The past few months have been scary for me. My apologies for the length. I badly need some advice as I continue to work with medical professionals to try to figure out what is going on. Even they are at an "I don't know" point in all of this.
History: March 2018, I had an in-lab sleep study after lots of blood work at my GP doctor. I was chasing down the "tired" feeling I have had since my early teenage years that nobody could figure out. I'm in my mid-30's at this point. MRI of the brain shows nothing wrong. I ask for a referral for a sleep study after learning about the process (I wasn't aware of how it worked before and never really thought about sleep issues when I was younger).
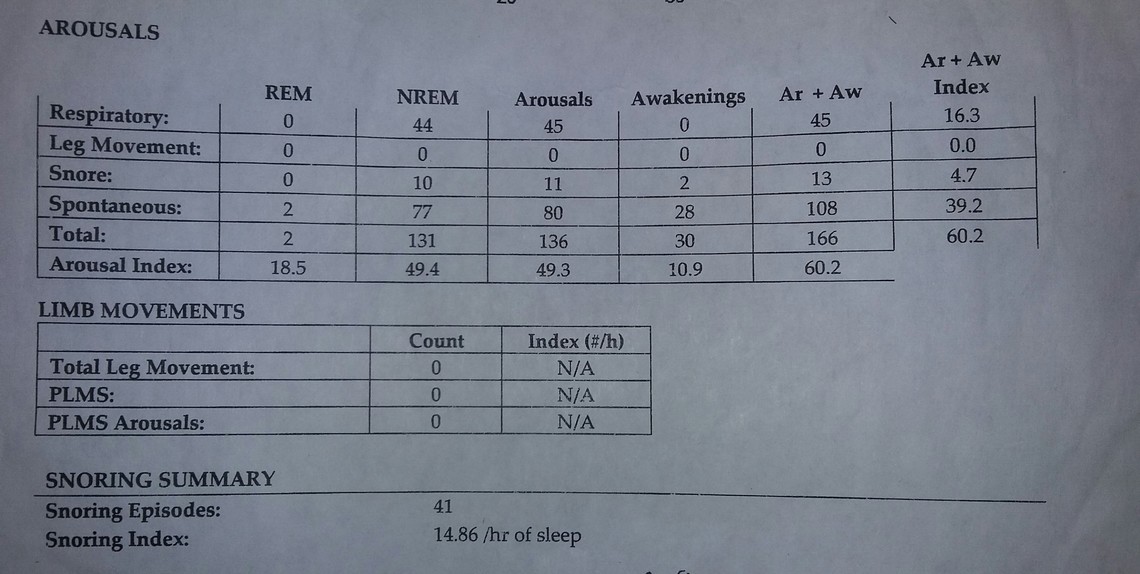
Polysomnogram Interpretation: "The polysomnogram shows severe sleep fragmentation. Sleep efficiency was reduced. There were 13 obstructive apneas and hypopneas present for an overall apnea-hypopnea index of 4.7. There were 50 respiratory events including RERAs for an RDI of 18.1. Supine AHI: 6.1. REM AHI: 9.2 (REM time - 6.5 minutes). The total time with oxygen saturation under 90% was 0.0 minutes with a nadir of 92%. The desaturation index was 4.4 events/hour. Cardiac was normal sinus rhythm. Snoring was present. 0/hr periodic limb movement index and PLM arousal index - 0/hr sleep. Impression: snoring. No sleep disordered breathing. Insomnia vs first night effect."
Doc said I didn't have sleep apnea. I have a very scalloped/crenated tongue, which I've had since I was a kid. He said that's a "classic sign" of sleep apnea. No CPAP.
I go to my ENT doc and show her the results. CT scan of the sinuses requested. Deviated septum surgery and turbinate reduction surgery. I breathed much easier now. It used to take 2.5+ seconds to exhale a full breath. Now it takes about 1 or so. I still feel horrible, though. I request a home sleep study. It shows a variety of apneas/hypopneas averaging 20-30 seconds and one apnea up to 80+ seconds. Lowest heart rate was 42bpm. No dangerous oxygen drops noted. Puzzled.
Over the past few months, I started having what docs think are anxiety attacks. I've never had them like that. Haven't been sleeping well. I sleep 8-9 hours and wake up with a flush-hot feeling in my face, sometimes a little pinkish on each side of my cheeks and face. The more I exert myself doing stuff at work/home, the more hot and flush my face feels with pressure.
I've been to the ER three times over the past couple of months with a random racing heart (140+bpm out of nowhere, right before bed), shaking all over with adrenaline as if freezing to death and feeling like I can't breathe and I'm dying. Classic panic attack symptoms. Blood pressure was going up as high as 1703/90. I've never had anxiety like that, ever. Not in 37 years. Now I get "adrenaline pulses" when I yawn that shake my whole body as if freezing cold.
GP doctor did thyroid blood work (TSH), CBC, everything. ER worked me for everything from a heart attack enzyme/blood clot, a few EKG's, x-rays of the chest cavity, everything. All came back normal. I've had so many blood tests that I'm sick of them.
Even on days when I sleep more/better, I'm still exhausted. I have trouble getting my body to turn off early, before 11 or 12. Sometimes later. It wants to stay up and awake, even when dead tired. I have set up a nigh vision home security camera trained on my bed. It's attached to the security system DVR. About every 10-15 minutes all night long, I either wake up and look around or I toss and turn from one side to another. Sometimes just a slight movement shows that I've awaken. During the in-lab study, I remember hearing the sleep tech a couple of rooms over say regarding someone, "He keeps waking up!" I think it was for me. I've had a couple of panic attacks an hour or two after going to sleep and I would wake up with my heart just racing immediately for no reason. I would feel like I was losing my breath and struggle to keep from going to pieces. The more you panic, the worse it gets. About 6-8 months ago, I asked my ENT doc to help me get an Air Sense 10 APAP based on my home sleep study results of 5.2 AHI. She agreed because she knew my sleep doctor refused to give me one. I figured out the settings to get my obstructives down to 0.5 AHI every night. But about a week ago, I woke up after an hour while USING the APAP and had a bad panic attack. My AHI had spiked to 3+ out of nowhere for that night. I have since stopped using it until I get more sleep study work done.
When I work out, my heart beats upwards of 140+ bpm. It feels like it is going to pound out of my chest just sitting down and pedaling moderately on the elliptical cardio machine at home. The pule rate is higher during the day when I'm resting, usually up around 110 or so. Picking up a 10 pound box at work and moving it over to sit it down makes my heart race. I've been to a Cardiologist when my blood pressure was up and I was feeling odd. Stress Echocardiogram showed a perfectly healthy heart with no issues. Yet exercising would make you think I have heart trouble. I'm not alert enough to drive or use machinery at work. I've made mistakes driving before (e.g. not paying attention and turning left in front of opposite traffic about to start moving, while I had the red light...or over-compensating turning off from our street and nearly hitting a mailbox).
Big concerns: I 'vibrate' when I sleep. There are times when I'm so tired that I fall over into my bed and within a few minutes, my skin feels like it is crawling in place about a quarter of an inch all over my body and my whole body feels like my organs and skin are vibrating as if they're shaking back and forth with my heartbeat or something. Other times, I might fall asleep in my computer chair and I wake up with my body still 'asleep' basically. So my brain is alert and I can turn my head and everything, but I wake up knowing that my body is still asleep. After 30 seconds-minute, my heart will start beating what feels like very fast as my body 'wakes up' to catch up to the brain. It is quite scary. I have started automatically grabbing my chest whenever I get those odd feelings. It is sort of a jerk reaction probably related to the anxiety that whatever this is is causing. GP doc wouldn't listen and wanted to give Metoprolol for lowering the heart rate/blood pressure. When I'm really tired, I'll feel like I'm going to faint over with that. I stopped taking it. Other days my whole body just shakes and feels trembly.
I sign up for my employer's health insurance in March. It kicks in April 1. I'm planning to get a Type 2 home sleep study from this place online: http://axgsleepdiagnostics.com/product/comprehensive-type-2-diagnostic-home-sleep-study-unattended/
In-lab studies...I don't sleep enough to be beneficial and I'm scared that I won't get good results in my next in-lab study, either. I'll follow up with an in-lab study after the home study. That one is almost similar to an in-lab, minus the sleep tech watching everything, of course.
My household got a stomach bug/virus around the first of February. Now my digestive/GI system seems all messed up and I'll be getting probed for an upper endoscopy on March 5. Doc thinks I might have a stomach ulcer. Bladder wall has stiffened since being sick, for no reason. Feels odd when I bend over. Docs don't know what causes this. Urine sample was negative. Even a culture growth sample was negative over 2-3 days. They have no idea why my bladder wall has thickened, per the CT scan data over the past couple of weeks.
Could all of this be related to UARS? They put me on metoprolol at my GP doc, but sometimes when I'm really tired and I take that, I feel like I'm swaying a little and could faint anywhere.
Where do I go from here? Everything has been checked. All blood work is normal. Heart doc warned that the meds were suppressing the symptoms, not treating them. He 'thought' it is anxiety since my heart is healthy, but we don't know what is causing that anxiety. I've had a full abdomen MRI (nothing but a few benign cysts found in the liver, which most people have) and CT scan. The hospital even checked the heart/lungs, pancreas, everything.
I feel pressure in my face even when I lay down at night to sleep. When I take my blood pressure, sometimes it is quite normal even though my face looks pink, confusing me even more. I do get 'anxiety' out of nowhere just over the past few months - worried about all kinds of stuff now because of all that is going on. I manage that with breathing and it goes away. I just don't understanding.
Hi singingkeys.
I like that name btw
I'm glad that you posted the above query in this forum because, although you are unlikely to get the answers you might hope for, at least the comments you get will be well intended.
I confess to having only skimmed through your notes above. For that I apologise.
The thought that first comes to mind is that life is complicated and messy for all of us and I'd gladly trade places with you, in a heartbeat.
My second thought is perhaps a tad more constructive.
You sound like you could use a protracted series of counselling sessions to give you the tools to manage uncertainties and worries more effectively.
I hope you find the answers you need.
Life, despite being complicated and messy, is too precious to waste in perpetual worry.
As I have said before, I don't think your issues are related to UARS or apnea, but keep in mind I am not a medical professional. I have a couple of thoughts on the issues you are having. One is doing an extended test to what your heart is doing over a longer period. There is one specific test where you are given an instrument to wear for a couple of days, and then the data from it is read to determine if there are any abnormal heart conditions. Some information:
My second thought was on the beta blocker medication you tried. Beta blockers are not all the same. They are mainly used to treat irregular heart rate issues. The Holter test will be helpful in deciding if that is an issue. They are also used to treat anxiety but that is an off label use. You may want to ask your doctor what type of beta blocker may be best suited for you. Some may disturb sleep less than others as well. The other issue with beta blockers is that they can cause a "rebound" effect. If you keep starting them and stopping them, you could make things worse instead of better. It is also best to use a beta blocker that has a long lasting consistent effect.
That is about all I know on the issues you raise.