Hello - I'm using a ResMed CFlex+ and am trying a variety masks. No matter what mask I use, what settings I use (changing pressure, CFlex setting) I just can't push against the pressure to exhale. It feels like the air is just backing up...which it is...and I have to exhale through my mouth. At the tail end of my last sleep study (June '18) they fitted me with a nasal mask (sorry, I'm just too tired to check the make/model) and I seemed to do fine with it. Two nights later I suddenly just couldn't breathe out. I even tried it with some earlier masks I had been able to use in the past (they just didn't fit well which was the reason for the test) and found I couldn't breathe out with those anymore either. I've been to an ENT, had an endoscopy, tried using a Good Morning Snore product (which pulls tongue forward), and spoken with a couple Drs who specialize in sleep apnea. I haven't gotten any further towards finding out what's wrong and treating it. I'm in pretty good shape, no lung problems, and nothing else I can think of which would cause this. Can anyone help shed some light on this. It's starting to get really bad. Thanks...Rick
Hi Rick and welcome to the forum.
Are you using the ResMed Airsense 10 Auto CPAP? What are your current settings? Are you using the ramp feature? What settings were recommended/prescribed by your clinician?
Do you have a copy of your sleep study results? In this report should be a figure for AHI (Apnea Hypopnea Index). Any level over five is indicative of obstructive sleep apnea (OSA). If your number is 30 or greater than 30, your level of OSA is considered to be severe. CPAP is the first, most effective and least invasive of all the treatments for OSA. CPAP or XPAP is the gold standard for treatment of sleep apnea.
Sleep Apnea is related to a number of different medical conditions, but it happens even to those who are in pretty good shape and without any lung problems. There are studies that demonstrate genetic tendencies, as sleep apnea tends to run in families. Because my husband and I have OSA, our children are 98.7% likely to develop OSA sometime during their lifetimes. My brother and my sister both have OSA. I suspect my father had it as he snored so thunderously, but not everyone who snores has OSA. We'll never know for sure because he never had a sleep study done. OSA tends to worsen with age and with changing conditions (lack of fitness and weight gain). Having a sleep study done and finding out that you have obstructive sleep apnea is a great gift...because now you can do something about it. And it's worth getting the best treatment for it because untreated OSA will likely lead to an entire host of health ills (diabetes, high blood pressure, car accidents, high cholesterol and atherosclerosis, stroke, kidney disease, CHF - even cancer and early death). My husband's father, who also snored thunderously, developed all of these ills along with all the diabetic complications. But he also was never sleep tested, though we encouraged him to get a study done. The thought of being hooked up to a machine made him never want to know. It was really too bad. We tried to show him that CPAP is just a different way of sleeping and once acclimated to it, you never give it another thought. And that's usually because you just feel so much better when the apnea is adequately treated...much less sleepy and fatigued during the day. Our pleas fell on deaf ears. He died 5 years ago. My father died 10 years ago.
So...let's get your therapy up and running. Your difficulty breathing out against pressure most likely is related to your treatment pressures and settings. This is a common complaint of patients who are using fixed, rather than auto CPAP and/or who are not using ramp for comfort. Please answer the above questions and we'll try to help you more directly.
Hi SnuzzyQ - thank you very much. I'm sorry I didn't get back to you sooner. I didn't do a very good job explaining what's happening. It's exactly like the process you go through to hold your breath (without letting cheeks expand). Breathe in and close something off to hold breath in. I just don't know enough about the anatomy to say what exactly what you do when you hold your breath. If I knew that then I could revisit my doctors to figure it all out....Rick Joy
Your post generates a lot more questions than answers. SnuzyQ has asked more of them, but I will throw in my 2 cents.
You talk about using a ResMed with CFlex+... ResMed does not use that terminology. Their expiratory pressure relief is called just that EPR. Phillips Respironics (DreamStation) uses the Flex terminology. So which manufacturer and model of a machine do you have? I am not trying to be picky with words, as there actually is a difference in the two methods. The ResMed EPR provides actual pressure relief approximately equal to the setting. If you have a pressure setting of 10 cm, and EPR is set to 3, then you get 10 cm pressure in inspiration, and 7 cm on exhale. That can make breathing out against higher pressures quite a bit easier. Respironics on the other hand with their Flex technology shape the pressure reduction to make it feel a little better, but it really does not reduce pressure equal to the Flex setting. It is less.
Can you tell us more about your pressures? What is the minimum pressure, the maximum pressure, and what actual pressure do you get during the night.
It really does matter exactly what mask models have worked the best and the worst. Nasal pillow masks where part of the mask goes right into your nose, if poorly fitted can collapse under exhale and you can't breathe out. My wife has had that issue with a F&P Brevida mask. The small size collapses on her. The larger size works better but it has to be correctly placed or it can be a problem too.
So if you can give us some more information I may be able to help you if it is a CPAP related issue.
Hi Sierra - thank you very much. I'm sorry I didn't get back to you sooner. I didn't do a very good job explaining what's happening. It's exactly like the process you go through to hold your breath (without letting cheeks expand). Breathe in and close something off to held breath in. I just don't know enough about the anatomy to say what exactly what you do when you hold your breath. If I knew that then I could revisit my doctors to figure it all out....Rick Joy
I can exhale with my machine, but it is different. With normal breathing, we work to inhale and relax to exhale. With the CPAP, we relax to inhale and work to exhale. I also noticed this with SCUBA gear, but I would never sleep underwater.
Neil - thanks very much for your reply. It does make a lot of sense. After reading it I realized I was having the same problem sometimes (not always) with just regular breathing but never noticed it. The CPAP breathing problem seems to have all come on relatively quickly. I breathe a lot through my mouth a lot because of a deviated septum. I'm having that taken care of, but the ENT doesn't really think that will address this aspect of my breathing problems. I believe I'll try seeing a pulmonologist just to check things out...and because I really can't see that I have any other options. Just to add a bit more info with this condition...it's exactly like what happens when you hold your breath...you take in air and then do something to hold it in. I need to figure out what that is then I'll be able to talk about it a little better. Thanks again...Rick
I sometimes find it difficult to exhale through my nose with the nasal pillow also. My standard operating procedure now is to lay in bed for a couple of minutes before putting the nasal pillow on. I relax my body and try and lower my heart rate. I put the thing on and start it up. For the first 5-8 breaths, I will exhale through my mouth with pursed lips. Then I begin to exhale through my nose and get to sleep.
If your machine is set up properly you should not have to do that. The machine should immediately feel comfortable and breathing effort should be unrestricted like you are wearing no mask at all. The trick on an AirSense 10 is to set a minimum pressure of 7 cm for example, use the auto ramp feature with the start pressure also at 7 cm, set EPR to 3 cm and for Ramp only.
When set up like this the machine will immediately give you 7 cm on inhale, which most find comfortable. On exhale pressure will go down to 4 cm which is the lowest possible pressure for the machine. It will stay at those pressures until the machine senses you have fallen asleep. Then it will ramp pressure up to your machine minimum, which may be the same 7 cm in this example, and stop the EPR. Inhale and exhale will be the same. This gives you up to 30 minutes to fall asleep and get used to the machine.
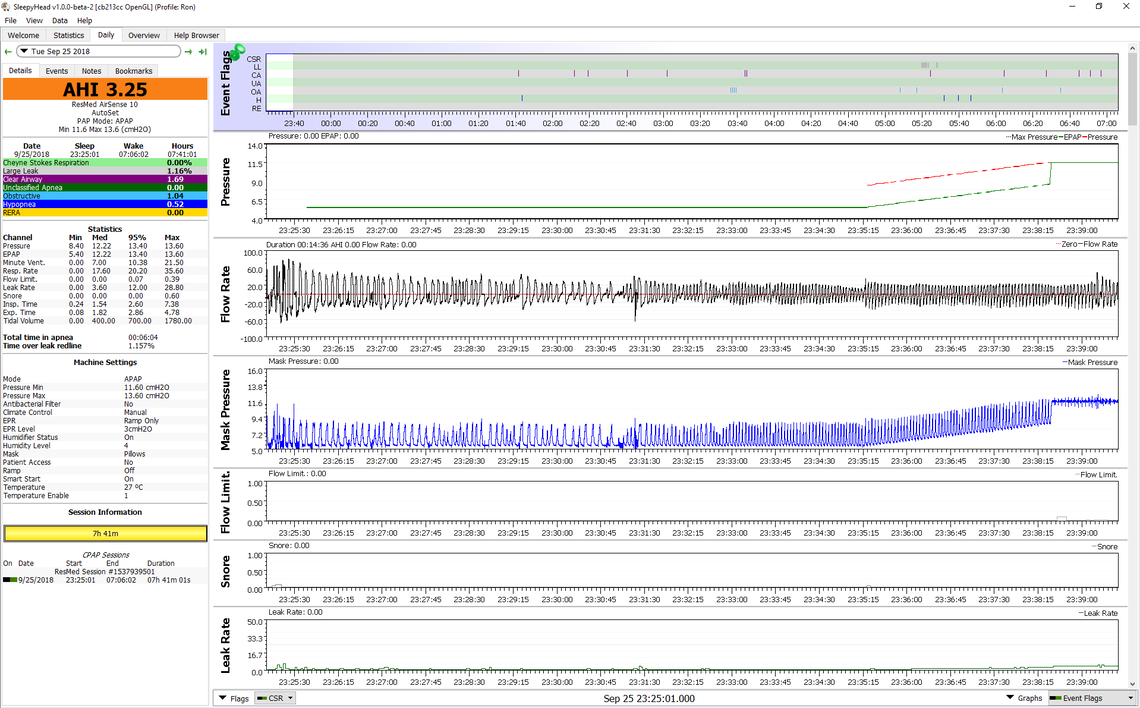
Here is a SleepyHead screen shot showing what that looks like. I use pressures a little higher than in my example. Ramp start of 8.4 cm and a minimum treatment pressure of 11.6 cm. At 11:24 I started the machine. About 10 minutes later at 11:35 the machine decides I am asleep and starts the ramp up. By 11:38 or over 3 minutes the ramp is complete, the EPR reduction on inhale is stopped, and I go to a constant 11.6 cm, until the machine decides I need more. Works really well for me.