Diagnosed in 2018, I have never been able to use my APAP consistently enough to sleep throughout the night. I recently bought an Apple Watch and have been using the Sleep tracking and have found, no surprise, that I get an average of about 4 hours sleep a night. I don't feel great and have put on a lot of weight. Stuck in a vicious cycle of having low energy for exercise contributing to the weight gain, which makes it harder to exercise. I need to break the cycle and I know getting my sleep apnea straightened out is a must.
The Apple Watch inspired me to take another shot at using the APAP and Googling about figuring out pressures, which lead me learning much more, including how useless the DreamMapper app is for making decisions or troubleshooting difficulties using APAP. This lead me to OSCAR.
I need help interpreting my sleep data. I do know I am a bit terrified by what I am seeing.
My machine (DreamStation2) was set for min 5 and max 20. I've turned the min up to 8 and the max down to 19. I've set the ramp to 9 and the time to 15 mins.
I'm using a ResMed Mirage Liberty Full Face Mask and am a side sleeper.
What is the best way to show my OSCAR graphs and/or data that would help you to advise me?
Thanks.
The best display is the Daily Tab. Set it up to full screen, and on a PC just press the F12 key and save the screenshot image. Find this file with File Explorer and left click on it, and then drag it to an open post here. Use the Orange Reply button at the bottom left of the screen to get a full width window. Here is an example of the way I like to see my layout. The key point is to be able to see the events bar and the pressure so you can figure out at what pressure the events are occurring. Just post one screenshot and then we can look at it. If you post multiple shots it may get delayed in moderation.
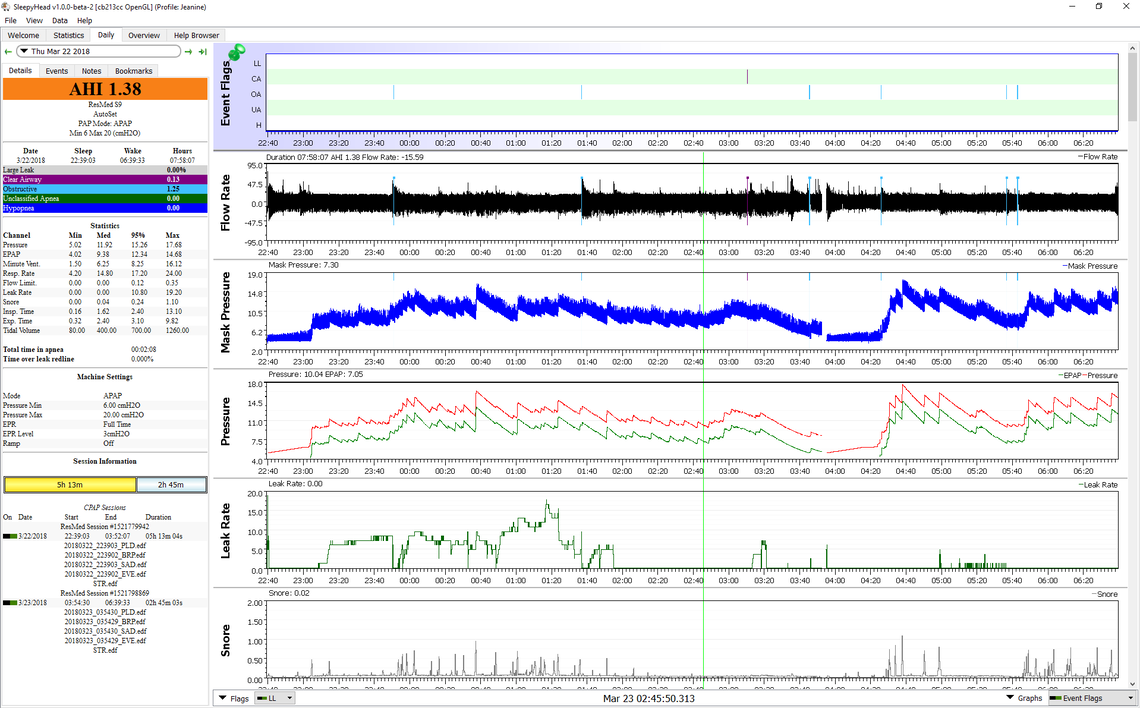
My graphs do not have Mask Pressure.
The largest component of your AHI seems to be hypopnea at about 4.7. In my experience with a ResMed machine the EPR seems to help reduce hypopnea frequency. On the DreamStation the Flex is similar and I see you have it at max already. I would not try it now, but later on you may want to turn Flex off to see if it helps or makes things better or worse. Trying it is about the only way to find out.
I think the first thing I would try is an increase of the minimum pressure. Increasing it to 12 or 13 cm may help the frequency of obstructive (OA) events as well as the hypopnea. I would give that a try for a few nights to see if that helps.
Yes, the DreamStation machines do not calculate or display the mask pressure. The ResMed machines estimate it based on machine pressure and flow. It is helpful but not essential.
Thanks. I'll give raising the minimum as you suggested. I've also made an appointment with the sleep clinic to review my stuff. They're also going to lend me a machine to re-evaluate me. I bought my CPAP out of pocket because my coverage did not cover CPAP at the time. It does now, so I'm hoping to get a new prescription that will cover a better machine and that I will only have to deal with a copay.
While I prefer the ResMed to the DreamStation based on a few minor details, the DreamStation is still a good machine. You do have some central apnea and on the night you posted, some periodic breathing. However, for most people the standard APAP should be good enough. And just changing brands is not likely to make any improvement. If you are short of pressure (and it does not look like you are), then a BiPAP can help. The specialized machines made to deal with central apnea when it is the dominant component and over 5 in AHI are called ASVs. They are very expensive, and again at this point it does not look like you would need one. I would exhaust all the alternatives in settings before jumping to another machine.
I've raised the minimum pressure to 13 and subsequently to 14 cmH2O. I've also backed off the max from 17 to 15 over the past three days. It seems like 16 and above leads to leaks. I haven't tested between 15 and 16. I am, of course using a full face mask. I get dry mouth sometimes even with the full face, so I've purchased mouth tape. This may make me a bit claustrophobic, but I'll give it a try. If I can tolerate it, I may try a nose mask as I understand that, with less surface area they have a lower likelihood of leaking. Still, my graph needs a lot of work.
What do you think?
You probably have a couple of options to try:
Don't try both at the same time. Perhaps try the Flex off first, and then the max pressure increase second.
1) I tried turning Flex off without changing pressures. Oh man it screwed with me. I couldn't exhale, was getting more leaks, and found myself panicking. It did not help that I was having a low blood sugar event (type 2 diabetic) and I was a bit disorientated. First time I've had that experience. I gave up using the CPAP for the evening.
2) Next night, I turned Flex on to level 2 (of 3), set the pressures to 12 min and 15 max, and switched to a nasal mask. I tried the Mewing technique to keep my mouth closed. I don't buy the fad that it will fix your jaw and all that, but I did find that the tongue position did create a seal and I was able to sleep throughout the night, except for one bathroom trip, with an unbelievably low leak rate and no dry mouth. I still had too many OAs, Hs, etc, but I still considered it progress. Even with a full face mask, I was getting dry mouth and woke up several times a night.
I had tried a full face mask when I first got my CPAP, but was unable to tolerate it. I felt like my mouth was being forced open by the pressure. Either that, or I'd end up getting stuffed up. In hindsight, I realize that I was poorly trained by the technician and that the 5-20 cmH20 I was set up with was too high and was enflaming the turbinites of the nasal cavities. I believe the lower max pressure I used, 15 cmH20, helped me tolerate the nasal mask. I would say it was almost comfortable (Phillips Respironics DreamWear Silicone Nasal Mask). I woke up in the end almost refreshed.
3) Last night, I turned Flex on to level 1 (of 3), set the pressures to 13 min and 15 max, and continued with the nasal mask and Mewing. Again, I only woke up once to use the bathroom and had no dry mouth and an amazing leak rate. Still too many OAs, etc. Lots of snoring.
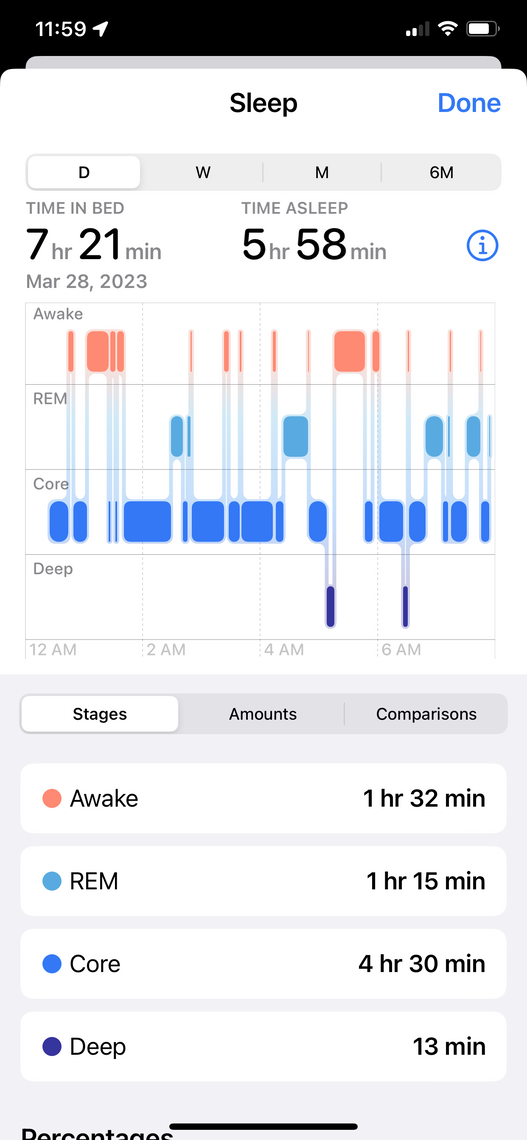
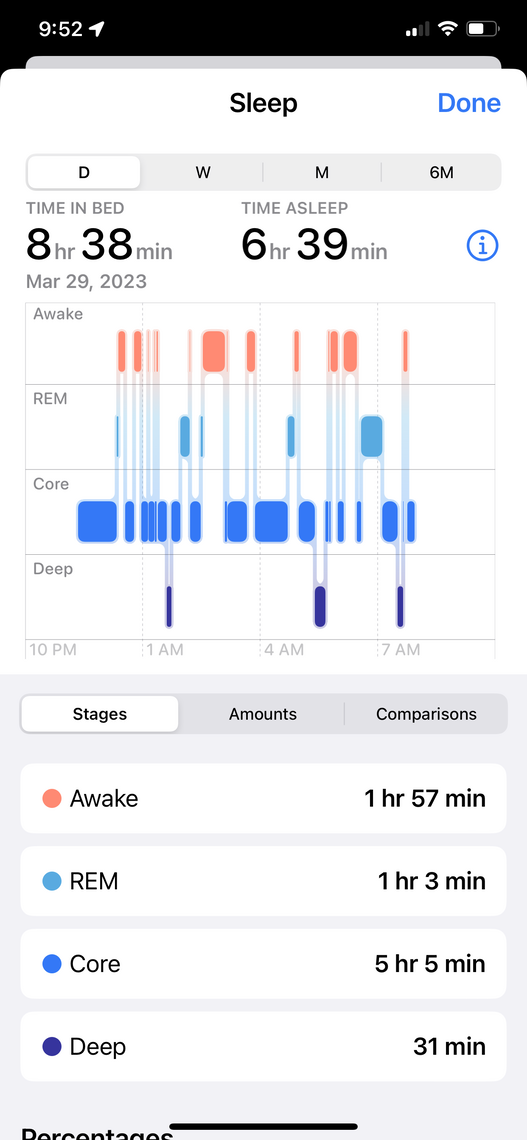
Also, per my Apple Watch, my REM and Deep sleep cycles are vastly improved. I used have had none of either for for the longest time.
After you settle on the best flex you may then want to try a fixed pressure in CPAP mode.
I'm using the Libre 2. It's what alerted me to my low blood sugar while I was trying to sleep.
I haven't given up on the idea of turning Flex completely off. I may have better response to having it off with the nasal mask. I will test this out again at some point. Meanwhile, I'm going to raise the lower pressure to 14 and the upper to 16. As you mentioned before, the CPAP is being kneecapped by limited it to 15. I wasn't able to do 16 before because the full face mask would leak too much, but I think I will get better results with the nasal mask.
I am trying to move towards fixed pressure CPAP mode. It seems, from what I've seen on the LankyLeft27 and CPAP Reviews YouTube channels, the best path. I am trying to get evaluated for BiPAP.
Thanks for all the guidance.
I am not so sure based on what I have seen of your results that you would benefit from a BiPAP. The only real difference between what you have and a BiPAP is that a BiPAP can go up to 25 cm maximum pressure instead of 20 cm. And the BiPAPs typically can give you up to 10 cm differential between inhale and exhale, while what you have with Flex limits you to 3 cm differential. It is not obvious at this point that you would benefit from either of those features. I have watched a few of the LankyLeft videos and to be frank, I think he is a bit of a wingnut. Be careful with his advice.
Another thing to keep in mind is the use of a cervical collar if you have OA events in fairly rapid succession. Have a look at this thread. The OP has had very good outcomes with the use of a cervical collar in reducing OA event frequency. The idea is that it keeps your airway straighter and not kinked during sleep.
https://myapnea.org/forum/being-recommended-for-bipap-1-year-out-from-craniotomy
Good that you have the Libre 2. I tried one of the Libre 2 sensors and had issues with getting it to run on my iPhone. I've been waiting for an update to the Libre 2 app to bring it in line with what I have on my phone. They seem very slow in updating their apps.
I think the feature I think is favorable about BiPAP, if I understand them correctly, is that the min and max are set pressures, instead of relying on the pretty bad algorithms of APAPs to make correct adjustments, if any. Again, I'm looking to be evaluated. It may not be the right solution. Frankly, I'm hoping I'll have my APAP dialed in before my appointment.
I have a rectangular pillow and sleep on my side. I have always been a side sleeper. The pillow helps eliminate shoulder pain and, depending on the mask, minimizing interference with the mask and hose. I think my head position is okay. I have a fat neck and I don't think I could tolerate the collar.
I do find LL somewhat arrogant and I weigh his advice against others, like Nick on CPAP Reviews.
The only problem I've had with the iPhone app for the Libre 2 is that it wasn't available for a while. It's been fine for me (iPhone 11 Pro Max with iOS 16). I do hate that there is not Apple Health integration and I don't think Abbott intends on ever supporting it.
I believe at least the ResMed BiPAP still uses pretty the same algorithm as the APAP. The differential between the IPAP and EPAP is fixed but you can set it up to 10 cm, rather than 3 cm.
The aspect I like about the ResMed compared to the DreamStation is that the ResMed increases pressure fairly quickly and then is much slower to reduce it. The DreamStation in Auto tries to reduce pressure right away. So, it can spend the night going up and down quite a few times. But, you can take this away by narrowing the differential between min and max pressures. Or, if you switch to a fixed pressure than it is irrelevant.
I changed my pressures from 13 min and 15 max to 13.5 min and 16 max. No other changes. Other than waking up to use the bathroom, I also woke up to find I had rolled towards my back and had a mouth leak.
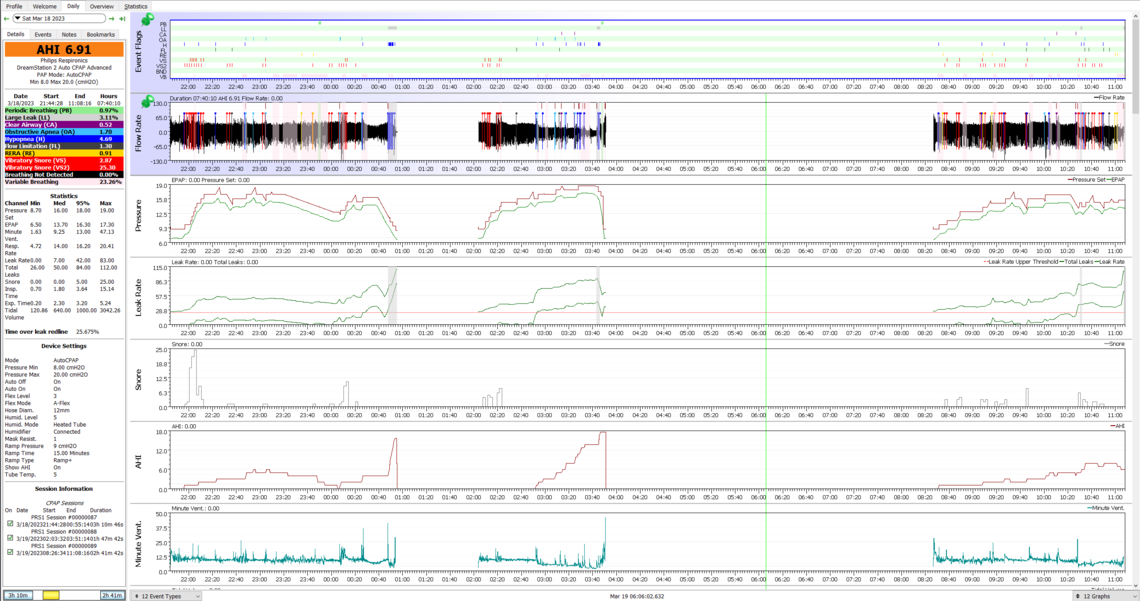
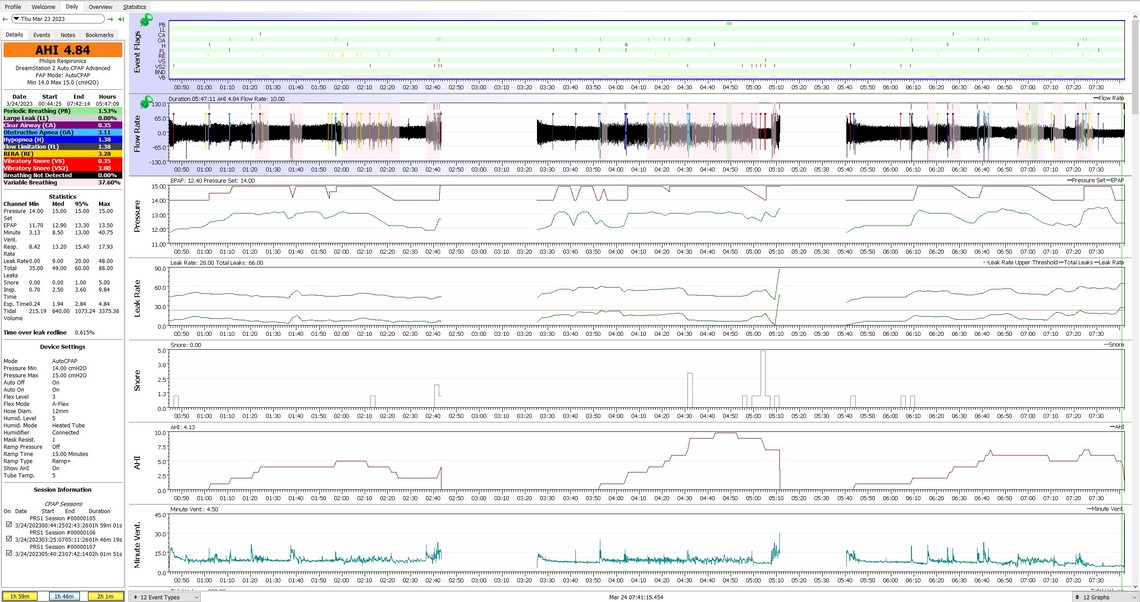
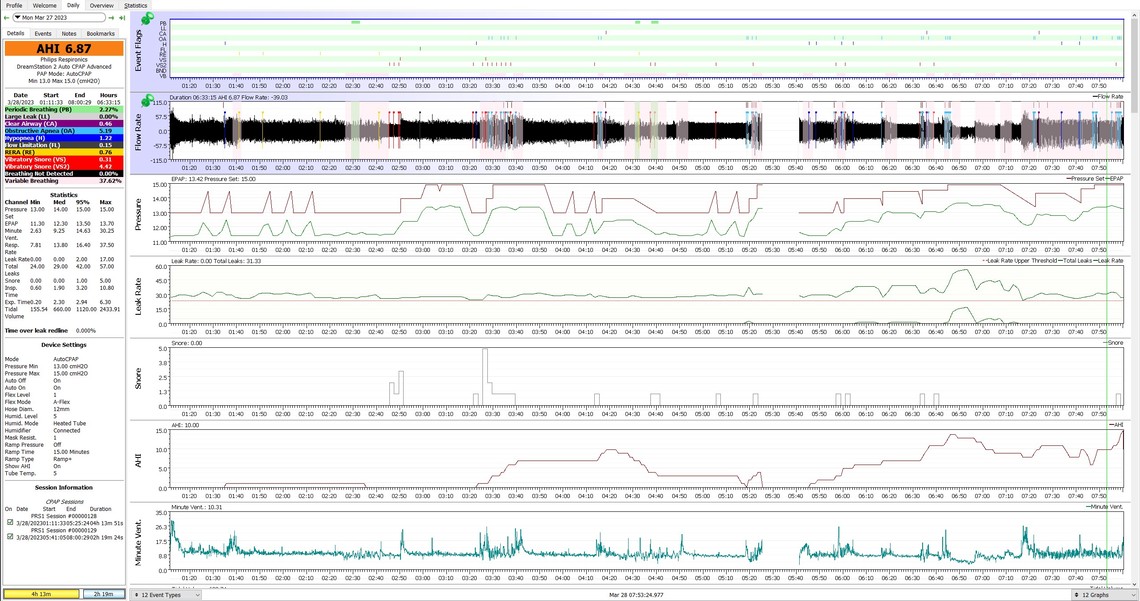
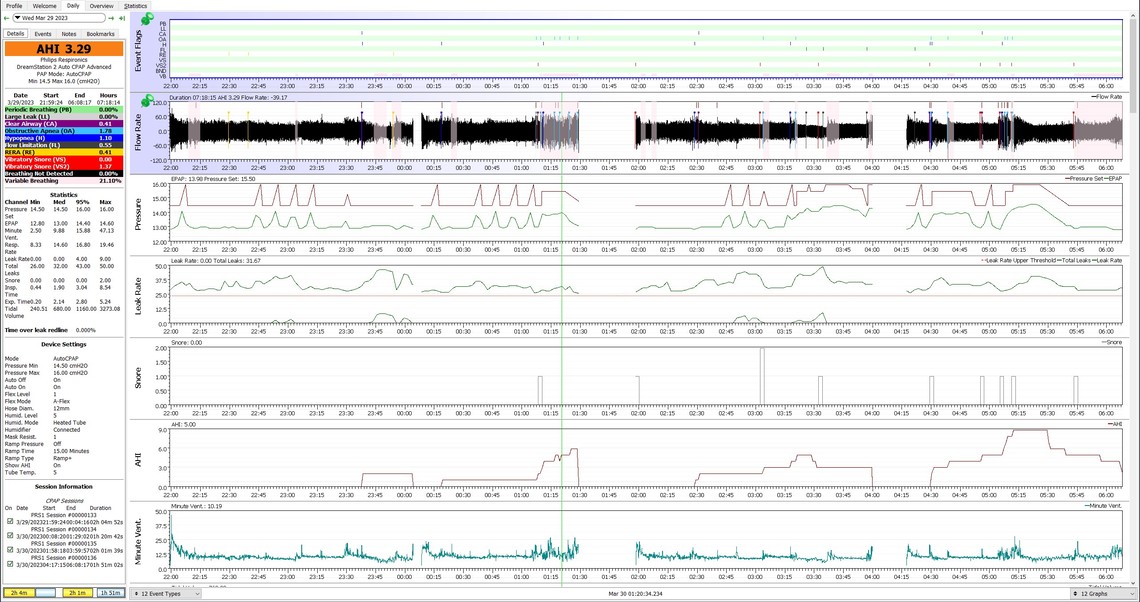
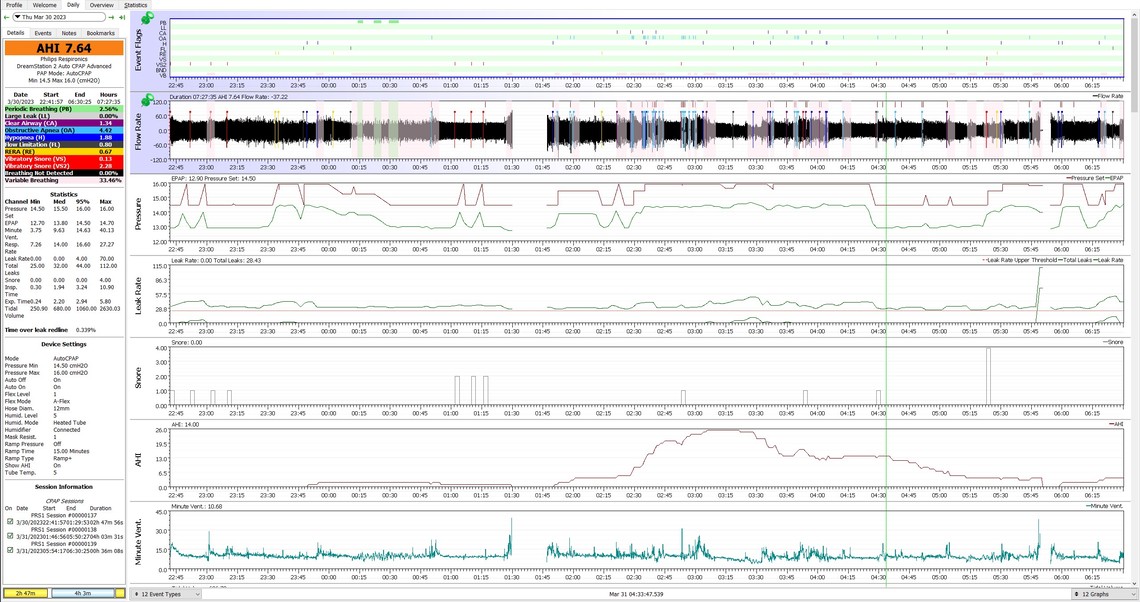
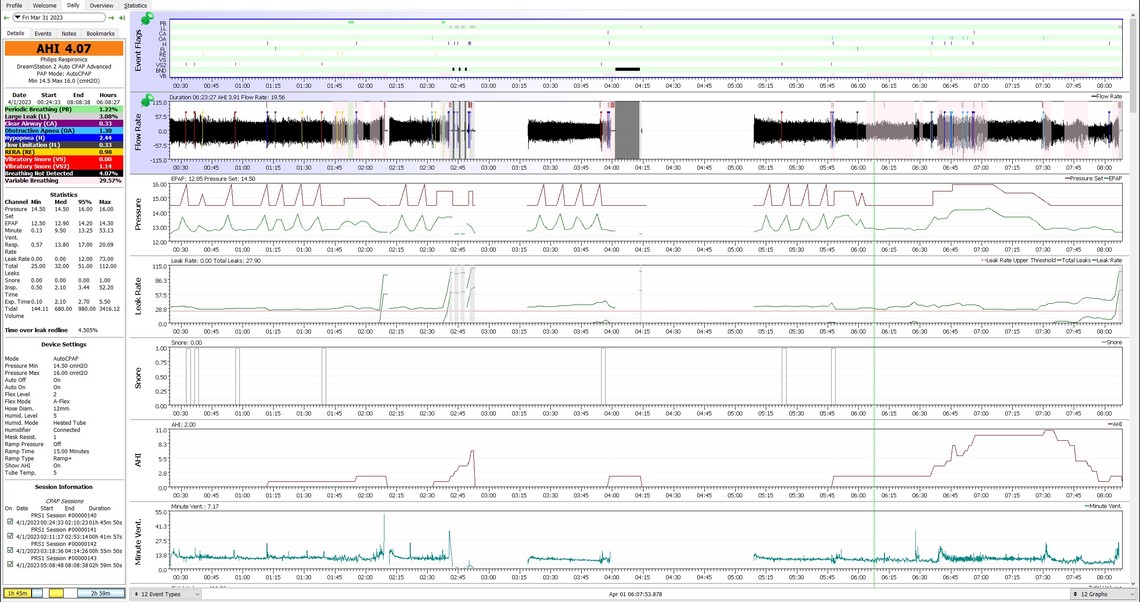
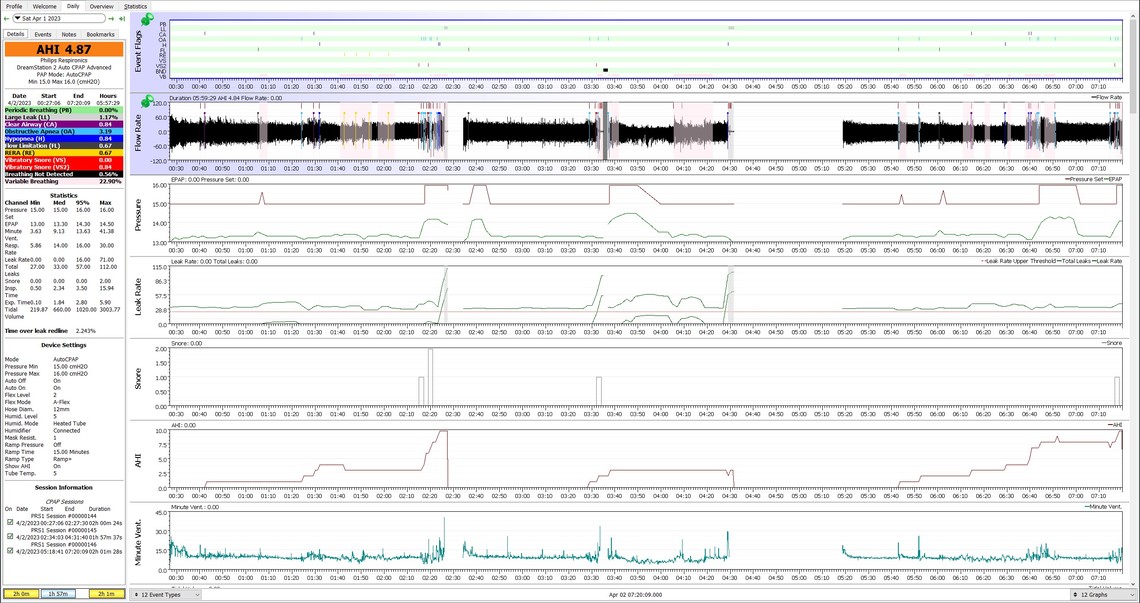
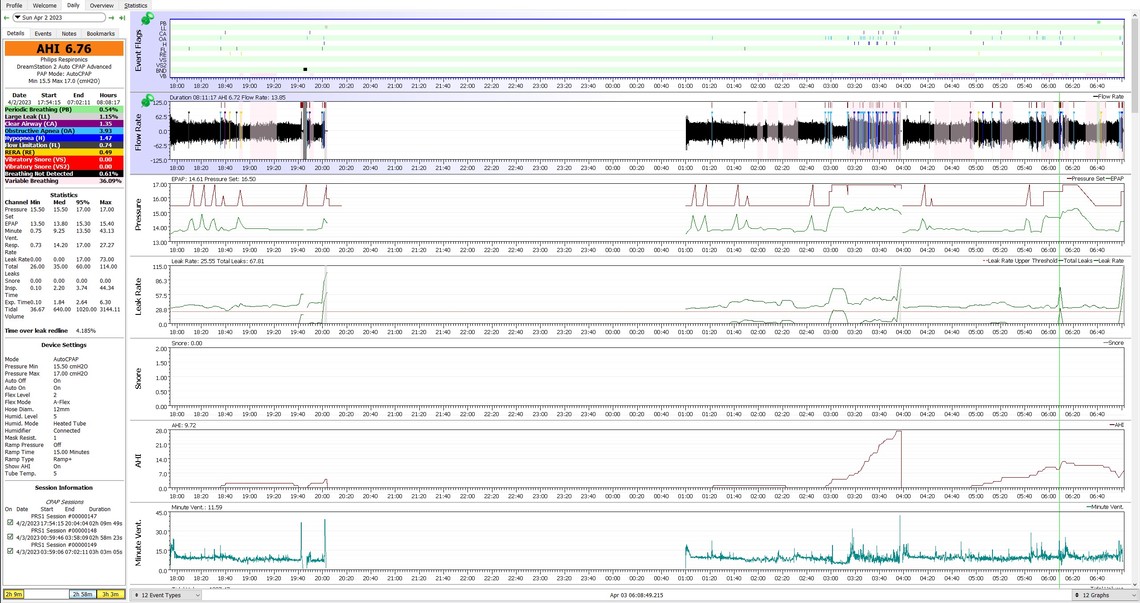
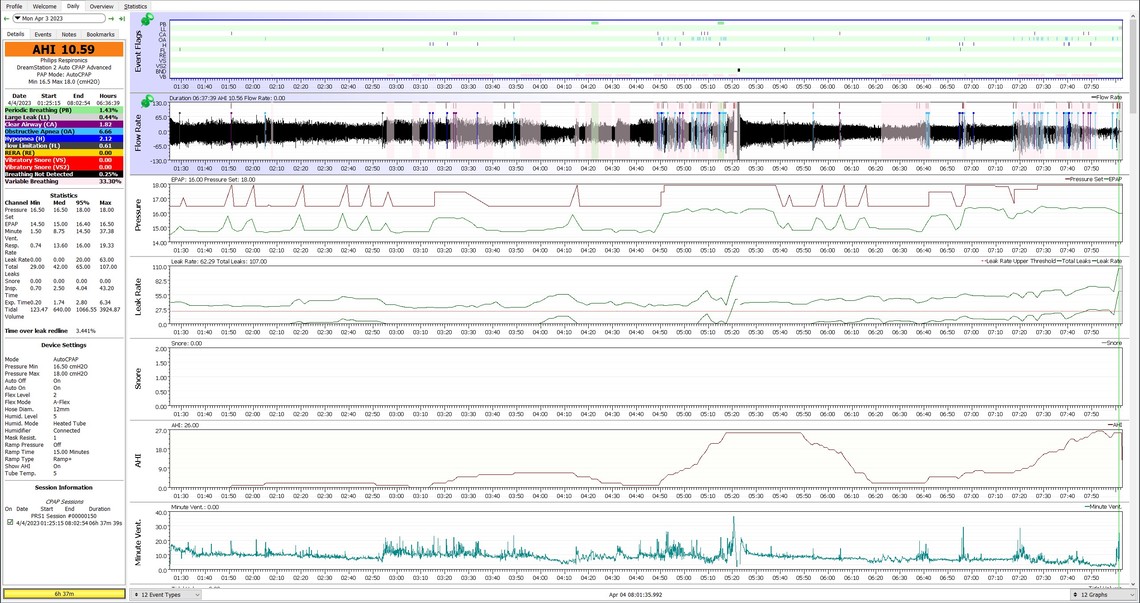
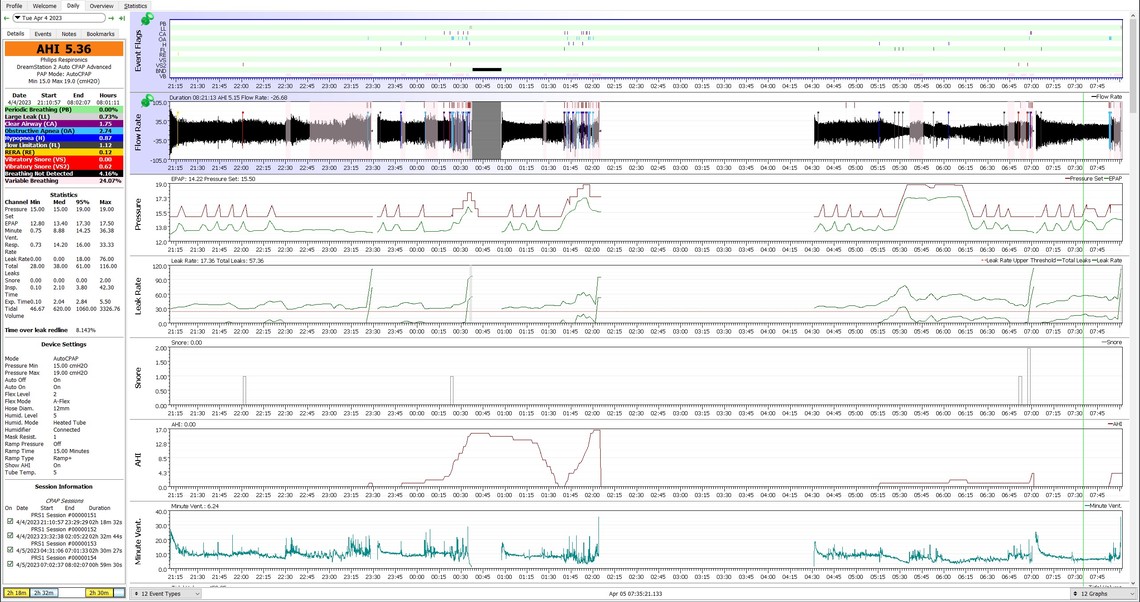
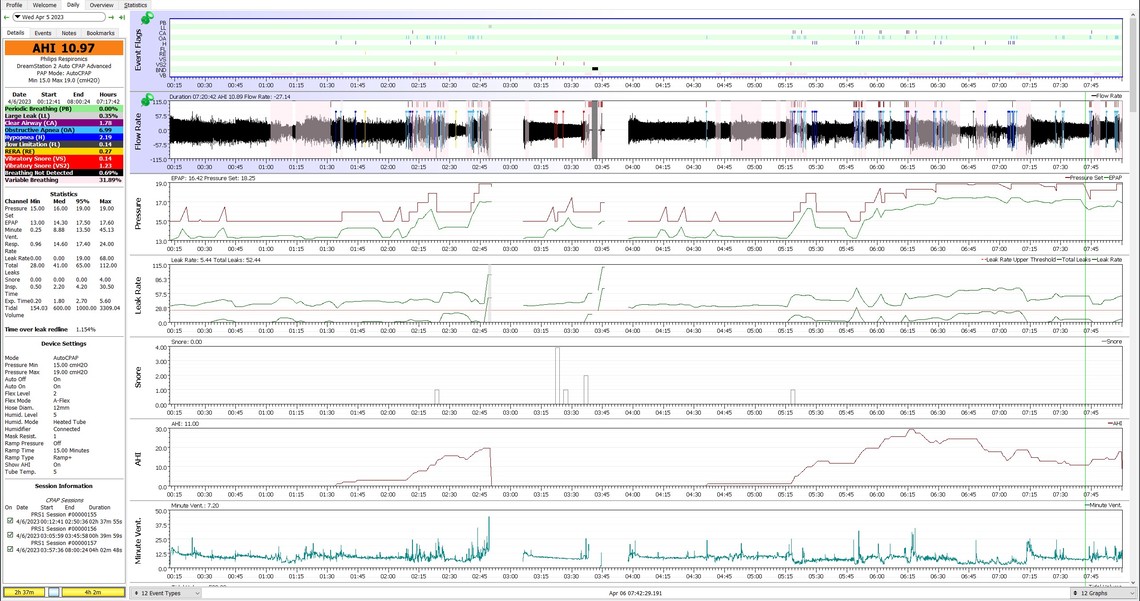
I've included my graph for last night, a comparison of my daily Details since my first post, and last night Apple Sleep graphs.
Thanks, John
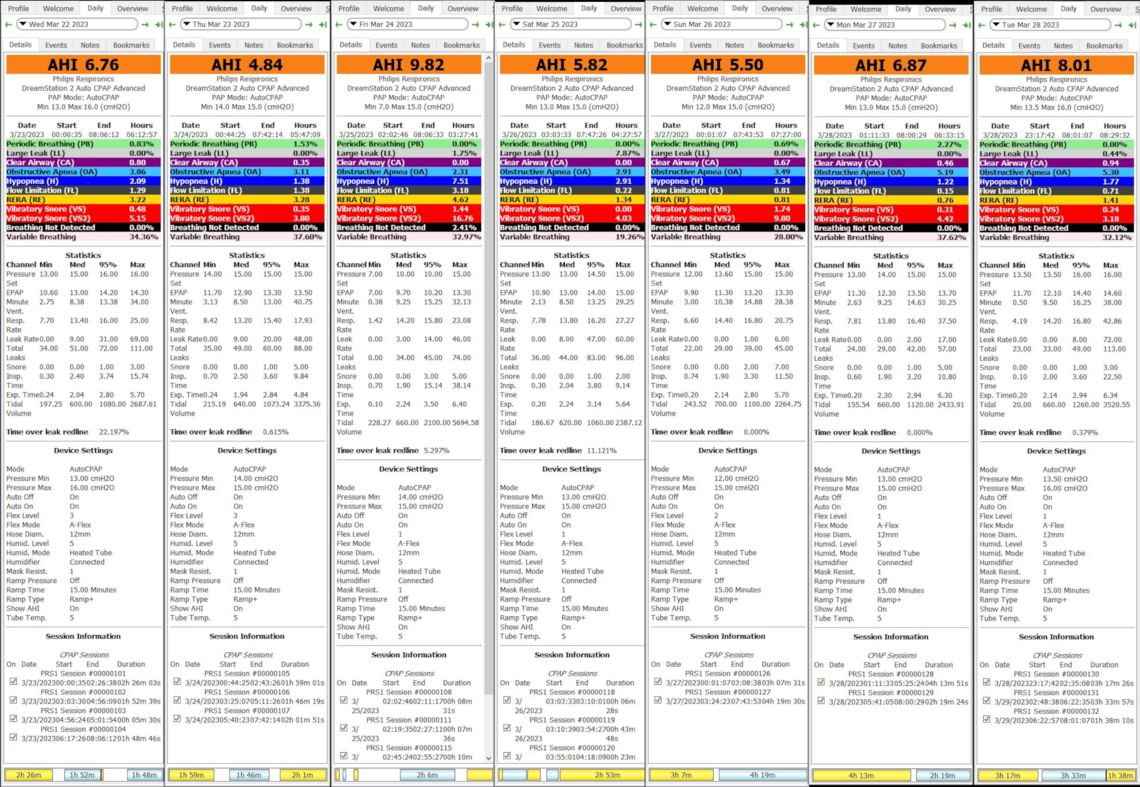
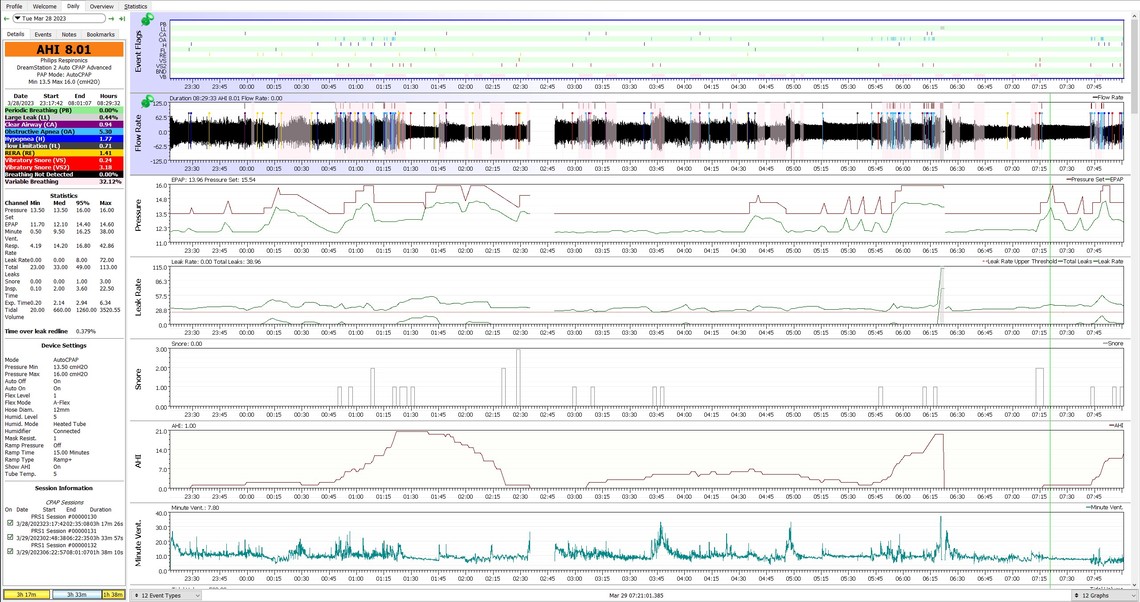
About all I can see for a pattern is that you got the lowest AHI with a minimum of 14 cm and Flex at 3. Raising the minimum can often be the best solution to high OA frequency. It can be more effective that raising the maximum. Narrowing the gap between min and max is more and more like a fixed CPAP pressure mode.
Raising the minimum has been my primary target :) While I may not have found the right pressures yet, I'm feeling optimistic that I will get there. I'm happy that my sleep stages are getting better.
The main reason I even started dropping the max pressures was mask and mouth leaks. I feel I can now raise the max pressures, if needed, with the nasal mask.
I raised my min from 13.5 to 14.5 and left my max at 16 and A-Flex at 1 two days ago. Woke up more (as opposed to arousals). Some difficulty exhaling at the start. I've never been one to panic, but CPAP definitely triggers panic in me and I have to be conscious of not hyperventilating. It may take some time, but I believe I will get there. I kept the same settings last night thinking that I need to get used to the settings and compare the results with the same settings. Second night (last night) was worse. I'm really pushing myself to find the right levels, but I guess I can't rush the process. I know that even when I find the right levels, they will change as I get healthier.
Here's the two graphs from last night and the night before with the same settings:
If you can increase the Flex to 2 or even 3 without increasing your OA frequency, it should help with the exhale effort. It may also reduce your hypopnea. But, as I said before, everyone is a bit different and trying it is the best way to find if it works or not. Same with going to a fixed pressure instead of automatic. You have to try it to find out if you gain or lose with it in fixed mode.
Here are screenshots since my last post. I don't know or remember the rules (looked for them). If it is okay, I can post a link to a google drive location where I can post these instead of putting too many in a post here.
The issue with posting multiple images is that it can trigger the spam filter. After you have made several posts it seems to be OK after that. The spam filter is a little mysterious in how it works...
About all I can say for what I see in these is that higher pressure seems to help sometimes. The majority of OA events are occurring when pressure is maxed out. It is possible that you may need a BiPAP with a 25 cm max pressure.
One other thought is sleeping position. Most people will have a higher apnea frequency when they sleep on their back, compared to sleeping on their side. If you have any awareness of when you are getting these bursts of OA events you could see if the cause might be sleeping on your back. Some people go to the extend of sewing a tennis ball into the back of their PJ's to discourage sleeping in the back position. Another recent poster here has had some success with this trick.
I had my appointment with the sleep tech at Kaiser last Tuesday, April 11th. The plan, in my mind, was to get evaluated for a BiPAP. I talked about what I was doing with OSCAR and my Phillips machine. The tech knew nothing about OSCAR and of course did not trust it out of ignorance. He assumed OSCAR was manipulating the data and I insisted it just showed the data in a graphical form. Also, I asked him if they even looked at the data for my Phillips at their end. They did not. He gave me a Resmed Airsense 10 as a loaner for a week and I have a follow-up appointment tomorrow. He asked me to not mess with the settings. I assured him I would not. I asked him what the settings were and he told me 5-20 cmH2O. I asked him to raise the lower to something like 10-13. I told him my current weight and he did raise it to 10 cmH20. I've been using the Resmed consistently. It has been surprisingly more comfortable than the Phillips. Unfortunately, the tech did not put in a SD card, so I was unable to upload the data. I do know that the settings are not getting me better sleep or rest and I am waking to often. Most nights, the numbers look good on the Resmed, including leaks, but I know how deceptive that report card can be. I'm concerned the tech will just go by those number and say I'm good to go.
There are no real big differences between the SleepStation and the ResMed. I prefer the ResMed, but I am not sure it is significantly more effective. Both my wife and I have the ResMed AirSense 10 Auto. She has the For Her version. In Auto the ResMed I believe is slightly better as it does not drop the pressure so fast after it raises it. Makes for a more constant pressure during the night. And, the EPR may be slightly more effective than the Flex. But, again the differences are very minor.
Unfortunately I don't think these techs know much about the machines and how they work. They just put them in Auto with a very wide range and hope for the best. A new machine out of the box is set at 4 to 20.
It is too bad that you did not put your own SD card in the machine so you could collect the data. All you needed to do is delete the data from the SleepStation and then use the card. To put it back in the SleepStation just delete the data again. They would not know that you saved the data to Oscar. OSCAR is smart enough to combine the data from the two different machines, so you will not lose any data in OSCAR. I periodically delete the data on the SD card as it makes it more responsive for downloading.
Having used both the Phillips and the ResMed, the ResMed felt better, though things still needed dialing in. Also, Kaiser doesn't support the Phillips, including having tools to look at the data. If I'm to get any support from Kaiser, I'll have to switch to the ResMed.
Kaiser lent me a BiPAP and my results were worse than the Airsense 10 they had lent me. They had also set it for higher default pressures which was blowing the fit of my full face masks and blowing my mouth open with the nasal pillows.
At this point, I managed to get them to refer me to an in-clinic sleep study. Hopefully, that will get me closer to a therapeutic solution
I hope you are making progress with your in-clinic sleep study.
You mentioned in an earlier post that you use a FreeStyle Libre 2. I have just started my first Libre 2 sensor that has worked (kind of), but I am having significant issues with it. I have an Apple iPhone 8+ and am on IOS 16.1.1. What is happening is recurring "Signal Loss Alarms". When I check the Bluetooth on my phone, the pairing has been lost. This is happening even though I always carry my phone in my pocket and it never gets more than a couple of feet away from the sensor on my arm. To clear it I have to turn the alarm functions off and back on again. Are you having any issues like that, and can you suggest any solutions?
I have an iPhone 11 Pro Max and iOS 16.5 and gave up on Signal Loss Alarms in the Libre 2 app a long time ago. It was constantly going off. I turned off the Signal Loss Alarm, as well as High Glucose and Low Glucose. I've left the Urgent Glucose Alarm on. Even when I get that alarm, I'm rarely that low when I double check with a finger stick.
Regarding the in-clinic sleep study: I'm on a list waiting for a cancellation. My study is complicated by my physical size (obesity) and because I have a seizure disorder. The size limits me due to they only have so many beds and toilets that will accommodate me. The seizure disorder requires they have someone monitor me one-on-one, rather than monitoring multiple patients.
My seizures have been under control for quite some time, but then, I don't know that I haven't had any during my sleep. I desperately hope this is not the case. I don't want to lose my driver's license.
Good to hear you are at least in the queue for a test. If you have a one on one test that should at assure they watch what is happening.
The Libre 2 has settled down a little bit. The annoying alarms are the signal loss ones. There seems to be no reason for them. I have the phone in my pocket less than 2 feet away from the sensor. For some reason I do not see an option on my app for a Urgent Glucose Alarm. I just have the high, low, and signal loss. My app version is 2.8.1.6120, and it seems to be the latest one available. I have been afraid to update my iOS as I initially had problems a few months ago with my first try with the Libre 2 and Abbott blamed it on my iOS. Perhaps I should update my iOS.... My phone wants to update to 16.5, but I keep holding off waiting for Abbott to update the app. Supposedly it is only approved for 16.1.0.
I took the plunge and upgraded iOS to 16.5. So far I have not had any loss of signal alarms, but that may be coincidence. I still see no evidence of any Urgent Glucose Alarm function. I have been edging up the Low Glucose Alarm setting to give me more time to intake some carbs to prevent a real low glucose situation. Currently have it at 4.2, and I may have to increase it a little more from there. I don't consider it to be a real low until it goes under 3.7 or so.
I got called in for the sleep study this past Sunday (May 21). Between all the sensors they attached to me, the overly firm mattress, problematic pillows, (unfamiliar bed) and my stress at getting good readings, I only managed to sleep for about 30 minutes according to the clinician. They still thought they got enough data to get me dialed in and also select the right machine, but I am exhausted. It seems likely it will be a BiPAP. They also fitted me with a couple of new masks. While the clinician could not tell me the pressure settings they put in that cleared my airway, I do know that it was over 20 cm/H20, which my personal machine cannot do. That pressure is BiPAP level.
Knowing that pressure was >20, I set my machine to 20 and wore one of the new masks. When it's on, it seems to help, but I've taken the damn thing off in my sleep. I'm thinking about taping the buckles with gentle adhesive tape to discourage removal in the night.
It'll take a couple of weeks for the doctor to review my results and come up with a prescription for settings and a machine.
I am concerned about how short the sleep I got and the amount of data they got, but I figure that, bottom line, with a new prescription, I can get a machine they support and can monitor remotely and make adjustments to my therapy.
Regarding the Libre 2 software on my iPhone, I'm running 2.7.3.3641. I regularly update my apps and I do not see 2.8.1.6120 in the app store. I appear to have the latest. Actually, I just found that the version you are mentioning is for FreeStyle LibreLink - US, and not for FreeStyle Libre 2 - US apps. I am using the latter.
Well at least you got a sleep test done. I don't think I would be a good candidate for an in lab sleep study. I can't think of a more difficult place to sleep than that. My apnea diagnosis was done with an at home Phillips Alice Night One or something like that. Probably the worst night of sleep in my life, but they said the test was good. In any case if your BiPAP is compatible with OSCAR you should be able to tell how well it is working for you. And if the extra pressure is not needed, on most machines you can set them up to be the same or very similar to an APAP.
On the Libre 2 app there appears to be Canadian ones which may be different from the ones in the US. Perhaps that is why I don't have the critical low alarm. May be a feature of the US app...
I was diagnosed with a machine that Kaiser sent me home with 5 years ago. It had a pulse ox and recorded audio. I don't know brand or model. The sleep clinic was not for diagnosis, it was for getting a better idea what the solution would be.
Last night, I put cover roll stretch tape over the clips so I'd have a harder time accidentally removing my mask while sleeping. It seemed to delay removal, but it still happened. Partial arousal is worse than waking up to consciousness. At least if I'm conscious, I am more likely to put my mask back on.
I'd love to have some sort of alarm that would wake me when my mask is off for a given period of time. No SO sharing my bed, so that's not an option :P