Hi Folks,
I would like to be able to interpret OSCAR data. My understanding is that OSCAR is geared towards end-users. Or, am I mistaken? I am currently learning a lot from Sierra. But I want to master OSCAR as I cannot rely on the NHS to provide the support that I want. Yes, I'm in the UK. And, at the moment, I don't know where else to turn. This forum is my saviour. How would you all suggest that I advance my knowledge of OSA and OSCAR?
Thanks in advance.
JPC
Hi jaypeecee
You could browse and Wiki and make notes and print lots of stuff and cross reference and dabble and guess and gradually form a kind of comprehension but I reckon the best option would be to do something like this: Uni course
I didn't really read the fine print on that link but there are courses available that are not that demanding and would actually qualify you to work in the industry if you have the means and the enthusiasm.
Of course they won't teach SleepyHead specifically but the official sleep industry software must work on related principles.
ResMed have software somewhat similar to OSCAR, but don't make it available to end users. It is called ResScan. I managed to find a copy of the manual for it, although it is somewhat dated. The Interpretation part starts on page 31. Some of the terminology is a bit different than DreamStation, but for the most part it is quite similar.
Here is a manual that covers a number of models of the DreamStation, That can be somewhat helpful too, but does not go much into interpretation of the data.
Can't write a whole manual, but here are a few quick tips in how you could use OSCAR. I will use one of your posted Daily Reports as an example.
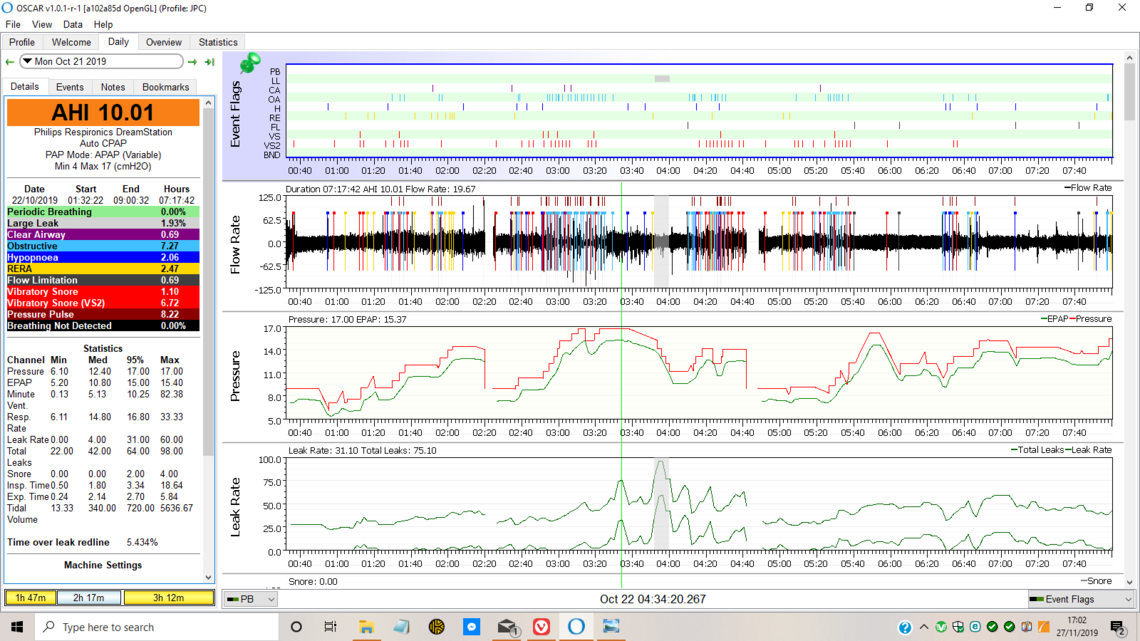
I look at the main AHI number first. That is a indication as to how the night went overall. The objective is to be under 5, but many with uncomplicated obstructive apnea can get under 1. Next I look at the breakdown of the CA, OA, and Hypopnea events. They make up the total of the AHI. If the ratio of the CA events to OA events is low, that is a good thing. From what I have seen, your ratio is low. The hypopnea events which are partial flow reductions but no stoppage are not classified as to whether they are obstructive or clear airway. Most assume they are obstructive in nature, but they may not be. My non professional opinion is that it may be a reasonable assumption that they will be in the same ratio as the CA to OA events are. In your case, most likely close to all are partial obstructions. CA events or CA related hypopnea is when the body simply does not try to breath, rather than trying but being obstructed. It is a very different issue, and you are blessed to not be suffering from it. I won't go into the complications of CA. RERA's are flow events that are likely to have caused an arousal. Generally if hypopnea is low they are low. Generally snoring and flow limitations go down as obstructive apnea goes down.
If any of these numbers are high, and in this example Obstructive OA events are high, I then look at the Event Flags next to see when they happened relative to the pressure at the time. As I mentioned before your machine at this time seems to be unusually set up with a ramp pressure of 10, but a minimum pressure of 4 cm. These settings should be in the Machine Settings panel, which is not displayed in this screen capture. So what happens is the pressure is held at 10 but when the ramp ends and it switches to Auto pressure control it brings pressure down quite a bit. DreamStation machines are set up to do this. They are quick to reduce pressure and slower to increase it. A ResMed in comparison tends to raise pressure quickly and not bring it down so quick. In any case what you see is that the pressure goes down initially and then a number of OA and H events are ratcheting up the pressure. At about 2:20 you must have disconnected the machine briefly, as their is a gap in data and then the steady pressure ramp hold again.
After that pressure ramps up again but does not seem to do a very effective job of controlling obstructive apnea, and you suffer a whole series of obstructive events. Some might suggest that could be a neck position issue and there might be some benefit to using a cervical collar. Or, it could just mean there was not enough pressure to keep the airway open.
At 4:40 the machine appears to have been shut off again and there is a data gap. The ramp up of pressure continues like before with more OA events this time coming when the pressure is lower. When you see OA events at lower pressures, but not at higher pressures, that suggests you will prevent at least some OA events when you set the minimum pressure higher. It avoids those times in the night where you are at lower pressure and are more susceptible to apnea events.
The two lines, one red, and one green, on the Pressure chart are indications of the inhale pressure (red) and the exhale pressure (green). While it would seem intuitive that this is a good idea, to have exhale lower to make it easy to breath out, the problem is that you can get apnea during exhale. So setting this differential, called Flex in a Dreamstation, can reduce the effectiveness of the pressure. I have found it is better to not use the Flex. This can allow the red pressure to come down, and allow you to set the maximum pressure a bit lower.
The Leak Rate chart on a DreamStation is a bit misleading. It plots two curves. The higher one is the total leak rate which includes unintended leaks, plus the intentional purge flow from the mask. The lower one excludes the intentional purge flow, and is the more important one to look at. Not sure about the DreamStation but on the ResMed you can right click on the vertical scale and set a line which is the leak red line. It shows the desired maximum leak rate. You can compare your leaks during the night to that red line. Sudden increases in leak rate that have a flat top followed by a sudden drop can be an indication of an open mouth with a nasal mask. A slow increasing leak is more likely the mask just being dislodges somewhat.
There is of course a lot more to it than that, but these points are kind of the quick and dirty things to check for. The basic objective in setting the machine up for simple apnea is to establish a comfortable going to sleep mode, and then follow that with an effective during sleep mode. During sleep one wants to keep pressure as low as possible but still control obstructive apnea. Obstructive Hypopnea will usually go down as the apnea goes down. And at the the other end you want the minimum pressure to be high enough to prevent the machine from going too low in pressure and causing apnea when in Auto mode. A well set up machine may have as little as 2 cm or so separation between min and max.
Hope that helps some. If you have any questions, just ask, or if you want some help with another area of OSCAR just ask. I find the overview tab and Statistics to be quite self explanatory.
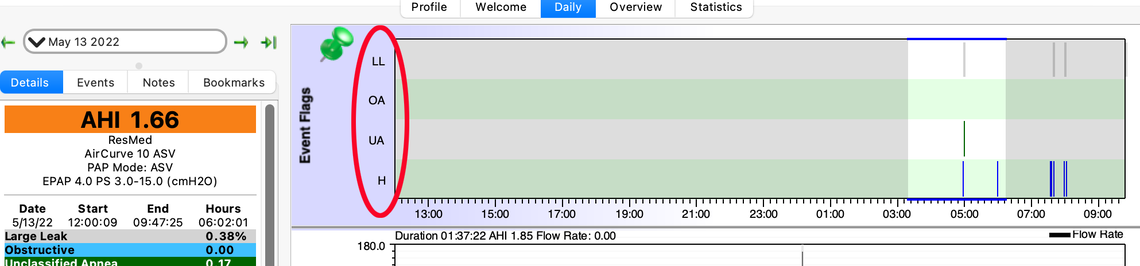
Sierra, I realize I'm responding to a post that's 2 years old but before I start a new post elsewhere, I thought I'd ask here. You mention seeing the numbers in Oscar reports for OA and CA. In jaypeecee's sample, there are a lot more readings than I see in my Oscar report under Event Flags. Specifically, I don't see my central apnea (clear airway) number... just LL, OA, UA, and H.Is it because I'm using an ASV machine? A tangential question is: you've stated before that "CPAP just uses air pressure to open up the airway. CA or Central Apnea is when the brain for reasons that are not totally understood simply does not tell you to take a breath. The airway is not collapsed and more air pressure does not help as it is already open." So how does the ASV or any PAP machine treat central apnea if not by air pressure?