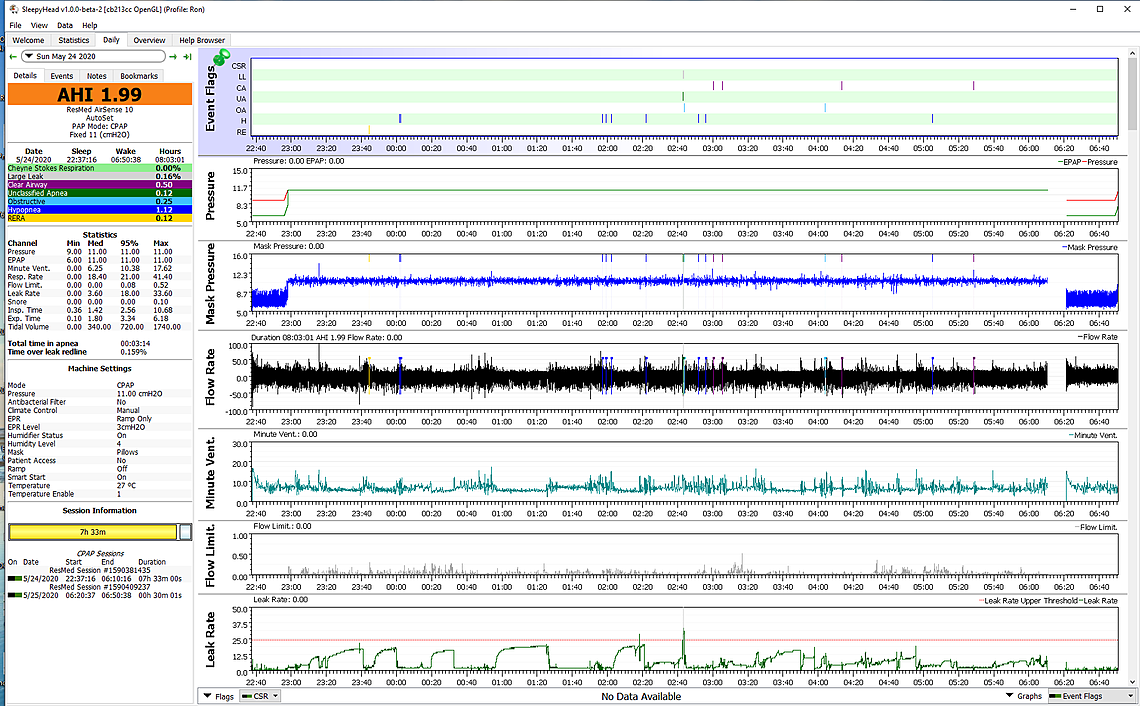
I have not used the OSCAR version of the software, but have used the original SleepyHead version for about 3 years or so. I find it very useful software if you really want to know what your CPAP machine is doing during the night, and how you are doing during the night. Here is what the Daily Report looked like for my sleep last night. It kind of depends on what your level of interest is in how the machine is set up and how well it works.
I used it, until I saw this...from CPAPtalk.com
A CA scored by either the ResMed or Philips Respironics CA algorithm is very likely to be a "real" CA in the sense that the airway is clear (open). As such, a real OA is not very likely to be mis-scored as a CA on either a ResMed or Philips Respironics machine. Scoring a real central apnea (as scored on an PSG) .sleep study Polymonogarph ) does not depend on the patency of the upper airway; hence there is a higher probability that a real CA may be mis-scored as an OA by the Philips Respironics and ResMed CA detection algorithms Both the Philips Respironics and ResMed CA-detection algorithms are more likely to have problems detecting CAs at higher pressures. In other words, as the pressure increases, the chances that a CA is mis-scored as an OA increase
Whadda think now?
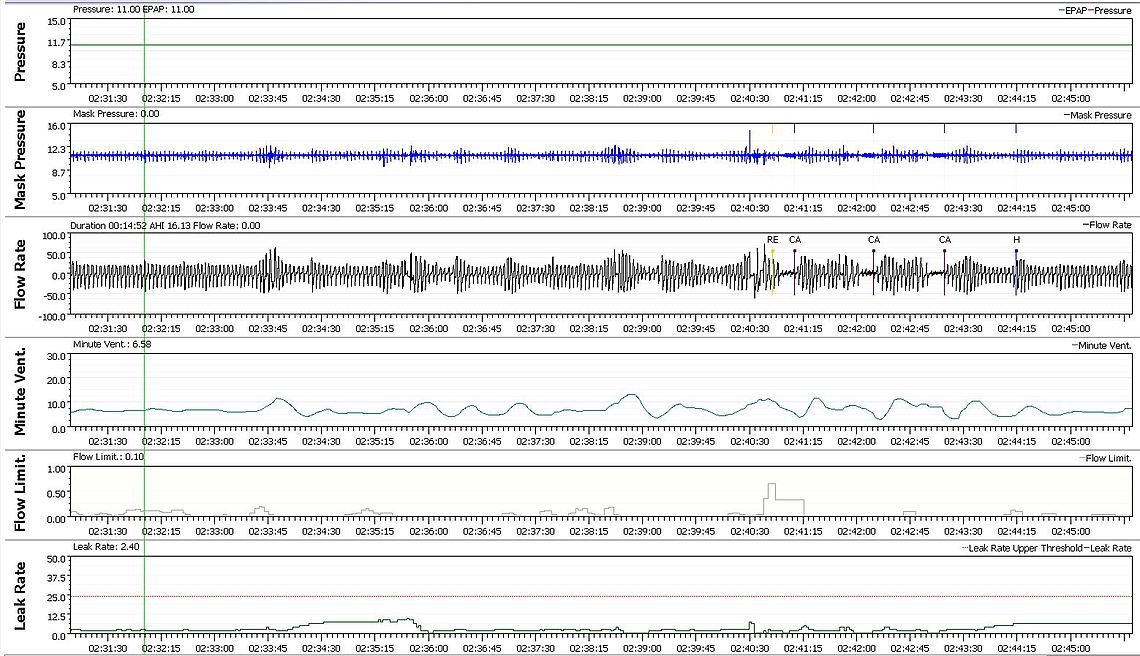
My first thought is that this is not a OSCAR or SleepyHead issue. All the software does is display the data that the CPAP/BiPAP machine has captured. It is the machine that determines the types of events. Yes, the machine can make mistakes, and the event classifications should not be considered as absolutely correct. However, they are a good indication of what is going on. If you want to zoom in on events to expand the scale and look at them in detail you can form your own opinion as to how accurate the classification is. I suffer from CA events, and then hypopnea events next. OA events are almost always low. Hypopnea is generally assumed to be a flow reduction due to restriction of air flow, or obstructive in nature. However, they can actually be due to reduced effort to breathe which is a central effect. My suspicion is that most of my hypopnea events are central in nature rather than obstructive. Here is an example from last night to look at zoomed in. You will see there is a series of events; RE, CA, CA, CA, H. If you look at the minute ventilation you can see that the flow was cycling prior to these events, and really started about 2:33.45. Something disturbed flow. Perhaps the mask moved or something. This was really the starting point of the event series and it is due to my issues with breathing control that cause central apnea. For whatever reason my breathing control system is not stable. If something upsets it, it starts to cycle as can be seen most easily with the minute ventilation. At the RE I may have even woken up. But you can see the cycle continues. The final event is classed as a hypopnea, but I would say almost for certain it is just a CA event that did not go to full loss of air flow. This is an example of why I more or less lump in my hypopnea events with the CA events as part of the same problem. Where the rubber hits the road is when you are trying to decide what to do about it. If the hypopnea events are obstructive in nature one would benefit from more pressure. If they are central, then more pressure may make it worse. For this night my total AHI was 3.31, with 1.66 CA, 0.25 OA, and 1.40 H. My conclusion is that if anything the pressure may be too high, not too low. This is an example of how I use SleepyHead.
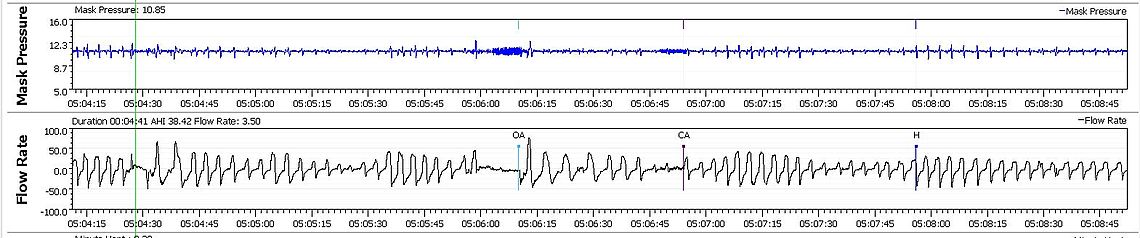
If you are wondering about whether an event is a CA or OA, you can second guess that too by looking at it up close. The ResMed tries to cycle flow to see what it does to pressure. If the airway is closed the pressure will fluctuate with a higher amplitude. If the airway is open the pressure fluctuation is lower. Here is an example of two events side by side. Here is an example of the two events side by side. Notice how the mask pressure fluctuates up and down and paints a band of pressure fluctuation in response to the machine testing for obstruction. In the OA event the band or pressure fluctuation is wider than for the event that gets classed as a CA. The difference is not huge, but it is there. Does the machine sometimes make a mistake in classification? Probably at times. By my eye the machine it right in this example. And again like the previous example that H that follows the CA event is probably central in nature.
Is this potential minor inaccuracy a reason not to use OSCAR? I would think absolutely not. The alternative is to fly absolutely blind. One does have to look at the results with some thought and purpose though. And remember the data comes from the machine not from the display software. If you go to a sleep specialist and do not take your SD card with you so they can look at it, they will see almost nothing for data. If you take your card, they will see the same as what OSCAR shows you.
Hope that helps some,
Is this potential minor inaccuracy a reason not to use OSCAR? I would think absolutely not. The alternative is to fly absolutely blind.???? Dr's office monitors it.... and just like any other lab result anyone can gain access to.
One does have to look at the results with some thought and purpose though. If it's not accurate then what good is it?
All a CAPA APAP does is provide air....... bilevel senses pressure differential and adjusts accordingly. APAP/CPAP does not. CPAP/APAP senses restriction and ramps up and down depending on restriction sensed.
If you look at the minute ventilation you can see that the flow was cycling prior to these events, and really started about 2:33.45....................
I'll meet you have way, on this. Three forums later you are the only one that cam this close to explaining the events flagging within Minute vent. Would you care to go further?
Convince me that the CA's in my chart are legit and why?
CA's , in my apneas ,need a Polymonographic readout to show positive legit CA's and to determine a titration Bilevel study to provide proper ventilatory assistance..hence (BiPAP...... Inahalation PAP Exahaltion PAP.)
Thus, whereas CPAP only opens the upper airway, BiPAP can supply actual ventilatory assistance. In all these modes of pressure application, the continuously positive airway pressure can act as a pneumatic splint against upper airway collapse, can reduce the work of breathing, and can thereby improve oxygenation.
There are two main differences in a BiPAP compared to a APAP. First the BiPAP can go up to 25 cm for maximum pressure while the APAP is limited to 20 cm. But the higher pressure is not an obvious advantage in treating CA. More pressure often makes CA worse. The second difference is the ability to produce a higher differential between inhale and exhale pressure. A ResMed APAP can give you a 3 cm difference with EPR. The BiPAP machines can provide much more, and adjust it automatically during the night. Again this is not necessarily an advantage in treating CA. The higher the differential you use, the higher that IPAP has to go compared to the EPAP. The lower the EPAP the more obstructive apnea you get. The higher the IPAP the more CA you get. One can end up with the worst of both worlds (more OA and more CA) using a BiPAP to treat CA. I think a BiPAP is more for someone that has air flow issues (smoking, COPD, asthma, lung issues) than it is for treating airway collapse and CA. I recall one study that found in 60% of the cases CA got worse when the patient is moved from an APAP to BiPAP. It seems to me that if someone cannot achieve an AHI of less than 5 and the main issue is CA events, then it is time to consider an ASV like the ResMed AirCurve 10 ASV rather than a BiPAP.
You are not addressing the management of CA's in you post about Titration hypoxemic Bilevel testing.
BPAP manages IPAP and EPAP.
"I think a BiPAP is more for someone that has air flow issues (smoking, COPD, asthma, lung issues) than it is for treating airway collapse and CA."???
If you really knew what you are saying, you wouldn't say "I think".......... BiPAP IS ventialtion for treating CA'S
ASV therapy is Bilevel therapy....same thing. Adaptive Servo Ventilation.... is working both IPAP and EPAP.
Bi meaning two..... two what.. two functions. IPAP and EPAP........ real easy. RES MED lists their ASV machines and describes essentially what it does. IPAP EPAP
No. A BiPAP is not at all the same as an ASV. A BiPAP increases and reduces pressure in a slow response to what it is seeing. An ASV adjusts pressure on a breath by breath basis. The response to reduced effort to breath is virtually instantaneous. The ResMed machine does not go over 20 cm of pressure either.
I don't think SleepyHead or Oscar should replace a medical professional.
Unfortunately most sleep professionals never look at the detailed data on the SD card. If they do not ask you to bring your SD card with you for analysis of the data, you have to be suspicious what they are basing their advice on.
My original Fisher-Paktel you had to bring the stick in so they could down the data.
When I picked up my Resmed the tech told me it didn't come with an SD card, I was sure it was supposed to. He said it connects to the internet via the cell tower. I mentioned that I have poor service were I live, and ask what happens if it doesn't connect. He said to bring the whole machine in.
I put my own SD card in it and use it with SleepyHead.
Everything changed a few years ago, at one time I thought the people at the medical supply company were terrific, the company and the people were great. Outstanding customer service.
A few years ago there were hospital mergers, buy outs, changes in the service providers. Service went down the tubes, it was horrid, awful in every sense of the word. It would take over a month to get cushions or any supplies.
I found out that some original people that I liked were part of a new company, different from the horrid service I received. I have a better understand as to what happened, I am not sure of the truth. The main people are still the same but the company is different. They don't provide the service they once did. I still have no idea why one of the techs (not the manager) told me I don't get an SD card.
They don't ask for mine.... but only one time. Bottom line? it's how I feel....... regardless what's seen by OSCAR or their charts on thier software. The first Polysomnograph showed severe OA although I had 10 CA's on my study printout. My Polumary Dr requested a titration study and the Ins. Co. refused and only allowed a APAP for therapy. Why? Because it manages OA's yes... And teh interpreting Dr wrote it up as severe OA and technically OA"s can trigger CA's. The SA02 scale was below boderline, at times, saturation which showed CA's did exist in my first study. But experincec Dr's experience with Ins. Co.'s show that they have to abide by Ins.Co's wishes to use CPAP first to clear OA"s first and quite possibly clear CA's. The second sleep split study titration CPAP/Bilevel I have to get will determine If I am Hypoxemic, or not. As of right now my Dr see that SAo2 is below normal which justifies Titration bi Level study.
Hypoxemia can have many causes. Living at a higher elevation can not only contribute to it, but it can also trigger central apnea events. I live at 2,000 feet of elevation, which is not that high, but I notice a reduction in CA event frequency when I travel to sea level. I have also seen other posters who have severe central apnea when they travel to higher elevations like Denver.
Thinner air requires more pressure up there. Higher pressures drive up CA's correct, however that doesn't address nor manage failure and inefficient Ex hale and the need of EPAP. Once the excess CO2 is ventilated and IPAP initiates the next breath.... Hypoxemia is present form the lack of exaltation assistance and Inhalation assisatnce. Chemo receptors wake one up to breathe.
It is kind of complicated, but APAP machines for some time now automatically compensate for elevation. They maintain the same differential pressure between outside of the body and the airway pressure. So the same airway splint effect to keep the airway open is present at higher elevation. The O2 and CO2 balance in the blood however can be upset by it, and as a result trigger the instability in the automatic breathing control system that the body has. It can initiate the minute ventilation cycle that is illustrated in the SleepyHead graphs above. That in turn can cause central apnea events.
You may want to look at the posts by a user called "lakechapala". I recall he lives in Canada at a lower elevation but stays in the winter at Lake Chapala in Mexico. He had major issues with central apnea that he could adjust for at his lower elevation home in Canada, but not at Lake Chapala which is at about 4,500 feet elevation. He tried many things including, I recall, a medication prescribed for altitude sickness. In the end he bought a ResMed ASV machine and solved the problems. That said if you have respiratory issues like COPD, asthma, or other lung issues this may not be the best route for you. It depends what the root cause of the issues are.
Here is a link to the abstract of that report that found using a BiPAP was more likely to increase central apnea than to reduce it.
Bilevel Positive Airway Pressure Worsens Central Apneas During Sleep
I have to have a second study done with one..... and it may not help. I don't know if it would but who knows. I'm not the kind of person who would just go out and buy one to see if it would work.
I wouldn't recommend just buying an ASV either. They are not cheap and run in the range of $4500 or so. They also need a special heart function test run before you go on one. But, if your problem is central apnea, it may be what you need. My basic plan if I get to the point where I cannot average under 5 for AHI with CA being the largest factor is to ask my doctor to prescribe one, after getting the necessary heart function tests done to see if I am suitable to use one. A quote from one source:
"In May of 2015, ResMed, a global maker of CPAP and ASV devices, issued a statement cautioning against the use of ASV treatment in patients who had symptomatic chronic heart failure and reduced left ventricular ejection fraction (LVEF) of less than or equal to 45 percent (normal LVEF is between 55 and 70 percent). Respironics, another manufacturer of sleep technologies, followed up a couple of days later with a statement of their own discouraging use of ASV for at-risk patients while more studies are being conducted."
can't post chart, but no pressure spike during CA events.
Update...... I watched a vid on an actual Polysomnograph chart..... and I can see the similarities. So yes it is an accurate interpretation.
What you have to do is identify all the CA events in a night and see what the IPAP pressure is at each event. This assumes the pressure is varying during the night. It can give you an idea if the CA events are more likely to happen at a higher pressure. There will not likely be any pressure spikes. The pressure will vary as the machine tries to prevent OA events. That is essentially what they are doing in a sleep titration test. They vary the pressure intentionally to see when you get CA events. The general idea is to get the pressure high enough to stop the OA events, but not high enough to initiate the CA events.
To post a chart save the daily report screen shot (F12 on a PC). With file explorer left click on the saved file and drag it into a full width message here. It should upload.
Dude, I am not sure why these posts appeared today out of the blue. However, when I look at your Oscar charts they are too zoomed in to make any sense out of. It is more of a longer term pressure issue that may cause CA events. Minutes not seconds. Based on the other data on the left your pressures are not going that high. Would have to see a non zoomed in daily report to make more sense of what may be happening.