Occassionally I'll wake up where my heart seems pounding a little and feel like I'm out of breath a little. My sleep apnea is well controlled now, with AHI <1 most nights. But even then, I'll occassionally have an event where I quit breathing for 20-25sec and my Contec SpO2 device records down to 85% and the alarm wakes me up. I don't wear it every night, but I kept waking up last night not feeling well, so turned it on.
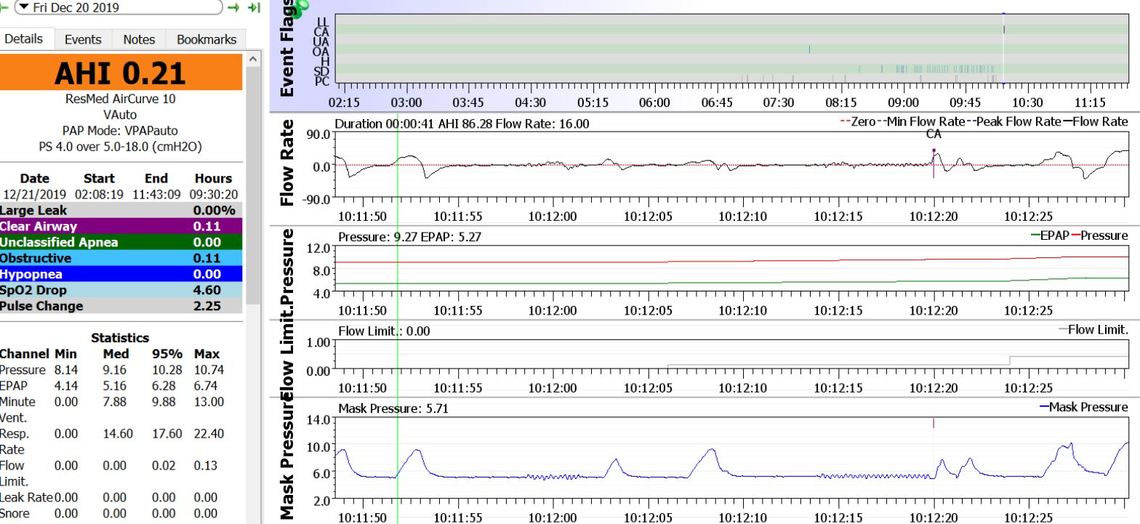
See the chart. It shows roughly a 25sec of no breathing, but the machine only marked a 10sec CA. My SpO2 dropped to 85%. May have gone lower if I didnt have the alarm set at 85%.
Are these sporadic episodes of any concern? My normal SpO2 during the day is around 94-95% max. This is due to past DVT/PE blood clots, and now I'm on blood thinners for that. I have started exercising regularly and lose weight but it doesnt seem to help with these events. My left side of chest feels weak or worn out after these events. I lay on my side.
I am not a medical professional and can't comment on the significance of O2 dropping that low for that length of time. It obviously is not ideal, but you would have to ask your doctor if it is a significant concern or not.
With respect to the machine only flagging a 10 second CA, I believe that is because you took a couple of partial breaths that were enough for it to start the count over again. I believe the machine starts the clock when the flow rate goes to zero, and at 4 second it starts a rapid pulse in the flow. It measures the impact that has on pressure. If it cause a larger pressure fluctuation, then it decides there is an obstruction. If the pressure does not have a significant pressure fluctuation then it concludes the airway is open. And when it lasts 10 seconds it flags it as an event. In the first section you can see the slight pressure fluctuation after 4 second, but the total event does not last 10 seconds, so it is not flagged. The smaller middle one did not last 4 seconds, so there is no flow pulse test. The last one starts the pulse after 4 seconds and lasts the full minimum of 10 seconds to flag the event as a CA.
I presume you have a BiLevel machine for a specific reason. Would it be to address central apnea issues? There are two ways that are often taken to address CA. One is to provide a pressure support (which I see is set at 4 cm) to help assist breathing. This appears to be the approach taken in your case. The other method used is to do everything possible to minimize pressure. In many cases the higher the pressure used the more likely central apnea events can occur.
What I see is that your EPAP pressure is very low, and it seems not much is needed to prevent obstructive apnea. However the 4 cm of pressure support forces IPAP to go much higher to 10 cm or so. You could ask your sleep doctor if setting the pressure support to zero would be a possibility. That would most likely keep the pressure up to 4 cm lower, and may reduce the frequency of central apnea events.
Hope that helps some,
Thanks. The reason I have bilevel is regular APAP didn't work to resolve my obstructions. I need the greater pressure support of 4 or more. I tried in the past to decrease it down to 3 or 2, but it made things worse with obstructions. I have mild apnea. I believe my sleep tests showed AHI 7 without CPAP. But it was really affecting me and my heart. My heart went into AFIB one time when I was on regular APAP. Which is another reason I switched to bilevel.
I usually don't have many CA's. Usually if I do they are only about 5 a night with no obstruction. But the ones that affect me are these longer 20second+ ones where my SpO2 drops rapidly.
I never heard of SpO2 dropping so rapidly when stopped breathing for only 20sec. People can hold their breaths for minutes when under water. Do their oxygen drop to 85% or below so rapidly?