I cruised around reports looking for periodic breathing for a few minutes. I see where one is about a minute and a half and another is 4:44 or something like that. I also notice that they are usually at the beginning of a sleep cycle and there's not many of them. I don't understand exactly what they are though. I mean, I know they can be indicators of other issues, but what, exactly is period breathing?
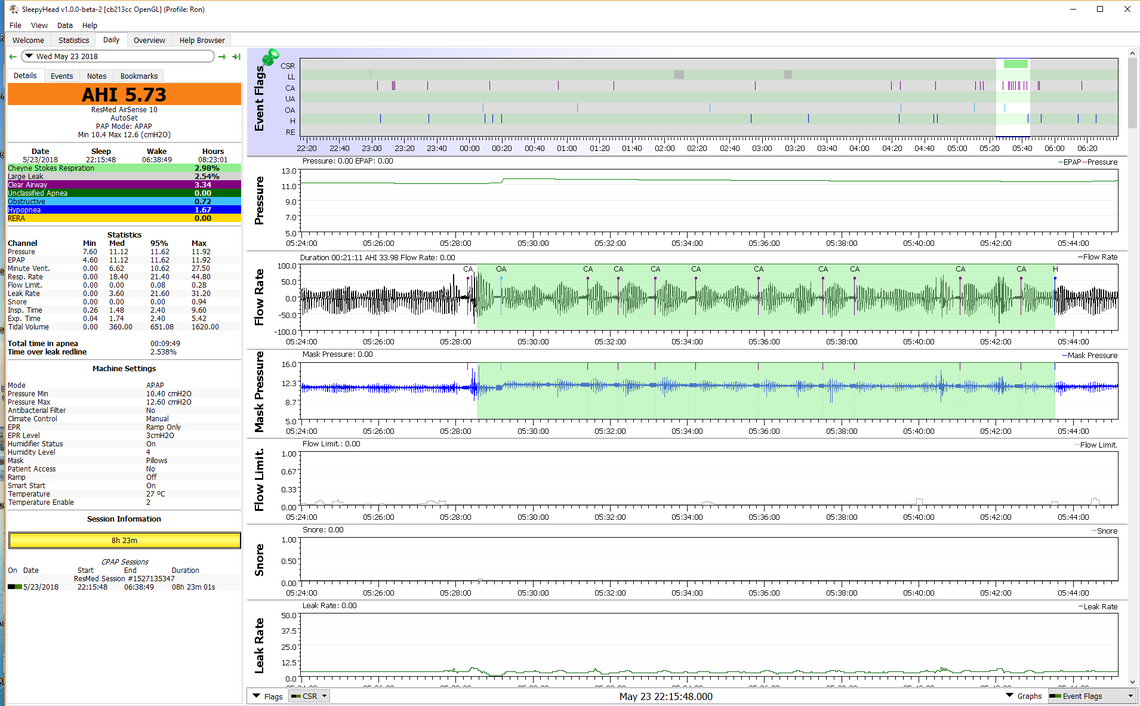
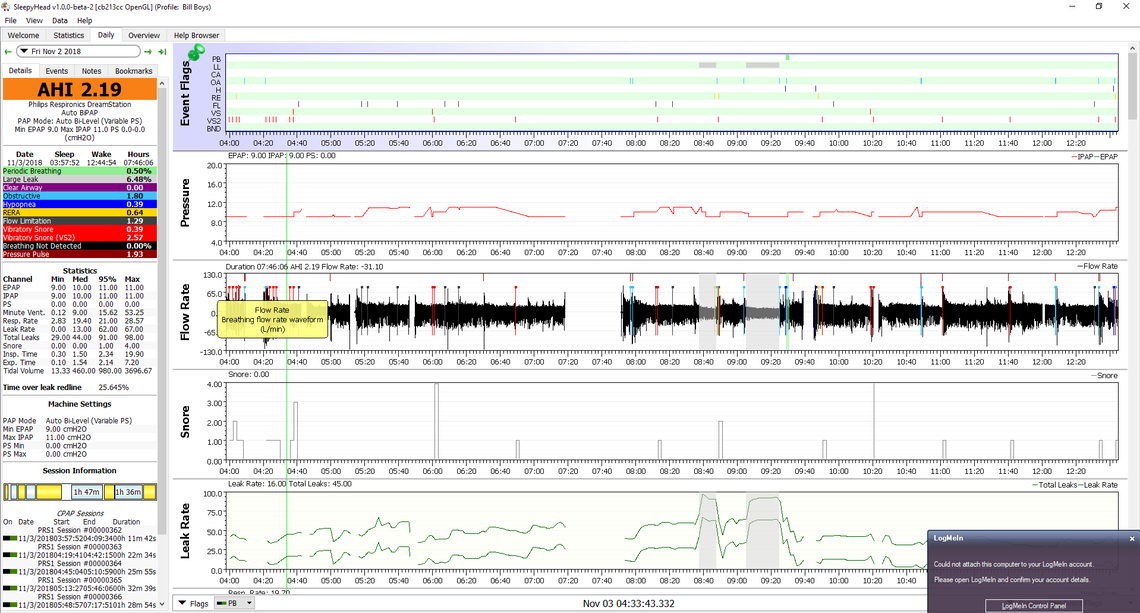
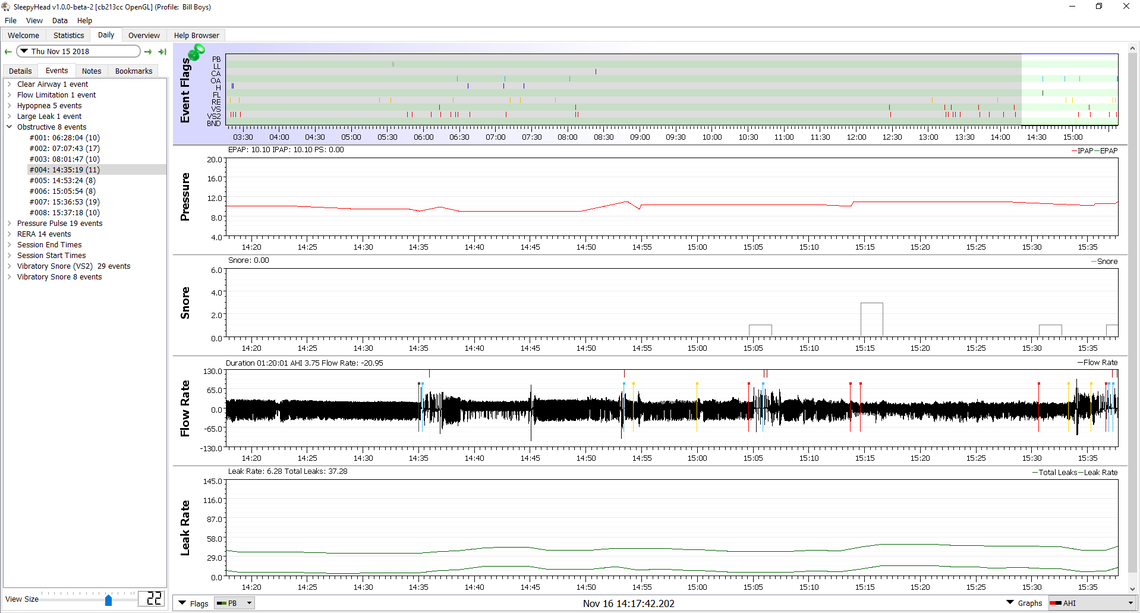
Periodic breathing is a more general term that describes a repeating pattern of breathing, and it is frequently associated with central apnea. One specific type is called Cheyne Stokes Respiration (CSR). Respironics likes to use the term periodic breathing, but I suspect they are reporting pretty much the same thing. I suffer from an infrequent and relatively small amount of CSR. I will post a screen capture below of what it looks like. Similar to the DreamStation it is highlighted in green. If yours is of this type and it becomes a reoccurring event then it is something that should be discussed with a cardiologist. One factor that could be causing it is reduced blood flow, but there can be many other reasons.
I have some experience in the field of industrial control systems, and it falls into what I would describe as an unstable control system problem -- not tuned properly. Something like a cruise control on your car that encounters a hill, slows down, then speeds up, but does not recover from the slow down speed up cycle, and just continues on for some time in the up down cycle. This can be the result of a time delay caused by low blood flow, or slow processing of the breathing data in the brain. Some drugs and especially opioids can cause the slow processing in the brain. I do not take them, and never have, but I do take a beta blocker (bisoprolol) for blood pressure which slows my heart rate down, and I have blamed it for some of my central apnea and possibly the CSR. I have convinced my doctor to reduce my dose of it in half and it seems to have helped some. I get CSR perhaps once every month or so.
I would not get alarmed at this point. It is just something to watch unless it becomes excessive. Here is a general article about central apnea which includes the issue of CSR. I'm hoping at this point that you will get to some pressure settings which minimize your central apnea. In some cases central apnea emerges as an issue in those who start CPAP treatment, but in 75% of those cases it goes away after a couple of months or so. Mine has not gone away, but I'm convinced it has reduced in frequency.
Also, My IPAP AND EPAP numbers have become so close together, they are almost cpap numbers, so my guess is 9.5 will either not effect any change or will not be good and 8.5 is more of a IPAP EPAP gap so that would be better. Neither of these guesses are rooted in science. LOL
In an ideal setup it is not unusual to have the minimum and maximum pressures close together. I currently have a minimum of 12.2 cm and a maximum of 13 cm. And before that I did about 3 weeks of essentially a fixed 12.2 cm and got almost the same results. Yes, you have a fancy machine that can do all sorts of things, but at the end of the day you may get the best results with a fixed pressure or very tight range.
On the comfort issue I do not seem to have any trouble breathing in and out against 12 to 13 cm. I assume when you say you feel like you are suffocating, it must be difficulty in breathing out?
This worthless med store owner led me to believe that basically the epap number should usually be half of the ipap number. It's obvious that he knows extremely little about how these machines he's selling, work, despite the fact that he's a patient himself. Who knows, I wouldn't put it past him to have come up with that rule just so I would buy the machine that is a "real investment' but It might be what you need." Without so much as looking at a single report. So we're on the same page now. I've had a lot to relearn. Seems like we're pretty close at 2.40. What's next, just stay at 9/15 until I can get a few good long sleeping nights behind me? That's what I'll plan to do if I don't hear from you tonight. I'll likely start sleeping about 1 to 1:30 and hopefully I won't get any interruptions like I did this morning (one stuffy nostril and an 11am phone call.
I think what we know now is that 8 cm is too low, and 11 cm may be too high. No problem trying 9 cm. I had picked 11 cm based on what the machine was doing itself in auto. At some point if you can find a pressure that is effective on the OA events, without causing you discomfort and without causing CA events then you may be pretty much there. Ideally you want to find a pressure you can tolerate all night and get a good sleep with. At that point the next step may be to start bringing the maximum pressure down to be about 1 cm higher than the minimum. That will prevent the machine from getting carried away and bringing pressure up too high.
This may take some time, and if there is no magic in between number then it may be time to try the pressure support (phase 2).
As I think about it, in the interest of trying to get you to the point of being comfortable through the night you may want to set the maximum pressure at 11 cm now. So that would be a minimum of 9 cm and max of 11 cm. If you can make it through the night with that lower and tighter setting, then we may be able to see if that is close to what will work for you in the longer term. If your AHI suffers then we will be able to see at what pressure and whether OA or CA is the bigger issue.
I have noticed that you seem to not be getting much sleep at a time and there are frequent breaks during the night. My thoughts were that if you could come up with a pressure that is as low as possible to control the obstructive apnea and not generate central apneas then the next step would be to work on the comfort issue to try and get as an interrupted sleep as is possible./
Toward finding the pressure you may want to try turning off all the session switches for that night on the left and then turn them on individually one at a time and see what SleepyHead reports for apnea frequency on each one. That may help you zero in on an effective pressure providing you were really sleeping for long enough. Then you may want to try that pressure and see if you can do a full night to gather better data.
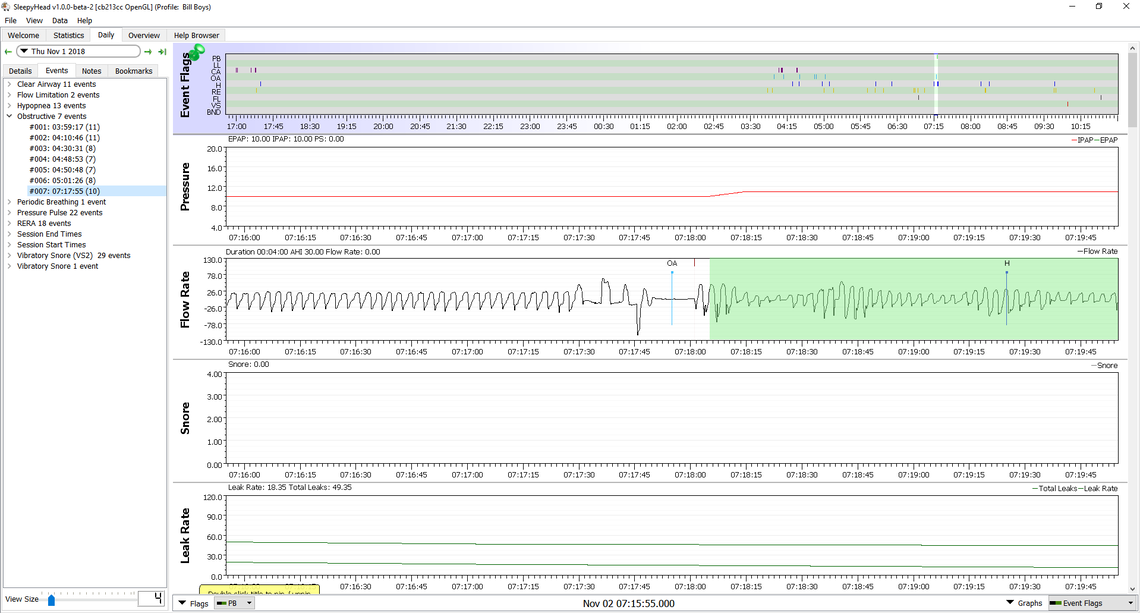
Oh, and on the periodic breathing issue, it does appear to be the control system instability issue. Your event seems to have started with an obstructive apnea which is like the sudden hill for the cruise control analogy. The upset it caused initiated a cycle in the breathing effort. In your case it is not pronounced enough to have caused a central apnea, only a hypopnea. I believe that is a good example of a hypopnea being a central event that did not go to full stoppage of breathing.
I would hope it is not serious as in comparison my periodic breathing is more fully developed, and I would suggest a little more serious looking... Something to watch, but not panic over in my opinion.
On the issue of comfort, are you using a timed ramp? Do you have a ramp start pressure set? These settings should be in the Comfort section of the setup menu. And also in the Comfort section of setup do you see a setting for Bi-Flex or Bi-Flex Comfort? Is it turned on or off and if on what is it set at?
I'm not using a timed ramp. I have never felt the need. Okay. I see what you mean about isolating various things. That's helpful. I've been wondering a long time about flex and bi-flex. The machine was preset to bi-flex on and there is a field that is labeled flex and that was preset on the numeral, 1. . The other choices were 2 and 3. Please explain bi-flex and the flex settings to me.
Using the ramp can improve going to sleep comfort if you are finding the minimum treatment pressure uncomfortable. If you need to go higher than 9 cm it may become more valuable to you. If you are going to use it I would suggest a ramp start pressure of about 6-7 cm, whatever feels comfortable to you. I like a pressure that feels like I am wearing no mask at all that is restricting my flow. If you don't set the ramp start pressure the machine will likely default to 4 cm, which I find much too low for comfort. As for time 15-20 minutes works for most. Ideally you want it to be at the minimum pressure by the time you go to sleep. Using the ramp will not affect the treatment effectiveness, and you should see the ramp effect in SleepyHead.
The Bi-Flex is a little more complicated, and I was leaving that aside until you got your basic pressures zoned in. On the ResMed machines it is a little simpler and it does affect your treatment effectiveness and the basic pressures you need. It works essentially like pressure support but in the opposite direction. It reduces pressure on exhale to make it easier to breathe out. A setting of 1, 2, or 3 is simply the number of cm it reduces pressure. ResMed call it EPR or Expiratory Pressure Relief. The problem with EPR is that it can increase apnea events due to the reduced pressure during EPAP. If the machine is in automatic mode, then it in turn causes pressure to go up, so you go full circle. For that reason using EPR on a ResMed is not a great idea unless you only use it during the ramp, which is what I do.
Bi-Flex is as I say more complicated. To my knowledge there is no way to set it so it is used during the ramp only, so you have it full time or not at all. The 1,2,3 setting is not really cm of pressure reduction like the EPR, but more like, a little effect, medium effect, and more effect. That is because Respironics do not reduce the pressure for the full exhale cycle. They mainly smooth the transition from Inhale to Exhale and vice versa. I have not seen it documented, but it is my personal theory that Flex does not impact treatment to the same degree as EPR does. However, some do think it has an impact on effectiveness. Here is a link to what looks like a quite old (2009?) document on their Flex technology.
This document shows how it affects the shape of the inhale exhale pressure. To my eye the affect is very minor, but Respironics have done studies which are claimed to show that users like how it feels to them.
So what does that mean for you? Again I think it is worthwhile to stay the course with optimizing the basic min max pressure settings first. When that seems to be working and you have a good baseline on what you can achieve for AHI it would not hurt to try the Bi-Flex at the various settings to see what it does to improve comfort for you. If it does nothing for comfort then just leave it turned off. If you feel it has improved comfort then leave it at the most comfortable setting and try it for a while to see if it has any negative impact on AHI. The objective is not only to get a low AHI but also equally important to get a long uninterrupted sleep. If the Flex can help get your there with no impact or very minimal impact on AHI I see no reason not to use it.
Thanks for the education . At this point, I couldn't imagine more comfort just the way it is. It's like the machine is hardly doing anything at all. This is probably because I was at 10 epap and 20 ipap for three months. By comparison, it's like someone was pressure washing my sinuses. Last night's report will follow this message
The provider preset biflex to 1. You said it brings my epap down one, and since I don't need that for comfort, It's better that I shut it off. Seems like a little troublemaker. I have shut if off. It seems like you've already suggested that. Just let me know if I'm wrong.
Wait. Am I soaking this in correctly? Bi-flex or C-flex brings epap down to eight, If I set epap at 9 and Bi-flex at 1? So Bi-flex set to a "1" position would be the same thing as shutting Bi-flex off and just setting epap at eight? So then what's the point of Bi-flex on the setting of Bipap or auto Bipap? You can set expiration at what you want to set it on anyway. Which brings me to the following point: Based on what I just said, by just now, turning the Bi-flex off, and leaving the setting on 9, I have, effectively, made the machine one numeral higher. Previously, it was set on 9 with a 1 Bi-flex, effectively making it an 8. Now, It's an honest nine. Seems to me, that I should change that 9 to an 8 for the machine to perform like it did last night. Correct or am I confused?
I went back and re-read and it made me even more firm on not using Bi-Flex...At least, like you said, until I get the ideal AHI plugged in. Since it's not like the ResMed, which takes the pressure down 1, 2 and 3 centimeters, and is instead more like low, medium and high, its vague how much pressure it gives you. I think, once we focus in on THE AHI number, I can use different flex settings, noticing the next day through the data, what the actual cm pressure difference is.
SUCCESS! I thought that it might be going along with your philosophy, to move EPAP from 9 to 9.5. My opinion is that IPAP doesn't need to change. Please let me know if you think that's okay. At this point I want to make sure I do exactly whatever you think I should do. I have this crazy urge to bring the AHI as low as possible. I would still be struggling if you never decided to help people in this way. I know it takes up a lot of your time and I appreciate it more than I can express. You're helping me live a life I didn't know I could live 3 months ago.
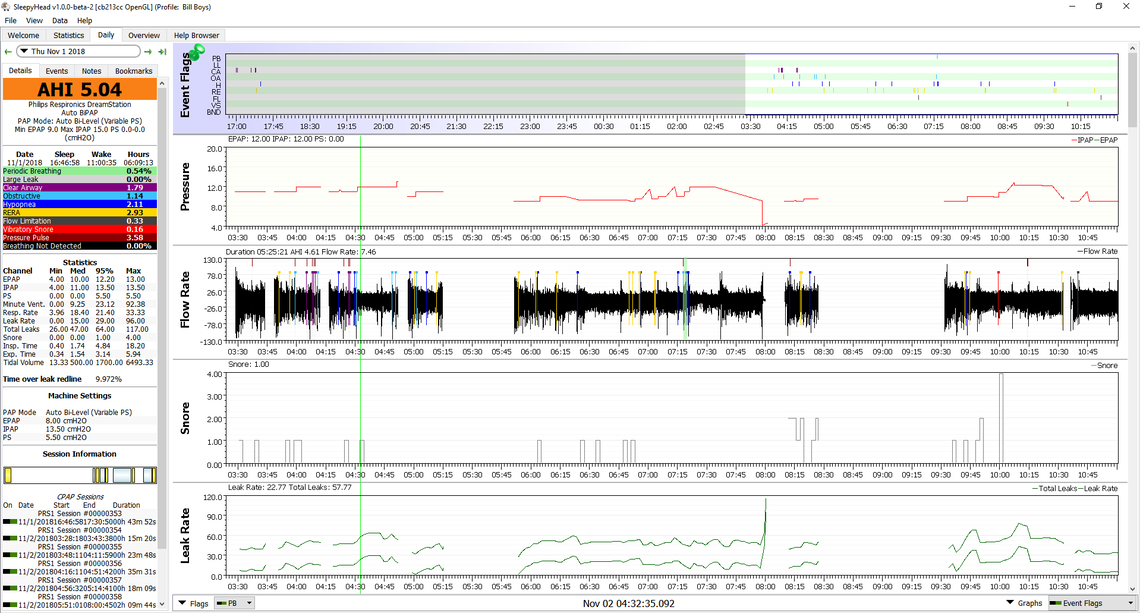
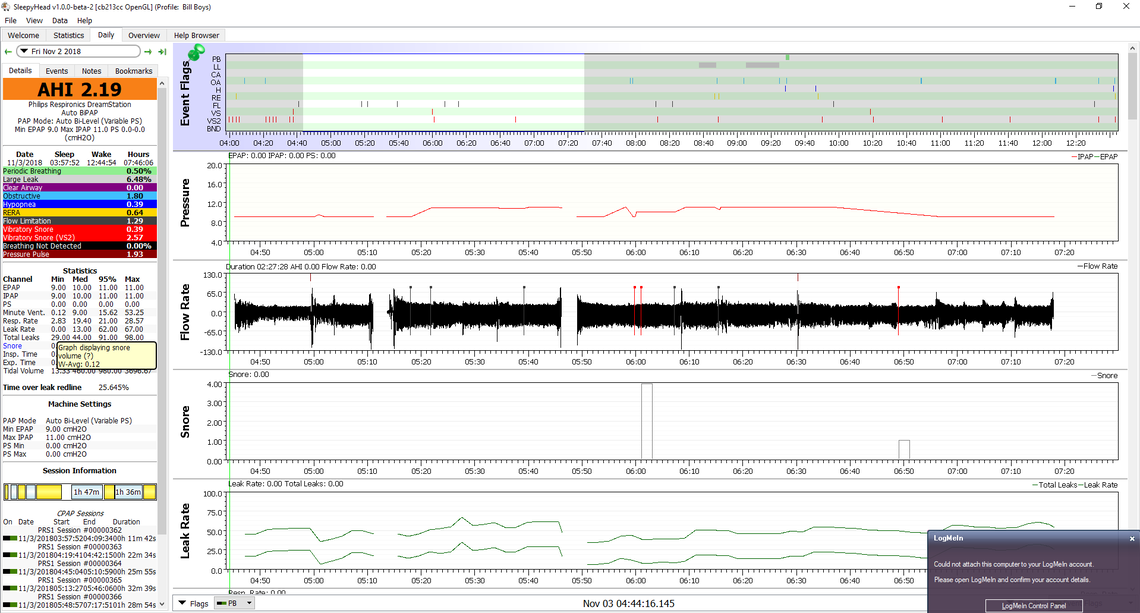
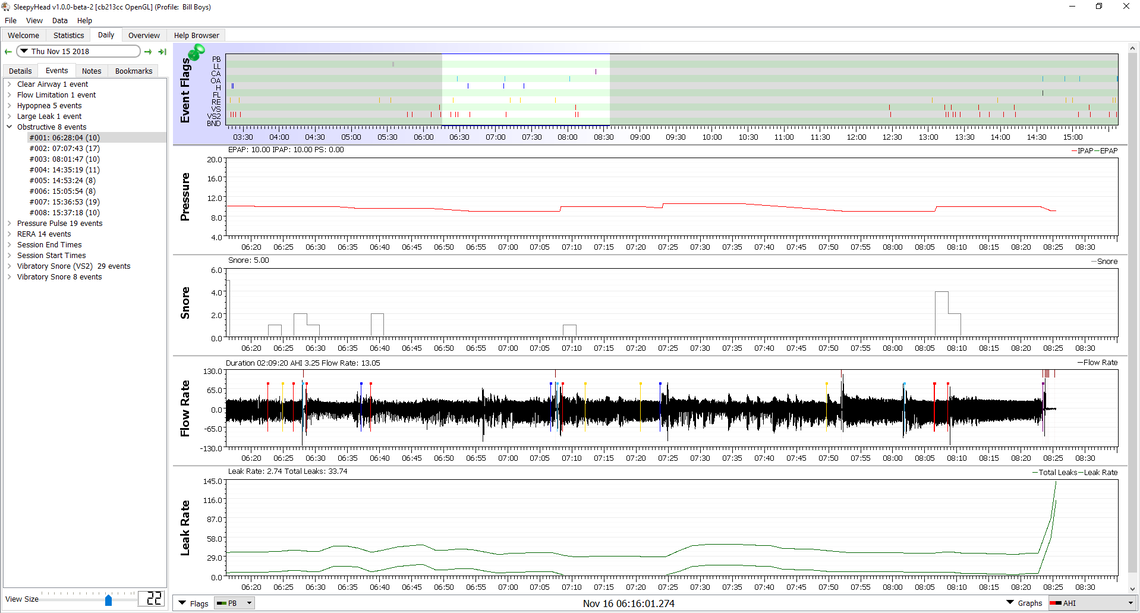
What I like to do, when using SleepyHead is just mouse over the OA events in the flagging bar while watching the pressure chart and in particular the numbers just above the left end of the Pressure chart that give the EPAP and IPAP where the cursor line is located. This will let you either mentally or by taking notes on a piece of paper identify what the pressure was just BEFORE the event occurred. It is not a perfect process but when I have a new pressure in mind, I keep track of how many of those events potentially may have been avoided with the higher pressure.
I tried to do that by eye with your charts, and as close as I can see, I would agree with you about changing the set pressures to 9.5 min and 11 max to try it. I think you may prevent a few OA events.
It is really encouraging to see that you got zero CA events. It would seem that preventing pressure from going above 11 cm may be preventing their occurrence.
The leak rate at times is a bit high, but overall this is so much better than where you started. For now I think the only change needed would be a 9.5 cm for a minimum.
It was easy checking the pressure. It goes into OA when both epap and ipap are on 9 exactly. Maybe 20 percent 10 and then one OA is at 10.5. Pressure never got beyond 10.5 and both epap and ipap were at 9 the majority of the time. That was with Bi-flex on 1, epap on 9 and ipap on 11. Automatic bipap, of course. Tonight I have changed it to no auto bipap, no Bi-flex, epap on 8.5 and ipap on 11.
Leak rate will be improved. I'll secure the mask just a touch more. Oh here's something weird. I notice that when the leak graph starts to climb, the AHI graph starts to drop. To me, this indicates, like before, that there's too much pressure. It seems logical and makes no sense at the same time. When leakages starts becoming a hill, AHI becomes a valley.
I am very pleasedwith no CAs too. I didn't think that was even possible. I stayed kind of groggy today, but I think the extra oxygen to my extremities has started to release this pain in my should that was bad enough for me to wonder if it was bone spurs. It's amazing how much better it feels. I'm looking forward to restorative sleep.
Probably too late for tonight, but I would set pressure minimum at 9.5 and leave Bi-Flex where it was. Not a good idea to change two things at once.
Totally agree. It could be a major set back in the face of a break through. Okay. Bi-Flex on 1, epap to 9.5 and ipap remains 11. Makes sense to keep it like that even though I'm curious about the results of 10.5, Ipap. Maybe later. I will be asleep by 2 am which will, by then, essentially be, 1am, since we fall back.
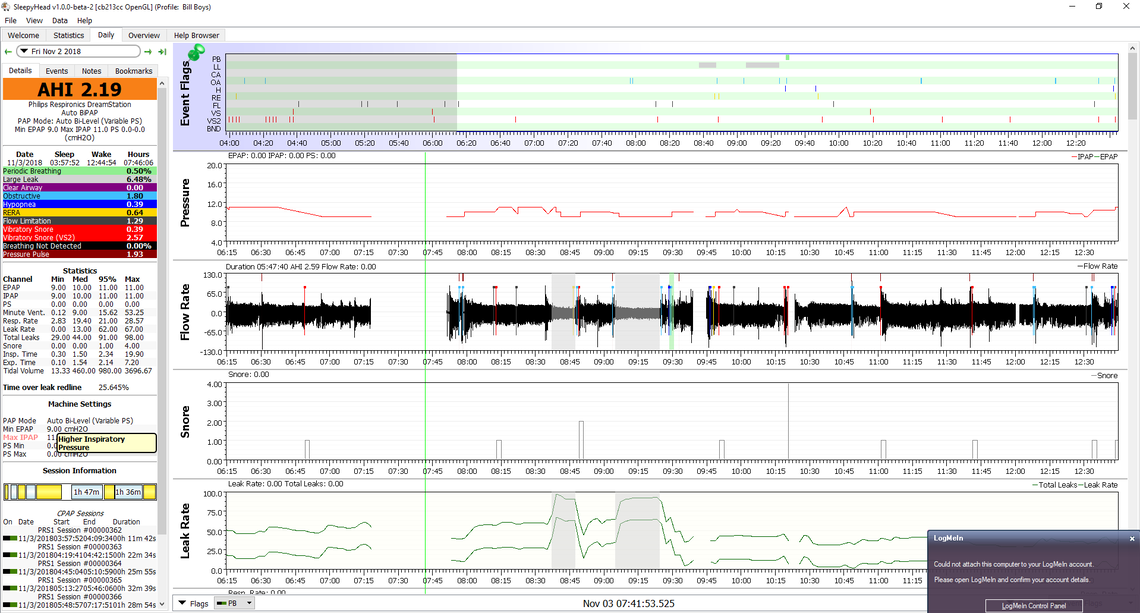
Okay. Tonight's a waste, partially to this 9.5 epap, and partially because I can't sleep, so I'm going to change the settings. I've been comparing tonight's brief report with yesterday's success, There are some things I observed that lead me into thoughts of changing EPAP and IPAP. 1)AHI stays lowest with a 9 Epap. 9 epap tends to hover around 1 and 2 AHI, 9.5 seems pretty stable too, but 9.0 has been the champ, so I shouldn't exclude it as a minimum. Also, just from looking at the graphs, I get the feeling that 9.5 Epap is , sort of pushing the IPAP as high as possible (11) and 11 is four time worse for AHI as 9. So my opinion is a range from 9.0 Epap to 10.0 Ipap, with 1 Bi-Flex, is where our next test should be. I believe it's possible that a 9.0 Epap and 9.5 Ipap could be the sweet spot, but I prefer to work in the gradual mode. May not seem gradual by going from 11 to 10 instead of stepping it down to 10.5 Ipap. That's because I haven't seen a favorable AHI during a 10.5 pressure, so why go visit the disaster? Also, as I said before, leaking masks produce lower AHI. Seems like too much pressure. One more thing. It's only hypopneas that survived tonight. That makes me think that the airway is being cleared too well. Pressure is too high. Both Epap pressure and Ipap pressure. Going back to sleep (briefly, because of job) and setting the auto bipap to Epap: 9, Ipap 10, Bilflex: 1.
The good news here is that CA is still zero. It is possible the hypopnea events are central apnea related though. You would have to zoom in to see what they look like.
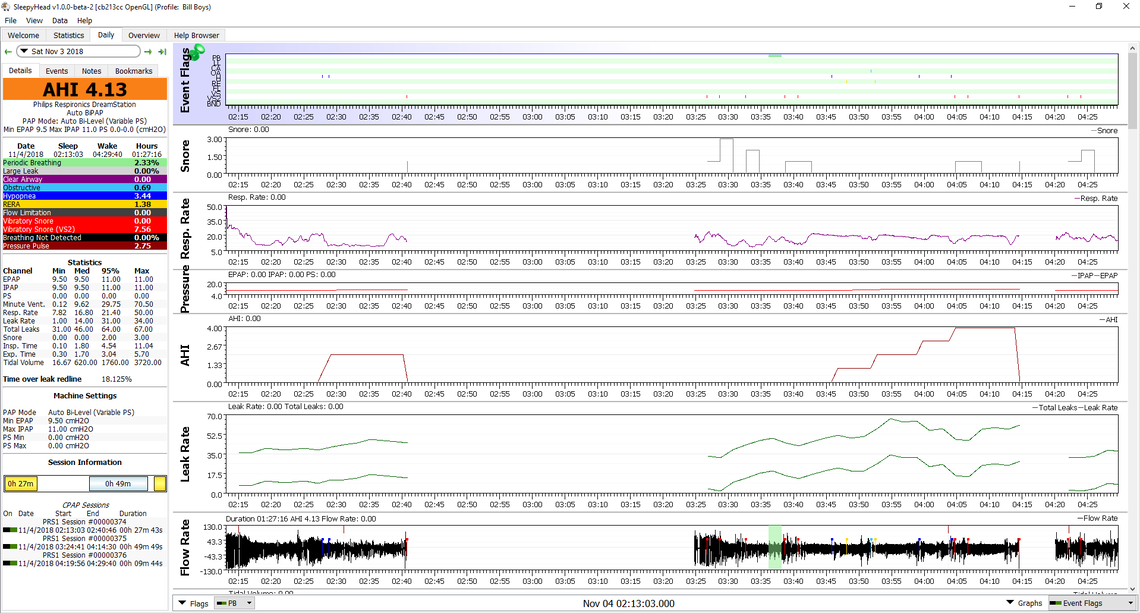
Some things to keep in mind in this. You have made very rapid progress, and are now at the point of making some pretty small changes. When you make a small change, you probably have to try them for a week or so before you can be sure what effect they have. It is kind of like changing the brand of your golf ball, playing one hole, and then trying to decide if it is better or worse. I have been averaging about 2.3 AHI for some time now with my latest settings. Last night it was 4.3. I had changed nothing other than we added a quilt for the winter and it may have been too hot...
In general your CA is zero so that suggests at first blush that pressure is not too high. Your OA is 0.69 which all considered is pretty good. That suggests your minimum pressure is not too low. The only remaining issue is the hypopnea. I would be suspicious that along with another green band of PB indicates central apnea may be at work but not just causing a full CA. I have to admit that when I see CA low and OA low, I kind of ignore the hypopnea, or at least give it a lower weighting for concern.
I see you have moved the AHI graph up. I find that graph somewhat misleading and not all that useful. My preference is to look at each event and see at what pressure was there before it occurred. That is why I put the pressure graph right below the events, and mouse over the cursor to see the digital display of pressure above the graph. It tends to be more accurate than trying to read the graph directly.
You said "So my opinion is a range from 9.0 Epap to 10.0 Ipap, with 1 Bi-Flex, is where our next test should be."
I think that is as good a setting as any from what I have seen so far. It would be worth trying that for a few days without making any other changes to see what it produces. Perhaps just leave the settings at that and post your daily screen each day to see if there is any kind of trend to the results before making any other changes.
I was moving the AHI up, just to have pressure, leakage and AHI together, since I was comparing them. I will go back to normal before I send you anything again. When I went to 10 Ipap, AHI went to 4 and I couldn't stay asleep. Same thing with Ipap at 10.5. Unfortunately, I can't get SleepyHead to download anything, so until I figure that out, I'll use the much less reliable dreammapper that just gives you almost nothing, but, at least it keeps up with the three AHI fields. Hopefully, I can fix it today. I have another computer, I can download the software on. I ended up back at 2.1 AHI after I returned to ipap of 11 and kept epap at 9 with bi-flex at one.
I went back to the Dreamstation and couldn't find anything to indicate a way to lock the sd card from the Dreamstation. The card is lockable by using a slide on the card. Could it be that only my provider can lock it and that he has done that? Not sure why he would do it, but I've looked all over for it and can't find anything.
Okay. I've been very tired lately. I'm going to leave the machine at 9/11-biflex-1. I slept fifteen hours total yesterday. I'm gonna take a couple of days off of experimentation to just leave it on that setting and be sure to get some sleep. I'm very interested in seeing if I can continue to bring my numbers down, but I know now that I have the machine to the point where I can get a lot of good sleep and I need that right now. I'll come back and attack the rest of this sometime later this week and I'll be more clear headed, and maybe less manic about it.
It is always good to get a few days of data without any changes. It gives you a benchmark that you can always come back to if further changes don't work out.
Good. I slept 13.33 hours (too long afternoon nap plus a very long nights sleep. According to Phillips dream mapper, I had 100 percent mask fit, my AHI was 4.5, 4 CAA, 39 OA, and 18 Hypopneas. I would hate to lose all that info that's in the SD card I can't download. I'll get creative and figure something out with it once I start getting benefits from this current auto bipap setting. When I feel like doing things, from being better rested. It hasn't escaped me that this rest I'm about to be getting is mostly due to your insight into a science that baffles medical professionals.
Oh...I have had very slight problems with my left nostril getting plugged up completely and a kind of weird scratchy throat, plus other things that would create an AHI reading twice as high as before with the same settings. My environment wasn't perfect. Maybe tonight will be better.
One of the things I do is to try and get my nose clear before I put the mask on. Early on I bought a container of the Walmart generic equivalent of Otrivin nasal decongestant. This type of drug cannot be used continuously or it loses effect. So what I do is only use it once occasionally at night only and in one nostril only. It helps to get cleared up before going to sleep or shortly after. I find with a nasal pillow mask once you get your nose clear it stays clear overnight.
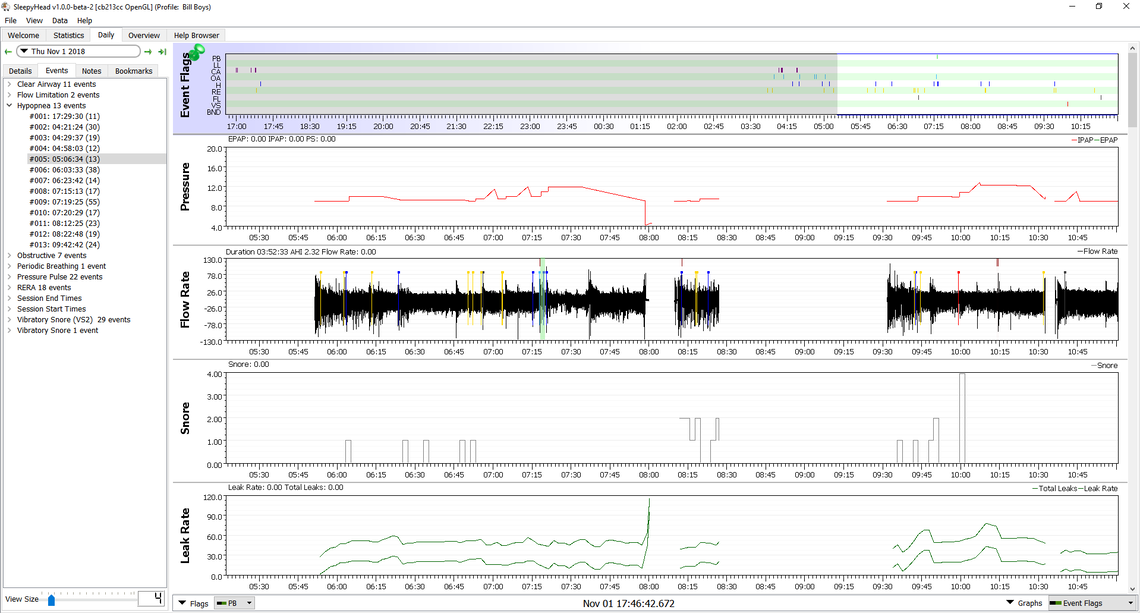
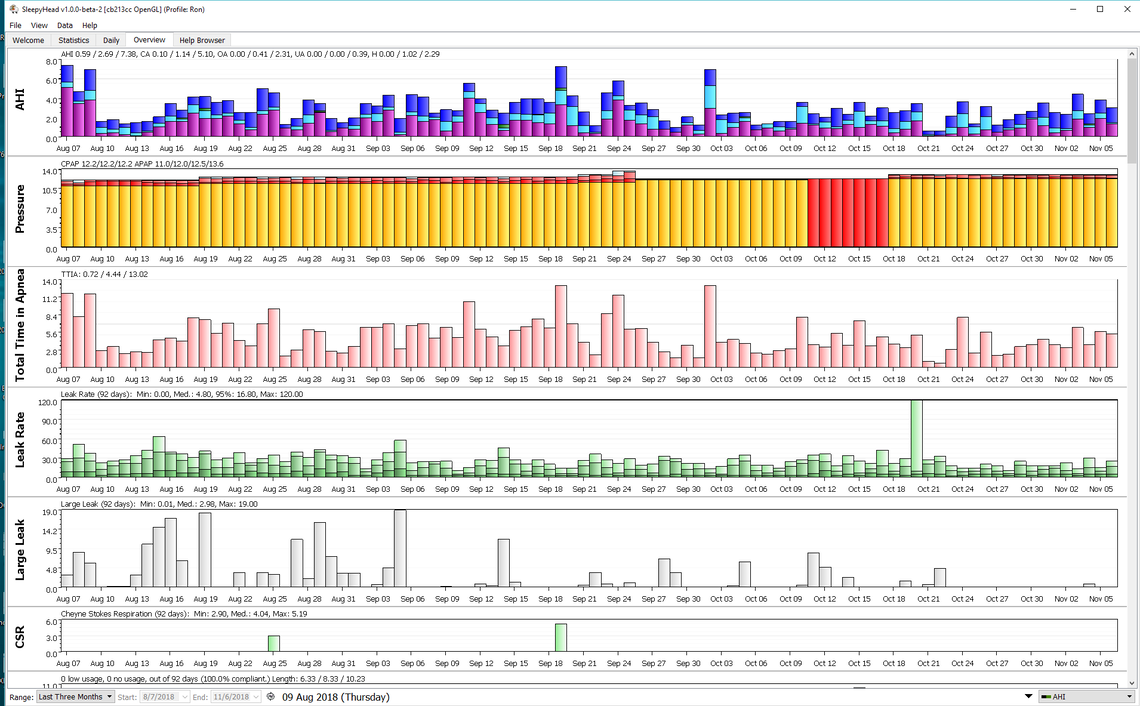
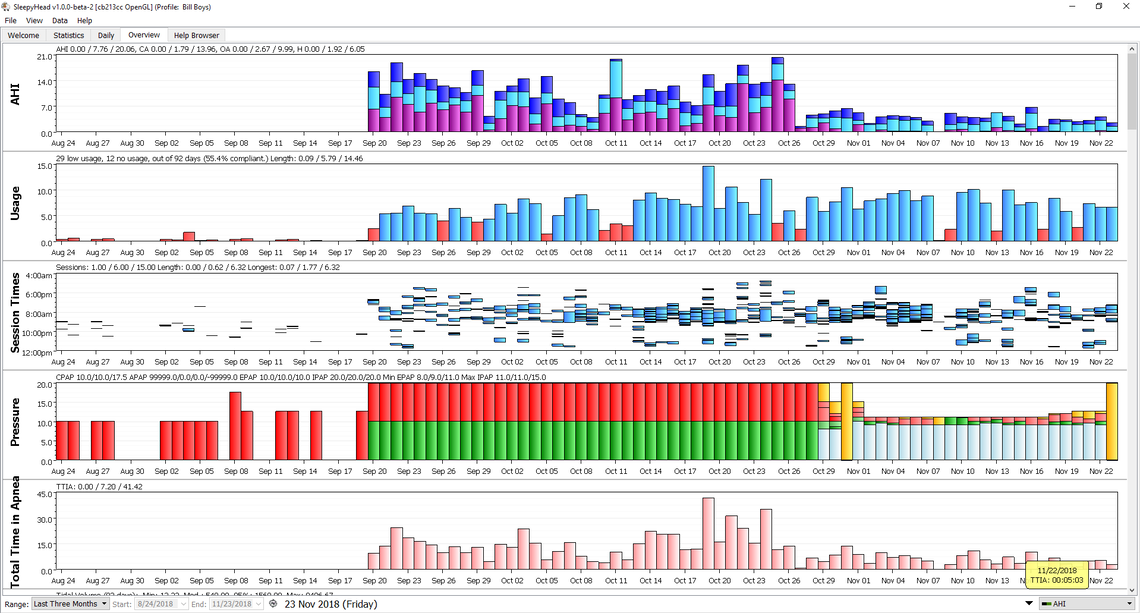
One thing to keep in mind is that with apnea and in particular complex apnea with a significant portion of central apnea one night to the next night variability can be quite high. In statistical terms standard deviation is very high. It takes many nights to see if there really has been a change in the average results when you make a change in treatment pressures. As an example I will post my last 3 month Overview from SleepyHead. I suspect my apnea severity and yours are not all that different, so my guess is that your long term ability to control AHI is likely to be quite similar in variability. This Overview includes my last three changes to treatment which in the scheme of things are pretty small.
Sep 26 - Oct 10 - Pressure at 12 min and 12.2 max essentially fixed - AHI 2.34
Oct 11 - Oct 17 - Pressure in CPAP mode fixed at 12.2 - AHI 2.64
Oct 18 - Nov 6 - Pressure at 12.2 min and 13 max - AHI 2.49
So on average pretty subtle changes. However over that time AHI has been as low as 0.6 and as high as 7.0. So I guess my point is that don't take one or two bad nights as a trend. You need quite a few nights at a setting to see what it will do in the longer term. I think it makes sense to make changes fairly quickly at first, and then after you get close to the optimum settings, then slow down and be patient to see what is happening. Hope that helps some. You have come a long way from the first settings you had, and have made excellent progress!
That's very helpful. I totally agree with you as far as how far I've come in a short period of time. It's very good to know I'm at a safe AHI. It only took us a couple of nights to get to less than five AHI. It has been hard for me to sleep through the night, but then, that's an old habit. Maybe in time. I'm willing to try anything you might suggest, including moving to the one of the other modes to see if it there are better settings that will drop my AHI. That includes raising or lowering pressure settings. I don't believe I gave that a fair chance, because a good night's sleep became more important. We are of the same mind when it comes to keeping this exact setting for a while. I see what you mean with all your ups and downs. I got a new SD card reader which fixed the import problem. In just a minute, I'm going to sent last night, separately. By the way, the next three nights might be useless as far as data because I'm taking care of my daughter's dog's and I'm mildly allergic. Enough to disturb my sleep.
Just a little update: I've had a toothache that kept me all night, was babysitting daughter's two dogs and I'm mildly allergic, have had blockage in right nostril that wakes me up or doesn't allow me to sleep. I think the season change is part of it. True to form at this time of year, I'm getting slightly wheezy. All these things on a consecutive day basis has made data useless. This is not ordinary. I'm not gonna waste your time until I can get back to more normal sleep. It's just been weird. Still, I pretty much stay under 5 AHI when I DO sleep and generally, I have zero CAAs. Plus, I'm tired and don't feel like doing much. Not negative though. Counting my blessings. Anyway, I'll send you some data, when my sleep settles down. Meantime I'm unchanged: 9.0-11.0. No Bi-flex, no PS. Auto Bipap.
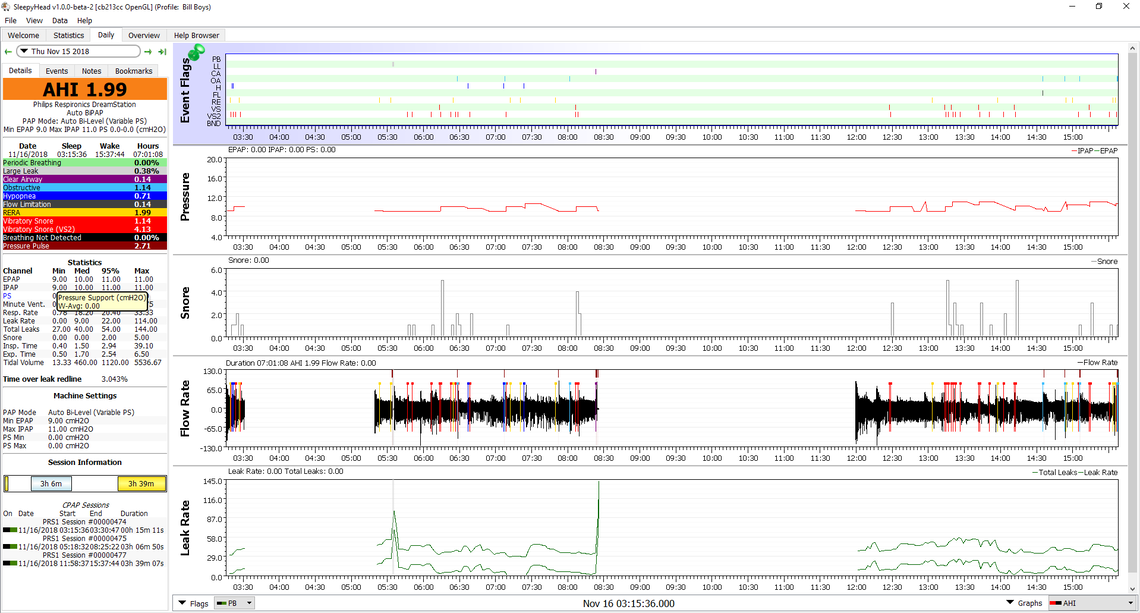
I think for someone with mixed apnea this is a pretty good result. You are probably not far off an optimum pressure setting if this is a typical result. Your CA event frequency is very low. I cannot achieve that on any kind of consistent basis. This indicates to me that (again if this is typical) your pressure is not too high. Your OA events are now dominating the total AHI. That suggests your pressure could be allowed to go slightly higher. However, that said, I would not be too quick to increase the maximum pressure setting. You are in a pretty good place now. It may be time to focus on the comfort issue or whatever you think may be preventing you from getting a 7 to 8 hour sleep at one stretch.
So right about comfort issue. It makes sense. Gotta figure out some way of getting more time out of it by being more comfortable. 1.99 AHI is not common. 3.4 is more common, but if I can manage to not get a clogged nostril, 1.99 is easier. I think my nostrils are always inflamed and it doesn't take much to close one up. I take Claritin D to clear my airway and because of some bad nights, I've added Flonase. I want to ditch the Claritin D and just stay on the Flonase, but since I just started on the Flonase, I'm not gonna rock the boat just yet. I'm open to any ideas on how to breath better on the machine. I just realized that there's enough room in my mask to use a Breath Right strip and I've been doing that with some success. Change of seasons has created a few congestion probs.
I just looked back for the first time in a while. I haven't had much of value to send you because there's something about this change of seasons that's causing my nostrils to clog. I've been lucky to get two consecutive hours. My breathing is so erratic, it's hard to pile up usable data. Last night (hated to do it) I added Afrin to my allergy regimen. I slept for 6 and a half hours, but more telling is that I slept 5 hours in a row (minus a bathroom break). I am only using one squirt and only using it if a nostril clogs up. I used one squirt per notril last night. I had a 2.32 AHI which is the second lowest I've produced. I've had some lower numbers but I don't count a two hour nap. Last thing I want is to be dependent on Afrin. Hopefully whatever is in the Middle Georgia air right now is going to pass soon. If my nose is completely clear, I think i'm about a 2.0 AFI patient, which is obviously great. I'm not positive the Flonase is helping and may drop it. I certainly don't need to be on three different medications if I can help it. Hope YOU are sleeping well.
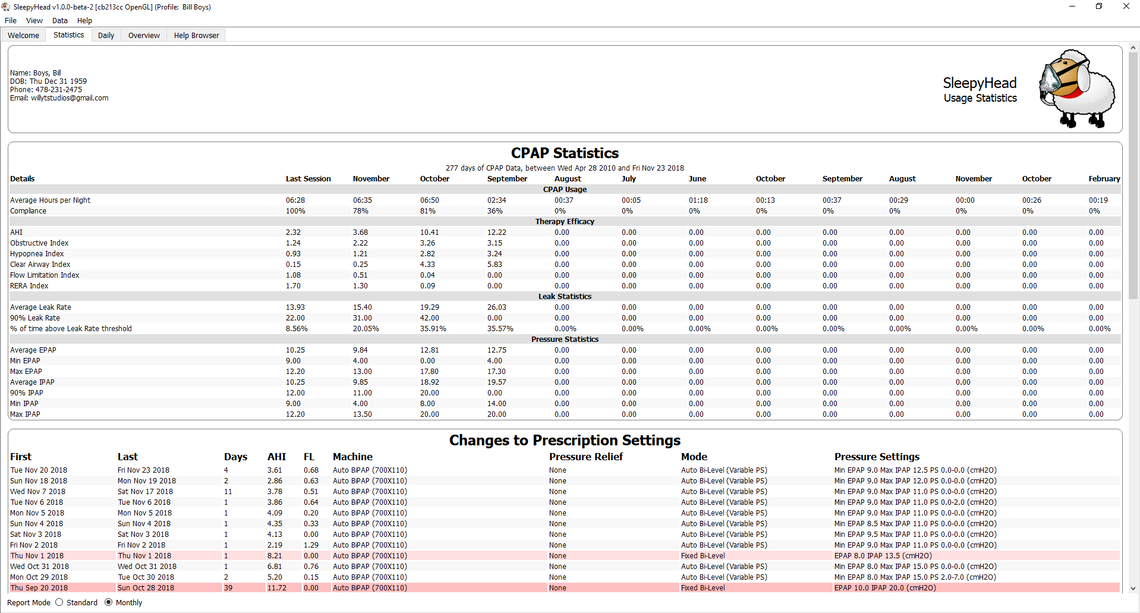
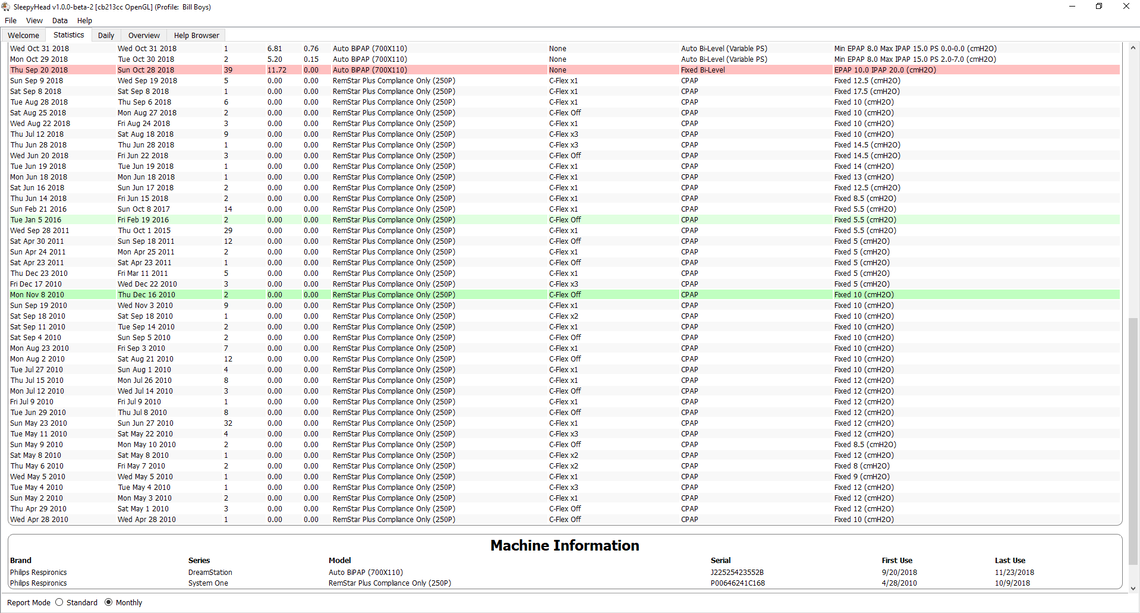
I believe I've mentioned how I don't trust the guy who runs the medical supply store that I've been getting my cpap supplies from. He sold me a DreamStation for 1400 dollars and told me I was getting a good deal. He never told me he was selling me a used (possibly refurbished) machine. I'm not sure I'm right, but I started using this unit in the middle of September of this year, but there is certain information that goes back to 2010. If I have any recourse, I surely would like to force this guy to give me a proper discount since he was dishonest and since a used unit goes for so much less. Do you know, if I can prove that this is a used unit with the information I'm sending you. If not, can do you have any ideas on how I can find out. This guy keeps looking more and more like a sleeze to me.
The Overview graph shows you have made a pretty significant improvement since Oct 27. One of the things I have been trying lately is using a fixed CPAP pressure. To date I have tried 12 cm, 11 cm, 10 cm, and last night 9 cm. I have been expecting to see a big jump up in obstructive apnea as I go down in pressure. So far I have not seen it. Last night at 9 cm I was under 1.0 for OA. CA was still a bit high though. I am going to try 8 cm tonight to see what happens. I saw a bit of snoring showing up last night at 9 cm so I may be getting near the limit for reducing pressure.
See my other comment on the old setups. I think you may be seeing the data from a previous machine you have used.
Bill, I am going to be away for a couple of weeks, and may not be checking in. Lately I have been trying a fixed CPAP mode to see what it can do compared to giving the Auto mode a range and letting it adjust pressure. My pressures run about the same as yours do, and in the past I have gone as high as 15 cm. But when I have done the fixed pressure testing I have gone as low as 8 cm. It didn't turn out real well (AHI 6+), but with 9 cm, 10 cm, 11 cm, and 12 cm, there is not a huge difference in AHI. It seems to be a bit of a mushy range where the proportion of central, obstructive, and hypopnea events show no real clear trend, and the total does not change much. But one of the things I have learned is that you need a lot of data to determine what pressure is best. 2-3 days is not enough. My thoughts now are that you need 2 weeks minimum at one fixed pressure to try and evaluate what it can do. So it would take a long time, but you may want to consider trying two weeks at each single fixed pressure for 8 cm, 9 cm, and 10 cm to see what may work best for you. I think there can be some comfort as well as AHI advantages of using a single pressure over an automatic range. For example if all of those pressures give you basically the same total AHI, then why not use the lowest one, and get more comfort?