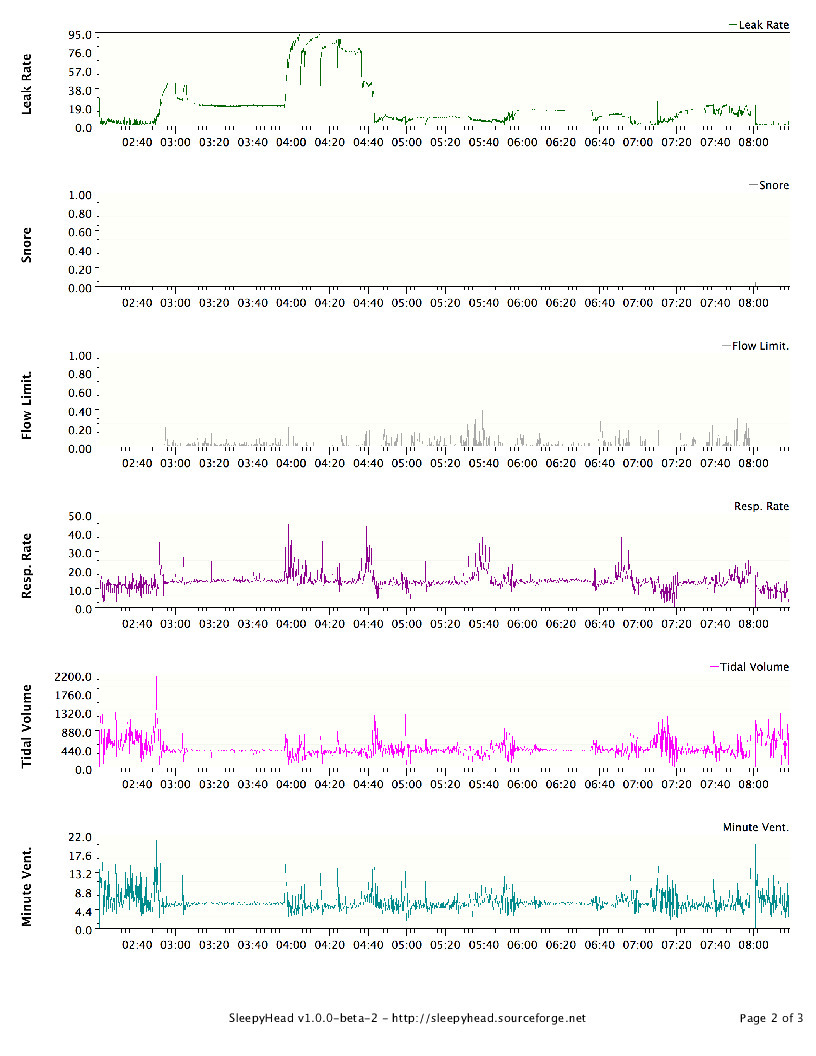
I picked up an SD Card and installed SleepyHead. Last night's data is attached here. I'm trying to wrap my head around it; any thoughts/tips are welcomed. I had much better sleep that last few nights at 10.2cm, but I'm trusting his judgment. I can provide some historic data but apparently the SD needs to be in the CPAP overnight to populate the waveform data (I'm guessing, since it's not there for previous nights. My plan is to stay at 12cm for a few nights and then increase by .2 - .4cm (up to 15cm) every couple nights until I find a sweet spot.
I'm determined to get this figured out and am really hoping these Central events subside.
Thanks,
O-
I can tell you that heaps of people feel that they don't sleep very well during their study but almost all of them get plenty of sleep for analysis, so don't be too put off by that. Also, we'd rather see a bad sleep because the idea is to see a problem if there is one. Just reading between the lines, and please remember that I don not wish to contradict your medical professionals who have all of the data to look at first hand, I THINK what might be happening is that there was evidence of significant central apnoea in your study (hence the tech's comment). Your doctor wants to be thorough so they want to rule out under-treated obstruction by increasing your pressure to see if your AHI reduces. If it does this would suggest that there was still some obstruction that needed clearing up. However, if your AHI stays the same or gets worse, that suggests central apnoea. The doc's comment about "advanced modality therapy that is a bi-level with a backup rate structure" is just along winded way of saying BiPAP and, at risk of sounding rude, it sounds a bit like he doesn't really know too much about it. What he is saying is BiPAP in S/T mode rather than S mode, which is quite common and no one who uses it much would use such a wordy way of saying it. Still, it's far more to do with the tech who has to titrate it for you. I noticed that you have EPR on full time at 3. That can cause central apnoeas by hyperventilating you. Have you tried CPAP without EPR? If you are quite attached to it for comfort reasons, you can set EPR to ramp only, so that once you are asleep it stops. EPR is only a comfort feature, and I have seen it cause problems for many people, so if you are not completely wedded to it I would suggest trying without. If any of the jargon I have used (or anyone else has used) confuses you, please let me know and I shall try to decipher it. That's my job after all. Hang in there buddy. It sounds like the plan your doctor has for you is a sensible one. You should be working your way towards some answers.
Thanks so much for this. It's been a particularly tough couple weeks; it's very helpful to talk this through with someone experienced on the matter.
Yes, indeed, there was evidence of CA in the study. My doctor had seen evidence of it, which is why he ordered the study. I had expected with this confirmation that he would consider that enough evidence. Alas, here I am. :/
I had wondered about the EPR, so I'm very glad you brought it up. I turned it off the other night and had a pretty rough go of it since I'm not used to it. It looked as you see on the attached. The next night, I changed the EPR to 2 and last night to 1. I had slightly better results each night (6.81 and 6.4 respectively). My mouth is opening a lot more during sleep (which means drool in the mask that I have to ignore) and I'm kind of uncomfortable when I wake up but manage to get back to sleep.
I think I'm going to go back to my originally prescribed pressure of 8cm and only use EPR on ramp to see how that goes. Wish me luck!
Thanks, Orvwik
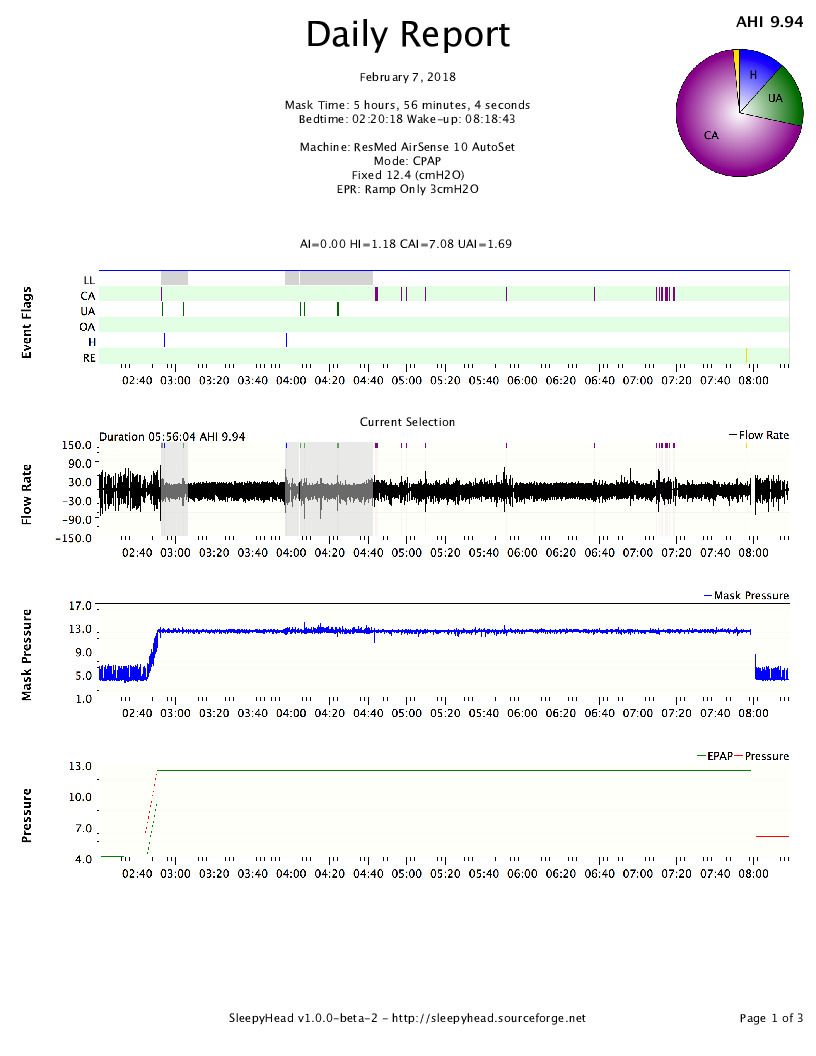
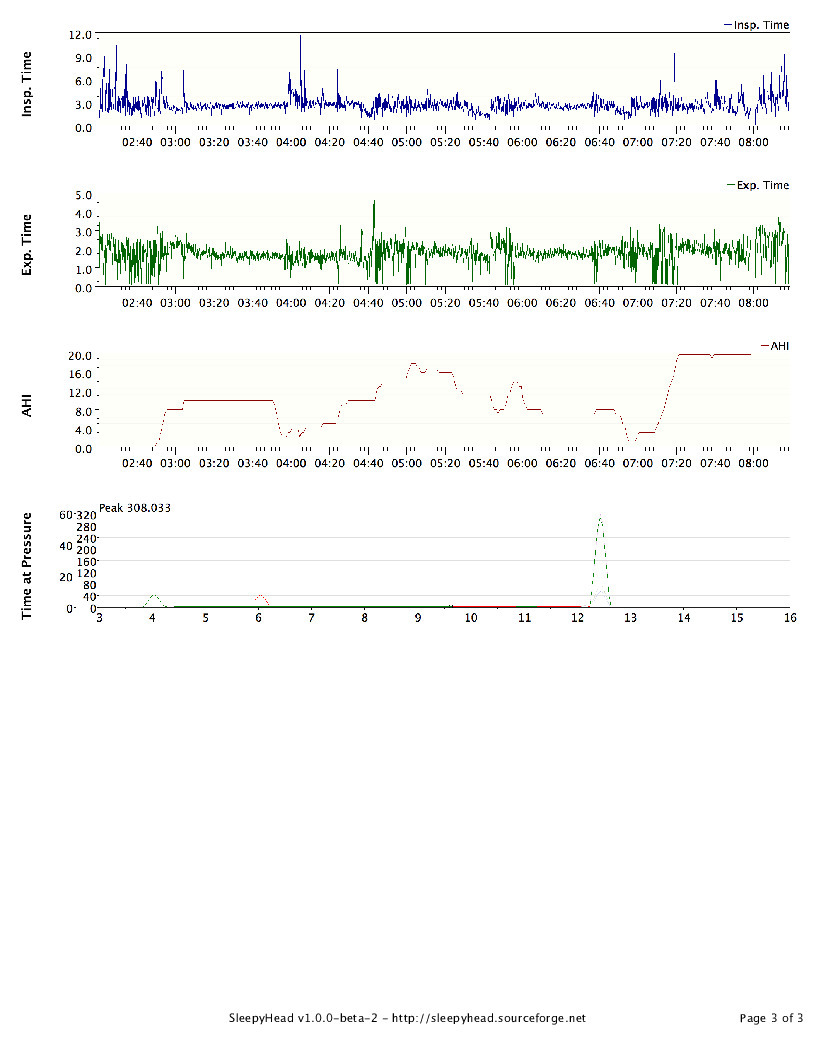
I see that your AHI and your central apnoea index both decreased a little without EPR, although not a heap. You may get some value in persisting without it a bit longer, but I don't want you to be too uncomfortable.
Another confounding factor with EPR is that it effectively lowers your CPAP pressure. If you are on 12 cmH2O but have a EPR of 3, you are effectively only getting CPAP of 9 - 10 cmH2O. I have had patients who were being under treated because they were issued CPAP set at the appropriate pressure, but with EPR on they were in fact getting less than they needed. We only use EPR with patients who have had it in a formal overnight study so that we can be sure it's not messing things up. In your case it is possible that with EPR off you CPAP pressure became too high. I don't recommend that you mess with it because that can cause more problems, I mention it mainly for your education.
You stick with whatever is working for you. Really your medical team should be managing this for you. Hopefully they will look at BiPAP/ASV soon.
That only applies to exhale right? A person would still get the 12cmH20 on inhale. So what difference does it make in the exhale how much the cmH20 is?
What sleeptech said has merit. In a sense, EPR of 3 on a ResMed is very close to being a bilevel with a 3 cmH2O difference. Bilevel can actually exacerbate treatment-emergent centrals. In fact the changes in pressure that sometimes occur with APAPs can increase centrals for some.
I would never be in a big rush to get to ASV, though. It is good to give straight CPAP the full shot for dealing with apneas--obstructive, central, or mixed. And payers have hoops they make doctors and patients jump through, making them try out less-expensive-than-ASV machines first, anyway.
But to get directly to point: The amount of pressure during exhale *can *be just as significant, and sometimes even more significant, than the pressure during inhale.
And although I DO fully agree with ResMed's choice to make their EPR a comfort feature than can be made available in the menu for the patient to adjust, I also feel that doctors, RRTs, and patients need to be aware that ResMed's exhale pressure relief is an especially powerful tool that can have a direct effect on treatment for a significant subset of patients, since it differs from other brands' forms of exhale relief, especially in the way that it is implemented *throughout *expiration.
Why is the pressure during exhale just as important or more important as the pressure during inhaling?
I don’t know if this thread is still active but I am very interested in this subject. I have been diagnosed with complex apneas including OA and CA. I’ve been on CPAP for 10 months. I found that by using a nasal mask, a boil and bite mouth guard, surgical tape over my mouth, a chin strap and a tight strap over my mouth I was able to reduce the obstructives considerably. My Dr prescribed Pulmicourt in a nasal rinse before bed and I take 1/4 Zopiclone per night. My AHI is down from a max of 33 to between 0.80 to 3.5 at present. I turned on the EPR which almost eliminated the obstructives and hypopnia completely but increased the centrals. I track my results daily with the SleapyHead app. I can get up to 8 centrals per night lasting up to 29 sec but typically around 15 sec. Since the EPR setting (3) has reduced my AHI and obstructives specifically should I not continue with this setting? Should I be more concerned with the increase in centrals or is this an acceptable level? I know that I should be asking my doc these questions but she doesn’t seem to have much time for questions.
8 events/night it not a lot, although they do sound like long ones. It's hard to say much without the benefit of data from a full study. The general rule is that if your total AHI is < 5 (all types of events added together, per hour) then you are probably OK. Generally, whatever gives the lowest overall AHI is best.
30 seconds is a long time not to take a breath. Usually it is increasing the EPR that reduces centrals not the other way round. If you have it set at 3 at the moment, try it at 2, but wait a few nights to what result you get before adjusting it again. If it gets worse, just go back to where you were. Sometimes you just have to try things, but do it slowly and with small adjustments. Go with the best average result you get between Obstructive and central. If you have an APAP it should deal with Obstructive Apneas, however, it has a problem dealing with Central Apneas. I would go for the lowest you can get in Central and leave the machine to deal with Obstructive ones, however, you do not want them to increase a lot either, so it might be a balancing act. Sometimes reducing pressure can help, I used to get quite a few Centrals, then I got a new machine that runs at a lower average pressure and the Central Apneas dropped almost to 0, but I still get the odd one. With the APAP and it running at a lower pressure I sometimes get a 0.0 result, however, when the headgear slips or I have a bad night it has been as high as 0.6 AHI with one central. This can be a bit frustrating!
EPR does not treat centrals. Although it operates in a similar way to low level BiPAP, the level is too low to effectively treat central apnoea. It is, however, just enough extra ventilation that, in a few cases, it causes hyperventilation which induces central apnoea. So EPR does not reduce centrals but it can cause them.