Hi All,
A longer introduction below, but I'm interested to know how many people have seen real-world health benefits from CPAP, other than reduced fatigue, that can be objectively measured with blood tests etc.
I was referred for a sleep study as I suffer from type 2 diabetes, hypothyroidism, hypertension, obesity (31 BMI), polycythaemia and elevated haematocrit, high triglycerides and low HDL cholesterol as well as low testosterone. The doctor who referred me felt that the only way all of these can come together is due to OSA and that treating this will resolve a lot of these issues. Therefore my question on how many people have actually seen a positive change in blood test results after 90 plus days of use.
During the sleep study done in May 2017, I was diagnosed with severe obstructive sleep apnea, AHI 31.5. Due to the quality of the sleep study, which by the looks of it from other's comments here are pretty standard, I wasn't convinced that CPAP was really indicated. My reason for this was that the study found only 2.9 events per hour of obstructive apnea when on my back (NREM) and zero for other positions, including during REM sleep, for an average of 1.1 NREM and 0 REM. The hypopnea events though was a lot higher at 31.9 NREM and 26.7 REM. The thing is, I don't sleep on my back and the NREM OA events of 2.9/hr was actually while I was awake, waiting for day to break.
After subsequent visits to an ENT and a pulmonologist, both recommending CPAP, I decided to take the plunge. Interestingly enough, and admittedly after only three nights of use, the machine reflects similar findings to the sleep study with an average of 0.43 obstructive and 0.73 hypopnea events. However, the clear airway events are 4.57 average, pushing the AHI up to 5.73. The sleep study didn't recognise any of the hypopnea events as central apnea but again understand that often happens with sleep studies.
I started using a ResMed AirSense 10 Autoset with N30i nasal mask three nights ago, but have done a lot of reading on machines, masks, OSA etc. before the time and found this forum to be a fantastic resource. We're currently still fine tuning the settings on the machine, so hopefully the central apnea events can be reduced while maintaining the obstructive and hypopnea events at a low level.
What makes life more complicated for me is that I work at an altitude of 2,200 meter (~7,200 foot) above sea level for up to 16 days at a time, with a break of 7 to 10 days at sea level. This also has an effect on my polycythaemia and elevated haematocrit, as the wonderfully adaptable body adjust for the lower level of oxygen by creating more red blood cells.
I also have Type 2, hypertension, obesity and was diagnosed with a 37 AHI sleep apnea. My red blood cell count, and hemoglobin always comes back just under the lower normal limit. I don't have hypothyroidism, or high triglycerides. I take Crestor to get my LDL under the limit for Type 2's. I might meet LDL normal limits without a statin. My Type 2 is well controlled with metformin and insulin. And my hypertension is also well controlled with meds. I've been on the CPAP for about 9 months now. I can't say I have seen any significant differences in my blood test results which I get done every 6 months (last about 3 months ago). When I was diagnosed the sleep tech tried to tell me that a CPAP would cure my diabetes. I told her that I thought that was total hogwash! My insulin requirements have not changed at all under CPAP treatment.
On the sleep test results, while I think it is possible (but difficult) hypopneas are not usually classified as obstructive or central. The central portion of my diagnosed AHI was very low. However with CPAP treatment it emerged as an issue. During my trial period on the CPAP I think I averaged about 4 AHI with most of it central. This sounds fairly similar to your situation. Over the last 9 months I have tried a lot of different settings (about 30 or so) with my AirSense AutoSet machine, and I now have my AHI on the latest trial under 2. Everyone is probably different, but the secret for me has been a switch from Auto mode to fixed CPAP pressure mode.
If you want to post some SleepyHead Daily report screen shots I can give you my thoughts on where your opportunities may lie for improvement. SleepyHead is free to download software that displays your sleep data from the SD card in your machine. You need a PC or Mac and a SD card reader. All your data since you got the machine should be on the card. Do you plan to adjust your own machine, or work through your sleep clinic?
I certainly would be interested in knowing how your results change at altitude compared to sea level. I have had a theory that higher elevation makes the frequency of centrals worse. We recently spent 2 weeks at sea level compared to our normal 2000 feet at home. There seemed to be a small improvement at sea level, but not sure it really statistically significant.
Hope that helps some. If you have any questions just ask.
Edit: Here is a link to the thread where I somewhat documented my journey to using fixed pressure CPAP mode. Oh, and after I thought about it a bit longer, I have made one change in my medication since starting CPAP. I did a trial and then convinced my GP to cut my beta blocker blood pressure dose in half. It seemed based on my trial that the lower dose reduced my central apnea frequency.
Good to get some real-world feedback. I was also told CPAP will cure T2DM and also laughed it off. The biggest driver for me starting to use CPAP is the polycythaemia, as this is apparently quite dangerous and can cause heart attacks and strokes due to the increased viscosity of the blood.
I couldn't tolerate metformin due to severe gastric symptoms so switched to dapagliflozin. The endo then added liraglutide, which dropped HbA1C it to just above the 'very good control' level. The great side effect of the liraglutide is assisting weight loss and it also appears to have a positive effect on cholesterol and triglycerides, as well as blood pressure. My total cholesterol and LDL is well within limits, despite the elevated triglycerides.
Although I've only used the machine for one night at sea level and two nights at altitude, there is about a threefold increase in CA events at altitude. There's quite a bit of literature on high altitude CA, so I suppose it isn't too unexpected.
I'll post some SleepyHead shots when there is a bit more history. I read your very good explanation on your journey and will probably reduce the pressures to see if the CA events reduce, but altitude may be the enemy here.
Your two elevation work and living arrangements may provide a bit of a challenge to get your machine optimized. It may be that you will have to use two different pressure settings; one for sea level, and one for the 7200 feet. I think with complex or mixed apnea the pressure settings are almost always a compromise as they can go in opposite directions with increasing treatment pressure. The compromise pressure may be different at sea level compared to at elevation. One would think in Auto that the machine would be smart enough to automatically compensate. However, it is just my personal theory, but I feel at least in my case, my machine chases hypopnea with pressure increases. That is fine if the hypopnea is obstructive. But if it is central it makes things worse. For that reason the machine may not work that well in auto mode.
I found this blog article at this website quite informative on the subject of complex sleep apnea. He mentions the use of acetazolamide to treat central sleep apnea. Apparently it is used to treat altitude sickness and is off label in treating central apnea, but there is some indication it works. It is a diuretic like some blood pressure meds. I have thought about asking my doctor to switch the beta blocker for the acetazolamide. But, my research indicates it is probably off label to treat blood pressure too, so it would be asking him for a lot. I've put that idea on the back burner now that with a lower fixed pressure I've gotten my AHI down to what I consider an acceptable value. For December my central index was 0.45, obstructive 0.34, and hypopnea 0.79. I suspect about half the hypopnea is central apnea related. If that continues, I'm OK with that.
Another thing to watch for is Cheyne Stokes Respiration. Your machine and SleepyHead will flag it if it is an issue. I have been seeing a bit of it about once a month. However over the last 3 months or so the frequency seems to have dropped. I have not had it since I went on the fixed 11 cm CPAP mode over a month ago. I'm hoping the lower pressure addresses that too.
If you don't have it already here is a link to the clinical manual for your machine. It is good to keep as a reference. Some good info in it on how the machine works.
Hi MountainGoat,
Why does my Resmed 9 have an altitude setting if it doesn't work?
Regarding real world health benefits I would have to say that in my case there are none, not even reduction of fatigue or tiredness, but I am still alive which might be considered a health benefit.
It isn't always that way, some people get significant benefits, but they are out surfing or hiking or maybe they went downtown partying but they certainly aren't here trying to understand why their magic wand is broken.
You have a unique combination of puzzles to solve and the right attitude to succeed so please let us know how you progress.
This forum could use someone with your skills because it's often good to have new perspectives. :)
I am not aware of an altitude setting on the S9 or the A10. What they do claim is that the machine automatically adjusts for altitude change. I think that is kind of like saying the wheels on our cars are round. CPAPs measure pressure in cm of water relative to the atmosphere - commonly called gauge pressure. So if your machine is set at 12 cm of pressure at sea level, that is relative to sea level atmospheric pressure. At 7000 feet it is the same. The machine will deliver 12 cm of pressure relative to the atmospheric pressure at 7000 feet. The machine maintains the same differential pressure which is what counts. The absolute pressure will change, but the gauge remains the same. To my knowledge all machines do it up to a point. When the air gets too thin (elevation too high) you can get to a point where the fan in the machine cannot pump enough air to maintain the pressure. So what you will find is that each machine will have a specification as to the maximum elevation it is good up to. For the S9 it is:
The key point is that while the gauge pressure remains the same at altitude, the oxygen content goes down as the air gets thinner. For those susceptible to central apnea that lower oxygen content can make the breathing regulation system more unstable, and cause additional central apnea events. To my knowledge the machine does not compensate for that factor.
Here is a link to the S9 technical manual, but on a quick read all I see in it is the maximum elevation number.
Did a little more research on this subject, and yes older machines did have an adjustment for altitude. I have not found a good reference for it yet, but here is what I have concluded so far.
The machines use gauge pressure so kind of by default they adjust automatically for altitude. However the problem is that these machines measure pressure in the machine, not at the mask. There is always a pressure drop due to flow resistance from the machine to the mask. And of course to prevent obstructive apnea it is the mask pressure that counts. For that reason the machine smarts estimate this pressure drop and use it to in turn estimate the actual mask pressure. Machines may have a setting for different hose sizes that is used to make this estimation more accurate. Larger diameter and shorter hoses have less pressure drop. The impact of altitude due to the thinner air is an increase in the pressure drop which impacts the accuracy of the estimated mask pressure. In the older machines you could correct to some degree for this by manually inputting an altitude or range of altitudes. Now it appears the modern machines may be measuring absolute pressure in addition to the gauge pressure. The absolute pressure then is used to make a better correction of pressure drop in the hose. I have not found a source that definitively says this, probably because manufacturers guard their technology for competition purposes.
In any case if the new machines are doing this I have to give them more credit than I have been. They may actually be automatically correcting for altitude pressure drop using a absolute pressure measurement (barometer). Will have to do some digging. About all I have seen from ResMed is that their new machines correct automatically but some of their portable machines may not. Perhaps it is an issue to fit the absolute pressure transducer in the small machines. That is a bit odd, because for those who want to use a CPAP on an airplane, the cabin pressure is maintained to the equivalent of about 7,000 feet.
It was while I was staying in the mountains that I bought my second machine so if I didn't make it back up there of a night I would have other options.
In this case, where some experimentation is likely to be needed with alternate settings for each location, having two machines might simplify things.
Of course having no machine might still be the best option.
I played around with the settings some more last night (at altitude at the moment). I dropped the max pressure to 12 and increased the min pressure to 8, without EPR and with Ramp turned off. I turned off the EPR as that is what the pulmonologist recommended. I also found that the machine ramped too slowly and it felt that I wasn't getting enough air when trying to fall asleep. This may have a lot to do with the oxygen content of the air on the mountain. With those settings, it was uncomfortable to sleep and, because of the back pressure on expiration, woke up with a dry mouth a few times, as I was trying to breathe out through my mouth.
In those few hours, I had 22 clear airway and 4 hypopnea events, resulting in an AHI of 12.13. When I woke up again, I gave up and then set the min to 6 and the max to 10, with an EPR of 3 and left Ramp turned off. This ended up being pretty close to the magic settings. The heated hose and humidifier was set to auto. The resulting AHI for the rest of the night (~3 hours) was 2.89, with most of the events occurring within the first 15 minutes of changing the settings. For the rest of the time I had only two CA events and no obstructive or hypopnea events.
I'm going to leave these settings as is for a few days and see what happens.
The altitude issue is going to be challenging. At the altitude I'm at, the relative oxygen content is about 16% compared to sea level at 21%, so quite a big difference.
I was also considering buying a second machine to leave at home and if a good deal comes up, I will probably do that. I'll keep the settings the same initially and see what happens. This could tell us if the machines do compensate for altitude, which is what the lab tech told me.
I agree with Biguglygremlin that no machine might still be the best option and hope that when I reach my target BMI of 25, I will be able to go without.
As far as real world benefits is concerned, I use a FB Versa and found that my resting heart rate reduced by 5 bpm since starting to use the machine. This is great news as my heart rate normally goes up by up to 10 bpm when I'm at altitude.
The Fitbit app now rates my 'cardio fitness level' as 'average to good', where it used to be 'fair to average'. Don't tell anyone but this machine is a fitness machine too, hehe!
I'm guessing a bit without being able to see the SleepyHead graphs but I think what you found out is that a minimum of 8 cm and maximum of 12 cm is too much pressure for you and caused your excessive central apnea events. This is kind of validated by the better results you got at 6 min and 10 max. And of those pressures the Max pressure is the critical one. It would seem you avoid centrals if pressure is under 10, but you get them when it is between 10 and 12.
I agree with the pulmonologist in that the EPR is better left off during the treatment period of the sleep. The reason is that your pressure is cycling up and down with each breath. If your obstructive apnea is occurring during the exhale the effective pressure preventing obstruction is for example only 7 cm when your inhale pressure is 10 cm. The problem with that is that you are getting an effective pressure of 7 cm to prevent obstructive events, while enduring a 10 cm pressure which may be causing central events. My conclusion has been that EPR of 3 is fine during the ramp, but can hurt you during treatment the rest of the night. In the extreme for example a 10 cm inhale with 7 cm exhale may be no better than a fixed pressure of 7 cm for preventing OA events. And, obviously 7 cm is better for avoiding CA events.
The trick with the ramp is to use the Auto Ramp feature. I find it works very well, and limits the ramp portion to the period of time you are awake. You do not have to guess how long it will take to fall asleep. And the second part of the Auto Ramp is to set the Ramp Start pressure high enough. So say for example you want to use a 6 cm min and 10 cm max. You set the EPR to Ramp Only with a start pressure equal to your minimum of 6 cm. Then while you are awake pressure will cycle from 6 cm inhale down to 4 cm exhale. When you fall asleep the EPR will stop and your inhale and exhale will be equal. You will have no reduction on exhale to make the treatment less effective. And, if it works well your machine will not have to increase pressure as much. The net result can be a significant reduction in actual pressure.
This all said another issue can be hypopnea events which are potentially central in nature can drive up the pressure. The only fix that I have found for that is to lower max pressure to prevent it, or in the extreme just switch to a fixed pressure. Remember the bottom line is that you want to limit pressure to as low as possible to prevent CA events, without having it so low that OA events start to spike up.
Generally apnea events which occur when you are awake are false flags. You won't get those false flags when using the Auto Ramp feature as the machine is smart enough to suppress those false flags until you actually fall asleep.
As far as needing different pressures at altitude I found one study that concluded with obstructive apnea there was no need to change pressure. That makes sense. The central apnea is a bit different matter. Your pressure needs for preventing OA should stay the same. The maximum pressure you can tolerate without excessive CA may be lower at altitude. That means the tradeoff pressure point might be different. I'm sure you will figure that out with some experience and with using SleepyHead.
Here is the conclusion of that study:
"For obstructive sleep apnea patients living at altitude, changes in elevation between 10,100 ft (3075 m) and sea level do not significantly alter absolute CPAP pressure requirements."
I take a bit of exception with the use of the word "absolute" because the machine does not use absolute pressure. I think they could have said it more accurately by simply saying you don't need to adjust the machine pressure setting for different elevations.
Edit: As for pressure settings, I think you might be better off with a minimum of 7 cm unless it causes centrals. It will give you more air while getting to sleep. It will let you move the ramp start up to 7 cm. I currently use a Ramp Start pressure of 9 cm for that reason. But, I run a fixed 11 cm, so I can start higher.
Thanks a lot for the advice and doing more research. Using Ramp and EPR only for falling asleep makes sense and I'll note those done to try in a couple of days. Given the good results I had for the second part of last night, I want to see how those play out and having more than 6 hours sleep may have some benefits too, not having to change settings every few hours.
Please guide me on inserting pictures. I'll paste a few screenshots from Sleepyhead, if that helps form a clearer picture.
What would be telling at this point is the pressure the machine is going to with EPR and then without EPR. The pressure it goes to, and a result the frequency of CA events is likely to be lower when pressure is lower. SleepyHead is good for seeing that.
On a PC you just press F12 to print a screen shot which saves to a directory that will be displayed (briefly) in the bottom right of the screen. When you get that screen shot capture file just use Windows Explorer to left click on it and then drag it to the body of a message here that you are composing. Make sure you use the Write a Reply button at the bottom to start the message so you get maximum width. Some tips to get a good layout in SleepyHead:
Hope that helps some. When thinking about it further, I suspect if you can get your pressure low enough to prevent undue CA events and minimal OA when at altitude that setting will probably be fine at Sea Level too.
When I first saw the altitude option on my machine I pictured a row of them in a tent at Base Camp to pump up the climbers before their ascent and to give them a fix on their return, with a team of sherpas to pedal the generators!
These machines might have more fun applications up where the air is thin. :)
The Fitbit is a good idea.
I just bought a Wellbeing Tracker because I wanted to be able to reference oxygen and blood pressure.
We have 2,000 people working on site, so it will be quite a row of machines : )
I tried to paste a photo of what the mountains look like. It is truly stunning but I'll need advice from someone on how to post a photo. I searched the help and the forum but couldn't find info on inserting pictures.
I had a look at the Kogan Pulse+ Wellbeing Tracker. I'm looking for something that can track SpO2 continuously, but it looks like this only does it when exercising. It's cheap enough, so I may buy one to try. Hopefully one can convince it you're 'exercising' the whole night, if the battery will last that long.
Apparently the Versa and Ionic have SpO2 sensors, but it isn't activated in the software as yet. Hopefully soon.
Posting photos is the same as posting a SleepyHead screen shot. I would keep them small in file size though. This site seems to do funny things when someone tries to upload several graphic files.
SleepyHead supports some O2 devices and apparantly integrates the results with CPAP results. If you click on the Oximetery Wizard Tab in the SleepyHead Welcome screen it will tell you which ones are compatible.
I'd love to see/know more about your mountain and what you're doing up there.
I'm sure Sierra will be able to explain how to upload pictures.
The Kogan Wellbeing Tracker is what I bought and it is only $39 here atm.
I haven't linked it to anything yet but as a wrist device it seems to mostly supply info on demand. You select the function and wait. It takes a few seconds (20-30) and buzzes you with the results. This process doesn't seem to require exercise. Perhaps that's the tracking aspect which I presume is uploaded to a device. It seems easy to use for my purposes and it's compact and discreet but I have no idea of what it's capable of beyond that.
The battery seems to last for days and the device is USB so it can charge off just about anything.
I am not recommending this wellbeing tracker although I have no complaints.
It is essentially a toy but it could help to make the user more aware of their general health and fitness.
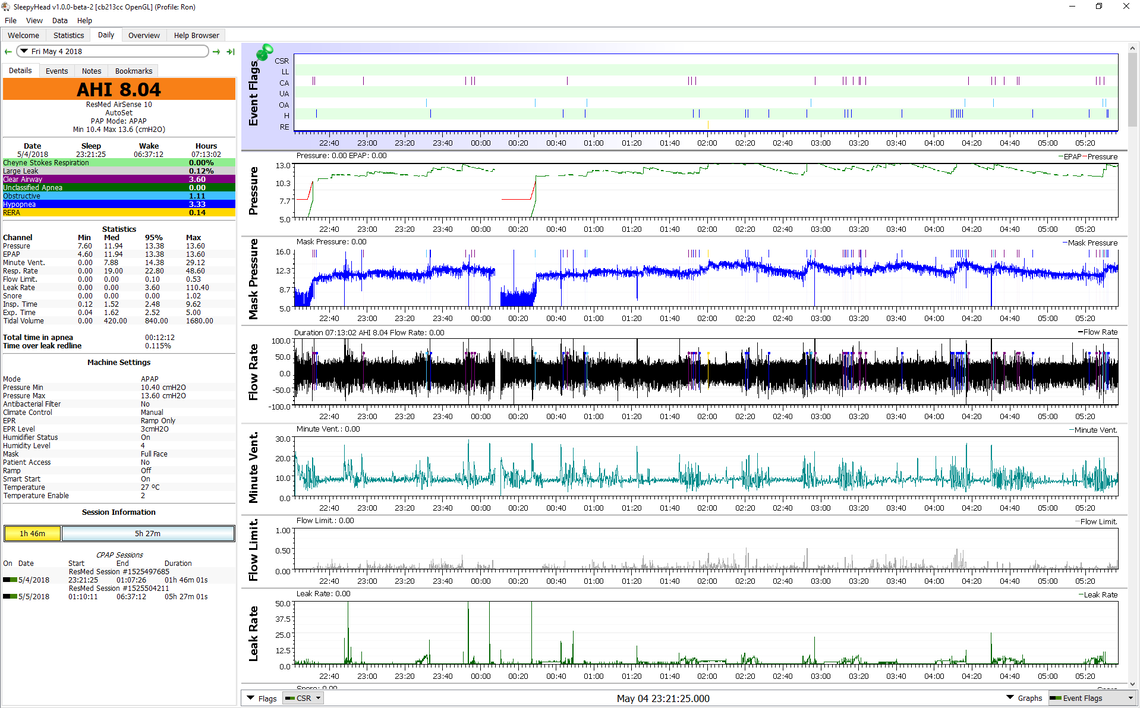
Here are some sample SleepyHead charts from my experience with CPAP. The first one was in Auto mode with pressures set at 10.4 min, and 13.6 max. EPR was in Ramp Only at 3 cm. Ramp mode was Auto with a start pressure of about 7.7. SleepyHead does not report the ramp status accurately. This was after I switched to ramp only EPR. I unfortunately had a major whoops and switched the SD card from my machine with that of my wife's, and I lost my early data. But, the pressures were running higher and results were worse with the EPR full time.
This is my sleep from last night which now is about right on with my average results. Fixed 11 cm pressure, EPR 3 Ramp Only, Auto Ramp, and a start pressure of 9 cm. More recently I have started to look at Minute Ventilation which is essentially the flow rate smoothed out a bit. It is kind of like a plot of your speed when driving in cruise control in a car. When cruise works well the speed is more constant. When it is not the speed varies up and down a lot. It becomes a bit more obvious when you zoom in. At least in my case this seems to be the root cause of my central apnea. My autonomic respiratory control system does not work well, and it works less well when the pressure is higher. It is like a control system hunting and not achieving stability. You can see now with a lower fixed pressure Minute Ventilation while still not perfectly flat, is much better.
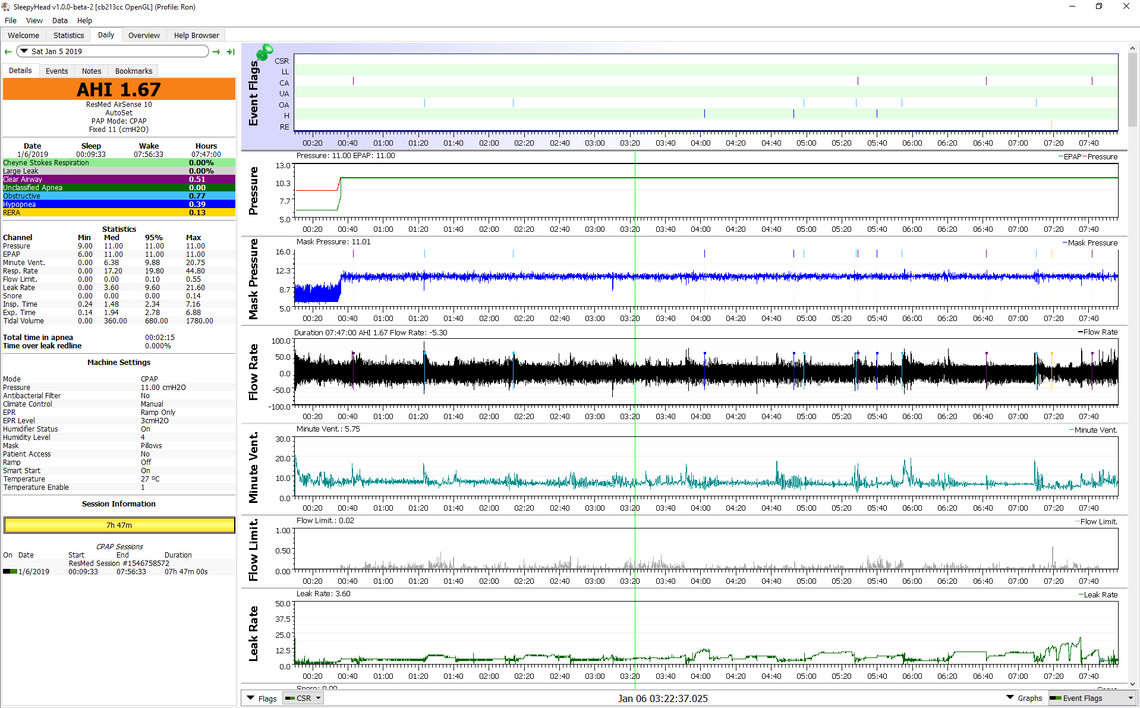
Not saying the same will work for you, but it might. One major learning for me was that the Auto mode seems to get fooled by hypopnea. I thought when I achieved pretty good results with a fixed pressure of about 12 cm, I could improve on that by going back to Auto, setting the minimum at 12 cm, and then the maximum at 13 to give it some room to correct abnormal obstructive apena, possibly when sleeping on back. In other words have the best of both worlds of fixed pressure and some automatic control. It did not work and in fact made my AHI worse. That was the point where I decided that in Auto my machine was chasing hypopnea events that were central in origin. Of course that just increases pressure and does not make things better, it makes things worse.
One other thought. If you end up with fixed pressure working for you and you want to go with two machines, you might want to buy a fixed pressure machine like the AirSense 10 Elite. While it does fixed pressure only, it still has detailed data capability. SleepyHead can handle data from two different machines. In Canada it would not be worth it as there is only about $30 difference between the Elite and the AutoSet, but I understand there may be a much larger difference in Australia in price. Avoid the AirSense CPAP model as it does not capture any detailed data - kind of a dumb brick. Or, if it is much cheaper, you may want to forego collecting data when using the brick, and just depend on the other machine to get an idea what is going on.
Hope that helps some,
Thanks for the detailed information Sierra.
Last night turned out to be a pretty good one, with an AHI of 2.93. It looks like the machine chasing events and then creating others apply to me too.
For the night, I had 1 hypopnea event, 4 OA and 20 CA. 11 of those CA events occurred within 10 minutes of the machine ramping up the pressure to 10 in response to two OA events, 11 and 10 seconds each. The longest of the CA events were 13 seconds, so nothing to write home about. Interestingly enough, if the limit for an event to qualify as an event was set at 15 seconds, I would have had one event the whole night.
Looking at the graphs below, it appears that the CA events dissipated when the pressure dropped below 9.5, so I'll set max pressure to 9.4 for tonight and see what happens. I can live with a few more short OA events in exchange for a lot fewer CA events.
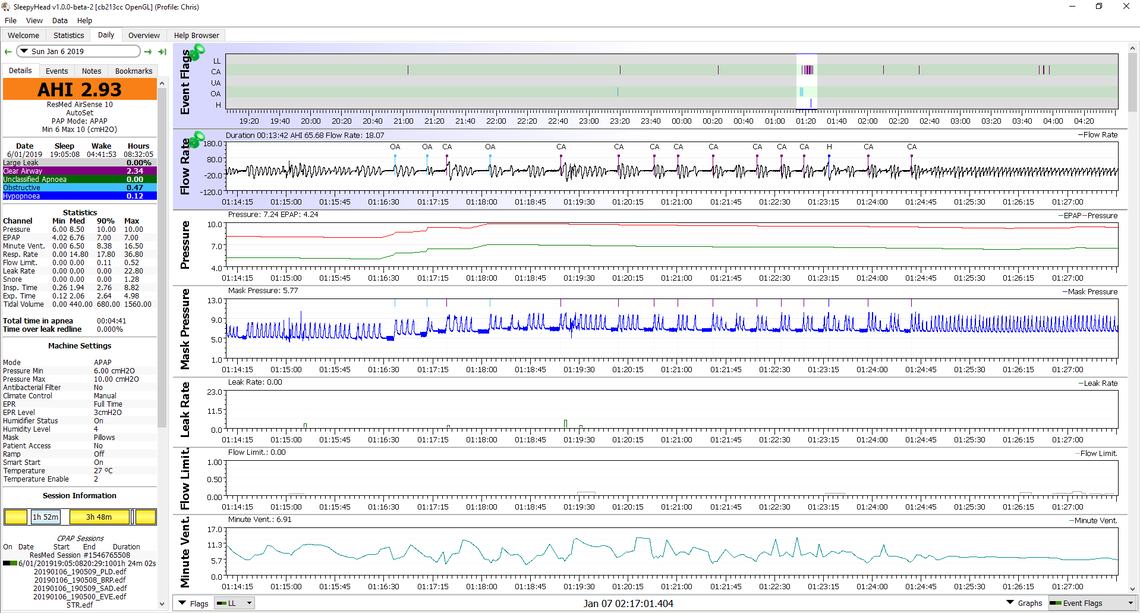
I think you are correct in concluding that the OA events led to the CA events. And in fact the initiating disturbance may have even started well in advance of the window you show. Notice how the Minute Ventilation was already cycling compared to the right side of the chart where it has stabilized. There may have been a less than 10 second hypopnea or OA event earlier that upset the stability. You will note on the mask pressure chart a higher frequency (4 Hz I think) oscillation toward the end of an event. That is the machine inducing a flow variation to test whether the airway is open or obstructed. If obstructed the flow variation results in the pressure making a larger amplitude. If the airway is open the amplitude is reduced. The difference is not huge, but if you look close you will see it. Knowing this is helpful because the flow test starts after about 4 seconds, and if the event lasts less than 10 seconds it does not get flagged or counted. This knowledge lets you manually identify the type of events it really is even if the event is not flagged. If you scroll left you might find a short event or something else starting that cycle.
My analysis of the way to control this is a bit different though. Your effective treatment pressure for obstructive apnea may be as low as the green (EPAP) pressure. That means your first OA event in this window probably happened at as low as 5 cm pressure. This is because you are using EPR. The machine responded to bring the green EPAP up to 7 cm and the OA events stopped. This suggests 7 cm is enough to stop OA events. The peak IPAP (red) pressure hit 10 cm and the CA events started. If you set the EPR for ramp only you will not have this split in pressure. I'm thinking the machine may then bring EPAP up to 7-8 cm instead of 10 cm and at that pressure you will not get CA events. Keep in mind that is a theory and the proof is in the practice.
My thoughts remain the same. Increase minimum pressure to 7 cm, use Auto Ramp, Start pressure of 7 cm, EPR still at 3, but Ramp Only. After that, I suspect you can reduce the maximum pressure to as low as 8. But for now the 10 cm max is not hurting you as long as the machine does not try to go there in Auto. I suspect it will not based on what I see.
Keep in mind that if you just reduce maximum pressure to 9.5 and leave EPR on, that will make maximum EPAP 6.5, and that may not be enough to prevent OA events.