I’m 81, I’ve been on CPAP for almost 3 years. My nightly AHI count is fine, at around 1. I rarely, if ever, had CSR events, but lately the OSCAR read-outs report CSR events more than usually Last night I had two of them, with a duration of 506 and 1067 ( seconds, I suppose)., respectively almost 18 minutes. It seems to me a hell of a lot, even though, I feel well, as usual.
I spoke to my respirologist. I had my annual apnea check-up about two months ago and everything was normal. He finds it strange that I should have CSR’s all of a sudden. I have requested an appointment, but the system is overloaded and it will take some time. I’m in very good health, generally. I’m on betablocker for occasional atrial fibrillation in the past, but I am exercising ( running) regularly.
I’m a bit intrigued, ( to say the least !) because medical literature associates CSR’s with congestive heart failure( of which I have no sign) and dying events.
Awaiting to hear from my doctor, I’d like to understand a little better about CSR.
There seems to be a connection with CO2 levels . If there is too much CO2, the system reacts with hyperventilation in order to remove the excess CO2, which depresses or slows s down breathing and this goes in a loop, sort of vicious circle. . Beyond this, if CO2 retention is the cause, I cannot understand what causes it, to the point of triggering the stop-and-go breathing pattern underlying the CSR. Perhaps the mask pressure ( too much or two little IPAP-EPAP ) needs to be adjusted?
I wonder if somebody is familiar with this issue.
Thanks
Ittiandro
I have had significant issues with CA events and occasional CSR flagging. It is a complex area and the combination of OA and CA events are called complex apnea. One of the better articles on the issue can be found here:
https://myapnea.org/blog/complex-sleep-apnea
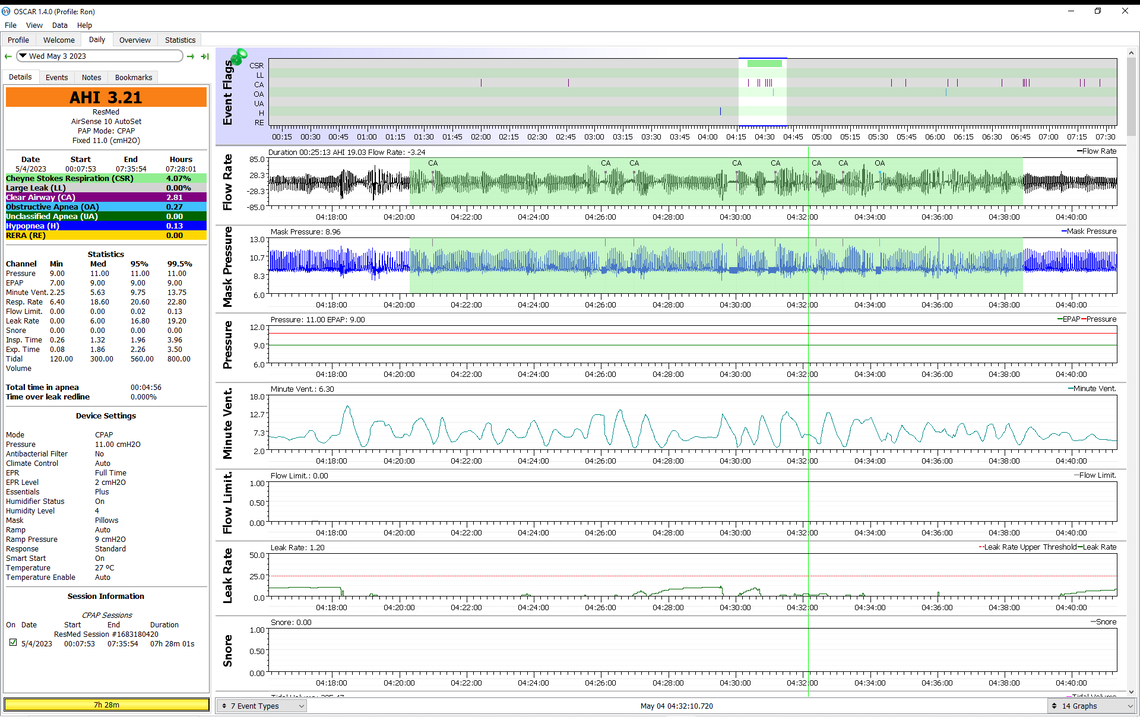
I am also on a beta blocker (bisoprolol). I was convinced that it was contributing to my CA frequency and CSR and convinced my doctor to reduce my daily dose from 5 mg to 2.5 mg (I split a 5 mg). That seemed to help some. And over the past year or so, I have made some changes to my CPAP settings. I had my EPR set to ramp only and I switched it to full time and set it at 2 cm. That has had a large impact on my hypopnea frequency, and it seems it may have also reduced my CSR frequency. I still see the periodic repetition of the CA events, but very seldom do they get flagged as CSR any more. That is about the only changes I have made. And of course I have not gotten any younger! I'm pushing 74 now.
It may be worthwhile discussing it with a cardiologist to see if they can suggest anything. Not sure what you are taking for a beta blocker, but my doctor thinks bisoprolol is better than the more common metoprolol (at least for me). You may also want to discuss the dose. I am mainly taking it for BP control, and also use perindopril. The combination seems to work quite well for me, but everyone is different when it comes to BP issues...
I am convinced that CSR is a blood circulation issue. That in turn leads to an instability in the control system that keeps O2 and CO2 at a constant level. But, the details are complex.
Another thing you may want to do is discuss the use of an ASV instead of an APAP with your respirologist. See this link. I am quite sure it would reduce your CA frequency and CSR, but they are expensive. https://document.resmed.com/documents/products/machine/aircurve-series/product-guide/1017631_aircurve10-asv-prod-guide_amer_eng.pdf
Sierra Thank yo so much for your feedback. It is a mine of info that I’ll keep in mind while trying to sort it out with my respirologist
To put thing into perspective, though, overall these CSR episodes don’t affect me as much. I usually sleep well and feel well at wake-up.
If I wrote this post it is because I am a bit concerned that these CSR’s, albeit rare, may be a precursor of something more serious to come, given the fact that I am 81 ( still running and windsurfing, though)
My betablocker is metoprolol. It was prescribed after two occasional tachycardia episodes at rest, two years ago, which led to an atrial fibrillation diagnosis.
My GP increased the dose to 2X50 mg/day after the 2nd tachycardia/ Afb episode 2 years ago. I am also on Metformin for borderline A1C and I read that metformin can be a factor in sleep disturbances.
By reading extensively about CSR and CA, I have come to realize that perhaps the CO2 dynamics may be involved. I asked myself whether there was some degree of CO2 retention( hypercapnia, as they call it) and I wondered whether the EPAP setting needed to be adjusted . Perhaps it was too high and impeded the full CO2 evacuation
. Currently, my pressure setting was 12.4-15.8. I thought that lowering the EPAP to 10.5 , with 15.8 IPAP could facilitate the CO2 evacuation. I’ll see how it works. If I still have CSR’s I’ll try the EPR adjustment you suggested , as a 2nd venue.
Another association I made is about the Tidal Volume. I noticed that when the AHI ‘s are on the rise ( above 1, which is rather rare) , particularly when I have CSR events, the minimum tidal volume drops to 0. AS I understand it, perhaps wrongly, if the TV is 0, there is no air exchange in the lungs and the blood CO2 then may increase.
Last night, with the new adjustment, I had an almost perfect AHI score of 0.59 ( 0.23 OA’s, 0.35 H). What is interesting is that the TV reached a peak of 1500 ( 99.5), which happened only once before with an even lower AHI score of 0.25. Usually, the TV is 1200-1300 at 99.5. Perhaps the lower EPAP setting has contributed to a higher TV.
Thanks again
Ittiandro
I think the advantage of the bisoprolol is that it is longer acting than the metoprolol, and only needs to be taken once a day and is said to have a more uniform effect throughout the day. I take my 2.5 mg once a day in the morning, and potentially it is having less of an impact during sleep. I have not heard that metformin is an issue. I take 500 mg x4 times a day. Apparently there are social media stories circulating that metformin prevents cancer and makes you live longer! I take it for diabetes, and expect no more than better BG control.
I think the breathing control issue is much like a cruise control on a vehicle that is not working well. Everything is fine until you come to a hill, and then the vehicle slows down too much, despite asking for more and more gas. Then at the top of the hill or just beyond it goes too fast, and tries to slow down. For me an event like a "hill" starts the cyclic breathing off and it can take some time to stop. The image below is typical. But, for reasons I don't quite understand things have been better over the last year. OSCAR reports 0% over the year. Before I was getting an event about once a month. I have had chronically low hemoglobin for years, and over the past year I started taking a prenatal vitamin with extra iron, and I have gotten my hemoglobin up somewhat, but it is at least within the lower part of the normal range. Perhaps the higher hemoglobin has had some effect on my O2 transport response.
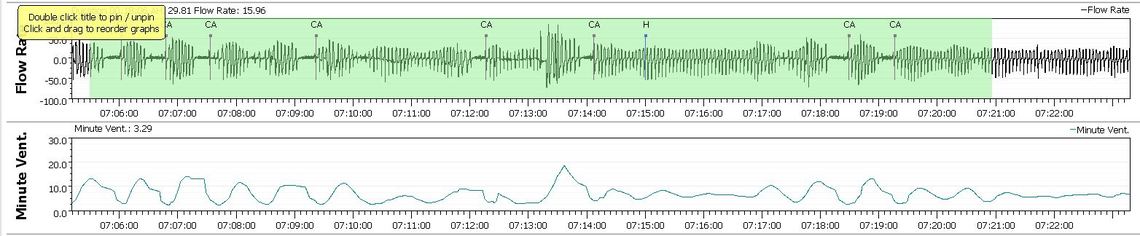
After saying that I have not had any CSR for over a year, I got a full session of it last night. No idea what may have triggered it other than it has been on the warm side for the last couple of days. But, I did get a restful sleep. The night before my AHI was 0.15, and now here I am over 3.0. Can't recall when that has happened before.