Update: It turned out that the first home sleep study wrongly indicated a dominance of central sleep apnea. In fact, a second home sleep study and the lab sleep study showed almost exclusively obstructive sleep apnea, whereas the second home sleep study showed only mild OSA while the lab sleep study showed moderate OSA. As you notice from the thread, the responses and answers move away from the CSA topic to my general experience on this journey.
Hi, This is my first post here. First, thank you for your patience and understanding.
Why I am writing I was just this week pre-"diagnosed" with mild mixed sleep apnea and I am supposed to get a sleep study in the lab. However, that is here in Canada (yay universal health care) at least 6 months out. Currently, I have a very hard time to deal with the potential outcomes, especially the implications of the central sleep apnea which, based on my internet research, first and foremost means there is an issue within the brain often caused by something else (more severe). Yes, I am also the kind of person which over-evaluates negative/worst outcomes.
Backup Information The respitatorist, with a tremendous lack of sensitivity, told me the machine used for the home study indicates mixed sleep apnea and for him the concerning part is the central sleep apnea portion of the mixed sleep apnea. Hence he is requesting a sleep study in the lab. I was so shocked, I didn't get the results written down. However, I am picking up another home study device this weekend from another place to do another home test.
About me I am 33 years old, male, BMI alright. My symptoms are waking up 4-6 times in a night, tiredness during the day and maybe moodiness. All the questions from the respitatorist (i.e. opioids, headaches waking up, strokes, head traumas, restless leg, heart disease) I was able to answer with no. The only other thing I have is mild GERD and a speech disorder since I was able to speak (stuttering - however I am able to manage it most time). Doing a sleep study only came up when my allergy test results (mild to dust milds) were not reason enough for the allergy doctor to conclude the allergies are causing my tiredness and waking up.
Where you can help me with (maybe, hopefully?) How concerned should I be regarding the central sleep apnea? I was expecting to hear that I need a CPAP, but hearing that my brain forgets to send signals to my lungs to breath was a bombshell and I am still shell-shocked.... Since I never had a stroke or not doing drugs, should I be very concerned about a brain tumor or any other brain illness or even a heart disease? Because from my research for CSA, those are the primary reason for that. If so, why didn't I get a referral for an MRI to rule out anything in the brain or already existing damage? Why do I have wait first 6 months for a lab sleep study? Should I insist for an MRI? Because if there is something wrong in the brain, then 6 months are a very long time and things might get worse and are curable. (yes I am panicking).
I hope you see with what I am struggling with. I know that you are not doctors and I don't expect a diagnosis. But maybe you can give me some feedback to interpret the CSA.
I am from Canada and understand what you are dealing with to some degree. I have had the home sleep study and the results indicated a small degree of central apnea. My results:
Type - Index (#/hr)
Central - 0.4
Obstructive - 17.4
Mixed - 0.7
Hypopneas - 18.8
Total - 37.3
That puts me in the severe classification (AHI > 30)
My issue has been that Auto CPAP treatment has significantly reduced the Obstructive apneas, and Hypopneas, but the Central apneas have increased. Under treatment my total AHI is about 3 with the largest portion being central, then hypopneas, and lowest are the obstructives. The hypopneas are probably partial centrals, so Centrals is likely a little understated. This said one is considered to be adequately treated if AHI is under 5.
To access your situation you need to get these kind of numbers. Ask your sleep test provider to e-mail them to you. They probably have them electronically already, or can scan them. If they won't, then ask your referring doctor to provide them. I don't believe they can refuse you, and you deserve to see the results.
When you get the results then you can start to assess the seriousness of your condition. It may not be bad at all. If you can post your numbers then I certainly will comment on them. I am not a doctor, but as centrals have been an issue for me, I have done a bit of research on it. If you have obstructive apnea to be treated, there is only so much a standard Auto CPAP can do. A BiPAP machine can do a little more, but not much. The ASV or ventilator machine can do more, but they would probably only be used if there were no other options to treat the underlying conditions.
Short story. Insist on getting a copy of the sleep report; both the first one and the second one. Do you know the name of the machine you used? ResMed make one called ApneaLinkAir, and Phillips make one called Alice NightOne. I had my test done with the NightOne. The link below is to the product brochure for the ResMed machine. See page 4 for an example of what the sleep report from it looks like. That is the report you want to get. There should also be a professional evaluation of the results and their comments should be included as well.
Thank you very much for the response, it means a lot to me, Sierra! I requested the results to be sent to my family doctor; they wouldn't give it out by email.
Unfortunately, I didn't remember the name of the device. Although, it definitely looks more like the ApneaLinkAir than the philips device (it was grey/black with 2xAA batteries, similar pouch, but it had only one led light). I only got a glimps of the chart, but I think it was something like the chart which you see in the ApneaLinkAir manual
I have been dealing with this at least for a long time now (feeling tired throughout the day, waking up during the nights, not feeling rested the next morning); even if it indicates "mild" I am totally exhausted at this point and my ability to focus is diminishing. Like today at work, I feel more like a zombie starring at the Excel sheets. For a while now I thought I might be bored by the work, but I start thinking the lack of interest in my work can be at least concluded by the lack of ability to focus on it (I wasn't like that always; especially during university I was able to focus for very long periods)
May I ask; how do you feel overall? Did it improve again your life quality?
Sounds like they are playing a little difficult with the sleep report. I would suggest you make an appointment with your doctor, ask to see the report, ask for his/her opinion as to what it means, and also ask for a copy.
My wife and I are now both on a CPAP. She was diagnosed nearly 4 years ago in the high severe range - around 80 I think. When she went on the machine she noticed an immediate benefit, and has used it every night since getting it. I was tested after I failed a screening test and then failed the sleep test with an AHI in the lower severe range - 37. I had no trouble sleeping before the machine, and did not suffer from any extreme sleepiness. So I did not see an obvious step change. Now after 6 months I am seeing more benefit. My wife's apnea is essentially all obstructive apnea and she averages about 1.0 for AHI under treatment. I am doing well to get under 3.0 due to my higher portion of central apnea. My wife also appreciates that I no longer snore too!
I did a quick check on BC's health care treatment of apnea. It is better than Alberta. We have to pay for our machines out of our pocket if we do not have private insurance plans that pay for it. I see in BC that if the severity is moderate (AHI 15-30) or severe (AHI >30) it looks like they pay. But, you may be on your own for cost if mild (5-15). We had to pay for our machines, and there is a wide variation in what they cost depending on where you get them. I can help you out with some suggestions on where to go for a better price if it comes to that.
In any case step one is to get your sleep report(s). That will provide a lot of guidance on what you are up against, and what your options may be. There are at least 5 different types of central apnea, and various types of treatment methods depending on the type you have. Here is a short report on it, if you have not seen it before.
Oh and the other important part of the sleep study report is the oxygen desaturation levels. The problem is not really that we stop breathing, it is that oxygen levels go down when we stop. That causes the problems. The report should say to what degree that is a problem for you.
Hope that helps some,
Don't get to worked up. Just because and event is scored as "mixed" on a diagnostic study doesn't mean that you have central apnoea. It is not really possible to tell with any great certainty whether someone has central or obstructive apnoea on a diagnostic study, especially a cut down home study of the type I suspect you had. The rules for classifying whether an event is obstructive or central are purely based on how it looks, and just because an event looks central doesn't mean it is. So you may not even have central apnoea.
Even if you do have central apnoea, it doesn't mean that something is wrong with your brain. I have had hundreds (probably thousands) of patients with central apnoea and almost none of them had anything wrong with their brain (beyond having central apnoea if you want to be picky). It is not usually an indicator of anything more insidious. Just take things a step at a time and deal with what's in front of you. Some more detail on your results would be quite useful.
Thank you very much for your kind words. I see what you mean; it is not really an exact science.
Since you are working in the field, do you often meet people with a previous history of speech disorder as a child? In my case, I was stuttering since the beginning and I was sent to speech therapy. That helped to some matter, but got worse again in puberty. Now, it is less often the case, but still existing. I am wondering if the "wrong" wiring in my brain contributes to sleep apnea, since there was a study in 2002 suggesting that: https://www.sciencedaily.com/releases/2002/11/021121065148.htm However, I haven't heard of a follow-up of that study or further evidence.
So I did another home test from a private sleep clinic with a ResMed ApneaAir Link device. I hope I get the results of my first home test tomorrow and those from the 2nd home test even today or in the next couple of days.
Is there a reason not to start with a CPAP device based on the home test if the respirologist wants a in-lab sleep study? I.e. is there a case a CPAP would make any other condition worse?
If you post your sleep test results I can give a much better response when the degree and type of apnea is detailed.
In Alberta it is normal practice to do a free in home trial of the CPAP as a first step. That will quickly confirm a few things. One is how much pressure you need, and that a standard APAP is suitable. The other is more data on the breakdown of your apnea events, and the degree to which an APAP can normalize the breathing. There is no reason not to do that that I know of. In some cases treatment can increase the frequency of central apnea but it is most often temporary. Again that will be quickly determined by your machine. If you get a good APAP like the ResMed AirSense 10 AutoSet, it will wirelessly send your data to your provider and they can monitor each night. You can also monitor it with SleepyHead software, which I would advise. I would ask about doing a free trial.
The only issue I can think of may be your BC Heathcare system. From what I can see they cover the cost of the machine if your AHI indicates moderate or severe. If mild you may be on your own. Perhaps your results are not bad enough to qualify for a free machine, and the clinic doing the testing is trying to help you if the test results are only in the high mild category. Just guessing.
But like I say, your test results will be very telling as to where you stand now, and what next would be advisable. When you see your provider, be sure to ask about a free at home trial of a machine. And if there is a choice I would ask for the ResMed AirSense 10 AutoSet. Second choice would be a Respironics DreamStation Auto.
So I had a difficult discussion with my family doctor. I wasn't given the result, but only said normally those devices don't pick up central apnea easily. The fact that it picked up central apnea means it must be investigated according her.
From the 2nd home study I know from the technician from the phone AHI 4 and ODI 6.8. Knowing that up to 5 (AhI) is normal doesn't make sense bc I have been having daytime fatigue and drowsiness all day each day for the last 3 weeks.
So I guess something else must affect my health? Bc you guys suffer from higher AHI values.
Upon the lab study,my family doctor is not willing to prescribe a cpap but I have to do a brain MRI instead. Particularly bc I mentiined
It's not allergies, either.
I'm not sure your family doctor is correct about the devices not picking up central apnea. My test with the Phillips Alice NightOne certainly picked central apnea up. But that said, your first test result was mild mixed apnea. Mild does indicate an AHI over 5 and less than 15. Your second test was an AHI of 4, which is in the normal category. I would say this indicates you do not have an apnea condition that requires urgent attention, and the full in lab test is probably being very cautious, even with a wait of 6 months.
The AHI of 5 being normal thing is a rough guide, not an absolute rule. It is possible to have an AHI < 5 and still suffer significant symptoms in terms of tiredness, low energy levels, poor memory etc. Different people are different. The usual practice is to give CPAP a try and see if that helps. However, it may also be something else that it causing your problems.
I will have a lab sleep-study on Thursday night. Just got the call; I guess someone cancelled (because cancellation policy is 48h and this is less than 48h). Or it is that urgent... Or maybe it is because it is far out from Metro Vancouver and no one wants to go there.
That sounds good. You should get a very good indication from an overnight study as to where you stand with the degree and type of apnea you have (or don't have!).
This time I would insist on a copy of the written report of the study findings. It is your right to get it. It is also your right to get copies of the two at home studies you have already had. See the link below and this excerpt from it.
"Enduring Access Are physicians required to give patients access to or copies of their medical records? Patients own the information in their medical records, as affirmed by the Supreme Court of Canada in its decision in McInerney v. MacDonald in 1992. Subject to bullet point 3, patients are entitled to examine and receive a complete copy of their medical record, which includes any records created by other physicians, and this access must be provided to the patient upon request (usually within 30 business days). The duty to provide a patient with access to the record may vary according to the applicable law, any relevant agreement with a third party and the consent of the individual. Physicians must ensure that they know the applicable legislation and rules with respect to a patient’s right of access. Physicians are encouraged to seek the guidance of the CMPA, or their legal counsel, if unsure about how to respond to a request for access. Section 29 of the Personal Information Protection Act (PIPA) states that a physician must generally respond to a patient’s request for that information within 30 business days."
You also may want to prepare yourself for a diagnosis of Mild Apnea. In Alberta CPAP treatment is considered the gold standard for mild apnea, but a dental appliance may be an option. They tend to be quite expensive if not covered by insurance. As I understand it BC Health does not cover the cost of a CPAP if you are in the Mild category (AHI 5-15). They only cover for Moderate (AHI 15-30), or severe (>30). If in this category, I would inquire about options to do a CPAP trial.
I am a dentist working in dental sleep medicine. Oral sleep apnea appliances have been around twenty or more years now. Given that length of time, they have been extensively tested and we now have a large body of test data about their efficacy. Actually, they have been found to be quite effective in treating both mild and moderate sleep apnea and are considered a first line treatment for both, as well as CPAP. I believe that many of the same oral appliances found in the USA are also available in Canada. A MyTap appliance can be had in the USA for about $650(US) and is quite effective. However, it is not very strong or long-lasting. It does make a great starter appliance for someone trying to see it the concept works for them. Please understand though, that these work only for obstructive sleep apnea and not for central sleep apnea. Arthur B. Luisi, Jr., D.m.d.
Thank you for the feedback. I had my lab sleep study just yesterday/tonight.
Now it is waiting for the results. Luckily I got sleeping pills prescribed for 2 weeks. I still notice that I wake up (now I even notice I do a gasping), but the brain fog is gone for now and I am able to focus again.
After talking to the technician I learned that the sleep lap at the University of British Columbia (Vancouver) only has 6 beds tops and they do sleep studies only so many days in a week. On the other hand, you have a dedicated sleep lab at the Abbotsford Regional Hospital with up to 9 beds and open 6 or 7 days a week. I am surprised that there are not bigger sleep lab facilities in the gentrified areas with most inhabitants (Vancouver area), because Abbotsford is 90km away from Vancouver and it is pretty much impossible to get there with transit.
I read an article at CBC on line about a University professor in Nova Scotia that is also a pharmacist. He (or more likely his grad students) has developed a website to provide resources to address insomnia and getting a good night's sleep without or with minimal medication. His view is that too many sleep aid medications are used, and they in turn are causing falls in seniors which cost the healthcare system a lot of money. He promotes the use of CBTi, or cognitive behavioural therapy for insomnia. It is a very good website, and I have gotten quite a bit out of it. There are a number of tools to evaluate your sleeping beliefs and habits. Check out the CBTi tab in particular. Here is the link:
Still waiting for the results of the sleep study in the lab. When I was spiraling, I did a 2nd home study using the device from a sleep clinics (those which throw CPAPs devices after you). My family doctor got those results as well; however this time it indicated only mild obstructive sleep apnea, nothing from CSA.
Actually, being on zopiclone (prescribed) and my previous PPI (proton pump inhibitor) for some days gave me some relief on some days (although I still don't get a restful night and I still wake up).
Anyways, waiting for the lab sleep study is the current course of action. Luckily, I was also able to get an MRI done (in an incredible short period for the public health system), results pending as well. Reason for that was to rule out organic stuff and since I brought up a study where an over proportional amount of adults with sleep apnea had speech disorders as children (which I still have) due to some wrong wiring in the brain respectively gray matter development.
So I got a brief email from the lung doctor that the lab sleep study shows "only" obstructive sleep apnea and I need a CPAP. I will see him next week.
Since my insurance pays to a certain amount a machine once in 5 years; for which ResMed model should I go for? If I have the choice, should I go for a APAP instead of a plain CPAP from Resmed? Does an APAP provide more data than a CPAP? Is an APAP machine basically a more modern BiPAP machine? Or can I run an APAP as CPAP or BiPAP?
Before I get the machine, I will have to do a split study or how would I find the right settings? I know these are questions for the lung doctor, but I want to be prepared when I meet him because it always takes forever to get an appointment.
I would strongly advise an Auto CPAP or APAP. Yes, you likely could get away with a fixed pressure CPAP but it is going to be more difficult to get setup properly, and the difference in price is quite small. When a fixed CPAP is prescribed it is usually after an in lab titration study to determine what pressure it should be set up. With an APAP you really do not need the titration study. The machine is just set with a fairly wide pressure range and then tweaked after you gain some experience with it. SleepyHead software would be very helpful if you are going to do the setup yourself.
The machine I would recommend would be the ResMed AirSense 10 AutoSet For Her. I would suggest the For Her version even if you are male. It has an extra setup mode that can be used or not used at your choice. Ask your sleep doctor about the need for a BiLevel machine. But, unless you need pressures of more than 20 cm it would not be necessary. My recollection is that your diagnosis was likely in mild apnea zone, and should not need high pressure to treat.
Here is a link to a package from a Toronto company that I bought from. They are pretty good to deal with. They will require a prescription if you decide to order from them. This package includes all you need to get started including a choice of a few different masks. I use the ResMed AirFit P10 and find it quite comfortable. Ideally you would want to try one before buying, but if that is not an option, I would suggest that one.
ResMed AirSense 10 AutoSet For Her Package
Hope that helps some,
If the process is to be done as best it can be, an in-lab titration study will have them hook you up to a machine and fiddle with the settings as you sleep and monitor how you react. Don't worry about which type machine is prescribed as that will be a function of the study. A straight CPAP machine costs a LOT less than other types of machines and that is what will be prescribed if one is called for. If you need a machine with more complicated function, that will be prescribed. Some durable medical equipment companies are ResMed places and some carry other brands so the choice really will be the result of the process and DME company chosen.
George, the prices of machines probably vary by country. However in Canada where the original poster is from the price difference between a CPAP and APAP is very small. The ResMed AirSense Elite (fixed CPAP) sells for $850, while the ResMed AirSense Autoset (APAP) sells for $880 Canadian. It makes no sense to get the CPAP machine. The APAP can be easily set to act like a CPAP if you want to as well.
I may have skipped over some of your questions.
"Does an APAP provide more data than a CPAP? Is an APAP machine basically a more modern BiPAP machine? Or can I run an APAP as CPAP or BiPAP?"
Yes, in some machines the fixed pressure CPAP does not store detailed data. I would not accept any machine that is not able to supply detailed data to the SleepyHead application. The ResMed AutoSet certainly does store all the data and is compatible with SleepyHead.
Both the APAP and BiPAP or BiLevel machines are state of the art design. There may be a few refinements on the current AirSense 10 (APAP) that are not on the current AirCurve 10 (BiLevel). But the BiLevel machine will also have some features that the APAP does not have. The main one is that the BiLevel will go up to 25 cm pressure instead of 20 cm. It can also provide up to 10 cm differential between inhale and exhale (pressure support). The APAP is limited to 3 cm differential. The BiLevel also has some adjustments on how it switches from inhale to exhale. Discuss this with your doctor, but I would suggest these are all moot points for you, as you are very unlikely to need very much pressure, and no where near 20 cm with a mild obstructive apnea. And it is usually better to run no differential between inhale and exhale, except during the going to sleep ramp up period.
You can run both the APAP and BiLevel (ResMed machines) in CPAP mode. Pressures are limited to 20 cm in CPAP mode. You can't run an APAP as a BiLevel as it does not have enough pressure. You can make a BiLevel behave pretty much like an APAP, but it is more complex to set it up to do that.
I think what you may be asking about is if you should get a BiLevel given that you may only get one shot at a machine each 5 years with your insurance company? First, I suspect that your doctor may not be willing to write a prescription for one if you only have mild obstructive apnea. And there may be a bit of a compromise in your comfort by using a BiLevel. For example I don't think it has the ramp only feature on the pressure differential between inhale and exhale. The APAP does.
Another thing to consider is what can you negotiate with the Insurance company. My son had a fairly generous insurance plan when he was prescribed an APAP. He talked direct to the insurance company and was able to negotiate getting two machines covered. The sleep clinic were offering the single APAP for $2400, but an on line store was offering the same APAP plus a travel APAP for less than $2000 total. The insurance company paid it. The other possibility is if you buy at a lower price and don't use up your maximum allowance, will they let you buy an updated machine in 3 years instead of 5 years?
Hope that helps some,
At the sleep clinic, I got a Philips Dreamstation with a Resmed Airfit N20 small nasal mask. I tried a nasal pillow in office, but it felt like as if my nostrils would be blown up and the resistance while breathing out felt like someone would try to suffocate me....
So I am only on 5cm with down to 4cm at ramp.
The first night was weird. I hope by sharing some impressions you can tell me if you experienced similar things.
On the good note, I had more absolute REM sleep time (+20min) according my Fitbit Charge 2 than ever in the last 4 weeks (even on zopiclone in that period); even when I slept longer in the last 4 weeks. I do not feel withdrawal symptoms from zopiclone. Last week, I tried 2 nights without zopiclone and it was brutal. I thought it might be withdrawal symptoms but now I think it might have been my regular symptoms of the apnea.
For the first time in a long time, I had nightmares. I got out of the nightmare when my wife closed my jaw since I was leaking air through my mouth (I woke up). I read somewhere that using for the first time CPAP could induce wild dreams; however I did not read that as nightmares.
At some point I woke up with a hot flush all over my body. I never had that before when sleeping. I had set the humidifier to 3 and the hose heat to 2. Could the warm air of the humidifier be the reason for that?
At some point I woke up feeling like a stuffed turkey; I assume air made it to my stomach. Is this normal or a common side effect of CPAP? Or is this something that needs to be addressed.
Later in the night I woke up due to the pressure of the mask. I guess it will take more time to get used to it or I have to change the mask.
EDIT: My dreamstation comes with cellular/wireless reporting to the therapist. Is there a way I can access the data with sleephead without her knowing that I also do my own research? Can I just remove the SD card and read it or will it report to the therapist that I am accessing it? I am asking because I know some specialist get cranky when you try to be your own specialist.
Some comments:
The DreamStation is a good machine, but if you have any choice in the matter, I believe the ResMed AirSense 10 AutoSet is a better machine. I like the way it automatically adjusts pressure better, and it has some ramp and EPR features the DreamStation does not have. But, it can do the job and many use it quite successfully. What I like on the ResMed is the Auto Ramp feature and the ability to use the EPR during the ramp hold period and then shut it off automatically when you go to sleep. I don't believe the DreamStation has the ability to do that. These features make it more comfortable to go to sleep and more effective in the treatment after you go to sleep. DreamStation use something called Flex which is similar to EPR but not as effective in my opinion.
I'm not clear what you mean with your pressures. There should be a minimum and maximum treatment pressure, and a ramp start pressure. Your ramp start is 4 cm? Minimum 5 cm? and Maximum ?? These are very low, and have the potential to be uncomfortable and feel somewhat suffocating.
There should be no functional difference between a nasal pillow mask and a plain nasal mask. They both feed air through your nose, and require you to keep your mouth closed while sleeping. I prefer the nasal pillow as it lets me scratch my nose during the night if it feels itchy, feels less confining, and has less contact on my face.
I think the issue on dreaming/nightmares is that if you wake up during them, you will remember it. If you do not wake up you will still have them, but will not remember them. So if anything it is an indication of how frequently you wake up.
I'm diabetic and if I have a hot flash during the night is is most often a sign of low blood sugar. Other than that, I have not experienced them. I do find sleep quality is affected negatively by a higher room temperature and/or too many covers.
If you want to stay with a nasal or nasal pillow mask, you will have to address the mouth leakage issue. You will wake up with a sore throat, and treatment may be compromised. Some learn to do it. Some report that it helps to keep your tongue on the top of your mouth and pressed up against the the back of your top teeth. The issue is still doing it when you are sleeping. I have resorted to using a Breathewear Halo chin strap. Sleep Yeti in Calgary have them for $25 plus $7 shipping. I have also found it necessary to use a 1" Nexcare Paper Medical Tape (from Walmart) to keep my mouth closed. Sounds awful, but it isn't really that bad.
Swallowing air can be an issue, but I think it is more of a problem with a full face mask. Suspect it may go away when you can learn or stop the mouth opening.
If you use a ramp start and wake up during the night, you will likely notice the higher pressure during the night. I find higher pressure only really wakes me up when the mask is leaking and for example blowing air into my eyes. Suspect it is not just the pressure that wakes you up. Do you know what pressure the machine is going up to?
I'm sure they will not know if you have taken the SD card out and copied the data to SleepyHead. It will transmit data briefly when you shut the machine off in the morning. If you change settings on the machine they may or may not notice. When I did my sleep test with a F&P SleepStyle machine it was not compatible with SleepyHead, so I switched it with my wife's ResMed S9 machine so I could see my data in SleepyHead. I then changed some settings in the F&P machine and started using it again. They never noticed that my wife used it one night, or that I changed settings. Or, at least did not mention it.
Is this just a trial machine, or have you (or your insurance company) bought it? At some point when you do own it, it is important to remember that it is your machine and your treatment, not theirs. It is good to involve the sleep specialist if they are cooperative. The more common issue is that they are not nearly as interested in your treatment as you are.
I would highly recommend loading your data into SleepyHead. That way you will see what the machine is really doing, and how effective it is.
Hope that helps some. Any questions, just ask. Regardless it takes some time to get used to sleeping with a mask on. But I'm sure you can do it with some perseverance.
Hi Sierra,
It is always nice to hear from you!
The therapist gave me the Dreamstation for trial because she said it has the better diagnostic tools for therapists. She said if I continue after the trial period I could choose the Resmed 10.
Regarding the pressure: I am reading the start pressure at the beginning when I am awake. The big ramp button lowers the pressure from 5 to 4. I don't know what the therapist set as minimum or maximum. I will take a picture later. At this point, I cannot speak for the pressure during the night. The next time I wake up I will have a look.
Thanks again!
It may be possible that the therapist has software that gives her better detail from the DreamStation. They typically use proprietary software from the manufacturer that is not legally available to us as users. SleepyHead is legal and free. In my experience looking at the SleepyHead reports from each, there is actually more information from the ResMed. The ResMed displays both set pressure and mask pressure. The set pressure is what the machine is being asked to deliver, and the mask pressure is what the machine actually does. The DreamStation only seems to give access to the set pressure. ResMed also gives a continuous flow limitation signal which can be graphed. DreamStation on the other hand seems to treat a flow limitation as an event rather than a continuous variable.
What I don't like about the DreamStation is how it automatically set the pressure. Some describe it as a "hunt and peck" strategy like a chicken pecking at the dirt on a repeated basis and mainly only finding dirt, but every once in a while finds something to eat. DreamStation apparently uses this technique to periodically increase pressure to see if anything gets better. If nothing gets better, then it then lower the pressure again. It does this all night. To the user having this pressure fluctuating up and down all night has to be annoying, and the machine is usually accomplishing nothing by doing it. The other difference is that the DreamStation seems to be slow to increase pressure, and needs more events to get the pressure up to an effective level.
And on the ramp feature I like the ability the ResMed has to only apply the EPR during the ramp and then turn it off when it detects you are asleep.
Those are some of the reasons I would choose a ResMed over the Respironics Dreamstation.
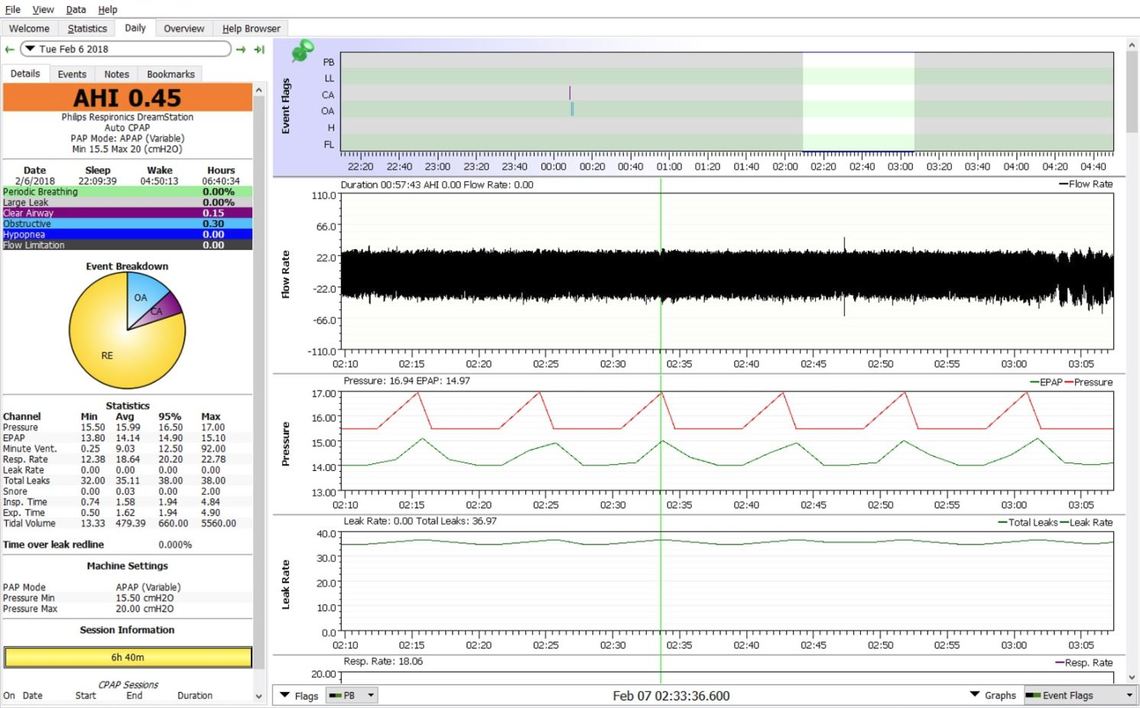
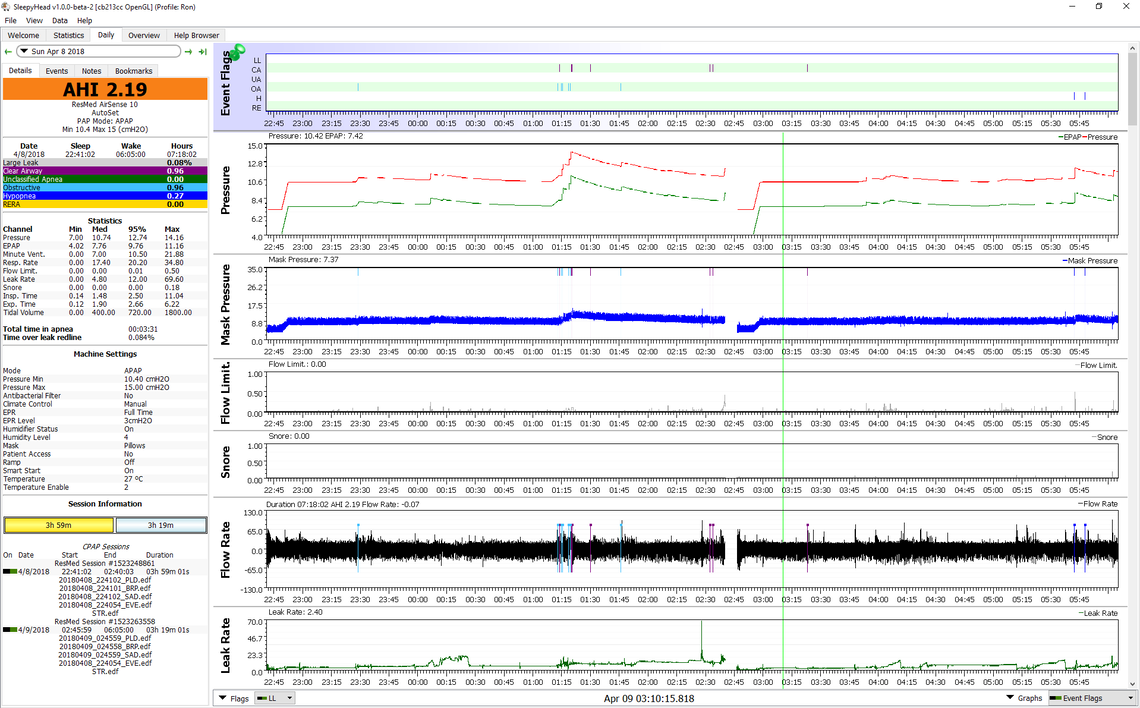
Here is an example of what the DreamStation does during the night. Take note of the red inhale pressure trace. You can almost set your watch by the ramp up in pressure every 10 minutes or so, while from the events flagging area, nothing is happening. It just does it. If you load your data into SleepyHead you probably will see something similar. For sure you will be able to see that the maximum pressures are. Below that is one of my ResMed reports when I had a wider pressure range set and you can see how it responds differently. In comparison the ResMed leaves things alone when there are no events, raises the pressure quickly when they occur, and then ramps down slowly after they occur in anticipation of more events.
DreamStation
ResMed AirSense 10
I think I mentioned it before, but if you do decide to go with the ResMed, be sure to ask about the "For Her" version of it. It is the same price, and does all the same things as the standard AirSense 10 AutoSet, but it offers an optional extra program that can be tried to see if it gives you better results. It is more suited to someone who may be using pressures in the lower range (<12 cm).
I have now Sleepy Head installed and I have 3 days of data available. I am still learning how to interpret it. I wanted to upload a screenshot, but somehow I don't see a function in this forum to upload images. In the reply field, I only have the option for bold, italic, link and quotes.
Here are some instructions assuming a PC is used. A Mac should be similar but with the Apple equivalents.
First the most important screen is the Daily Tab, but it has some clutter that should be cleared to make the most of the screen space. Especially here the image seems to get squashed down quite a bit. In the Daily Tab screen the F10 key turns the right menu bar on and off. Turn it off. Beside the current date in the top left is a little triangle. Use it to turn the full month calendar on and off. Turn it off. Then under File, Preferences, Appearance, uncheck the box that displays the event breakdown pie chart. It takes up too much room and displaces other important info. In the graph portion I like to keep the Event bar pinned, and then under that Pressure, Flow Rate, Mask Pressure, Flow Limitations, Snore, and Leak Rate. You can click on the left hand scale and drag them up and down to change the order. Clicking and dragging on the grey dividing bars lets you scrunch them down or expand them.
When you have the layout optimized, then maximize the window to full screen, and just press F12. This will save an image file to the Documents/SleepyHeadData/Screenshots directory. Use Windows File Explorer to display this file directory. Left click and drag the saved file to the body of a message here. The site uploads it and saves it here.
Hope that helps,
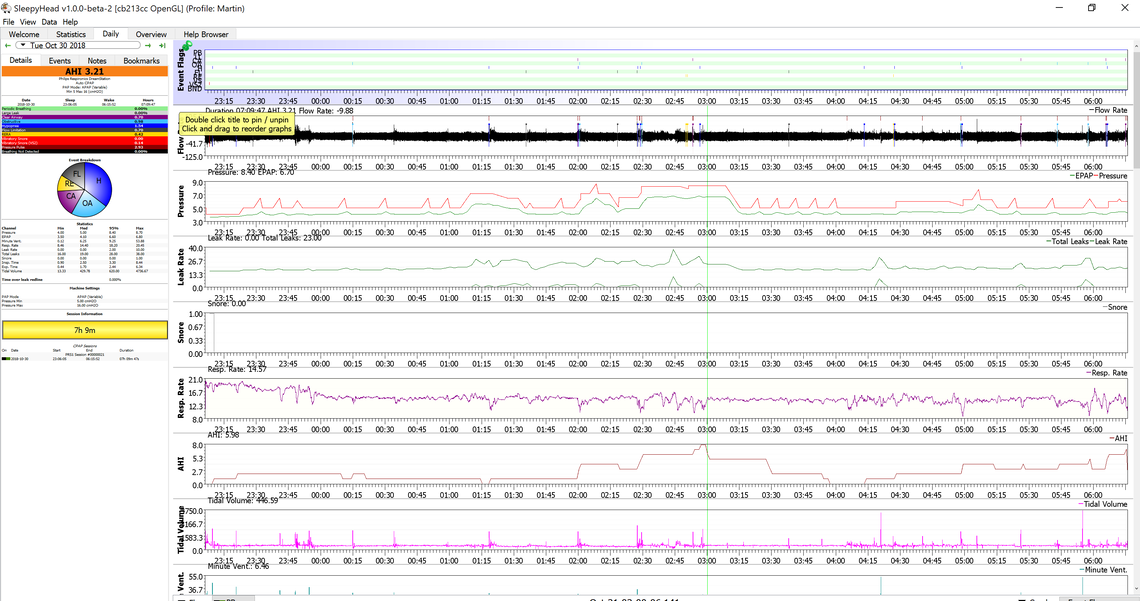
Could someone give me a rough interpretation how I am doing?
I already had contact with my therapist which receives the data through the modem. My concern of leaking air was played down respectively she thinks the data doesn't show that as concern. However, shouldn't I do better with an APAP that AHI of 5.35? In some nights?
My sleep is still very fragmented; I still wake up as before the treatment approx the first time 2.5 - 3 hours after going to bed and then every other hour. So far, my daytime symptoms are much better, but my sleep is still as bad as before. Not to complain, just a reflection.
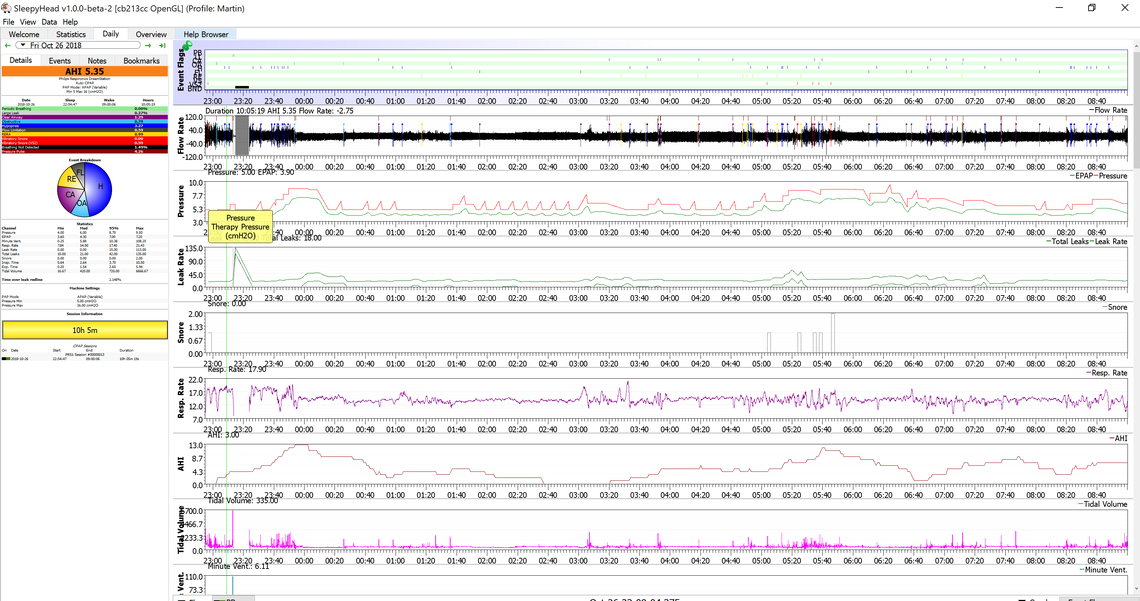
I think you are doing pretty good, considering that you are just starting with CPAP treatment. And yes the goal in CPAP treatment is to get AHI below 5.0 and lower is generally better.
Major leaks should be flagged with an area grayed out like the portion near the beginning of your sleep. Perhaps the mask was removed for a short period of time? The rest of the area does not look too bad. At the left hand side bar at the bottom of the Statistics section there should be a time over the leak redline. I like to see that under 1%.
I think your machine setup could be improved for comfort and effectiveness. The minimum pressure appears to be about 5.5. I would suggest that it should be a bit higher at 6.5 or 7 cm. The graphs are also indicating that some degree of Flex (possibly called A-Flex) is turned on. It reduces pressure on exhale. While this can be a small comfort benefit it also can affect effectiveness negatively. I would suggest turning it off or to 0. That is one nice feature of the ResMed A10. You can set it to use the pressure reduction on the going to sleep ramp portion only, and have it turn off automatically when you go to sleep. That way you get the comfort effect while going to sleep and the improved effectiveness when sleeping. Depending on how the machine is set up you may be able to turn Flex off yourself. The minimum pressure change will require going into the provider menu. You probably want to discuss the two changes with your provider and ask if they will change them. The effect of these two changes would be to keep the pressure more constant during the night, avoid some of the events which are happening at the lower pressure, and potentially reduce the maximum pressure that the machine is going to.
You have a very good layout of your SleepyHead daily report except that I can't read the text and I have a large screen computer. I just had a birthday and perhaps my vision has gone past the "best before" date! I would suggest a couple of changes. If you mouse over to just right of the left sidebar the cursor should change to the double bar. Click and drag right to make the left sidebar wider. Then go into File, Preferences, Appearance tab. There is an application data font size there that can be changed. Try 12 points or whatever works. When you are in there also uncheck the show pie chart event breakdown. The pie chart is not necessary once you make the sidebar and fonts large enough that one can read the colored bars that list the events and the frequency of each. last you do not need to display as many of the graphs. They are scrunched down quite a bit. The Events Flags and others are hard to read. Again click on the gray bar between the graphs and drag them down to make the Events Flags, Flow Rate, Pressure, Leaks and Snore bigger. The rest of the stuff is less important and let them scroll off the bottom as necessary. You can always scroll down to look at them if you want.
Last, I think you went into this knowing that there may be some central apnea issues, and your one chart does show it is a bit of a problem. Hypopneas are your highest portion, and I have concluded that hypopneas are actually incomplete obstructive OR central apneas. They have just not progressed to full stoppage of air flow. So your current hypopnea index could be a mixture of obstructive and central issues, and if you look at the central apnea it may be a bit understated. I believe that is the case with my results. I do not always get under and AHI of 5, and if I don't the main problem will be central apneas and hypopneas.
Hope that helps some,
Thank you very much for the detailed feedback!
I will adjust my screen accordingly. My laptop is a 4K screen and it seems the software is not scaling well with high resolution screens.
Regarding your interpretation of hypopneas being incomplete OSA; my last night's statistic show a bigger amount of OSA taken from the hypoapneas part.
Are hypopneas preferable over actual OSA or CSA?
Do you think the sleep therapists will be annoyed when I bring printouts of the daily statistics from sleepy head, which is not an official tool? Don't want to hurt their feelings :-)
I thought there must be something different about your computer. I have looked at many SleepyHead posts but never seen one so scrunched down in size. I think if you drag the bar width over and increase the font sizes significantly you will be able to make it readable. It also helps a lot to use the Write a Reply button near the bottom when you are going to post a screenshot. Then you at least get the full width here rather than the narrower and narrower window.
I can't really read the second screen you posted, but yes it appears there is more OA. I have found the most effective way to reduce OA is to increase the minimum pressure. It is far more effective than increasing the maximum pressure. And as I say setting the Flex to 0 should help some too.
Yes, I would say hypopneas are preferable to full apneas, but they seem to get the same weight in the AHI. I believe there is some dispute in the industry on whether or not the AHI as a result is as good a measure as it should be.
One issue with hypopneas is that I believe both the DreamStation and AirSense machines will respond to them with more pressure. If they are really a partial central apnea without flow restriction, then that is not appropriate, as more pressure will not help. At some point down the road you may find you have to restrict maximum pressure so the machine does not unnecessarily increase it. I do that on both my wife's machine and my own.
It will depend on the sleep therapist how they react. About 4 years ago when my wife got diagnosed we ended up buying her S9 machine on line. The clinic that sold the machine at that time offered some setup and follow up as part of the service. The technician told me about SleepyHead and helped me use it to set up my wife's machine. The S9 does not allow wireless monitoring or setup. Your technician may not be so cooperative. In theory they should have Phillips software that does basically the same thing as SleepyHead, and they should have the same data as you are seeing on SleepyHead. So again in theory they should be looking at the detailed results like you are with SleepyHead. But, that is where I think it breaks down sometimes. They often only look at the summary data and don't want to be bothered by the detail. Often they only look at two things: how many hours per night is the machine being used (Compliance), and what the AHI is. And if they see 5 hours or more, and an AHI of 5 or less, they can say "you are treated", and technically they are correct.
If you have been talking to them by phone I would just ask about making the two changes I suggested. They should be able to do it wirelessly. And, you will quickly find out how receptive they are to user input. Some are good with it, and some not so much.