I was diagnosed with mild sleep apnea (AHI 5) and have been using my cpap for about 6 weeks. No matter what pressures I try, I'm still so sleep during the day. Most of my events seem to be caused from SWJ. Any help will be appreciated! (The settings on the second screenshot are what I have been using for the past few days. I don't know why they changed in SleepyHead today.)
I tried to respond to your post for help on your pressure settings, but for some reason the ability to reply does not work. I would suggest posting your SleepyHead charts again in a new post. Not sure what is going on.
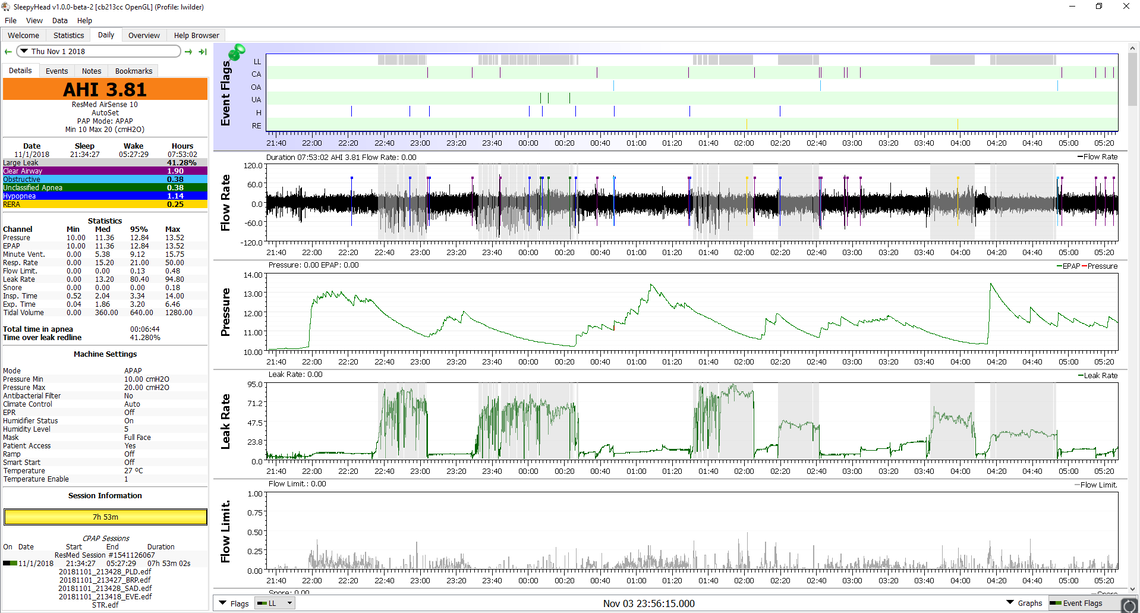
One question I had was about the mask you are using. One report says it is full face and the other says it is a nasal pillows mask. To get the mask leak report correct, you need to have the correct mask setting in your AirSense 10 to match the mask you are using. Or, did you use two different masks? One thing I see is that the pressure on one chart is significantly higher than the other.
That said, your main issue seems to be central apnea. Unfortunately that is not corrected with pressure, and in some people more pressure causes more central apnea. But in the two charts you posted I did not see much relation between when the centrals occur and when the pressure was higher.
My normal approach to setting pressure is raise the minimum pressure first, until it gets to the point where a good portion of the night the pressure is at minimum. This tends to lower obstructive apnea by getting the pressure up sooner in the night and avoiding some of the apnea. Next I lower the maximum pressure to clip off some of the higher pressure excursions. Part of that is for comfort, and avoiding higher mask pressures which cause leaks, and also in some cases it can reduce central apnea caused by too much pressure.
Hope that helps some, but post again and hopefully the reply function will work...
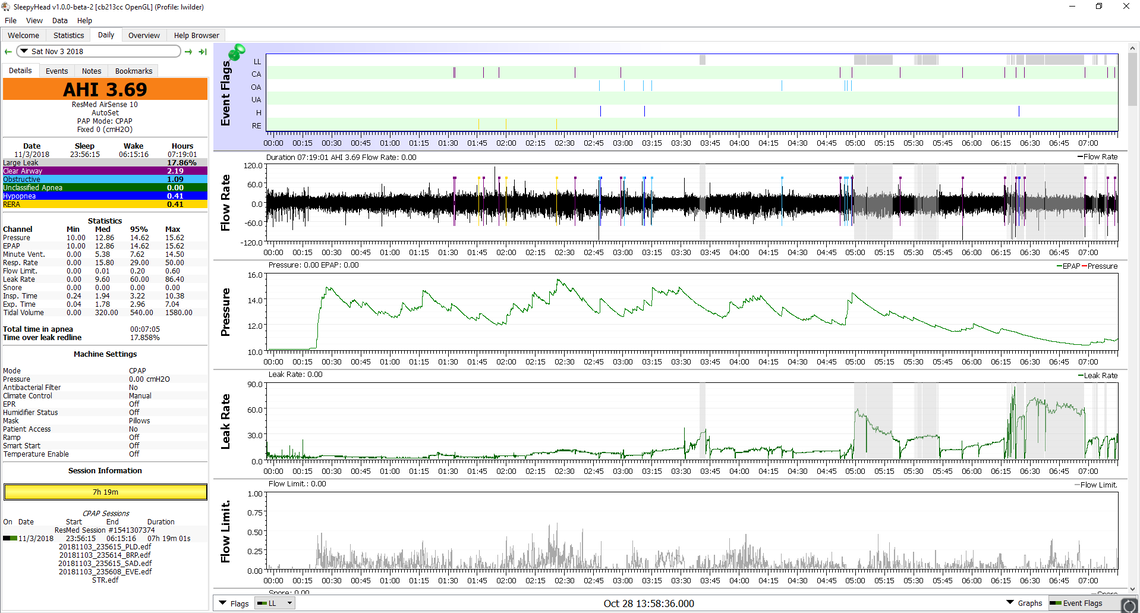
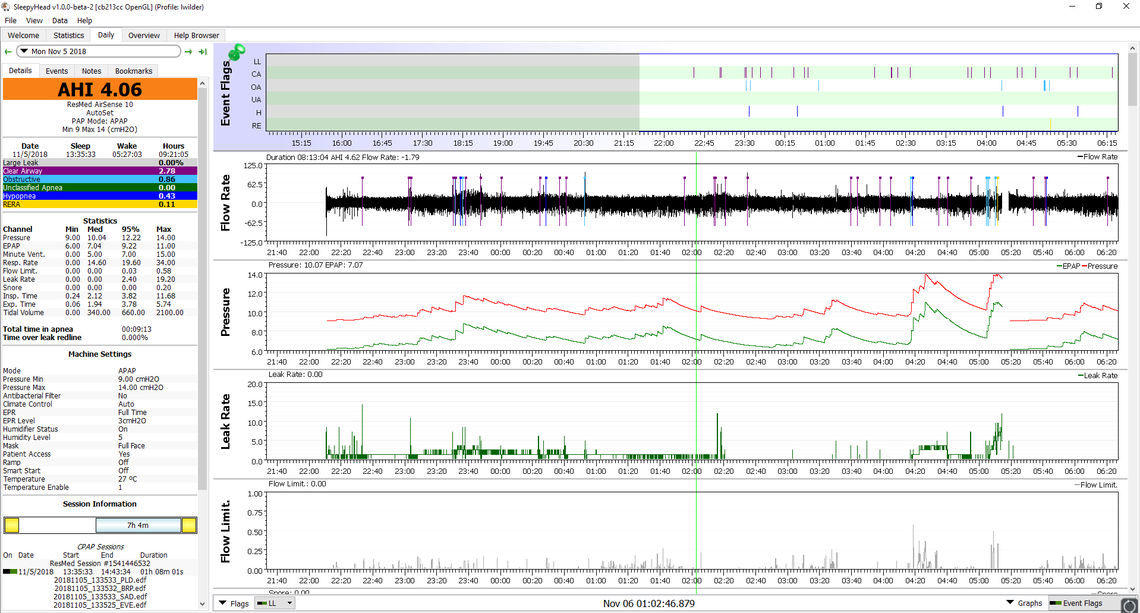
I am using a full face mask. SleepyHead must have had a glitch with the one day because all the info is wrong. I have attached last night's data and all the info is right on it. This is a pretty typical night for me.
While your AHI is technically within the treatment goal of 5 for apnea, there are a couple of things that are a bit concerning. First is that you were diagnosed with an AHI of only 5. That is right on the dividing line of no apnea (0-5 AHI) to mild apnea (5-15 AHI). Do you have the breakdown of the type of events you were having at diagnosis. Were the CA events significant at that time or have they developed with CPAP treatment?
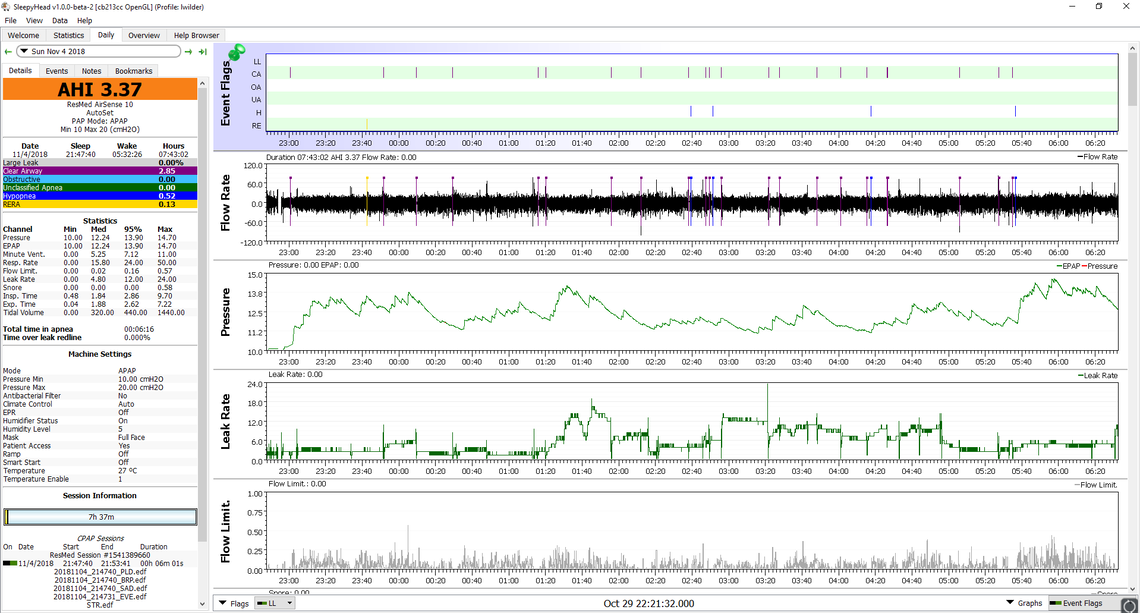
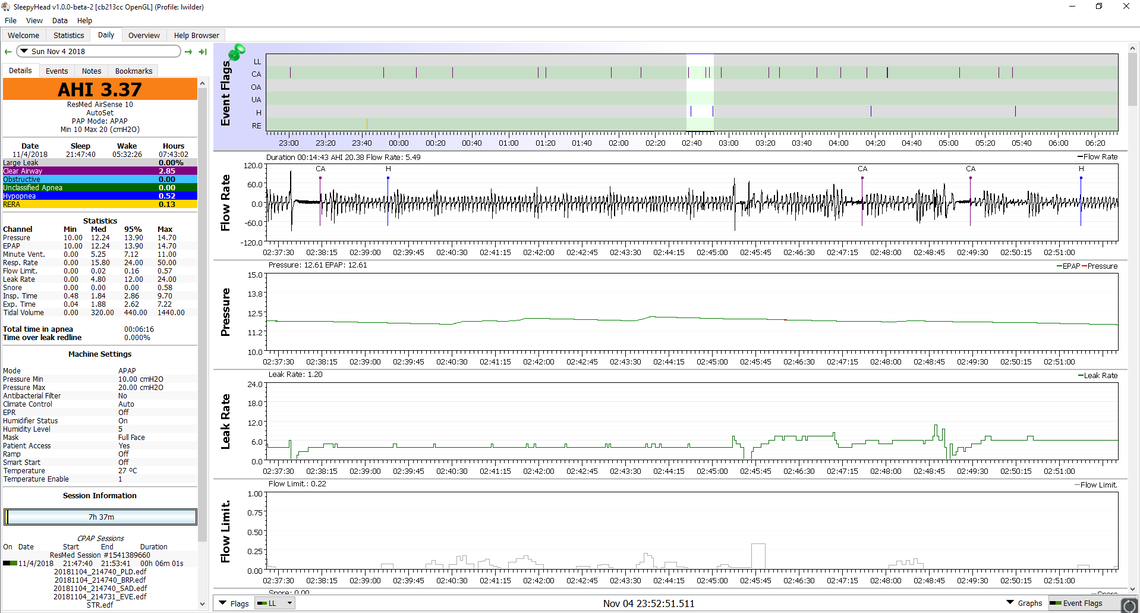
The second issue is that you have such a high proportion of CA events to OA events. You mentioned that you thought it was SWJ which I take to mean sleep wake junk due to waking up and going back to sleep frequently. Can you show a close up of the events when there are a number or mix of events. 2:50 looks like a good time, but there may be others. Just keep left clicking on that area until it is possible to see the individual breaths. Also do you have any thoughts on what may be waking you up frequently?
I mentioned that I like to move minimum pressure up first, but in your case if this is a typical night, there are really no OA events to prevent. So, I think I would instead start by bringing maximum pressure down. I see it is at the default maximum of 20 cm now. I think I would try 13 cm first to see what that does, and then follow that with steps down of 0.4 and see if there is a point where CA events start to decrease or OA events start to appear. It helps to try 2-3 nights at each pressure to get a representative picture of what each max pressure does.
On SleepyHead layout it may be helpful to squeeze in the snore chart unless nothing ever shows up as snore. It can drive pressure up. I also like to see mask pressure just to verify what the machine is doing. My interpretation is that Pressure is the machine setpoint, while Mask Pressure is the result.
So I hope that helps. Post your results as you progress and I will give further comments. There may be one other thing or two to try if reducing max pressure does not help.
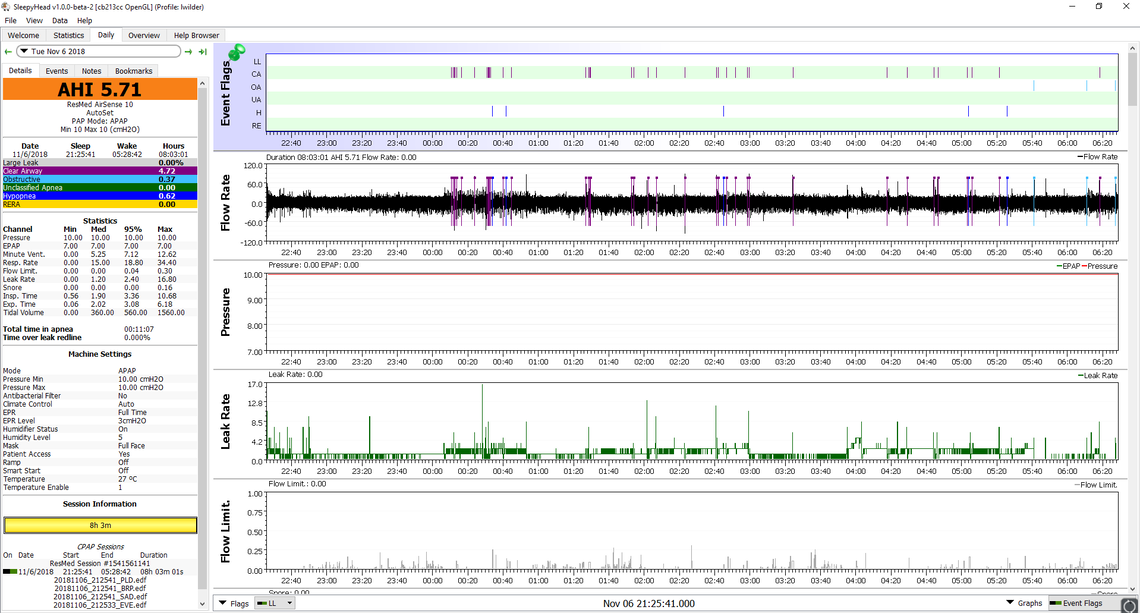
Here is a close up of that cluster of events at 2:50. I haven't gotten a copy of my sleep study so I don't know what kinds of events were recorded. Also, I never show anything on the Snore chart.
I have no idea what is waking me up so often. Usually I only remember waking up once maybe twice but my data indicates lots more arousals. Last night I tried adding EPR back in because that has helped lower FL before. I also adjusted my pressures to 9-14. The one pause in my sleep was my son waking me up. Also, I took a nap earlier in the day so I zoomed in just on my night's sleep.
What you are looking for in zooming in on those central apnea events is an indication of waxing and waning breathing depth. In one sense sleep wake junk can be dismissed at noise, but the underlying problem may be that your body respiration control system is not stable. To make a auto cruise control analogy, if your car encounters a hill and the car slows down, the cruise gives more power, and then you go to fast, and then slow down again. I see some evidence of that in your close up. If you scan through your events on multiple nights you will get an idea of how often you see that waxing an waning pattern. I find they sometimes produce a CA event, or sometimes an OA event, or sometimes a hypopnea event. However, the underlying problem is the breathing effort control system is not stable. The next question is why? Well then it starts to get complicated. Here is an article that is worth reading. It is from a blog area of this website.
One thing that can happen is that the CPAP significantly improves your breathing, your oxygen levels go up and CO2 levels down, but your body is not used to those levels and it brings out the control system instability. Increasing CPAP pressure can make things worse, and that is why the first step is to minimize the pressure used. EPR also improves breathing effort. It is kind of a double edged sword though. It changes O2 and CO2 levels, and may hurt, but at the same time it assists with breathing effort to counteract the body's waxing and waning effort. But the first step is usually to turn EPR off, and then try it as a last resort. That would be my suggestion to you.
In summary, I think I would turn EPR off, and continue to reduce maximum pressure in 0.4 steps. One would expect OA to rise and hopefully CA to reduce. The optimum may be when they are about equal. When you are getting close to an optimum maximum pressure and are starting to see OA events become significant you may be able to reduce the OA by increasing your minimum pressure. At the end of the day you may be best off with a fixed CPAP pressure.
On the EPR I have found that the AirSense 10 has a very useful feature. When you set your ramp function to Auto you get to set a Ramp Start pressure. And you can also set your EPR to be in effect during the ramp only. For example you could set your Ramp Start Pressure at 7 cm, EPR at 3, and EPR type to Ramp Only. Then it will cycle pressure during the ramp to 7 cm on inhale, 4 cm on exhale, and when you fall asleep the EPR will shut off. This will stop reducing your exhale pressure and probably reduce OA events.
Hope that makes some sense. Any questions just ask...
Here is an example of the control system issue from one of my SleepyHead reports. You can see the waxing and waning of breathing effort following a disturbance in breathing.
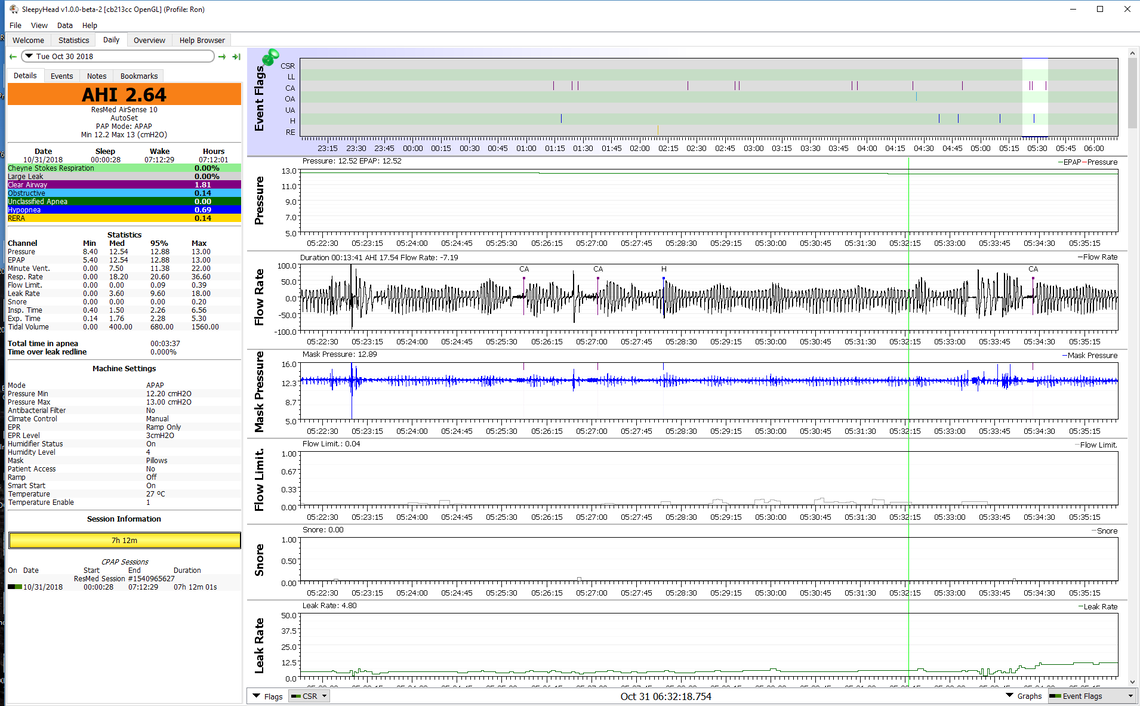
And in the extreme, this can progress to the point where it becomes unstable and the cycles are not damped out for a long period of time. ResMed flags that as Cheyne-Stokes Respiration. I experience that perhaps once a month or so.
It seems a little odd that you have such a low AHI and such high pressures. How was the range of 10 - 20 arrived at? Do you suffer from any restless legs?
My doctor started me out on 5-15 and after about 2 weeks I started tweaking the pressures to see if I could get my AHI to go down. I don't suffer from restless legs that I know. Last night I tried a steady pressure of 10 with an EPR of 3. I had a slightly higher AHI than normal (around 5). I can post my data from last night when I'm home at lunch time.
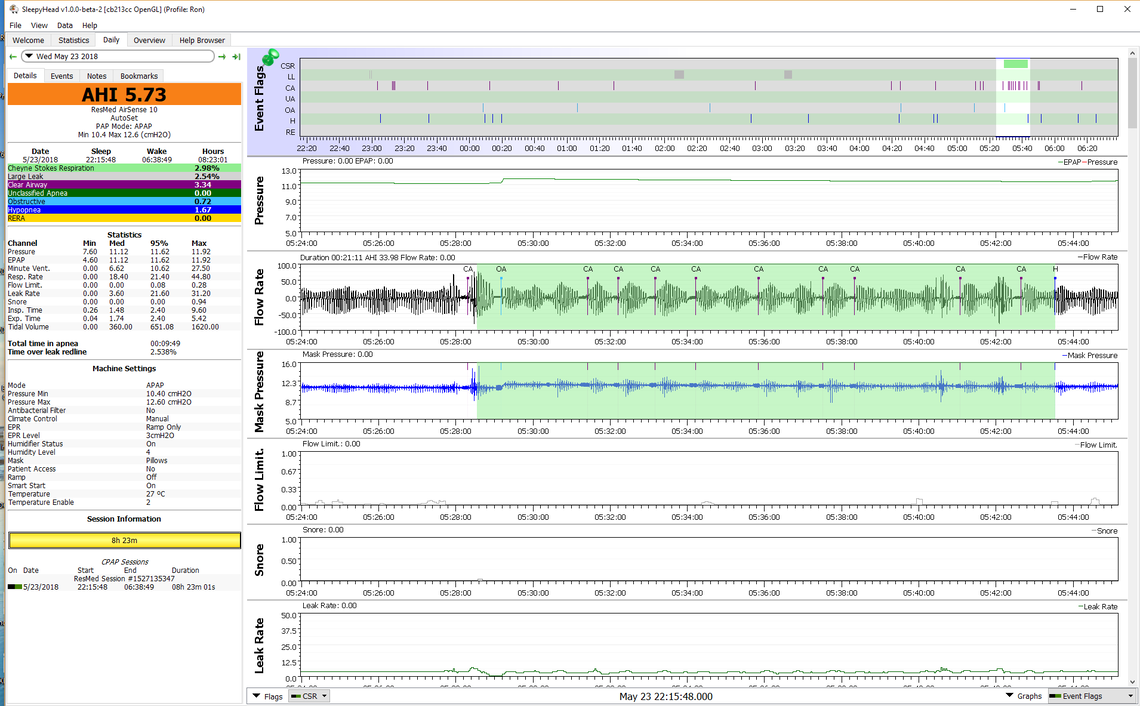
These are my results from last night. I used a steady pressure of 10 with an EPR of 3. I still had mostly CA's. Any thoughts?
I think this clearly shows that 10 cm combined with EPR is not good for controlling central apnea. It does show that 10 cm does control your obstructive apnea pretty well. I think you have a couple of options at this point. One would be to turn EPR off or to Ramp Only and see what that does. The other option which might be more informative would be turn EPR off or to ramp only and set minmum pressure to say 8 cm and maximum to 10. That would give the machine the option of keeping pressure lower, but not over 10 which may do some good in preventing CA. But again at this point I don't think EPR full time is doing you any favor.
I would suggest that you consider turning off the EPR because it can be the cause of central apnoeas. In theory, you should be able to set the minimum pressure much lower because the auto algorithm should adjust upward if an when required. However, I would also suggest that this should all be done in consultation with your doctor.