Hi, I am using RESMED airsense 10, regarding the EPR setting, 1 to 3, which one is the best? just want to understand the what is the difference of different pressure relief mean. thank you
http://www.resmed.com/assets/documents/technology/epr/fact_sheet/1011940_epr_fact-sheet_row_eng.pdf
I'm glad you asked. This is one of my favourite topics to bend people's ears about. EPR stands for Expiratory Pressure Relief. It is a function that ResMed introduced in their S8 and later models and it is the the same as C-Flex on Respironics machines, which they have had since the M series (although I'm sure both companies would swear blind they're totally different). The idea is to drop the pressure slightly on expiration in order to make the pressure more tolerable. Sounds reasonable but it is, in fact, a huge problem and should be avoided in almost every instance. "Why?", I hear you ask. I'll try not to get into too much detail explaining this.
The first problem is that EPR (and C-FLEX) lower your effective CPAP pressure. For example, if you need a CPAP 12 to breathe properly, but have EPR set on 3, you will only be getting an effective CPAP pressure of somewhere between 9 and 10, and because this is lower than is required you will obstruct. What will often happen next is that the patient will complain of persistent symptoms (because their OSA is not being adequately treated) and their download will show a higher than desirable AHI, so the pressure will be turned up making it less tolerable, increasing leak problems and leading to overall lower compliance with therapy. I have had to deal with this on more than one occasion.
The second problem is that by raising and lowering the pressure as you breathe, EPR actually increases the amount of air that you are breathing. With standard CPAP the pressure is constant, and the movement of air in and out of you lungs is done purely by your own respiratory muscles, so the amount of air you breathe is the normal amount that you should be breathing. All CPAP does is hold your airway open so that you can breathe normally. EPR works like low level BiPAP. As you breathe in the pressure increases and as you breathe out it decreases, which means that more air is moving in and out of your lungs than normal - the EPR is slightly augmenting your respiratory effort. This may sound all well and good, but there is a reason that you breathe the amount you do. Too little is a problem, we all know that, but too much can be a problem too. The extra breathing work done by EPR can be enough to hyperventilate you, sending your CO2 level too low which, in turn, causes central events. Again, I have recorded evidence of this happening.
Where I work, we only ever allow our patients to use EPR or C-Flex if they have had a sleep study with it and we can verify that it is not causing any harm. Otherwise we do not use it at all. I can think of fewer than 5 people who have actually had some benefit from using EPR/C-Flex in all my years of being a sleep tech. The people who sell the machines and the reps for the companies who make them will extol the virtues of EPR/C-Flex and tell you that it is perfectly safe. IT IS NOT. One of the engineers who designed the system admitted as much to another tech I work with.
So, to sum up, do not use EPR/C-Flex unless you have had a sleep study with it to make sure it's OK. It's not worth the risk. On ResMed machines EPR can be set to ramp only which is much less risky. Otherwise, if you think you really need it, get a study done while using it. As always, consult with your doctor, but you will probably find that they know nothing about this, as most of them don't in my experience.
Well, now you can think of 6, because it has been of great benefit to me. ;-) Made the treatment much more tolerable as I could not tolerate the constant pressure of 17 and would have probably quit (or just been miserable). Are the Central Apneas as detected by the ResMed not accurate? I rarely get one. I had one during my sleep study. My AHI is always 2 or lower.
Your ResMed machine should be able to detect the central apnoeas if they develop, so you're probably fine. I'm glad it's helpful for you. For most people EPR is probably harmless, it's just that there are risks, and the number of people for whom it is a problem, albeit the minority, is still pretty significant. Even a small proportion of sufferers from a condition as common as OSA can be tens of thousands of people (possibly even hundreds). This is exacerbated by the fact that the manufacturers tell everyone that it's completely harmless and everyone should use it, so most CPAP machines have it turned on by default. As usual, proper education is the key here, along with healthcare professionals who are prepared to put in all of the work required to do the job properly.
Not quite sure what you mean here...
That is how it increases the amount of air you breathe. Because the pressure increases every time you inhale, it is pushing more air in. It is functioning just like BiPAP. I'm struggling to think of a better way to explain it. Sorry.
So it sounds like this would be useful for a person like myself that uses a BiPap. I've been searching for a smaller travel BiPap and I haven't found anything that looks like it would work. However the Resmed AirMini™ AutoSet™ Travel CPAP Machine has EPR which leads me to believe I could use it as a BiPap replacement. My bipap settings are 14 inhale 11 exhale so it looks like this may be an option for me.
Yes, I believe you are correct. It sounds like your BiPAP is set to an EPAP of 11 cm, with 3 cm of Pressure Support. That is essentially the same as a ResMed APAP set to 14 cm of pressure with 3 cm of EPR.
I would think through the pros and cons of a travel CPAP though. We have a Z-1 that goes unused. The new AirSense full APAP 10 has a nice travel bag that is fairly compact, and it has two velcro straps on it that will secure it to a roller travel suitcase that has a two pipe extension handle. And, a CPAP is a medical device, so it does not count as an additional item or weight to your standard travel allowance.
Thank you!!! I just received my Airsense yesterday and, at 6am without any sleep, searched ‘What is EPR.”
I used to know but that brain cell is totally gone!
I upped my pressure by .2 and turned off the EPR and ahhhhhhh feels perfect!
Good night and thank you again!♥️
My thoughts about setting up the AirSense 10 are as follows:
Set your Ramp on Auto Set the Ramp Start pressure at about 7 cm Set the EPR to 3 Set the EPR to Ramp Only
This will give you an inhale pressure of 7 cm during the ramp and 4 cm exhale. I find that very comfortable. When the machine decides you are asleep it ramps fairly quickly up to your minimum pressure which I would assume is 7 cm or higher. The EPR is turned off at that point so inhale and exhale are the same.
At least that is what I have found best in all my different combinations I have tried I think I am on about version 20 of my machine setup now...
Hello Sleeptech, based upon your comments, it appears that you usually prefer straight cpap? What about apap? What about bipap? What do you recommend? I have two machines. A old respironics remstar auto and a resmed aircurve 10 bipap. Is the old machine ok or the bipap better? Recomendations? Thank you
Thanks tons for this knowledgeable post!
Suddenly the last week or two my CPAP therapy went to hell. AHI was 5x higher than normal. Getting terrible diaphragm muscle pains in the morning. Feeling tired. What the he!! happened? So I checked machine settings and saw EPR was on and set to 3. What the heck is EPR? So I Googled it and found this post.
Turned EPR off and slept like a baby last night. AHI is way way down Thank you.
Not sure how it got turned on, but glad its off now
Had my sleep doc turn it down first as it was very annoying. Still hated it it so I had him turn it off completely. No patient option to adjust or turn off on my machine. Very comfortable now. I could tell that when my cpap thought I was asleep it would turn it off automatically. Sometimes I would try to fool machine into thinking I was asleep so it would shut it off. My doc thought that was very interesting and laughed about it. Now to find the perfect mask. Smalls are too narrow on my mouth but mediums are too tall on my nose. And I wish headgear straps were much WIDER. I wear mine probably tighter than most and find straps bind after being on all night. But I do it for minimal leakage.
Had you thought of switching to nasal pillows? These masks can and should be worn much more loosely. Ours are quite comfortable. We started out with the full face masks but found them impossible for numerous reasons and made the switch after the first 5 months on CPAP. We've never looked back. I was worried about the nasal pillows because I had been a lifelong mouth breather. From the first night of using my new mask, I found the feel of having pressure escape when I opened my mouth was very uncomfortable and I closed my mouth to avoid that uncomfortable feeling. My brain was very quickly trained to close my mouth while I sleep. I get through the night with minimal to no leakage at all. Also, I found posts to the forum during that time (6 years ago) that offered other very helpful techniques for keeping the mouth closed at night and all without using physical means such as chin straps, etc.. I'm truly amazed at how pliable and powerful our minds are. Happy 'pappin' to you.
Nasal or nasal pillow masks are not really suitable for high pressure therapy settings. Mask type is sometimes limited for high pressure prescriptions. If Cyberslayer is having a hard time with mask SIZE due the mouth and nose variation, he could look at a mask like the Amara View. It has a size but that size pertains mostly to the mouth area as it fits up under the nose and is considered a full face mask without covering the nose.
EPR is a ResMed term for Expiratory Pressure Relief. It is simply a reduction in the mask pressure when you exhale compared to when you inhale. In theory the setting refers to the number of cm of water pressure difference. To the CPAP user it usually feels subjectively good. The higher pressure on inhalation helps you get air in, while the lower pressure on exhalation makes it easier to get air out. It sounds like a good thing, so why wouldn't you always use it? This is where it starts to get complicated, but my resolution of it is that for most, but potentially not all people, obstructive apnea occurs on the exhale side of the cycle, not the inhale. So, if you have your machine set at 12 cm for example, and the EPR at 3 cm, you are only getting 9 cm pressure on the exhale cycle and that is your effective treatment pressure preventing obstructive apnea on exhale. And, at the same time your mask has to seal against the 12 cm pressure. Now if your machine is in APAP or AutoSet mode it will increase pressure to compensate for the EPR providing your maximum is high enough. If it is not, then treatment is going to be limited, and your AHI is likely to go up.
I use the AirSense 10 Autoset machine, and this is how I use EPR. I have found that I can run about 1.5 cm lower pressure and get the same effectiveness with the EPR off compared to having EPR set at 3. But, I still use EPR set at 3 during the Ramp cycle of use. I find the EPR of 3 makes the CPAP more comfortable when I am awake and trying to go to sleep. I set the Ramp start pressure fairly high (8.4 cm currently for myself), so it cycles between 8.4 cm on inhale to 5.4 cm on exhale during the ramp period. I use the A10 Auto Ramp feature, which holds the pressure at that level until it senses you are asleep, instead of the gradual ramp up for a set period of time. And, there is a setting to make EPR effective on Ramp Only in the Clinical Menu.
This said, is turning EPR off effective for everyone? Well for my wife not so much. She seems to get less benefit than I do from turning it off. Must have something to do with when/how she gets apnea. She seems to gain less than 1 cm by turning it off.
What about A-FLEX or C-Flex used by Dreamstation. Well, it seems they don't really reduce the pressure on expiry although they use the same 1, 2, 3 setting scheme. They just shape the pressure response a bit on expiry, but the average pressure is not really reduced any significant amount. So, while I have not used those machines, I kind of think the setting may be a bit of a comfort perception thing. If you try it and like it, then use it. But, it probably does not change the treatment effectiveness like it does on the ResMed machines. Those are just my conclusions. Here is a link to an article on the differences between the machines in this feature.
C-Flex and A-flex do reduce the pressure on expiration, but not always by the same amount as is the case with EPR. I cannot remember the details of exactly how C-Flex differs from EPR (one of the reps explained it to me recently) but it is effectively the same thing and I can testify from first hand experience that it can cause the same problems as EPR. Use with caution and consultation.
There is a link below to a good article/study on the different techniques. I think the short story is that EPR is a fixed pressure drop equal to the setting, but does not allow pressure to drop below 4 cm, so it gets limited with low mask pressures. The Flex pressure drops are modified to be flow dependent and more drop is allowed at higher treatment pressures. The net result seems to be that Flex has a drop, but it is less than EPR, except for the P-Flex, and it has less of an effect on AHI.
Here are a couple of real life examples of using EPR compared to not using it.
On my AirSense 10 AutoSet I adjusted pressure over time to do the best I could with an EPR of 3. To get a technically acceptable but poor AHI of about 4 I needed a maximum pressure setting of 15 cm. Now over time with EPR set at 3, but acting only during the ramp (set on auto) period of time, I have managed to get my maximum pressure setting down to 12 cm. While my AHI is still not super great because I have central apnea issue, I still have gotten it down to the 2.4 range, with the lower pressure of 12 cm. If you look at obstructive apnea events only, I do much better, with my last night actual scoring at zero for OAs! After I go to sleep I don't find it hard to exhale against 12 cm of pressure.
My wife uses a ResMed S9, and has been using it over 3 years now. I tried some time ago to convince her to stop the EPR, but she said she did not like it. So up until a couple of weeks ago she was using a maximum pressure setting of 15 cm and an EPR of 2 (that was our compromise a while ago), and getting an AHI of 1.6. While she started with a diagnosed AHI in the 70's and more than double my diagnosis, she gets much better AHI's as she has almost no centrals. Two weeks ago I convinced her to try the no EPR route again. I set her machine at EPR 3 but ramp only, with a maximum pressure of 14. Her average AHI to date with this setting is 1.1, and she even got a zero AHI in the past week. So far, my wife has not complained this time about exhaling against 14 cm of pressure. Now if she stops getting nights with zero AHI the discussion may be back on again!!
So, I gained the full 3 cm of pressure reduction with the elimination of EPR during the sleep period. My wife gained 1 cm reduction with a 2 cm change in EPR. So, it seems the hit from EPR can be a bit of an individual thing.
On the issue of getting more oxygen due to the high pressure during inhale compared to exhale, I am not so convinced. For sure it is real, but I have to question the magnitude of it. Why? The amount of oxygen in air is determined by the absolute pressure of the air, not the relative or gauge pressure that we use in CPAP. At sea level using CPAP units of pressure the absolute pressure is 1033 cm of water. So if we make an EPR 3 cm change in pressure that changes the oxygen content in the same volume of air by 3/1033 or 0.3%. Not a big number. And to put it in context our weather is changing our actual atmospheric pressure in the order of 35 cm of water from a high pressure event to a low pressure event. That means oxygen content is changing just due to weather as much as 35/1033 or 3.3%. That is a much higher impact than using EPR.
That said, I encourage using EPR, but only during the ramp period where it does not compromise the treatment of apena when you are sleeping.
Hi, I am using RESMED airsense 10. Please excuse my English. In German fores it is said to raise the EPR in order to avoid the air to be going into the stomach. Does that really help?
I understand excessive air in the stomach is called aerophagia, and does occur in some CPAP users. I have not had any issues with it while using EPR and when not using it, so no personal experience. I will give you a link to read about it. There seem to be many potential causes and many potential ways to address it. Pressure can be too low, causing you to gulp air. Pressure can be too high, forcing excess air into your stomach. With respect to using EPR, it is suggested that raising it, or setting it at 3, not zero can reduce pressure during exhale and may reduce the swallowing of air. While that might be true on a fixed pressure CPAP, an Auto CPAP like the AirSense 10 AutoSet, may respond to the reduced air on exhale if it produces any apnea events or flow limitations. It increases pressure to compensate, and effectively defeating the EPR.
In short, complex. The easiest thing to do is try using EPR at 3 and compare it to EPR turned off. Watch what happens to your AHI scores. Do they get worse? If this is not an obvious solution you probably should go back to your provider to see where you stand with pressures and what could be changed to reduce the aerophagia. Suitability of your mask should also be reviewed.
Thanks for all the info on EPR. I had. No idea. . . Have been on CPAP for just over 2 years (air sense 10, nasal pillows). At diagnosis, my AHI, ranged from 5-8. Wth treatment it was about .5, until this past month. Now it is jumping all over the place. Several in the 4-6 range. AHI is now 1.6 for the last 30 days. I had a similar spike last year, only lasting a couple weeks, and my provider was not concerned, as AHI was still just below 1.0. Early on the central AI was about 50% of the total AHI. Now it is closer to 90%, if I am understanding the numbers correctly. Today's reading for last 30 days AHI 1.6, central AI 1.4. I turned off EPR, and will see how that goes.
Central apena do not respond well to APAP treatment, but turning off the EPR is certainly worth a try. Your machine simply ignores CA events and does not respond to them.
Tried EPR off a couple nights. Did not like the feeling. Also no change, event wise. So it is back on and I see sleep Doc soon.
I have similar issues with central apnea. I seem to go in stretches when my AHI and CA's are low. Then I go on a stretch where I get an AHI over 5. Last night I actually hit 7.5. I don't think they are going to get very concerned about it until you start to average over 5 for AHI.
On trying EPR off, I would focus on the obstructive events. Compare the number of OAs you get with and without EPR. My thoughts are that if I can get OA down then I can live with higher CA.
EPR is fixed 1 2 or 3 cm H2O on entite exhalation. A-Flex\C-Flex 1 2 or 3 depends on the amount of inhalation. Big breath it the relief is bygger, small inhalation small relief. But nerver more than its value 1/2/3 cm. And c-flex a-flex differs because it doesnt relief more than half of the exhalation cycle. After half exhalation it goes back to initial pressure that was at the start of the inhalation. This prevents apneas that can occour if u use pressure relief on entire exhalation
I believe the other difference in the two methods is that the Flex methods use a timed predictive technique in the switching between the two pressure levels. The EPR method is based on flow. It tries to follow what you want to do. There are pros and cons to each method.
The EPR is static on 1 2 or 3 cm not flowbased like Flex
Yes, I understand that Flex uses the flow rate, and set pressure to determine how much and when to cut back or increase EPAP during the exhale portion of the cycle. What I am talking about is the "decision" by the machine to make the switch from EPAP to IPAP or back. I believe Flex tries to predict using timing when you are going to breath out or in, while ResMed uses flow rate. I didn't see flow change for 1 sec so it is time to switch kind of logic.
I used a Fisher and Paykel machine in my trial period, and while they are not very forthcoming on how they do the switch from IPAP to EPAP, I strongly suspect it is a timing based logic similar to Flex. I often found the machine trying to force me to start a new breath when I really didn't want to. It wasn't a major effect, but it was noticeable. I complained about it, and I think all they did was turn down the EPR. I find the ResMed AirSense to be totally unobtrusive in making the switch when EPR is on and even set at 3.
Are we talking Bipap/Bipap-Auto and BiFlex? Or do you relate inspiratory flow as IPAP and EPAP as expiratory because u set Flex. In a APAP u dont talk about EPAP and IPAP. Auto -pressure with pressure relief but i understand what u mean. Resmeds algoritm is more aggressive and Philips algoritm is like u say waiting for the patients breath.
coimeten2099 - what's your take on sleeptech's comments:
"do not use EPR/C-Flex unless you have had a sleep study with it to make sure it's OK. It's not worth the risk."
Sleeptech makes a lot of good comments and is obviously very experienced. However, this is one subject where I partly agree, but not 100%. I believe the main problem with EPR or Flex is that it reduces EPAP (exhale pressure). Apnea can occur on the exhale as well as on the inhale. So if you have an APAP that is set up and working reasonable well, and then turn on EPR at 3, then it will reduce your EPAP by 3 cm. That is most likely to increase apnea, which will in turn cause the APAP to increase the treatment pressure. The net result will be an increase in maximum mask pressure, which may cause discomfort or mask leaks. But, your apnea incidence is likely to remain unchanged albeit with a higher IPAP (inhale pressure). A problem can occur if your maximum pressure is set such that the APAP cannot compensate for the EPR. Then apnea incidence is likely to go up.
I would suggest it is controversial whether or not EPR, and especially Flex actually increases oxygen uptake and as a result may cause some central apnea. I have tried with and without, and can see little difference. This said there are some instances where EPR or Pressure Support in a BiPAP can actually help with the breathing effort, and may reduce central apnea. I believe this only works when the body is slowly reducing breathing effort, and the APAP or BiPAP somewhat compensates for this by switching quickly back and forth between IPAP and EPAP pressures. It is kind of like artificial breathing, but the effect is pretty modest. It is more effective in a BiPAP where the pressure support can be increased above the 3 cm limit of EPR.
What does this mean? For me the increase in IPAP and thus mask pressure is real when I use EPR. I can reduce maximum pressure by about 2 cm when EPR of 3 is turned off. But, especially when going to sleep there is a definite comfort benefit in using EPR. What I do is use the AirSense 10's auto ramp feature to set a comfortable start pressure, and set the EPR at 3, but for the ramp only. After I go to sleep and the ramp ends, the EPR ends. Pressure then ramps up to my minimum, and I don't notice it when I am sleeping.
So in short I think EPR is good for ramp only for most users, but it is not a big risk to use it full time especially if your maximum pressure is low. But if you want to minimize mask pressure, then turn it off. Treatment of central apnea is more complex, and EPR or Pressure Support may help if carefully tuned.
Thank wiredgeorge and Sierra for your replies.
(My native language is Swedish, so bare with me)
Wiredgeorge, yes sleeptech is a trustworthy source here.
I also understand that coimeten2099 has valid inputs. And gives us a wider knowledge about different brands in comparison.
Sierra, I am a 52 year old man that was diagnosed with obstructive apnea. I also have astma, but not central apnea.
I use the RESMED airsense 10 since one year approximately.
The healthcare detected high blood pressure cause of apnea. And since I got the apap treatment the blood pressure has gone down. But now when I went through a 24 hour test I've noticed that the blood pressure is high during awakening.
I've also noticed that I can wake up a couple of times catching my breath........ when I'm half awake, so to speak, it's almost like I have central apnea.
This is quite scary, when you find yourself not even atempting to breathe.
What sleeptech is writing is not to be taken lightly. The industry itself will never bring up matters like this. Obviously they want to develop their products to be as good as possible to be competitive and sell more. But during development there will be issues like this. And these "issues" can actually cost lives(!)
Now to my point. I've tried with decreasing the EPR-level from the preset level 3 to 2, 1 and finally the last weeks turning it off.
When the EPR turned off completely, I've noticed a very big difference. I breathe much better and sleeps better. My natural brething (respiratory effort) is normal again.
If the EPR-funtion (Expiratory Pressure Relief) affects and increases the CO² levels creating central apnea we should never even consider trying out the EPR(!)
As sleeptech mentioned: "should be avoided in almost every instance."
Concering CO²-levels and central apnea: "I have recorded evidence of this happening."
"Where I work, we only ever allow our patients to use EPR or C-Flex if they have had a sleep study with it and we can verify that it is not causing any harm. Otherwise we do not use it at all. I can think of fewer than 5 people who have actually had some benefit from using EPR/C-Flex in all my years of being a sleep tech."
Please take his warnings seriously.
(For comfort, setting the ramp with EPR is of no harm obviously.)
A post from Ace copied and pasted here:
"Sierra, I am a 52 year old man that was diagnosed with obstructive apnea. I also have astma, but not central apnea. I use the RESMED airsense 10 since one year approximately. The healthcare detected high blood pressure cause of apnea. And since I got the apap treatment the blood pressure has gone down. But now when I went through a 24 hour test I've noticed that the blood pressure is high during awakening. I've also noticed that I can wake up a couple of times catching my breath........ when I'm half awake, so to speak, it's almost like I have central apnea. This is quite scary, when you find yourself not even atempting to breathe. What sleeptech is writing is not to be taken lightly. The industry itself will never bring up matters like this. Obviously they want to develop their products to be as good as possible to be competitive and sell more. But during development there will be issues like this. And these "issues" can actually cost lives(!) Now to my point. I've tried with decreasing the EPR-level from the preset level 3 to 2, 1 and finally the last weeks turning it off. When the EPR turned off completely, I've noticed a very big difference. I breathe much better and sleeps better. My natural brething (respiratory effort) is normal again. If the EPR-funtion (Expiratory Pressure Relief) affects and increases the CO² levels creating central apnea we should never even consider trying out the EPR(!) As sleeptech mentioned: "should be avoided in almost every instance." Concering CO²-levels and central apnea: "I have recorded evidence of this happening." "Where I work, we only ever allow our patients to use EPR or C-Flex if they have had a sleep study with it and we can verify that it is not causing any harm. Otherwise we do not use it at all. I can think of fewer than 5 people who have actually had some benefit from using EPR/C-Flex in all my years of being a sleep tech." Please take his warnings seriously. (For comfort, setting the ramp with EPR is of no harm obviously.)"
My reply to your post:
Based on my personal experience when I awaken during the night short of air, I believe I have had an apnea. It could be either central or obstructive. I unfortunately suffer from more central apnea events than obstructive, and increased pressure is of no benefit in reducing central events.
I have also adjusted EPR from none to 3 on numerous occasions. As I said in my post, it has had no repeatable impact on my frequency of central apnea. But also as I said I can get the same apnea normalization with less maximum mask pressure when EPR is turned off. On that part I agree with Sleeptech. It has some negative impacts but I would suggest it is in mask pressure not any impact on central apnea frequency.
With respect to impact on oxygen and CO2 levels I think you have to put it in perspective. We are talking about a pressure increase of 3 cm of water. Yes, that means more oxygen will go into the lungs, but the question is whether or not 3 cm is significant. I won't bore you with the math, but if you do it the atmospheric air pressure when the weather changes from a low pressure formation to a high pressure formation, the pressure in CPAP units changes by about 35 cm of water. That is a factor more than 10 times higher than turning EPR on or off at a setting of 3 cm. My conclusion is that 3 cm is not significant in the scheme of things. Also remember that standard atmospheric pressure is about 1030 cm of water in absolute units. A change of 3 divided by 1030 results in a very small percentage change.
You mentioned that you gained some benefit by turning EPR off. Again without going through my previous post again, I think that is quite possible in that depending on how your machine is set up turning EPR off may reduce the frequency of obstructive apnea. Have you quantified what your before and after central and obstructive apnea frequency was? I find one needs to document at least a month's worth of data to determine what the change had been.
Another thing to consider is that one of the treatments for higher than 5 AHI due to central apnea is to use a BiPAP machine. A BiPAP really only differs from an APAP in that it can use an EPR of higher than 3 cm. Yes it is called pressure support but it is really the same thing -- a split in the IPAP and EPAP pressures. And central apnea is actually treated by using a higher than 3 cm split in the pressures. Some question the effectiveness of it, but it is done. I know because I suffer from central apnea and I have investigated all options to deal with it including a BiPAP and an ASV machine.
So I will say again that I agree with Sleeptech in that there are some downsides to using EPR for someone who is mainly suffering from obstructive apnea, but causing central apnea is not a very likely one. It certainly has not been my personal observation although I wish it was. I don't think you will find credible sources elsewhere that suggest it causes central apnea either. If there are, I have missed them. If you have them, then I certainly would be interested in looking at them.
Most likly, there aren't any studies on EPR causing central apnea.
But the single fact that EPR can cause a brething pattern like hyperventilation is enuogh evidence to see the link with raising CO² levels and central apnea.
What we have experienced in person is not the most accountable matter here when professionals in clinical tests have proven otherwise. And the words of sleeptech are not wage.
Everyone are responsible for their own wellbeing, and I can understand your eagerness in finding solutions for your health. We all are in the same position I believe. But as I mentioned, sleeptech is quite direct in his statements. We should be aware when someone in his position and with his knowledge very honestly shares his warnings.
Contradicting myself a bit, by referring to my own experience, I have experienced when half awake that my natural respiratory efforts are almost nonexistent. Not a pleasant experience.
This doesn't occur when the EPR is switched off. But you're right about having a longer test period as basis to my point of view.
Wow, what a very interesting post. Why did I read it? Well, I recently was provided with the ResMed 10 auto. This is probably the forth or fifth machine that I’ve had over the years and the only one that has prevented a good night’s sleep.
I use a full face mask as I’m a mouth breather and ‘suffocate’ when breathing solely through my nose. My mask is a Fisher Paykel which, to me, is good mainly because the exhaust points up and away from my wife. I sleep on my side and have until recently not had a problem. However; both my friend and I have suffered the same issues with the ResMed 10.
In my case, I have no ramp set as I can’t stand it or I’m asleep before it kicks in. ResMed ‘no ramp’ is a slow ramp anyway! Minimum used to be 7.5 on my old machine but I’ve had to up this to 8.4 because the EPR will not turn off and I can sense OSA just before drifting off to sleep. Is the machine supposed to ‘bounce’ (rapid pulses) the air if it senses OSA? The bounce is something that I have experienced a couple of times so was wondering if it was supposed to do this? I’ve not seen any documentation on this ‘feature’.
Interestingly, a friend also received the same machine within a couple fo weeks and it was his first time ever to use one. The biggest issue that both my friend and I have is that when awake during the night for whatever reason, the pressure appears to be at its strongest with the mask leaking from the side. I’ve reduced the setting to 12.6 from 20 in an attempt to reduce the mask leak. Probably the noise from this is what wakes me anyway but once awake and lying there adjusting the mask for no leak, the air pressure does not reduce itself at all. The only way out of this is to turn the machine off and then back on again by which time I’m usually fully awake!
He contacted the manufacturer and they agree it was faulty and he had it replaced twice as the second machine showed the same problem! I will be getting mine sorted soo too. Is it just the latest machines that do this?
Back to EPR. Even with this set to off, I still get a reduced pressure on exhale. I hate this. What are suggestions to make it work for me please. Maybe the best option is to return to my previous machine and get a good night’s sleep for once!
I use the AirSense 10 AutoSet and find the ramp and EPR works very well for me now that I have it set up properly. Here are my basic settings:
Ramp: Auto (Which means it holds the pressure until I go to sleep and then it ramps up)
Ramp Start Pressure: 8.4 (This is what I find comfortable but somewhere in the 7-8.6 range should work for most)
EPR: On
EPR: 3 cm
EPR Type: Ramp Only
So what that does for me is give me an 8.4 cm inhale pressure which I find very comfortable, like I am wearing no mask at all. It also gives me an exhale pressure of 5.4 cm (8.4 minus the EPR), which I also find very comfortable. It continues this way until the machine detects I am asleep. Then the pressure ramps up fairly quickly to my minimum set pressure of 12.2 cm, and the EPR turns off. Both inhale and exhale are now 12.2 cm. I also find that quite comfortable even when I wake up in the middle of the night.
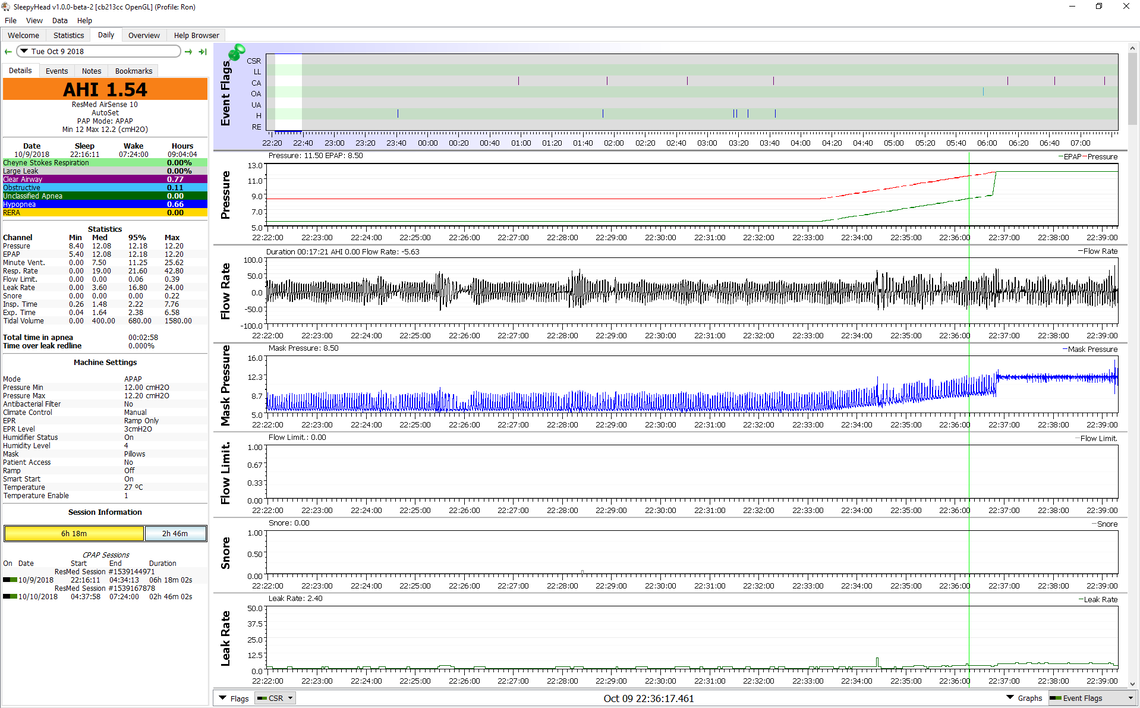
Here is what this looks like in SleepyHead. You can see that the pressure holds at 8.5 while cycling down to 5.4 (mask pressure) for about 11 minutes, and then ramps up over about the next 3-4 minutes, and then the EPR turns off. This varies of course from night to night depending on how fast I go to sleep. Just after 22:28 you can see a tiny blip on the snore chart. That is where I probably start to fall asleep. I frequently see that, but not always.
I do know that some machines, particularly autos send a pressure pulse down the tube to work out if an events is obstructive or central. This may be responsible for the "bouncing" you feel. Other than that, if EPR is turned off your pressure should remain constant. If you watch the display as you breathe, it should tell you of the pressure is fluctuating. Turning the machine off and on again, as you have described, is exactly what you are supposed to do if the pressure is to high. It will restart it a low pressure.
Hi am totally confused would love help. Auto set mode Pressure on 9 Max pressure 20 Min pressure 4 Ramp time 45 Start pressure 4 EPR set on 3
I have 5 different masks. The clinic just say don’t worry. No help at all
Should I change ramp from 45? To auto. What will that do. Also this EPR at 3 should I turn off
Regards
Rob
Hi Rob,
If you read the posts in this thread you will see there is no uniform opinion on the use of EPR. Over time I have changed my opinion on it too. While I initially thought there was some benefit in just turning it off, I now think that at least in some cases (like mine) it does have value.
First, what machine do you have? Since you use the term EPR and have an auto ramp setting, I assume it is an AirSense 10 AutoSet? If so I like to use the AutoRamp feature. It is not really a ramp, but is an initial pressure HOLD mode that keeps the pressure constant until you fall asleep. It has a Ramp Start Pressure that you can set to determine what the hold pressure is. I find that if you experiment with different settings you will find a hold pressure that is comfortable to go to sleep with. It needs to be high enough that it is comfortable to take deep breaths without it feeling like the machine is restricting the flow of air. I think 4 cm is way too low, and 7 cm is more reasonable. I have my machine set now at 9 cm for ramp start. It is a personal preference for comfort.
On EPR I used to use it set at 3 cm and Ramp Only. Then I would get the pressure relief for comfort, and when I go to sleep the EPR would shut off. In some there is an advantage to doing that. In others it may not. About the only way you can find out is to try it both ways to find out what works for you. What I found is that some EPR set at 2 cm makes a significant reduction in my hypopnea events. I also find that the OSCAR program which is free to download is very helpful in determining how the machine is working for me.
If you have any questions just ask,
I have resmed 10
I am totally confused with 4 different masks. The clinic is so unhelpful they have not got a clue.
I just changed ramp from 45 to 10. But might put it on auto
I changed start pressure from 4 to 5
So min pressure now 5 Max 20
But I just noticed on
It’s also set mode auto set
Just noticed on sleep report pressure used to say 9. Now it says 8.9 🤷🏻♂️
In regards the EPR it’s set on 3. But I watched a video of a guy on this machine he said it’s quite dangerous
https://m.youtube.com/watch?v=hw7D7G0aZI8&pp=QAFIAQ%3D%3D
Regards Rob
And changed
I don't think much of this LankyLefty guy and his youtube videos. He makes me wonder if he even uses a CPAP machine.
Using the EPR is certainly not dangerous, but it may not give you the optimum results. About all you can do is monitor your results with OSCAR with it (for a week or more) and without it. For me using EPR at 2 cm made a very significant reduction in my hypopnea events. However, if you are not having hypopnea events, then it may be worth while to set the machine up to use EPR on ramp only, and then it is off after your go to sleep. In some this allows the maximum pressure to be lower.
Depending on what you are getting for results I think a max of 20 may not be ideal. I find it best to limit maximum pressure to what is really needed to limit the occurrence of OA (obstructive) events. What is your breakdown of typical OA, CA, and H events, and your total AHI?
The display of the 8.9 must be a rounding issue. You can only set the A10 in increments of 0.2 cm.
I would set your machine to AutoRamp as I find it works quite well. However, a start pressure of 5 may still be a little low. But it is what you find comfortable.
Hi
I am not sure. I have changed everything back to what it was in settings. Just lay on bed with mask on for only 16 mins. And it come up with 18 minutes use and 6.6AHI. Normally if I had mask on but not alseep the AHI would be 0.0. Not sure what I have done wrong
The machine disables the recording of events while the ramp is in effect. However if the ramp is turned off then it records everything from the time the machine starts.
If you download OSCAR you can take the SD card out of the machine and view all of your data since day 1. The software requires a SD card reader and a PC or Mac.
If you go into the clinical menu you can set it to show an enhanced sleep record on your machine. Under Options, set Essentials to Plus. This will give you some more detail, but OSCAR is much better. See this link.
rob12345 said: "What mask do you use? What are your AHI normally. How long have you had Cpap. Do you feel fresh when you wake I feel tired"
Running out of width. I use a ResMed AirFit P10 nasal pillow mask, but I have modified the headgear on it. See this post. What masks have you tried?
I have had lots of trouble with central apnea events. Initially I was getting AHI's in the 7-8 range. Once I got pressures in a narrower range I got the AHI down to about 3. Next switched my machine (AirSense 10 AutoSet) to a fixed pressure CPAP mode with EPR set to Ramp Only. This brought my AHI down to about 2.1. My next change was to turn the EPR back on with it set at 2 cm full time. AHI came down to 0.85 or so.
I do feel reasonably fresh when I get up providing I get about 7.5 hours of sleep. But, that said I never really did feel that apnea affected my sleep a lot. It certainly did make me snore and disturb my wife though.
But, each person is a bit different. The starting point is to figure out what your main issues are. Having no, or minimal central apnea makes it easier. Mixed central and obstructive apnea is much more difficult.