36 year old male, 5'8 and 165 pounds. I have hovered around 140-145 since I was a late teenager. This year, I jumped to 165 for some reason. I'm active, lift weights, etc. Since my early teen years, I have always been much more exhausted than what felt like normal. Never figured out why. Had a bunch of medical tests, blood work, etc., done at the beginning of the year. Also checked thyroid, but it was normal. Everything seemed fine medically, but I apparently fainted from sheer exhaustion for about 10-15 minutes during one of the blood draws. Blood pressure shot down to 60/60 with 52bpm heart rate. They never figured out why. That was the first and only time that happened and it did not repeat during a blood draw on another day. I had never fainted during one. I have always been very twitchy/jumpy since I was a kid. Others noticed it. I still am, for some reason. They said my reflexes were too high. Went to a neurologist and she said that my reflexes were normal and healthy for someone my age. For the "jumps" that I get sometimes, she said I might want to have an MRI of my back.
Went to ENT doc. Had an MRI of the brain. Deviated septum was casually noted, but nothing wrong. Eventually had a CT scan of the sinuses. In July, I had turbinate reduction surgery for enlarged turbinates and also had a deviated septum with right-sided spurring corrected. I breathe way easier and my nasal airway is much quieter when I breathe. Before, my breathing was loud and took much longer than normal to let out a full breath.
Had a sleep study on March 27th. Their pillows were hard, their bedding felt like sandpaper and nobody told me that I should probably take a melatonin or two right before the sleep study. I slept 2 hours 45 minutes for the whole study period.
Results: "The polysomnogram shows severe sleep fragmentation. Sleep efficiency was reduced. There were 13 obstructive apneas and hypopneas present for an overall apnea-hypopnea index (AHI) of 4.7. There were 50 respiratory events including RERAs for a RDI of 18.1 Supine AHI: 6.1. (Supine time 290 minutes). REM AHI: 9.2. (REM time - 6.5 minutes). The total time with oxygen saturation under 90% was 0.0 minutes with a nadir of 92%. The desaturation index was 4.4 (#events/hour). Cardiac was normal sinus rhythm. Snoring was present. Periodic limb movement index - 0/hr sleep and PLM arousal index - 0/hr sleep."
That confuses me. A hypopnea by definition is abnormally slow or shallow breathing. An apnea by definition is temporary cessation of breathing, especially during sleep. I don't know for sure if those numbers would have been twice or three times as high if I would have gotten that much more sleep for the study. The sleep doctor said I was 0.3 from the minimum 5.0 AHI required for mild sleep apnea diagnosis. Not sure if this would have been higher had I slept more. However, he also noted no drop in oxygen levels, so now I'm confused. If it was obstructive, why isn't my oxygen level dropping any? I woke up a lot during my study, but they didn't seem to think I have sleep apnea. In the mornings, I feel awful and drained of energy, ready to go back to bed as soon as I get up. So if I am waking up as if it is obstructive and yet it obviously isn't obstructing but for a few seconds (if at all), then all that I am doing is waking up.
Some mornings I know when I wake up a lot of times, but not sure why. There are times when I jump awake like that feeling when you're dreaming that you're falling and jerk awake. Only that happens a lot some nights and not so much on others. Other times, I wake up with this loud pop-like noise that sounds like it is in my face/head and cannot figure out what in the world it is. It sounds like something cracking in my maxillofacial area, but could possibly also be ear-related. Nothing was ever found to be wrong in my ears. It seems to happen mostly when I'm laying on my back. Laying on my side and stomach seem to make me rest better, but that's not very comfortable and laying on my stomach makes me press my tongue into my teeth even more. Sometimes when drifting off to sleep, a leg or arm might jump once or twice and that's it.
My jaw does pop a little (probably TMJ-related), but nothing too major. An orthodontist did mentioned one time that my teeth all seemed ground flat, so I probably do grind. I also have a very pronounced crenated/scalloped tongue all the way around all edges and also on the top edge every morning. I get that almost daily. I get canker sores from those places sometimes. I likely thrust my tongue and/or bite the edges of it while sleeping. The ENT doc said it looked a little too big sometimes or something. I also feel that my bottom jaw seems to naturally move forward a good bit when I sleep. I'm planning to get a mouth guard (but I'm reading that they move teeth), but I don't think these things are the cause of my frequent awakening
I'm at my wits' end. Got any advice? I'm planning to have another sleep study at the beginning of the year. Would they be able to determine if I have some type of central sleep apnea during the same sleep study? I have GOT to find out what this is. It feels awful.
I would start with a full physical by your primary care physician. Have them check blood sugar via A1C measurement and things that are outside the purview of a specialist you have visited. The heart doc will be myopic with regard to things outside his/her specialty. The ENT the same. Try to eliminate things that are not obvious to a specific specialist. The teeth/tongue issues, should be addressed by an orthodontist.
Primary care doc: Lots of visits. A1C, thyroid and some other things were fine. Neurologist: Nothing wrong. ENT doc: suggested a mouth guard from the dentist, but unknown as to the cause of waking up, though the surgery improved nasal breathing.
Haven't been to a cardiologist, but the primary care doctor saw nothing odd/off about my heartbeat, blood pressure, etc. I had some palpitations before the nasal surgery. They were related to not getting enough sleep. After the surgery, for the most part, those palpitations went away and seemed to be related to just being severely behind on sleep.
So yeah, I'm running out of docs to go to. Planning to have another sleep study after the first of the year (waiting on a new insurance deductible through a new employer). Hopefully that will shed some light on it. If not for the waking up when I sleep on my back and the (seemingly) disappearance of it when I sleep on my stomach/side, I almost wonder if it isn't some type of central sleep apnea. Yet the lack of drop in oxygen level is very puzzling.
If I recall from my sleep study that sleeping is a tad more difficult due wires, grease for the electrodes, etc. Both central apneas and OSA will result in degraded oxygen concentration in the blood; mine was down to about 70 during my test for LONG periods which explains why I am pretty much brain dead today. Anyway, I am not sure where to go with your issues but just hang in there and keep looking for some answers. Looking at your results, it is almost surprising you got into REM sleep during the nap you took during the study. The 9.2 AHI is telling and should have disturbed your sleep if I interpret correctly and led to the "fragmentation" comment. When you come up for a new study, a sleep lab is the most accurate place to determine sleep apnea issues (plus others like restless leg syndrome) and if you have the opportunity after that, if warranted, get a LAB titration study to determine what prescription works best. Good luck.
Yeah, the last study was in the sleep lab and supposedly checked for everything. They claimed that I didn't have restless leg syndrome. They did put electrodes on my legs, head and all over my body, put a microphone in front of my mouth, some kind of device that measured breathing through my nostrils, etc.. So I walked away with "severely fragmented sleep" and yet the sleep doctor said, "Well, your oxygen levels didn't drop, so that's good!"
Then he indicated that I "didn't have sleep apnea" because I was 0.3 away from the 5.0 AHI required. Yet he said, "If you want, we can try CPAP!" Well, why would I want to try a CPAP if I supposedly don't have it? What's waking me up?
What I don't understand at all from the sleep study that I had before is how I had 13 hypopneas and 50 "breathing events" in 2.75 hours and yet they said that my oxygen level didn't drop. If hypopneas are by definition slow/no breathing, my oxygen levels should have dropped, even if just for a short time. They didn't seem to know what the 50 "breathing events" were in detail.
I would be fine with the lab titration study, but why can't they find anything during the actual study itself? :-/ If I have OSA or Central, they should be able to determine that.
When they rate apnea they just count the events and do not consider the length of each event, or how close together they are. If your events were short and spread out, that would likely have less impact on the O2 levels.
During a sleep study they do not treat you for apnea. They just monitor your apnea events. In a titration study you are being treated for apnea with pressure. They try each pressure level for an hour or so to see what impact it has on obstructive apnea and whether or not it increases central apnea events. The purpose is to determine what pressure your CPAP should be set at. If you have an automatic CPAP it is not really necessary to do a titration study. If they were to give you an Auto CPAP like the ResMed AirSense 10 AutoSet to try for a couple of weeks it would collect all this data automatically. You would find out whether or not there is any benefit to using one.
Perhaps a study of greater duration will yield more accurate results. 5 is the magic number for prescribing therapy as it is the bottom end of the mild scale and if your O2 level didn't drop, that is a very positive factor. You may have had events but not of sufficient duration to cause blood oxygen desaturation.
I can't say why the wake ups but in my case, I only sleep 5-6 hours tops normally; prior to therapy the same. Prior to therapy, I was up 3-4 times a night for potty runs and had vivid dreams. I found I wasn't getting into REM sleep after the study and I now never get up during the night for potty runs and seldom have vivid dreams I can remember. I constantly dozed off during the day (mostly inopportune times) and now don't. If you are not in REM sleep long, it may be because the apnea events are wakening you and you never get there.... just spit balling. Now that you are self-educating, might be time to get back to the sleep doc and have him explain things in more detail which I suspect you will follow better than when first embarking on this path.
It would seem from what you describe that you probably do not have apnea to the point where it should be causing big issues with your sleep. To get a better read on it, you may want to consider an at home sleep test. It still will not be real comfortable, but probably significantly more so than in a lab. Machines such as the Phillips Alice NightOne can detect obstructive and central sleep apnea and produce a detailed report. It would be better to get a report based on more sleep.
I wouldn't discourage you from trying a CPAP. If you have the software like SleepyHead it produces a very detailed report of what goes on during the night. It of course will use a minimum of 4 cm of pressure and will normalize some of the apnea, but you will see what residual there is. And if it is an Auto CPAP you will see what pressure it uses to normalize the apnea events. Last you will find out if you are going to be able to tolerate using one. I am assuming they will let you try one at no cost. You of course would want to be much more certain of the need before buying one though.
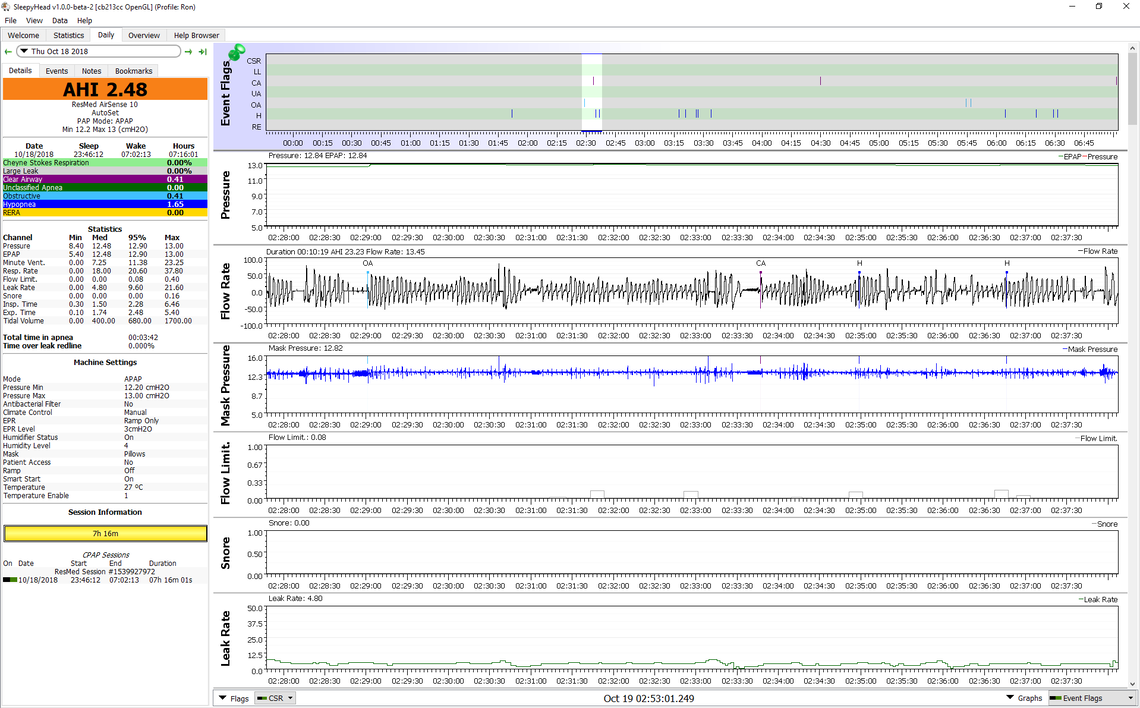
I did a screen shot from a few nights ago on my machine where there was an example of an obstructive event (OA), a central apnea (CA), and a hypopnea (H). You can see what they look like and how they compare. The ResMed machine I use distinguishes between OA and CA events by imposing a flow cycle when the breathing is stopped. If the pressure fluctuates up and down more then it is classed as an OA, and if the pressure is less then it is classed as a CA. In a CA event the airway is open so pressure is less influenced by a flow variation. You can see that also in this graph of the mask pressure.
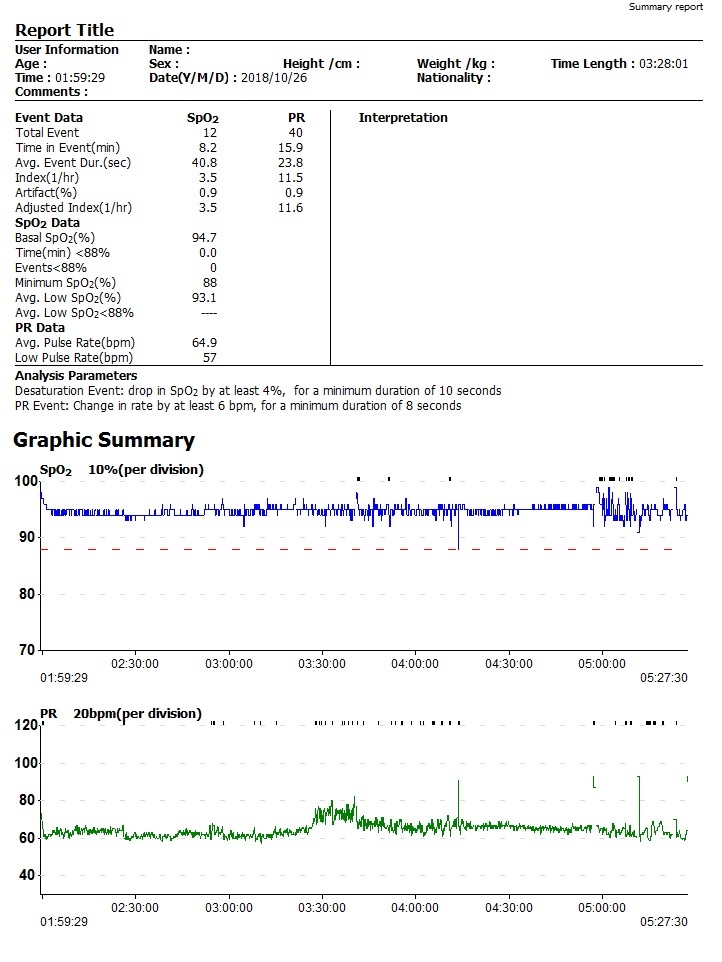
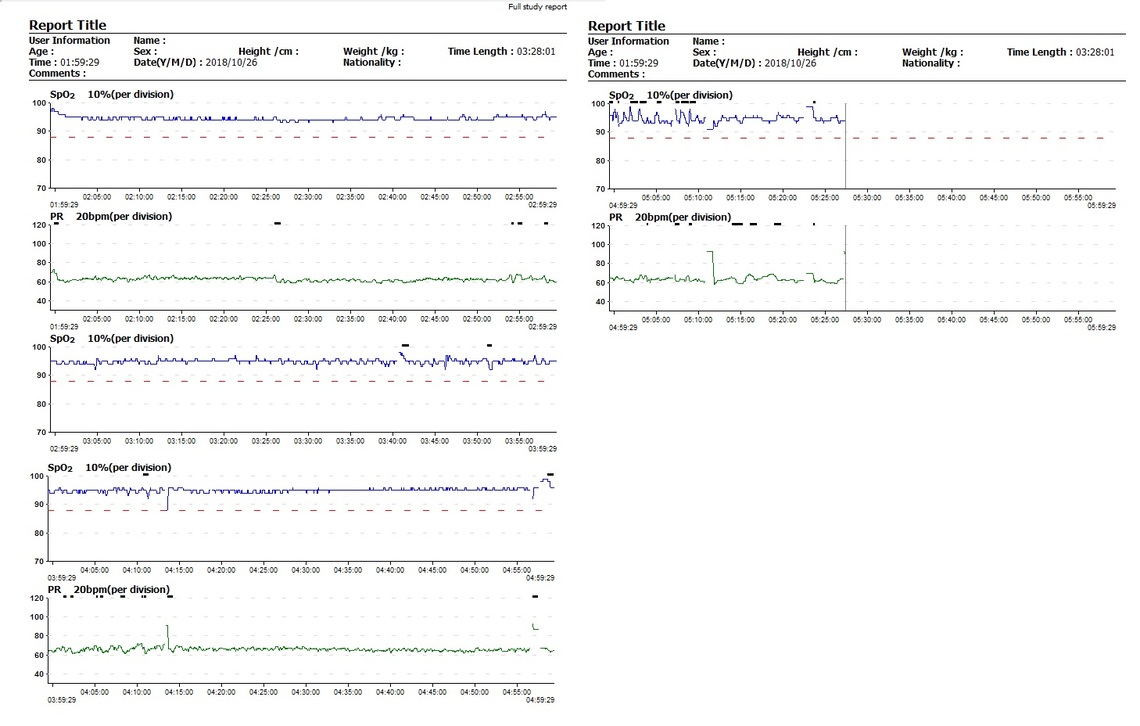
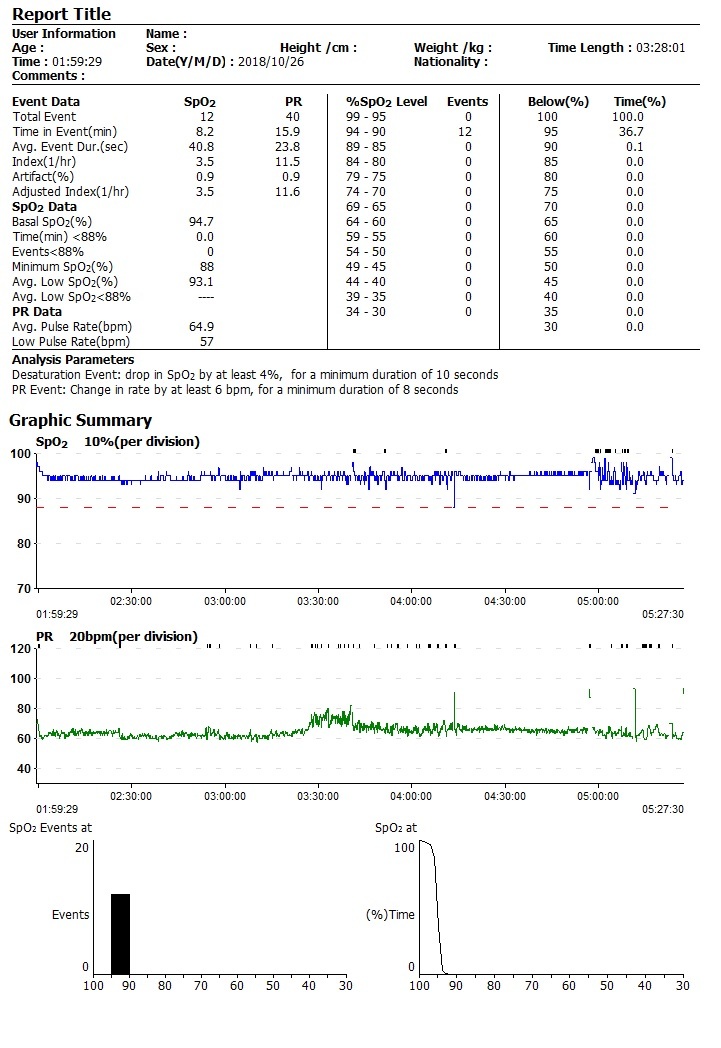
So here are my results from 10/16. I started it earlier than that, but something must have happened and I restarted it again when I got up for the bathroom at 2:00am. This was for the 3 hour period from 2:00am to 5:30am. Looks like my heart rate started going up and down about halfway through and at one point my SPO2 level went down to 88%. A number of others in the low 90's.
I am not a dentist so maybe one of the dentist here can address this issue. I think you have confused a mouth guard with a dental appliance for sleep apena. I believe a mouth guard is for people who grind their teeth while sleeping. It is made like a retainer and fits over your teeth. It does not move your teeth at all, just protects your teeth.
To start off, I have ordered a wrist oximeter with a finger sleeve to test myself throughout the night and verify that in fact my oxygen levels are not dropping. If they for sure aren't, I must be having some other kind of odd issue. The only thing that is for sure true is that I feel like a truck ran over me in the morning and have zero energy. That info will be useful when I have another sleep study.
As a little update, after 4-5 hours or so of sleep this morning, I woke up laying on my stomach. I had awaken twice within about a minute. I woke up with the typical "feels like my body is moving around lightly" feeling that a lot of people tend to normally feel after being in deep sleep. However, in addition to that, I felt two distinct and separate little "jumps" that seemed to have awaken me each time, maybe 15-20 seconds apart. Not a hard jerk awake like the "just dreamed that I was falling" thing. It was more light/subtle and barely there, but yet somehow still a full-body jerk enough to wake me up. It felt more neurological and that was all while on my stomach, which is usually said to not be OSA-related since it supposedly mostly happens when laying on the back. It almost felt like the little single full-body "jumps" that I get sometimes throughout the day while awake. They tend to be hours apart and a little worse the more tired I am. I felt a little tingly all over right after waking up, as well. Each time that I woke up, I was breathing and somehow remembered to mentally note that instantly as soon as I woke up. So I'm not sure that I stopped breathing and woke up because of that, but if nothing else, I did jump awake in an odd way. I had a little bit of a headache after waking up and felt kind of tingly all over.
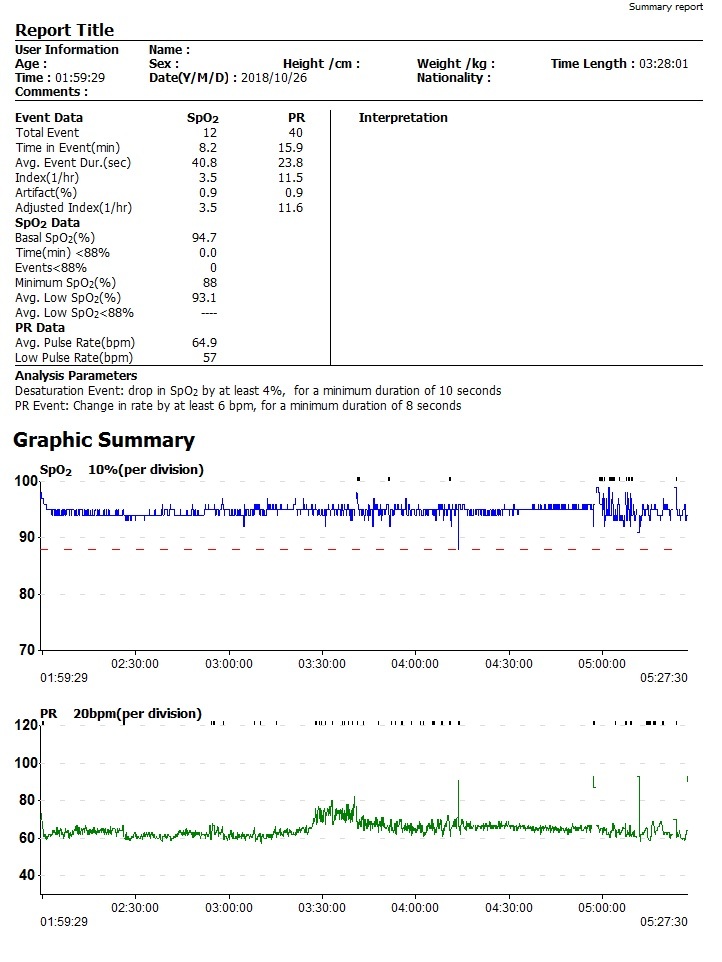
So here was a result from last night. I'm not sure why it starts at 1:59...I went to bed about 12:30am and started it then, then I got up at 5:30am. I think I may have accidentally turned it off and nothing was visible until 2am when I turned it back on after getting up for the bathroom. An hour and a half into sleep, it looks like my heart rate started elevating and going up and down apparently in relation to whatever was going on. At one point, it looks like my SPO2 level dropped to 88%.
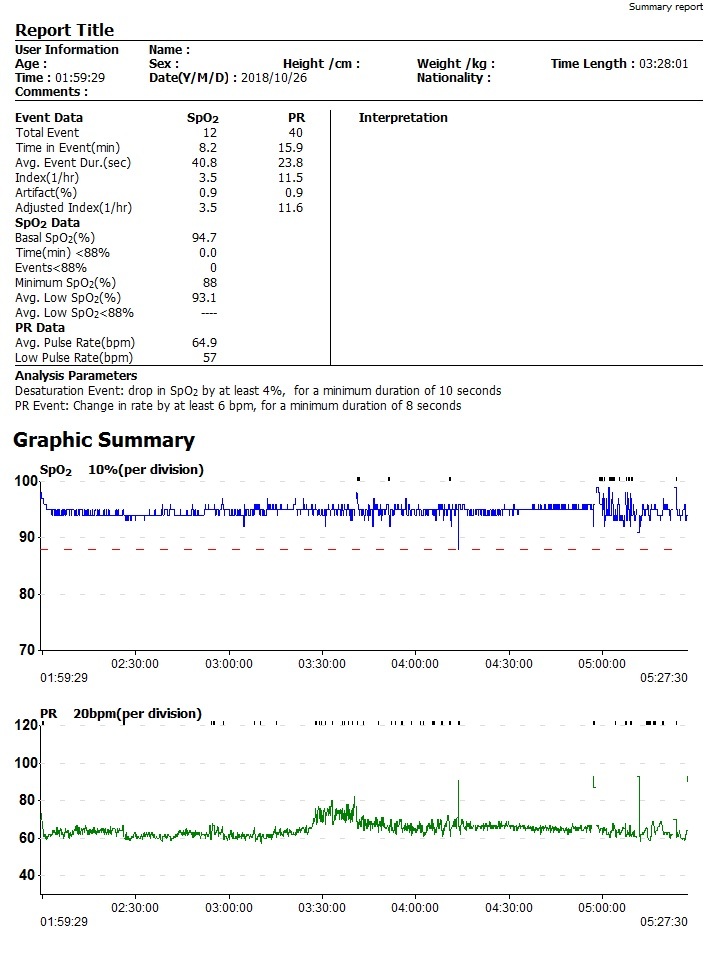
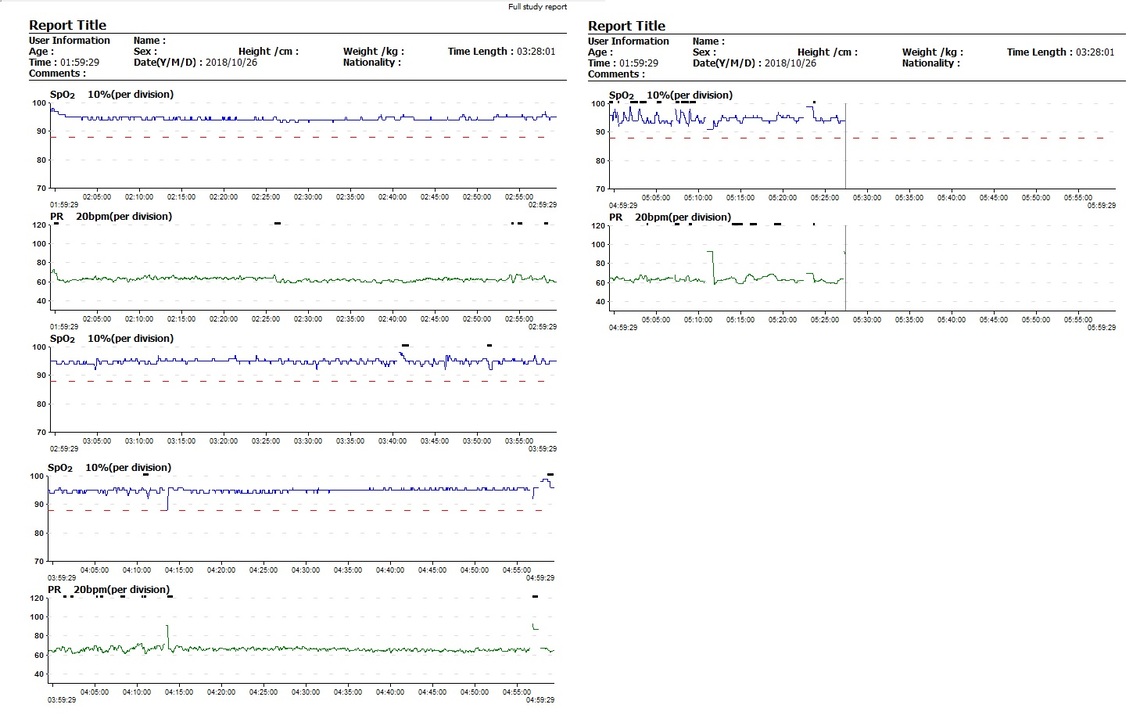
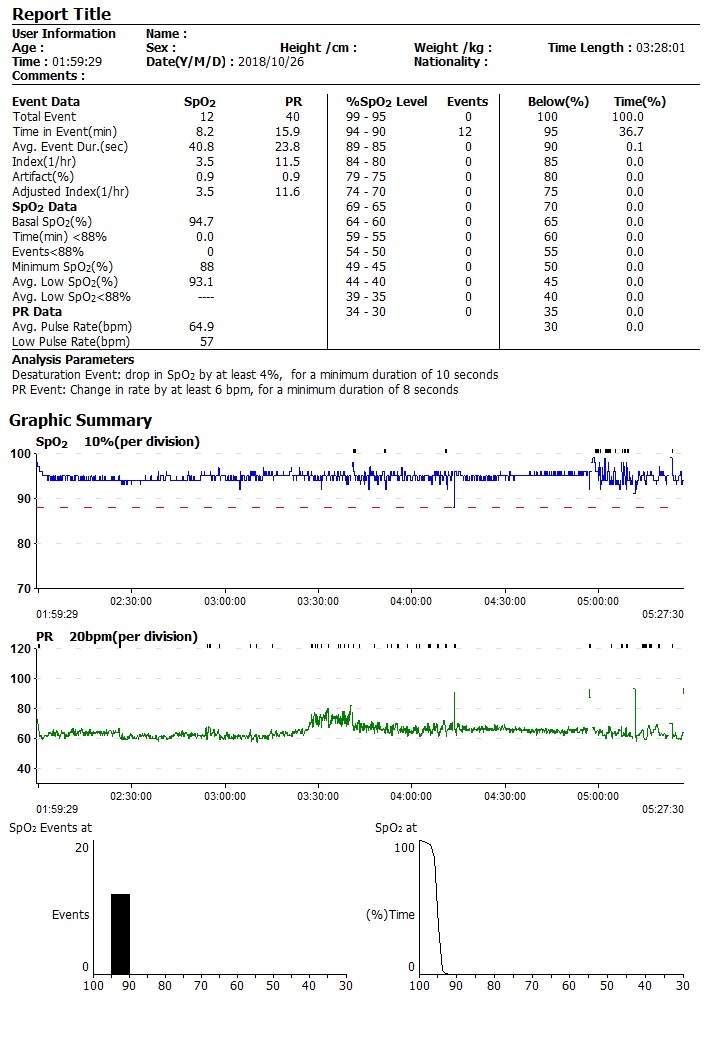
So here are my results from 10/16. I started it earlier than that, but something must have happened and I restarted it again when I got up for the bathroom at 2:00am. This was for the 3 hour period from 2:00am to 5:30am. Looks like my heart rate started going up and down about halfway through and at one point my SPO2 level went down to 88%. A number of others in the low 90's.
https://image.ibb.co/jtL9dA/1.jpg https://image.ibb.co/jORhyA/2.jpg https://image.ibb.co/jvtjBV/3.jpg
So here are my results from 10/16. I started it earlier than that, but something must have happened and I restarted it again when I got up for the bathroom at 2:00am. This was for the 3 hour period from 2:00am to 5:30am. Looks like my heart rate started going up and down about halfway through and at one point my SPO2 level went down to 88%. A number of others in the low 90's. The heart rate time and SPO2 variations, as I figured, coincide some. Going to try for an 8-hour more thorough check tonight.
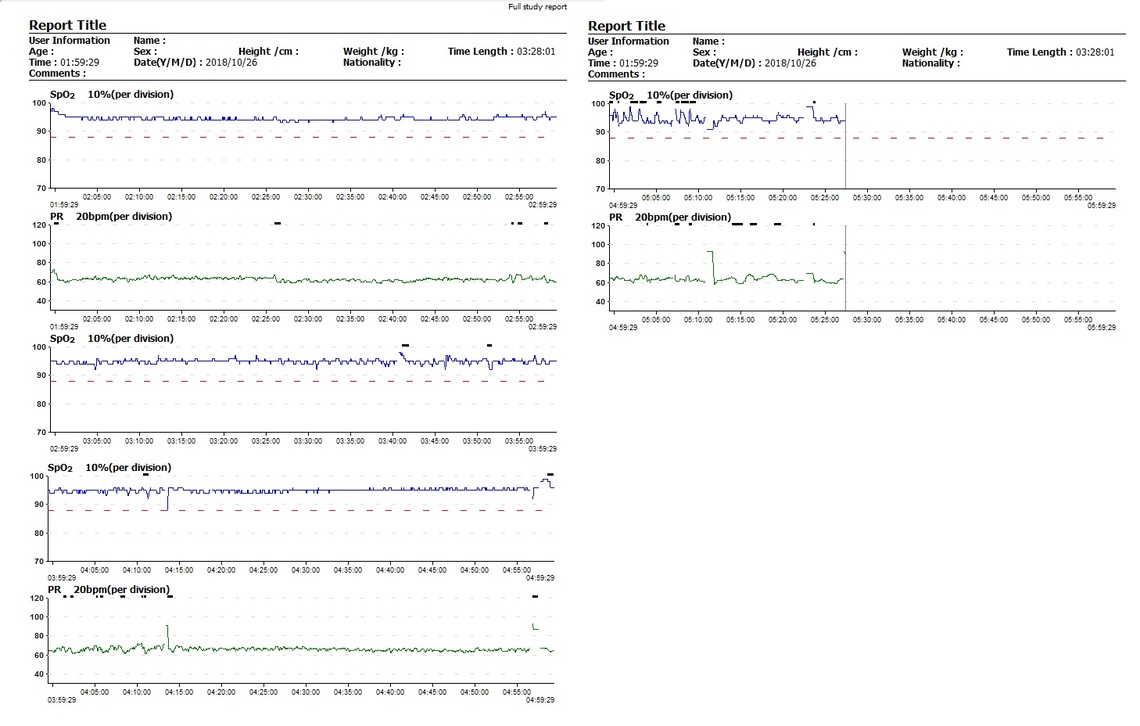
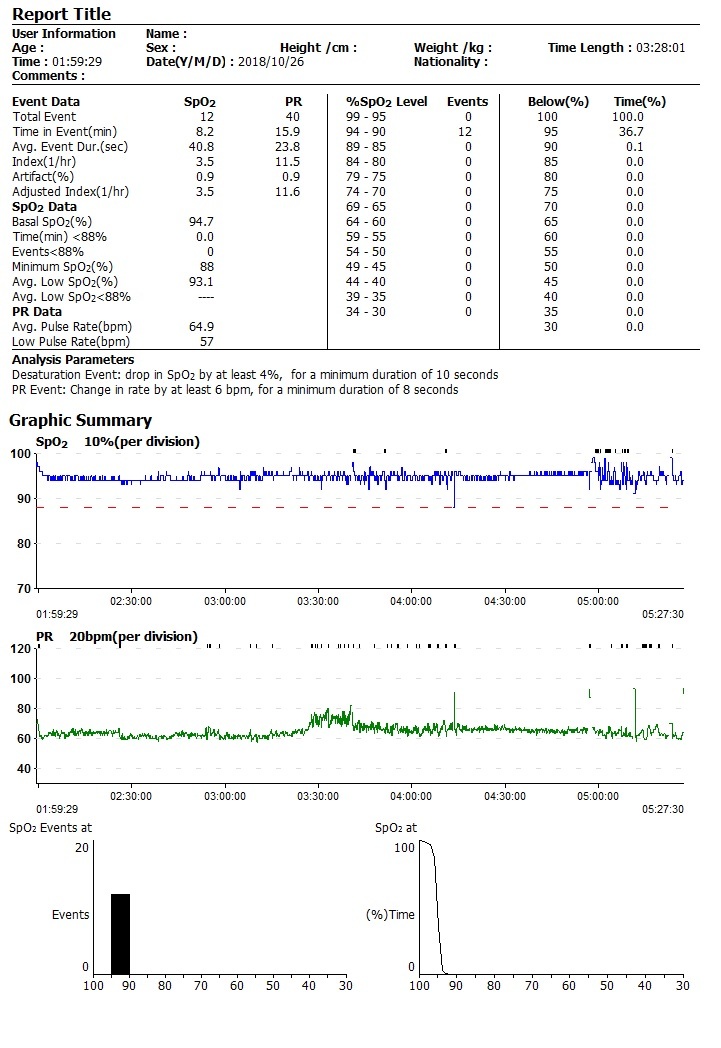
Average 94 is a shade low and 88 is lower than what is considered acceptable but the 88 was a single event that was most likely caused by excessive movement of your hand/finger, etc. If you sit on the couch and wiggle a bit you can observe that readings are bogus for the times of movement. I would say your SPO2 is pretty decent and wouldn't worry about the 88 too much.
So where should I go from this point on? Should I try to get another sleep study later on? I have found that later into sleep, when there's like 2-3 hours left before the time that I would get up, I wake myself up making an odd noise that sounds almost like I'm puffing air out of pursed lips in the corner of my mouth. Only it isn't that and when I try to immediately recreate it right after waking up, thinking that it was that, it doesn't sound anywhere near the same. It is something else. While the numbers aren't as bad as many people have...the same thing reflects in them. Towards last 2-3 hours, I get erratic heartbeats going up and down with oxygen levels wavering, even if still within the decent range. Then that distinct noise wakes me up and I don't know what it is. Upon waking, I feel like I'm at the end of the day about to go to bed instead of about to get up from a night's sleep. I'm that exhausted every morning.
You wrote the following in an earlier post:
"Then he indicated that I "didn't have sleep apnea" because I was 0.3 away from the 5.0 AHI required. Yet he said, "If you want, we can try CPAP!" Well, why would I want to try a CPAP if I supposedly don't have it? What's waking me up?"
Assuming they are offering the CPAP as a free no obligation trial, I would take them up on the offer. That is the cut to the chase option. If it works for you, then it works. To get a new machine you will need a prescription, and if you are having an insurance company pay for it, then that will need a prescription too. So assuming if you try it and it works, and they write a prescription then you are good.
The AHI measures full apnea and hypopnea. There can be other less severe events which may be waking you up, so the AHI may be understating your issues. Just a thought...
I think he meant buy one. I'm kind of confused, though. A lot of people are telling me that I shouldn't need a CPAP because my numbers and apneas are too low. Others are saying to try one to see if that fixes whatever unknown things are happening. Is that pretty much the best that I will know about it other than the machine either helps or doesn't when I try it?
So are my minor apneas something that I should be concerned about for future health problems similar to someone who has heavier sleep apnea? If they are light, I feel about the equivalent of if they were moderate to heavy. I'm not sure why they kick in for the last 2-3 hours, either. I would think that REM sleep would have set in within 2-3 hours max. It is bad enough to where I'm now scared to drive because my body isn't alert enough to react quickly enough and make necessary adjustments. I can do repetitive job tasks and tasks that are essentially ingrained in my brain, but some days I can't even type properly due to being so tired. So frustrating. Ugh. :-/
You may want to try the site at the link below. There are quite a few different tools and tips on improving your sleep without drugs or a CPAP.
So basically the people who have mild sleep apnea or light apnea so minor that they don't consider them to actually have it...pretty much just struggle through life trying to get enough sleep even though their sleep is fragmented? From what I have gathered about mine simply by what I remember from waking up and the time on the graphs, it appears that usually after 4-6 hours of being asleep, I start making some kind of weird, unknown noise that keeps repeating itself. The SPO2 graphs back up that something is going on with my heart speeding up/slowing down and my oxygen levels fluctuating up and down a little bit. Not enough to drop oxygen considerably, but enough to wake me up a lot of times. I used to think it was the "puffing" of air out of the corner of my mouth, but having tried to reproduce the sound immediately after waking up, it isn't it. It is louder and I don't think it is a snore. I am so tired of waking up in that way that it is ingrained in my brain to instantly try to figure out/reproduce the noise right after waking up and that's what I do every time. I also find that right after waking up when I have been asleep for several hours...I can almost reproduce the situation. It is either my tongue falling back or my throat closing over just enough to wake me. When I'm relaxed after that much sleep, I can almost feel it repeat itself on purpose as I'm falling asleep. So I presume it was maybe the tongue falling back into the throat or the throat closing enough to make a noise to wake me up immediately after without the oxygen level dropping much or at all. My apneas/hypopneas may be rather short, but it seems to be enough to make my sleep miserable every single day. By interrupting the latter portion of my sleep, it is like I'm getting just a little more than half of a night's sleep. It interferes with my driving. I am still unable to drive. I don't feel alert enough and I would probably have an accident on any given day if I got behind the wheel. I literally almost hit someone's mailbox up the street one day as I was turning off from our street onto the large main street to go to the store one mile away. My body was fidgety/not alert enough to be driving due to poor sleep. My cognition just wasn't there and that can be a daily thing for me.
I can't help but wonder how many people's lifespans are being reduced simply by having symptoms "too light" for CPAP. Their oxygen level isn't dropping, so they're not losing brain cells or getting brain damage from lack of oxygen. However, their sleep is interrupted dozens of times per night. Eventually, the fatigue probably causes their body to start failing in various ways after years or decades of doing that. That may be source of my "jumps." They get worse as I get more tired each day.
I have tried a lot of "tips" from various sites to improve sleep, but it hasn't helped any. I have actually gone as far as finding what are considered to be "rare" exercises developed by a few doctors for some of their patients with light/mild sleep apnea or hypopneas. Tongue exercises to strengthen/tighten the muscle (to help keep it from falling back as much while sleeping on the back), actual throat exercises to add more muscle mass and tighten the throat muscles so that it can't fall forward as much. Apparently as some people age, they lose muscle mass in the throat and it starts an onset in the 30's or 40's. I have also tried melatonin (but avoid sleeping tablets), but I don't care for how it makes me feel in the morning.
I'll see if the sleep clinic that I have been to even does CPAP trials. Doesn't sound familiar and I don't remember reading about it as part of their literature, but I'll give it a go. I feel pretty confident that it will help me with my issues. I know that a lot of people tend to think that with such a "mild/light" case, CPAP probably won't help much and isn't worth the trouble. However, when you wake up every day feeling like you've had 5-6 hours of sleep when you should have had 8-10, it becomes an issue and you start to wonder if having one would in fact help somehow. If it did work during a trial, it seems like the benefits would greatly outnumber the inconvenience of it. If I'm waking up several dozen times per night even with no low oxygen levels, no wonder I'm so tired. My eyes are puffy and look swollen every day. Contacts hurt to put in because the eyes didn't rest enough during sleep.
After some research, I've read where a lot of people couldn't even get the type of CPAP machine that they wanted. They had no say-so in it, the sleep doc wrote a prescription/brand and they didn't get what they wanted. It seems that some sleep docs get a type of kickback from prescribing certain brands. I have pretty much concluded that I would want a ResMed Auto Air 10 to avoid all of the titration and lab nonsense. Getting him to agree to that (of course he'd rather that I come in and have titration so that he could make more money for the lab) may be another story.
You've convinced me. I feel like you need to be on cpap just so you'll know whether you are right or wrong. When you're in a position of being tired all the time, you want to try anything to make it better, because it gets harder and harder to tolerate. I hope you'll figure out a way to get one. I think if you're willing to pay for a machine and you think it will improve you, you should be allowed to do it, Even it you have to do it by paying the full price of the product. I think some people are extra sensitive to lower HCIs or there's a problem that the sleep study's missing for some reason, or the sleep study caught you on the three best days of your life for less apneas. I don't think a few days is enough time to monitor sleep apnea. No two nights of sleep are the same. I've had my own AHI numbers monitored since the middle of September. That's around 50 numbers. Each one is different.
What is about to be killer is I have been hired for a very good paying job at a manufacturing company. Repetitive machine work, but 12-hour shifts. A normal work week is 50 hours/4 days and there's always 10 hours of overtime no matter what each week. Not enough direct hire employees yet, so when I get called to start soon, people are working 60 and 72 hours per week over 5 or 6 days. Definitely not a good time to have even a light case of sleep apnea. Trying to do that with 6 hours of sleep for 5 or 6 nights per week is going to be brutal. I won't have the insurance at all yet, but I may end up buying a machine after 2-3 weeks if things get too bad with my energy level. I'm thinking the ResMed Auto Air 10 with nasal pillows. Don't know anything about the other accessories yet such as the humidifier/heater for the tube, etc.
The ResMed AirSense 10 AutoSet For Her is a very good auto CPAP. The selectable For Her mode can be better for those requiring less pressure. But it can be put in standard response mode too. The humidifier is built in. About the only other necessary option is a mask, and the ResMed AirFit P10 is not a bad guess for comfortable mask. Get the Fit Pack version which comes with three sizes of inserts so you can try each and decide what fits best. The other option and is not essential is the heated ClimateLine hose. It is a nice to have, and is about $30-40 extra. You will need a prescription in the US to get the machine though, unless you buy a used one.
So the "eureka!" moment came this morning. My brain is so used to checking immediately upon awakening to see what is wrong with me and I finally caught one. I now know that my throat is closing or my tongue is falling back. I'm leaning towards the latter based on the fact that it feels like I'm choking on my tongue and I make a very odd and distinctive choking noise upon awakening. It is one or the other, which is close enough. The "pop" is apparently the pressure in one or both ears (it was the left ear only this morning), which is probably surging as air attempts to find a way out through the eustachian tubes when the airway closes. I suppose it could also be a vacuum created by the lungs in attempt to get air after the airway has closed, but I'm pretty sure that those tubes are in the upper throat area and would make that unlikely. This seems to be a back-to-back event that can happen a lot of times rather quickly once I'm in deep sleep or tired enough to fall back to sleep immediately after waking. It seemed like 3-4 times per minute this morning even after I had been up and about. Took the dog out in the yard, stayed up for about 15-20 minutes and not long after I had been asleep, I started having those events.
I don't think a legitimate device exists for holding the tongue in place so that it doesn't fall back and the mouth appliances are apparently known to move teeth and also make the lower jaw extend much further out than normal and can cause TMJ issues (which I already have some of). I see various gimmicks online where you put something on the end of your tongue that holds it in place (a little rubber thing that can't get past the lips and squeezes the tip of the tongue) throughout the night, but it looks unhealthy and uncomfortable.
My issues seem to happen when I'm on my back. As much as many people have told me that a CPAP might not benefit me, I'm going to give that a try soon. I'm a little bit of a germophobe and the idea of basically "renting" a CPAP from a sleep doctor for a trial makes me cringe and think of all of the other germs I could pick up from it if they didn't clean it properly. Given that seemingly everyone nowadays can't seem to get anything done right no matter where you go, I'd probably ask about buying one before I'd be okay with renting one. Don't want someone else's nasty head cold, TB risks or any other gross stuff I could pick up from one. I know that CPAPs only blow air out, but the thought of someone wearing a full face mask and sneezing into (and up through the line and into the machine) it before turning the CPAP on gives me the chills. lol I sleep on my back a lot and I have noticed that on my stomach and side I don't seem to have issues, but I don't want to lose my back sleeping and would rather have a machine. Will let you know how that works out when I get one. I'm sure it will take some getting used to having something crammed into the front of my nose all night. Nasal pillows are apparently for people with light/mild cases, so I'll see if I can get used to them.
I am not a medical professional, just an apnea sufferer, but I believe that the tongue is part of the anatomy that causes obstructive apnea. Generally the incidence of obstructive apnea is higher when one sleeps on their back. When you are relaxed the tongue kind of sags under gravity and can restrict or block air flow. Some even go as far as sewing a tennis ball into the back of their PJ's to make it hard to sleep on their back!
I have read a lot about that. Plus, I think my tongue is a bit "big" in general. One time the ENT doc told me that she could tell a little bit by the way that I speak that it may be a bit big and told me that I may want to see a speech pathologist. What I definitely do not want is somebody whacking away at my tongue to remove some of it or do any kind of surgery (I've read about that, too) to shorten the tongue's ability to fall back into the throat. I have also read about the UVVV surgery that a lot of apnea sufferers have where they scrape some of the tissue from the back of the throat, remove the adenoids and some other stuff. A coworker at my last job almost had her husband bleed to death after his stitches popped out and my brother had something similar happen when he had that surgery. I didn't mind having the deviated septum/turbinate reduction, but I drew the line after that.
I will eventually get a mouth guard because I wake up with indentations (teeth marks) on the top front of the tongue and all the way around it aka scalloped tongue or crenated tongue. It makes sense if my tongue is falling back because the perimeter teeth marks are from the inside as if the tongue was thrust downwards and flattened against the bottom teeth on all sides. Sleep doc told me that's a "classic sign" of sleep apnea and yet he said I didn't have it.