This question has been subject to a lot of debate as APAP machines have become less expensive and the trend has gone away from using overnight in lab titration studies to determine what pressure to set a fixed CPAP at. In any case here are my thoughts based on 6 months experience using an Auto CPAP (ResMed AirSense 10 AutoSet). In the beginning I would have answered this question without hesitation and said that an Auto CPAP is the obvious choice. But, my experience has led me to a slightly different conclusion now.
Auto CPAP or APAP: With the cost of an in lab titration test going up and the cost of an APAP going down they have certainly become more popular. The more common method of prescribing them now is to do an at home sleep test (like I had) and then prescribe an APAP as a trial. Follow up is done to see what adjustments are needed to the pressure settings, and then that is about it. The machine is left to kind of self adapt to the user needs. Sounds good, but does it give the best results?
Fixed CPAP: To be properly set up they require an in lab titration test where different pressures are tried for about an hour at each pressure during the night to see what works best. Based on the test a fixed pressure CPAP is prescribed and the patient left to use it. If it works that is it, until treatment becomes ineffective and then they are most likely required to come back for another expensive titration test to see if adjustments are required. Not surprising that insurance companies are liking this route less and less and pushing for the use of an Auto CPAP.
My conclusions based on going the Auto CPAP route have evolved over the last 6 months, and my current thinking is that there are really two answers to this basic question.
The Auto CPAP route certainly makes a lot more sense to minimize the cost and time to get a patient into treatment and maintain it over the longer term. If one uses software such as SleepyHead you have the ability to see how well the machine is performing and whether adjustments are needed. Some will choose to do those adjustments themselves, while others will make requests of their provider to do the adjusting. Either way, the outcome is pretty good. However, what is debatable is whether or not the effectiveness of the treatment is the better than a fixed pressure CPAP.
My conclusion is that while the APAP machine is the right choice, at least for some, there can be an improvement in treatment effectiveness by going to a fixed pressure instead of a variable pressure, once you know what pressure you need. Fortunately most APAP machines have that feature built in and it is a simple configuration set up change to make the machine work as a fixed pressure CPAP. And with SleepyHead you can come up with a pretty accurate estimate of needed pressure without undergoing an in lab titration test. You can get the information from the APAP machine data.
Why do I think that? Well it may be slightly premature, but I am 12 days into a fixed pressure mode trial and am actually seeing improved AHI results compared to running it with variable pressure controlled by the machine. My AHI has improved to an average over this period of 2.4 compared to a long term average with the machine on Auto of 3.2. Not a huge difference, but an improvement. I notice no difference in comfort, and if anything have fewer major leak episodes.
While it may seem regressive to set a fancy auto machine into manual mode, it may actually improve the results you get. I think the reason for getting better results is quite simple. Pressure is increased as soon as the ramp (if used) ends. This eliminates the need for apnea events to trigger an auto increase in pressure. Yes, you do have a few apnea events which may have been prevented if the machine was allowed to go higher than the fixed setting, but taken together more are avoided by the early ramp up of pressure.
So, I throw that out there to share what I have learned and for comments. As always one person does not make a study, but it seems to be working for me.
I am curious what your fixed pressure is and how you arrived at it. Also, what pressure limits were you using with machine on Auto when you had the 3.2 average?
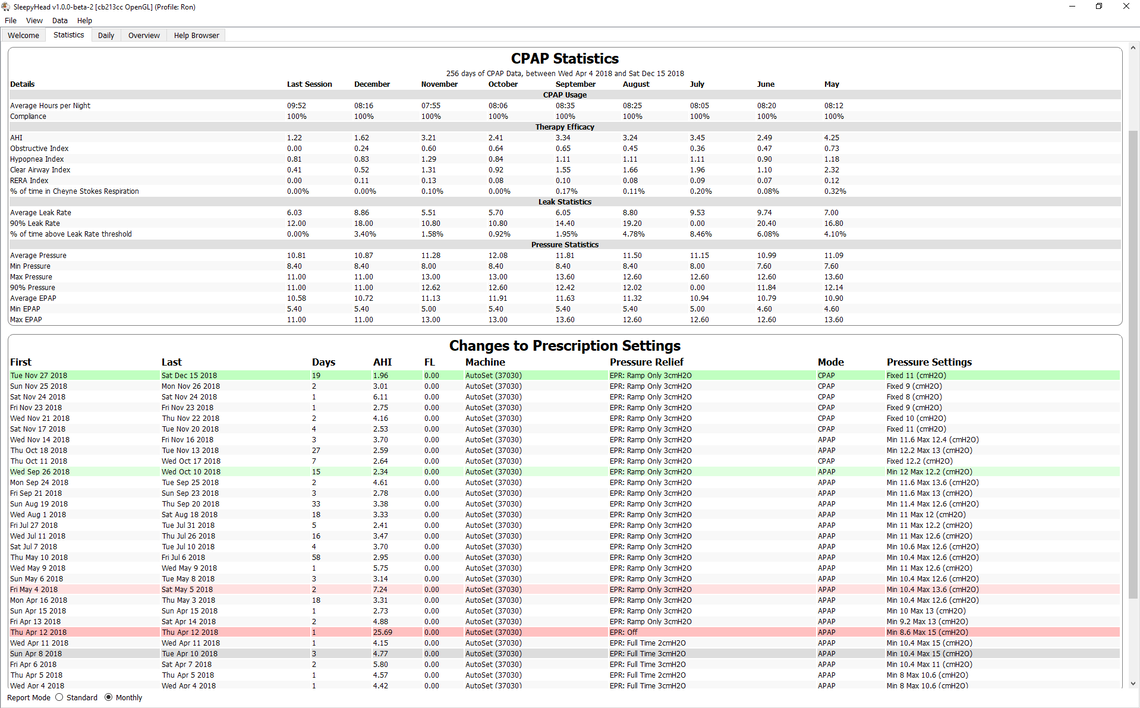
I have had my minimum as low as 8 cm and maximum as high as 15 cm over the past 6 months. The first 3 weeks or so the EPR was at 3 cm full time. Since then it has been set to ramp only. Over the past 5 months I have been narrowing and narrowing the gap between minimum and maximum. I got a good 5 day stretch with a minimum of 11 and max of 12.2. I then tried increasing the maximum again and AHI got worse instead of better. The 6 month average was in the 3.2 range with a wide variety of settings.
Then I finally decided to set the minimum at 12 cm and maximum at 12.2. So technically it is not in full fixed CPAP mode, but for all practical purposes it is acting that way. I will probably let it go on another week or so and if things are still all good, I will switch the mode to CPAP and set the pressure at 12.2 cm. This said there is certainly nothing real predictable about AHI when central apnea is involved. In the 12 days of fixed pressure my worst AHI has been 7.0 and best just under 1.0. In think that is why one needs to look at long term averages. From night to night the variation can be quite large.
I think this is very specific to the individual patient. I would not miss an opportunity to discuss different treatment approaches with the physician who is overseeing your sleep therapy or a sleep tech.
Haven't been able to see sleep medicine doctor yet. Had the home sleep test (I have Kaiser), trial of a machine for a couple of days (helped), then machine was ordered. Got machine about 10 days ago. I am going to give another try to getting an appt which will probably be 3-4 weeks from now if I am lucky. Going to get a different mask on Friday from the company Kaiser contracts with to provide durable medical equipment as initial one causing soreness in one nostril. I would be thrilled to see a sleep physician or sleep tech if I could.
I found this article on CPAP vs APAP at the link below. It appears to be targeted to the sleep professional audience and addresses changes in the industry.
AutoPAP Versus CPAP Which is Better?
The last paragraph lists some possible unique situations where an APAP may give the better treatment. However, the interesting part of the article is that the reported trend for sleep practitioners (under the influence of insurance providers no doubt) is to prescribe an APAP for convenience and overall cost. But after 30 days of in home use in APAP mode by the patient they then set the machine to fixed CPAP mode. Even more interesting for me was that the method suggested is to look at the sleep data record and use the 90% or 95% pressure average over the 30 day trial, and use that as the CPAP mode fixed pressure.
That prompted me to look at my first full month of data (May 2018) in SleepyHead and see what the 90% pressure was on average for that month. It turns out to be 12.14 cm. It appears I have spent 5 months or so now trying to adjust my APAP settings to some optimum values (over 20 different settings), and if I had followed this simple rule of thumb I would be in exactly the same place as I have now arrived: Fixed CPAP at 12.2 cm of pressure! Ouch! Kind of reminds me of the Expedia World Traveler in search of the perfect beach. See video at link below:
Just as an update I stopped the fixed pressure trial after 22 days. The AHI average after 22 days was the same 2.4 as I reported after the initial 12 days. So the 25% reduction in AHI using a fixed pressure compared to running in Auto held in the longer term.
I am now 6 days into my next test. I rationalized that if I put the machine back in Auto and set the minimum pressure at what appeared to be the optimum single fixed CPAP pressure of 12.2 cm, and then the maximum pressure a bit above that at 13 cm, then I might get even better results. That setup would get the pressure up to an effective level early in the sleep, and then still be able to respond a bit higher to abnormal events which may occur later on. I can report that so far my average is now 2.0 or about another 17% reduction. But, I know from past experience that it takes a lot longer than 6 days to set a true average. So we will see if this method holds up in the longer term.
Another update. I did 27 days on the 12.2 min to 13 max pressure setting. The AHI initial AHI average of 2.0 did not hold and I got a final median AHI of 2.64, so not quite as good as a simple CPAP fixed pressure of 12.2.
Since then I have tried going the other way with a fixed pressure again, but lower instead of higher - 11cm or 1.2 cm lower. After only 4 days I have an average of 2.53. Next I plan to go lower still and see if there is a break point where lower pressure starts to cause more obstructive events, and fewer central. Will try 10 cm next to see what that does. I am trying to validate the theory that higher pressure may not only produce more central events, but if you suffer from mixed apnea like I do, then it may cause more obstructive events too. Time will tell, but I am starting to come to the conclusion that fixed CPAP may very well be a better solution than Auto CPAP, especially with a mix of obstructive and central events...
Another update on my testing of Auto vs Fixed CPAP pressure effectiveness. I have kind of gone through three phases with this testing:
Standard Auto Mode - This is the setup where most machines are put in for patient use. A common starting point is 5 cm to 20 cm. Then if one is fortunate to have an attentive sleep technician, this range gets a further refinement based on data collected over the first month or so. Since my trial machine was not compatible with SleepyHead, I don't have a record of the first two weeks, but I recall I started out something like that. Fairly quickly I reduced that range based on what I was seeing in SleepyHead to the 10 cm to 15 cm range. The outcome of this phase was getting AHI fairly reliably under 5.
Limited Auto Mode - My next strategy was to try and optimize the set pressures by narrowing that range more and more. I also, with thanks to a post by sleeptech at this forum switched to a EPR on ramp only. Using EPR on ramp only resulted in a reduction in pressure, and that was further improved by narrowing the range of pressures allowed. The outcome of this phase was getting AHI down to the 3 range.
Fixed Pressure CPAP Mode - My third and latest strategy has been to try the fixed pressure mode. I was getting suspicious that even with a narrow pressure range, the machine was running pressure up too high and was increasing the frequency of central apnea and hypopnea events. My thoughts were to keep reducing this fixed pressure setting until obstructive events started to increase. Unfortunately I have not been very disciplined about leaving the pressure at one setting long enough to collect sufficient data. But, that said a pressure of about 12 cm gave me an AHI of 2.3 over 15 days. And now at my latest longer term trial at 11 cm for 19 days I have an average AHI of just under 2. For many with basic apnea that probably does not sound that great, but for me where most of my apnea is central, that is pretty good.
What is my conclusion in all of this? Well, first off, one person does not make a study. My AHI at diagnosis was about 34, and there was very little central apnea identified. However, with PAP treatment, central apnea increased, and really has not decreased after the 6-8 weeks that some studies have shown. It stayed high with my apnea remaining mixed, with the highest portion being central. So these results may only apply to someone in a similar situation, or where there is at least some central apnea in the picture. But, for me, it appears a fixed pressure CPAP mode has been much more effective than a wide open auto mode, and better even that a limited pressure auto mode.
Could someone get to this point by starting with a fixed pressure CPAP machine instead of an Auto CPAP? Yes, possibly, BUT, I think it would be very difficult unless the machine stores detailed data on a SD card that can be read by SleepyHead. One would have to try one pressure for at least a week if not 2-3 weeks, and then try another pressure. It would take a long time, but I suspect it can be done. The Auto machine allows you to identify the range of possible effective pressures very quickly, which in turn makes the testing for ideal single pressures quicker. And it is kind of a moot point anyway as the last time I checked the cost of the ResMed Autoset is only about $80 more than the ResMed Elite fixed pressure machine (which has data capability). To me it makes much more sense to start out with the Auto machine, and then switch to fixed CPAP mode later if that works better.
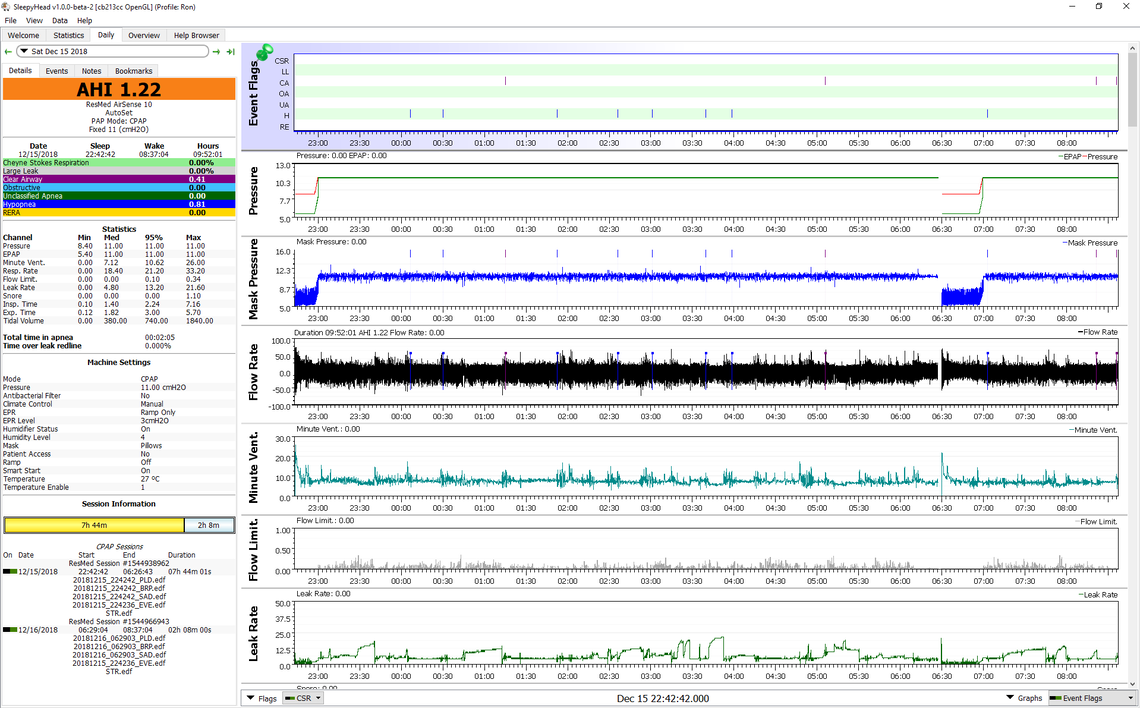
Hope that helps those who are dealing with this issue. The biggest benefit in all of this for me is that I find my sleep more comfortable now with a fixed pressure. A fixed pressure of 11 cm is certainly more tolerable than an auto mode which was running pressures up to 15 cm, while potentially causing more apneas than it was avoiding. Here is my sleep report from last night which is better than average for me, but somewhat typical. And I will also attach the Statistics page which kind of details my journey through these three phases identified above. To date I have now tried 30 different setups!
Brilliantly written Sierra and I love the disclaimer. :)
I suspect that the underlying concept reflects on the nature of man nearly as much as it does on the potential of technology.
I can only vaguely comprehend all the options and details but it seems to me that the principal applies to almost everything that we have and use. Even your argument for the most advanced fully optioned machine because it provides better feedback is true of just about anything that is available on the market. Cars, washing machines, fridges, toasters ........... the list is endless.
They all have multiple options and menus and feedback loops that are essentially redundant to their real function. Once we get them home and finish playing with them we usually revert to the basic, simplest application and all those extra options are largely ignored. Yes it's fun to know they are there but there is also appeal in simplicity.
I am an exceptionally systematic individual and sort of a do it yourselfer and will screen the outcomes intently. None of this looks particularly like advanced science. I was not awed that after my rest consider, the specialist couldn't give me separate outcomes for the time I spent dozing on my back versus on my side where I might possibly have occasions. I don't feel like I am going out on a limb very far going to an APAP range, which surrounds the CPAP setting which has worked for me. I am trying the APAP partially so I can find out if lower pressures are effective for me since a relatively high pressure of 15 requires the mask to be pretty tight which is somewhat problematic.
Carroll,
I would make some points on what you are thinking about.
Yes great say, in addition one of my friend suggest me to purchase a Cleaner for my machine of soclean but I am confused which one is suitable , https://sortedforyou.com/best-cpap-cleaner I read this but still confused can you suggest me which on is better?
I am in the camp that says CPAP cleaners are an unnecessary gimmick. I would worry about the impacts of ozone on the life of the equipment. Neither ResMed or Respironics recommend them, that I am aware of. I just disinfect with vinegar, followed by Dawn dish soap and water, and then a final rinse with water to hang to dry.
I am really glad to see this thread. I have a Resporonics APAP that was set by doctor to go as low as 4 and as high as 15. I set the flex to 3 and ramp time to 30 min. After a year since starting therapy my average AHI is 4 -6, sometimes as high as 7. I watched some youtube vids and decided to adjust the machine to CPAP mode just to see what would happen. I put it at 12 and left the flex and ramp the way it was. It felt a little windy but my AHI went down to an average of 3 to 4. Then I set it to 10 and now after a couple of weeks I am getting an AHI between 1.5 and 3 constantly and the pressure feels comfortable. I have never had this few events! I would also like to add a disclaimer: 1. I am not a sleep technician and am just experimenting with my settings. 2. This is working well for me but I am not advocating that it is the correct approach for anyone else.
I think if a person is suffering from central apnea events and hypopnea events that are central in nature, there can be significant benefits to a fixed pressure mode. The Respironics and ResMed machines are smart enough to distinguish between central and obstructive full apnea events. And, they do not raise pressure in response to a central apnea event. However, I don't think either can distinguish between central (reduced breathing effort) and obstructive (flow resistance) hypopnea. As a result the machine can chase its tail and raise pressure unnecessarily. If one is sensitive to pressure that raises central events even more. In other words, the Auto is not so auto or good.
You may get a further improvement by turning off the Flex. That in turn could let you lower your pressure even more. The lower pressure is more comfortable, and may create fewer central events.