Resmed CPAP machines tend to report a significantly lower AHI than Philips Respironics machines do, on the same patient (I know because I have both machines). Proponents of Resmed machines (like CPAP resellers and DMEs) explain this difference by alleging that Resmed machines provide better Apnea therapy than Philips Respironics machines do. However according to my own experiments and corroborated by many others, it appears that Resmed machines only report lower AHI numbers because these machines software does NOT check some critical sleep data like "Patient Initiated Breaths" or "a backup rate of Breaths Per Minute setting", or "periodic breathing" or "Clear Airway".
Have you ever come across the same question before? Tell us what your experience has been like.
Having used only RESMED machines, I wasn’t aware of that difference in reporting of AHIs between the two brands. But I think it’s extremely interesting and bears further exploration.
It would be very interesting to know the specifics of the different “counting” of apneas as between the two brands of machines. Presumably, they both have chips working on algos, but have chosen different algos.
Also, is this entirely about the residual apneas or or does it extend beyond that?
My 30 day AHI averages 4.5 on Respironics where as on resmed my AHI averages only 0.6. Is Resmed providing a 12 fold better therapy? It is highly doubtful.
I have severe Central Apnea disorder (>52) with less than a 10% Obstructive Apnea and I am very interested in studying my condition. For this purpose I analyze my sleep data using various software. OSCAR cpap analyzer is my choice however.
Since my therapy is with Adaptive Servo Ventilation (ASV) type of machines, I have bought both, a Respironics Dreamstation ASV and a Resmed Aircurve 10 ASV machine. Since ASV therapy monitors my respiration on a breath by breath basis, when I monitor the data I have a very detailed set to look at, like flow rate, mask pressure, tidal volume,minute ventilation and so on, on a breath by breath basis. So when I compare graphs between resmed data and Respironics, I note that at high resolution (zoomed up to 20 seconds windows), Resmed simply ignores to flag events such as Hypopnea, clear airway,Obstructive Apnea etc, on average 80% less times than Respironics algorithm does. In fact Respironics algo never misses a single event when I examine data at high res.
This explains why Resmed machines generally report a much lower AHI than Respironics. Its too bad that I can't post images here because I can post several comparison examples of sleep data to support what I am saying here.
Cyrus, Have you done a recorded overnight oximetry for at least a week on both machines. If not I would talk to your doctor about doing that as an objective measure to check the efficacy of the machines. Subjectively , it’s how you feel after using the machine. The ODI from the oximetry will confirm the activity of events.
As far as the AHI on the download it’s a moot point. Clinically anything under 5 is acceptable especially if you are severe and on download it can be other factors such as head position or leak that can cause it to be artifact.
Doctors don't like getting into debates about brand efficacy, because of its implications with insurance companies and their unpaid involvement which can then become open-ended. They just write a prescription for a machine. They do NOT specify which brand of machines and leave that entirely to the DMEs and that's where the problem lies because the DMEs in turn use Philips recall, as an opportunity to flog their Resmed machines because they know there is a huge potential with duplicate business with Philips Respironics users who are now desperate to find an alternate machine to their Philips brand.
I do keep a meticulous SpO2 record and no, my SpO2 doesn't change between machines, however the purpose in the treatment of Central Apnea is not to control SpO2 because otherwise supplemental Oxygen would have just been fine instead of ASV therapy and yes, my sleep quality improves monumentally on my Respironics machine, which is why after 4 months of tinkering with my brand new Resmed Aircurve 10 ASV machine, I went back to my Respironics machine, despite the "recall".
The point that I am trying to highlight in my OP is the fact that Resmed machine algorithm shows false reporting of AHI which Resmed and their resellers then use to claim high efficacy therapy.
I would not buy a DreamStation APAP unless I was really forced to, by unavailability of a ResMed. I do not like their auto program that continually tries to force the pressure down, and then bumping it back up again when apnea events are triggered. I find that the only way you can make a DreamStation machine behave in Auto is to push the minimum pressure up to prevent the cycling up and down of the pressure.
I'm not sure how Philips Respironics APAPS work because I am on a ASV machine. ASV machines are more akin to Ventilators than they are to PAP machines because they provide a close to spontaneous breath when you miss one while they also they provide auto EPAP pressures to minimize patency in OSA events. CSA events are essentially Clear Airway events that last more than 10 seconds, in which case a ASV algo should deliver successive and elevating IPAP pressures for the preset length of time, based on your Inspiration time. (Resemd has no alternate manual settings for any of this while Dreamstation algo allows you a fiully auto setup or manual setup).
I have no issues with my dreamstation. It is set to the max range of IPAP and EPAP and Pressure support. So when I am awake I can barely even feel it (which is what it should be like) and when I fall asleep it just automatically adjusts the pressures for each breath and I never ever feel it or get bothered by it.
In contrast my Resmed does some crazy things, like just adjusting the pressure up and up for no apparent reason and when I asked Resemed support how to fix it, they suggested that I "keep blowing back hard into the tube", which I thought was pretty stupid.
Resmed algo just looks at the last 90 seconds of my breathing pattern and sets up its backup based on that 90 seconds. It does not even have a manual backup rate setting. What this means is that if someone is seriously sick and their breathing pattern is all over the place, Resmed algorithm doesn't care and takes that pattern as its baseline:-)...So good luck if you average like 6 breaths per minute because Resemd ain't gonna give you more than that, if you stop breathing:-)
This is what I found in the ResMed ASV clinical manual:
"Backup rate The AirCurve 10 ASV device uses breath phase mapping to provide a timed backup rate that is synchronized with the patient’s own breathing. When the patient deviates from the ventilatory target, the ASV device aims to stabilize the patient by adjusting Pressure Support. If necessary, it will adjust the timed backup rate from one that matches the patient’s own recent rate towards the built-in default 15 BPM backup rate."
Right, so if the patient's breathing is all over the place due to a respiratory issue or sickness, then Resmed's algo will be calculating faulty backup:-) This is why a Dreamstation algo has BOTH choices, an Auto Backup calculation OR a manual backup breath rate, manual Inspiratory time and even manual setting for the "RISE time", the transition time between IPAP and EPAP. Clearly they have worked a lot more on Dreamstation algo than they have on Resmed and that's only understandable, given that Respironics INVENTED CPAP therapy back in the 70s:, some 10 years before Resmed started as a company-)
This is the history of ResMed as I know it. Colin Sullivan started out by using parts from a vacuum cleaner and I recall a dog for the first subject. Tests in people were done by gluing the mask to the face of the subject. Sounds gruesome compared to what we have today. I also recall that ResMed and Respironics came close to amalgamating at one point, but it did not happen. Have not read the full article for a while now, so forget most of it. Seems like they spend most of their time suing each other over patent rights.
All I know is that Boston based Respironics invented its first medical CPAP machine in the mid 70s and later was taken over by Philips in the 90s and then California based Resmed started under their current name in the 80s,long after CPAP already had a market , so I am pretty sure Resmed didn't have to reinvent the wheel:-)
It will be interesting to observe how this discussion plays out because it seems to me that this forum is significantly biased in favour of Resmed and essentially blind to any real issues with Resmed machines regardless of the credibility or number of complainants.
From everything I have seen of the DreamStation and ResMed APAP machines the ResMed is the superior one. I don't have much experience with the ASV machines. From the few ASV SleepyHead charts the ResMed ASV is like magic. It just makes the apnea events disappear. It is like the machine is programmed to not allow apnea (as detected by the machine) to occur, and that may actually be the simple explanation of it.
LOL:-) Yes, it (Resmed) is "designed to make apnea disappear", by NOT reporting the events:-)
The truth will be in the flow rate graph when you expand it to reveal the detail. Either the breaths will be there or they will not. The machine is simply reporting flow rate on a second by second basis.
I just posted an example of how resmed fails to report clear events, by showing flow rate stationary for over 12 seconds despite a breath provided by the machine, yet resmed doesn't register these events, of which there many many through the night. I guess I have to wait for the image to be moderated now.
It seems that way. I think it is primarily because online forums have been littered with DME's and other parties who have an interest in Resmed products and since Philips Respironics are currently on recall, these operatives use the opportunity to flog as many Resmed machines as they can with dubious and favourable claims. Fact is however that if you do not use a Ozone cleaner to sanitize your machine, you have very little to no worries about the "foam" related recall. In fact I have used this opportunity to purchase brand new Dreamstations online and massively discounted prices, for spare and just in case they decide to discontinue this very awesome product line.
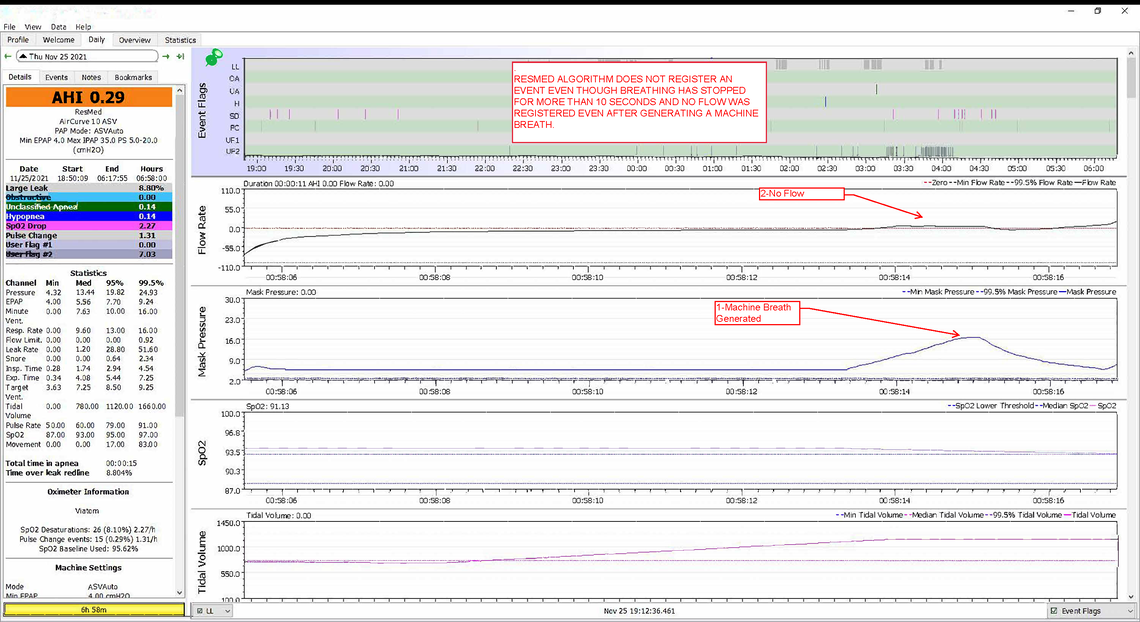
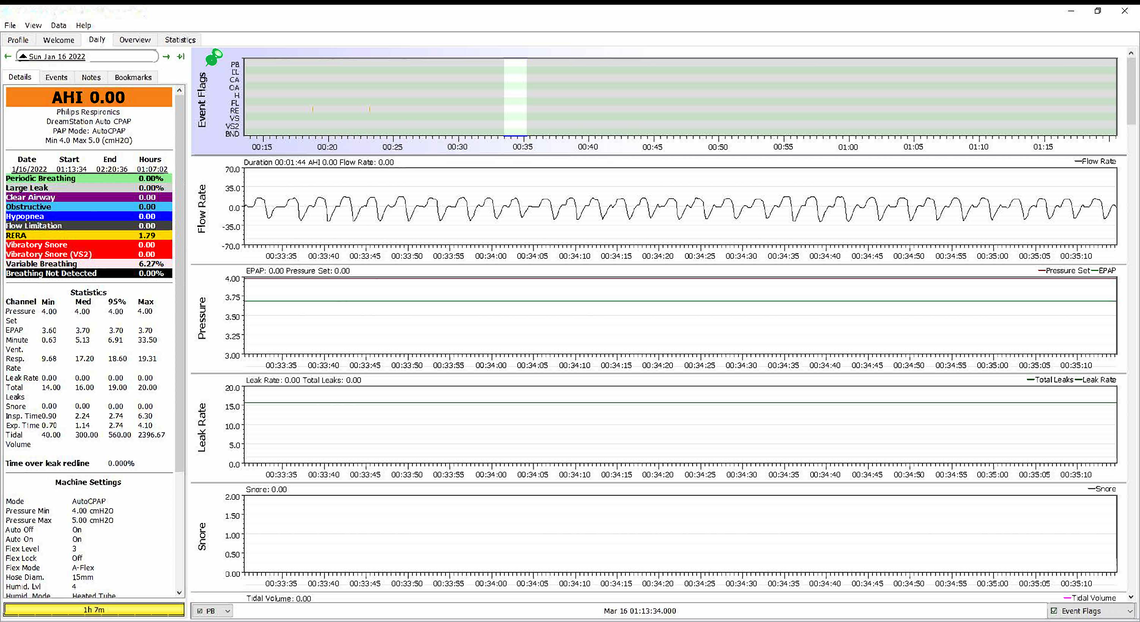
So this is an example of how Resmed fails to register Apnea events. The graph is a slice of about 12 seconds as seen on the time stamp.
"Flow Rate" graph clearly shows no movement in the flow (no air in or out of the upper airway, even though the upper airway is wide open) for over 10 seconds. According to protocol, no flow change over 10 seconds should be recognized as an apnea event, a cessation of breathing or "Clear Airway"...or "Central Apnea event", yet Resmed registers no event whatsoever. In fact that night I had at least 80 (eighty) or so of such events however Resmed only registered ONE:-)
Resmed algorithm appears to have been designed to ignore all events that last less than 15 seconds but international apnea protocol is clear: "A cessation of breathing, lasting up to TEN seconds, is an Apnea event"
I'm just starting on an ASV after both CPAP and BiPAP units didn't work for me. I'm brand new to the ASV and to Oscar so I'll have to consider your thoughts about ResMed vs. Respironics. My ResMed ASV (which was ordered FOR me) appears to be reducing my AHI numbers (both OS and CA) but your point that those readings are inaccurate is not lost on me. For the time being, however, my question is: Why does everyone else get more categories in the Oscar Event Flags list than I do (see picture of mine... no CA event line). I'm just starting with Oscar so maybe I missed something when setting it up?
Also, since you have central and use an ASV maybe you can answer this: If "CPAP just uses air pressure to open up the airway. CA or Central Apnea is when the brain for reasons that are not totally understood simply does not tell you to take a breath. The airway is not collapsed and more air pressure does not help as it is already open."... then how does any kind of PAP device (including an ASV one) treat CA?
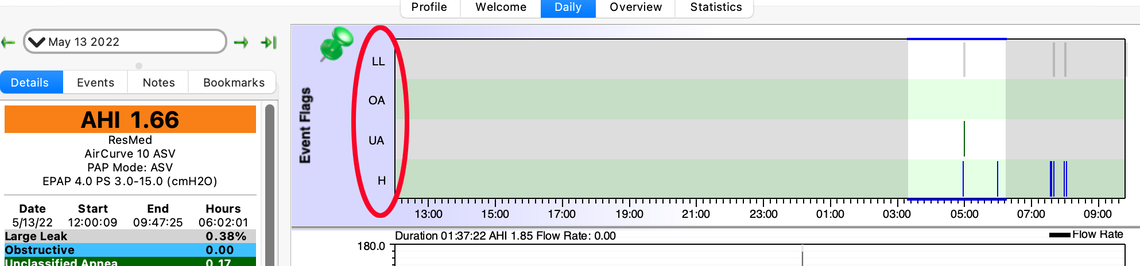
On the bottom left corner of the graphs section of the Daily screen there is a box just to the right of the "Flags" box. The Flags box seems to turn all the flags on or off. The one to the right of that allows you to turn on and off individual flags. You may be correct that if there are no events of a particular type the category may not display in the Events Flag section. I have no shortage of events so I see all of my types...
One the issue of how the ASV suppresses CA events it does it by monitoring the flow rate breath by breath and increases pressure to assist you in making a breath if you do not do it yourself. I do not have an ASV so can't show you an example, but I suspect if you zoom in on the flow rate chart in the area where there are H and UA flags you may see how the pressure and flow responds to potential CA events. You may have to press the up arrow key a few times to get the level of detail needed to see each individual breath and how it may be impacted by the ASV algorithm.
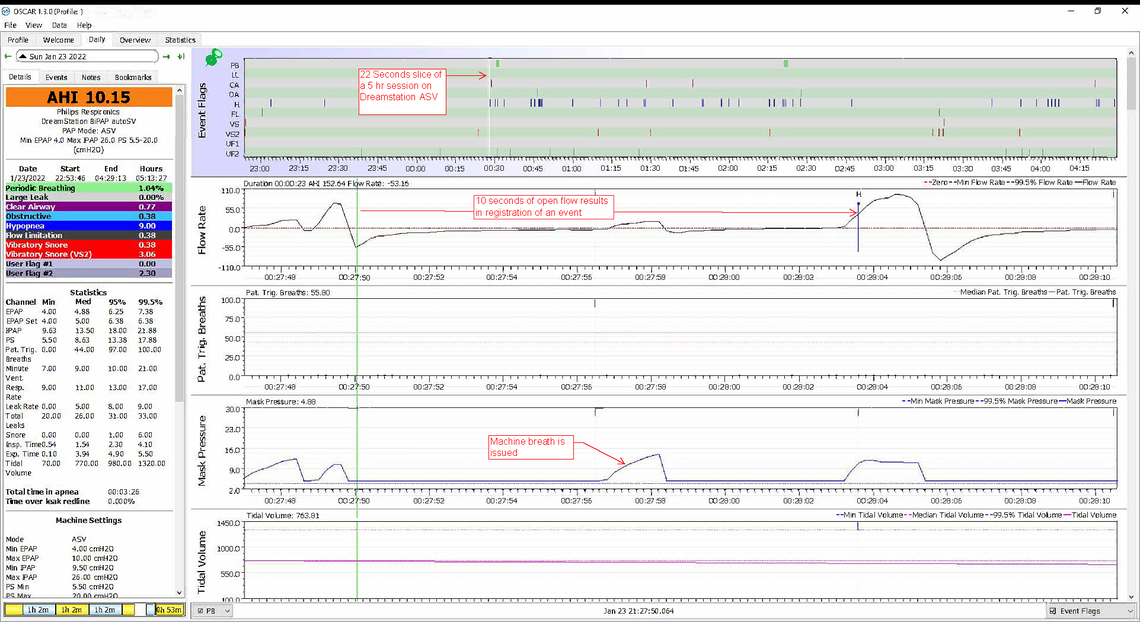
Of course I must post an example of how my Philips Respironics Dreamstation handles an apnea event and how it catches absolutely all suspect events. Below is a 22 seconds slice of a 5 hour sleep session which should a cessation in flow rate (breathing stop). Graph shows the machine issuing a breath however flow does not change significantly. The machine issues another breath and registers a Hypopnea event shortly after. My Dreamstation does this all night. In fact I cannot find a single event that has been missed by the missine, throughout.
When I was participating in a hospital-based support group in CT some years ago, there was a generally pro-RESMED machine attitude/preference based on the ability of the RESMED algorithm to detect the need for higher pressures and provide them within three breaths. But not having used the non-REMED machines, I can’t provide a comparison.
Also, my apneas are almost exclusively obstructive, rather than central. If treating centrals, or mixed Apnea, I would really try to find a practitioner who is very experienced in dealing with the challenging issues presented by centrals.
I just posted a graph above that you should look at. Yes, with regular CPAP therapy provided for the treatment of OSA, it doesn't really matter because all you need is some positive air pressure to maint your upper airway open, so your machine algo does not need a breath by breath analysis, even though I personally think that it should, for efficiency and also comfort of the patient so they only receive positive pressure when their airway is open.
In the case of CSA treatment, the airway is always open , but the patient simply stops breathing (at times), so providing a "Continuous Pressure" is pointless . So the algorithm must monitor breathing and ONLY provide a breath when one is missing (a cessation of breathing lasting more than 10 seconds)...This is why ASV machines are used for the treatment of complex or CSA patients, so again I think that OSA patients too will benefit from ASV therapy just as much, in that they won't have to receive a "continuous Positive" pressure when their upper airway is open.
Anyway, all this means that I am better able to test a machine algorithm for efficacy, than I would be examining a regular CPAP machine that is always ON , providing a positive pressure.
Cyrus: Do you think that years of treatment for obstructives, or perhaps just the aging process itself, eventually leads to the creation of centrals? I’ve been concerned about that, because I watched my Dad develop both centrals and CHF after which he wasn’t able to use PAP and there weren’t any really effective alternative treatments at that time. (Early aughts.)
There was a study being done recently by a combination of Sleep docs and cardiologists evaluating the use of O2 for patients with a combination of CHF and centrals, because there are still no good treatments for that population. Unfortunately, the study was terminated by the NIH before it could reach any useful conclusions.
Well there is a clear scientific observation that connects patients with CHF to CSA. So they believe that CHF can lead to CSA and vice versa. Some scientists want to start studies into whether or not the development of CSA is a natural response to CHF in order for the body to moderate its PaCO2 levels...THAT is way out in the woods for me:-)
Studies also show that "treatment emergent CSA" is a thing, meaning that the long term CPAP therapy for OSA, leads to the development of CSA. (Remember that CSA itself was only isolated as a disorder back in 2008 at Mayo clinic so it is a relatively new subject and under intense study, internationally.) BUT I have also seen studies that suggest " treatment emergent CSA" will go away by itself within 6-8 weeks, after OSA CPAP therapy stops, but who would stop their therapy, unless they get an "implant surgery", like "INSPIRE" at a cost of like $30 K.??
This being said, it does not mean that people can't just develop Central Apnea without CHF (I am an example of that). There is also a clear scientific consensus that "UNTREATED CSA or OSA" will eventually lead to all kinds of Cardiovascular issues, including and not limited to CHF, however it is believed that the long term use of opiates can also be a driver of CSA.
As to O2 therapy for patients with CHF and Centrals, it makes a lot of sense because CSA folks (again like me) can watch their blood oxygen saturation level (SpO2) drop significantly overnight, if they are not using ASV therapy. I would imagine that supplemental Oxygen used in conjunction with PAP therapy for this group (CHF+CSA) would be very efficient and beneficial because CJHF itself is a cause for lowered SpO2.
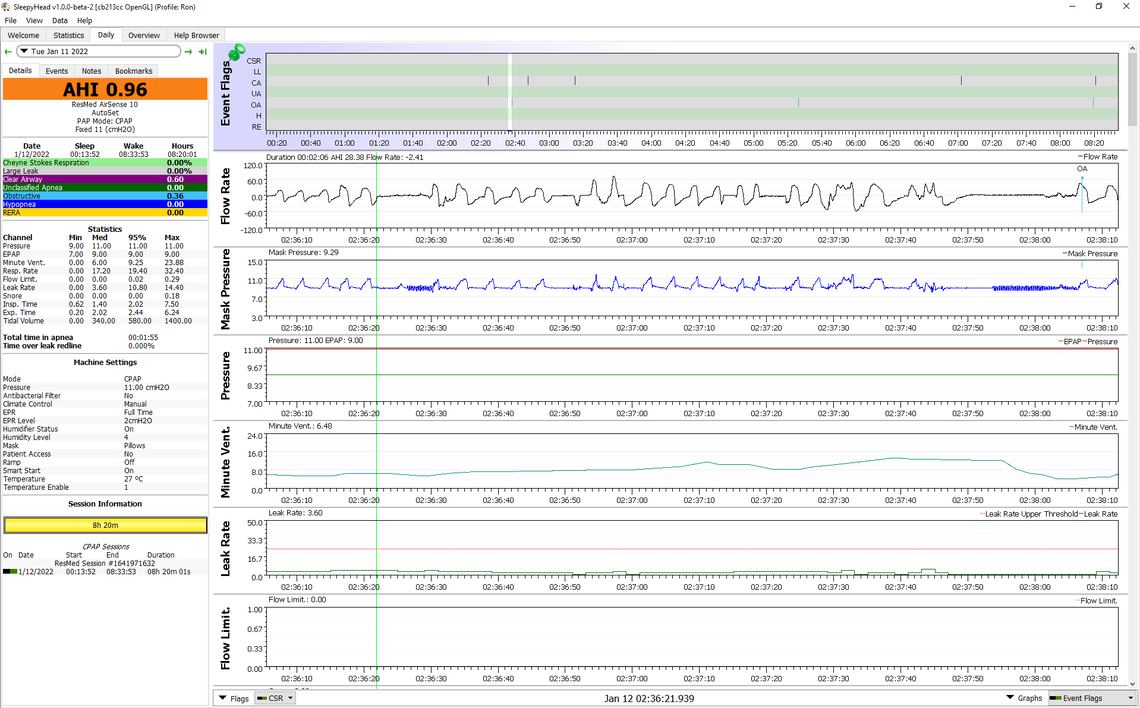
I have not used an ASV and really cannot comment on how the ResMed ASV compares to the Phillips ASV. I have personal experience with a ResMed S9 Auto and AirSense 10 AutoSet. And, have helped numerous people set up adjust their DreamStation APAPs. I have no concerns that the ResMed is ignoring apnea events, and from what I have seen it seems to quite accurately identify them, what type they are, and how long they last. I very occasionally get unidentified events where the machine flags them but does not classify them. It seems to happen when the leak rate is high but not over the leak rate redline. When the leak rate does go over the redline the machine stops reporting all events and when in Auto does not take any pressure action. ResMed claims this is to avoid inappropriate action due to misclassification. Here is an expanded screenshot of a couple of events in succession. The first one lasts about 8 seconds and is not flagged as an event. You can see that after about 4 second the machine starts the pressure pulses to detect the type of apnea it is. Higher amplitude pulses indicate an obstructive event, while lower amplitude indicates CA events. By my eye this one is an obstructive event, but it does not last long enough to get flagged and classified. It has to go over 10 seconds. The second one proceeds the same but lasts longer. Pressure pulse starts at 4 seconds and the total length is about 17 seconds. It gets flagged as a OA event. By my eye the pulse amplitude starts out high but reduces as the event goes on. It in fact may have progressed from an obstructive event to a central during the apnea.
As far as the APAP machines compare I like the ResMed one better because of a few differences:
In any case these are some of the reasons why I recommend a ResMed over a DreamStation for an APAP when I am asked. The DreamStation is still a good machine and I would use one if I had to, but in my opinion it is not as refined a product as the ResMed. And for an ASV things may be totally different. I just have no experience other than reading the Clinical manual for the ResMed model.
We also have both, a Resmed Airsense 10 like yours and a Dreamstation-1 APAP which my wife uses for he OSA. (and no, she does not use the "FOR HER" feature of the Resmed for good reasons...See below) She finds the difference between the 2 machines, like night and day in that she now refuses to use her Resmed altogether.
1- Resmed Airsense algo does what Resmed wants to do, not what the patient wants it to do and thus its response to patient comfort is very limited, even when the EPR is turned on, where as according to my wife, she doesn't even know she is wearing a mask when she is on her DS-1. That is because Dreamstation algorithm to treat OSA is not only more responsive during inspiratory-Expiratory transition, but also much smoother in when changing pressures, unlike Resmed which according to her tends to have a much sharper (jerkier)n transition. so it is not that DS is "slower" than Resmed but that the DS algo makes the transition between IPAP and EPAP a lot smoother so patients can't feel the change with Dreamstation patented C-Flex technology..
2- Resmed's Auto PPAP algio essentially fakes mask pressure on data because they do not have separate sensors for the mask pressure built in, so they just derive this from calculation. The displayed mask pressure therefore is hypothetical, not an actual one, so I wouldn't place too much emphasis on that feature.
3-In contrast, Dreamstation-1 APA reports FLOW rate, precisely measured as you can see in my wife's chart. Her flow rate is perfect breath by breath, in comparison to your Airsense chart which reports a flow rate that is far from perfect, not necessarily because you are not breathing well naturally, but because you are not breathing well BECAUSE of Resmed's faulty pressure delivery. Worth looking into.
4-"For Her" algorithm that Resmed keeps coming up with (yes they have them on their latest model 11 too), is more of a sales gimmick than it is a real medical feature.A pap machine algo should respond to one's respiratory needs, regardless of their gender. Dreamstation machines algos are "Gender-Blind" and this even more "politically correct":-)
5-Her Dreamstation also has all the comfort settings that her Resmed has, including a cool Ramp feature that truly "RAMPS" the pressure up over the period that ramp has been set to, unlike how Resmed controls Ramp which at times jolts her awake. Ramp function should be true to the meaning of the word, a linear increase in pressure, divided precicely over TIME setting, which is what Dreamstation delivers.
At any rate, as the original inventors of PAP technology and their sizeable investment into the development of these essential medical devices, it is natural that Philips-Respironics software has been worked on a lot longer and naturally at a much deeper level than Resmed systems. Problem here is Resmed algorithm clearly does NOT recognize clear apnea events and ignores them, thus reporting a much lower AHI while not delivering full therapy. This is simply wrong .
All I can say is that everyone is welcome to their own opinions. I like my AirSense 10 and that is what we plan to buy when my wife's S9 gives out. Would not consider a DreamStation unless I was forced too. A while back the DreamStation's were so cheap that they are hard to resist, but I would spend the extra for a ResMed. The DreamStation 2 still seems to be about 30% cheaper than the AirSense 10, but regardless nothing in stock of either brand where we buy. I hope my wife's S9 is like the energizer bunny and just keeps going and going...