I was dianosed with severe sleep apnea in September and after a sleep study in Canada was put on a resmed S7 apap. This brought my AHI from 64 to 15-25. I had another overnight sleep study in October and due to a large % of centrals was put on a resmed bpap. This has brought my AHI to 5-20 My 2 sleep studies were done at an altitude of 500 feet. The problem is that I spend 6 months at 500 feet and 6 months in a warmer climate at 5500 feet. At 500 feet my AHI readings range from 3-7. At 5500 feet they range from 5- 20 and average around 10. I understand that Resmed states that their machines correct for altitude but my readings over the last four months are directly related to what altitude I am at. I am thinking that I should ask my Doctor to have another sleep study at 5500 feet ( I don't mind paying) with the possibility of using two different settings depending on my altitude.My current settings on my Aircurve 10Vauto is IPAP Max 20.0 and Min 7.0. My airflow feels stronger at 500 feet than it does at 5500 feet Has anyone else experienced this situation or have any suggestions. I am a newby so please try not to get too technical. Thanks
Hi lakechapala
There were recent posts by mountaingoat who has similar altitude adjustment issues.
There are two separate issues here. One is in how the machine compensates for altitude, and the second is the issue of lower absolute pressure and as a result lower oxygen in the air on a mass basis. I'll try to keep this simple, but it is actually complicated.
First the machine compensation - The machine simply creates a differential pressure between the atmospheric pressure of the day and location. In other words it supplies 4 cm to 20 cm for example above atmospheric. The machine measures this differential pressure and controls to it without any compensation required. There is a BUT though. The machine measures pressure in the machine not the mask. It only tries to estimate pressure in the mask. As you go higher in elevation the air becomes thinner and the pressure drop in the hose and mask increases. So you are getting a lower pressure than the machine thinks it is supplying. That S7 machine from what I can see probably did not compensate for that error. The AirCurve machine should be compensating. I believe it does this by using a barometric pressure device that measures absolute pressure - which goes down as you increase elevation. The machine uses that pressure to compensate for the increased pressure drop in the hose and mask, and if the ResMed engineers have done their job properly, the machine increases pressure to compensate for the increased pressure drop in the hose. On machines without compensation you had to do this manually. Bottom line is that your machine should be doing this for you, and it should not be the source of your problems.
Now the thin air issue - While the machine is keeping the relative pressure in the mask the same, the absolute pressure is going down. The relative pressure is what keeps your airway open, so it should do just as good a job at elevation of avoiding obstructive apnea. However, the absolute pressure is going down (air is thinner), so the oxygen being delivered goes down. In most people up to 7,000 feet or so, that is not a problem. Your body adjusts breathing and all is good. But, if someone is susceptible to central apnea, which is really a control system problem, it can upset the apple cart. It is like a car on cruise control that keeps over correcting for going to fast and too slow. The speed just hunts up and down and is not stable. Same with breathing except when it goes down or even stops you have an apnea event or hypopnea event. My guess is that is what your issue is.
Guessing a bit here, but usually what this comes down to is that pressure in the machine may be causing the central apnea, and it may need to be lowered. The problem is that lowering pressure can create more obstructive apnea. What this means is that with your current machine the compromise setting of pressure is likely going to be different at elevation than at lower levels. But, if you can get a good compromise setting at altitude, it most likely will also work at lower level. If not, then you would have to change the settings so you use two different setups. I presume you are going to Mexico(?) seasonally? If so, that would not be a big deal.
You can do what you are suggesting and get another sleep study done at elevation. However, what I would suggest is that you download a free software program called SleepyHead and use it to view your data which should be all on the SD card in your machine since the day you started using it. From that, you may be able to determine what settings are best. If you post a typical daily detail report for the two elevations, I would give you my comments. I am not a medical professional, but I also suffer from mixed apnea, and can comment from a user perspective. It is not the easiest type to apnea to deal with. At the end of the day, if you are unable to get successful treatment (AHI<5) by optimizing the settings of your AirCurve 10 VAuto, there is another machine, which could work much better called the AirCurve 10 ASV. It is expensive and some heart function tests have to be done before going on it. Something to discuss with a sleep doctor, and a cardiologist. Depending on what part of Canada you are from, that can be difficult... This all said, there may be options to set up your existing VAuto machine better. I would investigate those with SleepyHead first.
Thinking about your dilemma, I came up with a couple of other options to consider.
I know it may sound regressive as you have gone from the S7 machine to the AirCurve 10 VAuto, but you might want to consider going to a fixed CPAP pressure mode. The AirCurve 10 can do that. I have actually done that with my AirSense 10 AutoSet and I am getting better results than I was in Auto mode. See this link to another thread for more info.
There is a good article in the Blog section of this website on Complex Sleep Apnea. The article mentions the off label use of a drug called acetazolamide to potentially treat central apnea. The intended purpose of the drug is to treat altitude sickness, but the conditions are related. It is something you could discuss with your doctor. If you are only going to high altitude seasonally, perhaps it could only be used when you go to altitude. Again, I am not a medical professional, so I cannot recommend it to you. I just raise it as something you may want to discuss with your doctor.
Thank you Sierra. I have downloaded SleepyHead and will post the data once i figure out how to do it
There are some things to do to optimize the layout on the Daily Detail screen before you post it so you can get the critical data to show.
When you have it set up just press F12 (PC) to capture the screen. A box will pop up in the bottom right showing where the image file is saved. With Windows Explorer left click on the file and drag it into the body of a message you are composing here. Use the Write a Reply button near the bottom so you get a full width window here to display it.
You can use the date functions to go back to what you think looks like a typical day (for AHI) at both elevation levels. Just remember to hide the calendar again. You can use the Overview tab to look back for what you think are typical days. But, just do the daily detail screen shots. It has the critical stuff.
Any questions, just ask...
As far as I am aware, the machines will correct for altitude but the have to adjusted MANUALLY to do so.
I did a fair amount of research on this when mountaingoat raised the altitude issue recently. I've sure that the post I made above is a reasonable interpretation of where the technology stands. In the ResMed line, I think the last non portable machine that had to be adjusted manually was the S6. The older machines had ranges of elevation that you had to set to your applicable range. So, it was an approximate correction. I suspect the new machines measure actual atmospheric pressure and correct exactly to the altitude.
This however only compensates for the pressure drop in the hose issue, and is quite effective for obstructive apnea. It has nothing to do with individual central apnea sensitivity to altitude changes though.
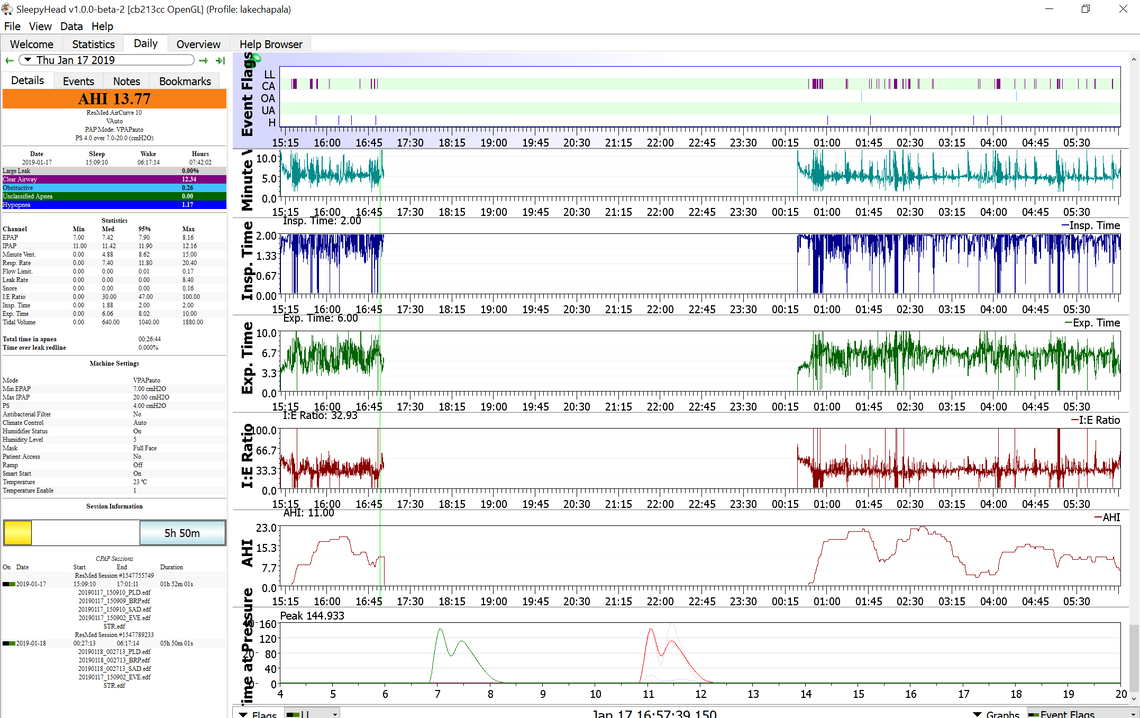
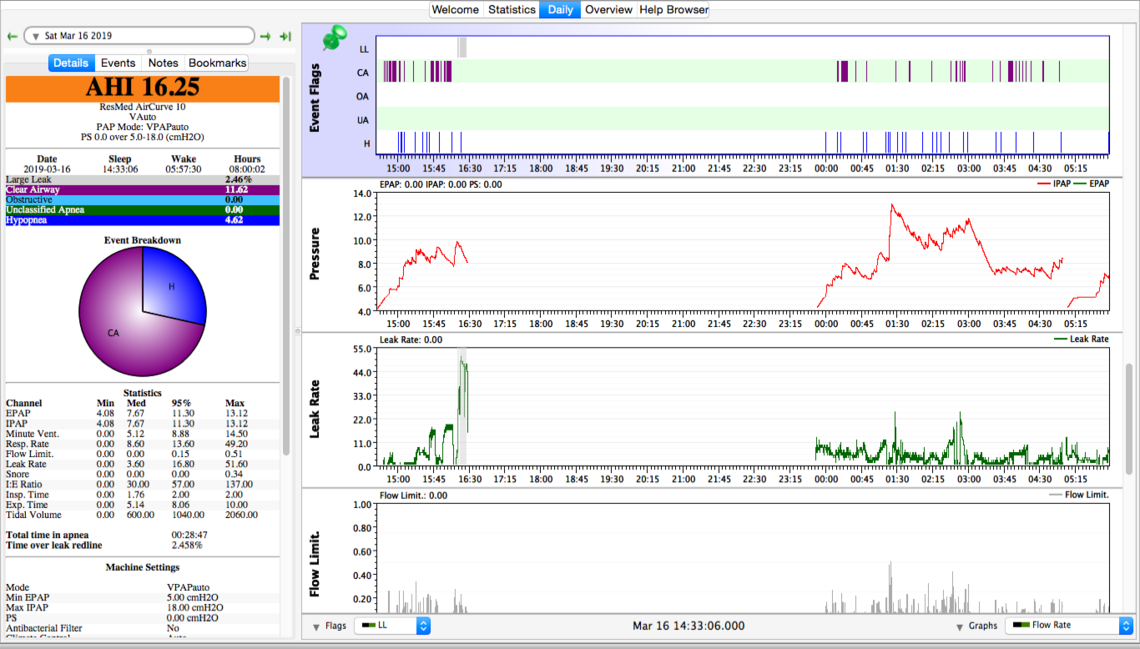
here is a screenshot (hopefully)
That looks pretty good. I would suggest one more layout change. Slide the bar up on the right so the Pressure, Mask Pressure, Flow Rate, Minute Vent., Flow Limit., and Leak Rate show on the screen. You can change the order by left clicking on the title of the graph and then drag it up or down. Clicking and dragging on the gray dividing lines between the graphs can make individual graphs bigger or smaller.
From what I can see your leaks are fine, and your pressures are not all that high. Your obstructive apnea is low, suggesting you do not need more pressure. Your central apnea index is very high though, which suggests less pressure is needed. The machine as it is set up is not behaving much different than a AirSense 10 AutoSet with EPR turned on. The only difference is that your pressure support is 4 cm and the maximum EPR on an AutoSet is 3 cm. Pressure support and EPR are both simply the difference between inhale pressure (IPAP) and exhale pressure (EPAP).
Are you planning to try to adjust and improve the setup yourself, or are you going to ask the clinic to adjust it for you. My initial thought if you were going to adjust it yourself would be to set the pressure support to zero. That alone may help quite a bit. Central apnea often can be aggravated by higher pressure. Reducing pressure support should reduce pressure. If that helps but is not enough to bring down the centrals to an acceptable level, then I would next start to reduce the Maximum IPAP. While making these changes you will want to watch the obstructive apnea index. Reducing pressure support should not hurt it. But reducing IPAP may eventually cause it to come up, and there can be a trade off point where reduced centrals are being offset with increased obstructives.
If you are going to make these changes yourself here is a video on how to get into the clinical menu to do it. It is for an AirSense, but the AirCurve should be very similar. The menu choices will be slightly different. The only setting you would want to change initially would be Pressure Support, and then perhaps later Max IPAP if necessary.
If you are going to have a clinic do it, I would just ask if you can try no pressure support, and if that does not help, then reduced IPAP.
If you can post this same graph with the graphs I listed above showing, I can give you a better idea as to what the IPAP may have to be reduced to. While my AHI were not as high as yours, I live at 2000 feet, and I have had central apnea issues. I was able to improve AHI a lot by turning off EPR which is essentially the same as PS, and by reducing pressures, in my case from a maximum of 15 cm to around 11 cm. I have a feeling you may be able to reduce pressures down into the 8-9 cm range. But, the proof is always in the pudding. One has to try it to see what it actually does.
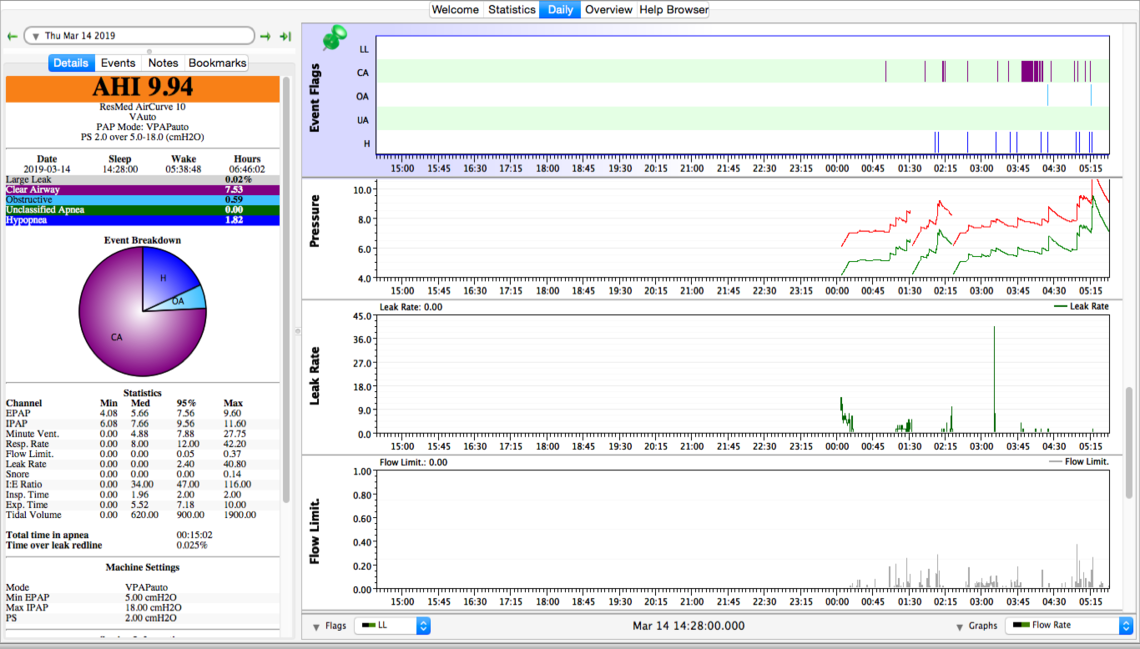
here is a snapshot at 500 feet altitude. the previous one was at 5000 feet altitude.
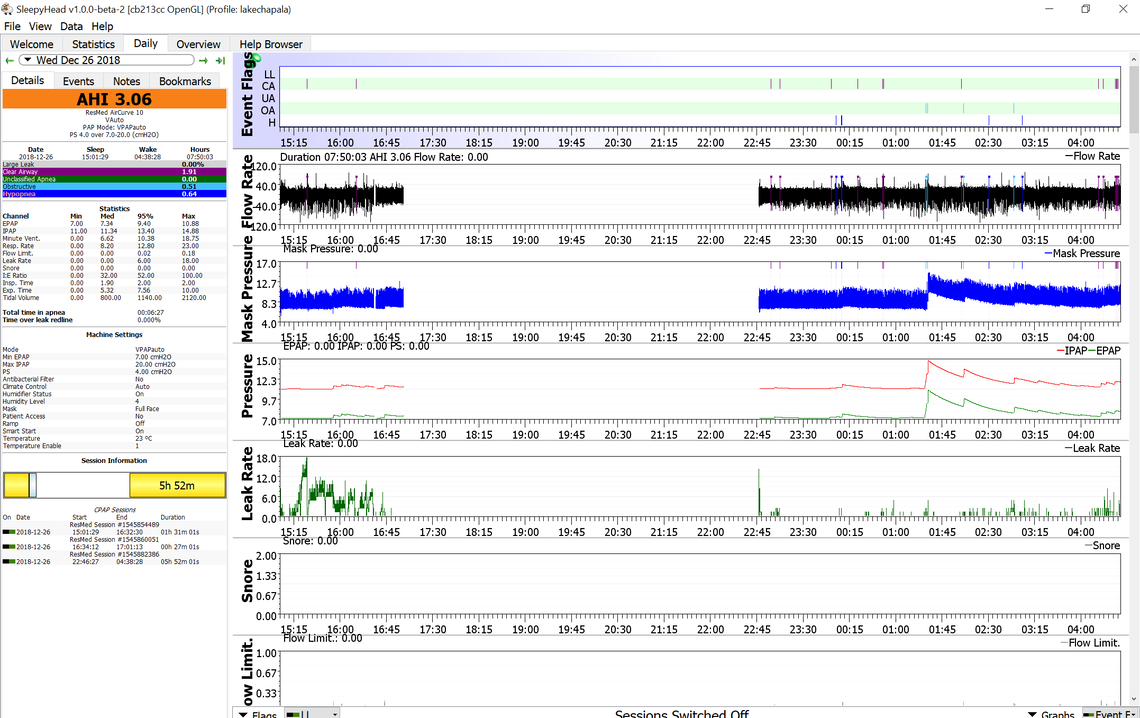
Yes, that is about what I would have expected. Centrals are down, while obstructives are still not that bad. My comments would be the same. If it were me I would first try setting pressure support to zero. And if that is not enough then start lowering IPAP Max. I suspect with some adjustments a setup can be achieved that will work at both elevations.
Keep in mind I am not a medical professional. I have no sleep clinic to depend on, so what I know comes from what I have tried myself, and what worked for me.
I may not have explained the logic in setting the pressure support to zero, and potentially reducing EPAP pressure. The thinking is that the minimum of EPAP and IPAP can be responsible for obstructive apnea events. And at the same time the highest pressure of the IPAP can be responsible for creating central events. With a pressure split between the IPAP and EPAP you can get the worst of both worlds -- more obstructive events and more central events. I hope that makes some sense... If not just ask.
There are other reasons to have a larger split between IPAP and EPAP that might outweigh these issues in some individuals that are having trouble breathing. It does not look like that would be the case for you, so lets leave that aside for now.
Excellent ideas Sierra. My slow response is due to my newby status. Took me a few days to figure out how to post comments and figure out SleepyHead and how to paste charts- but I am learning fast. I have challenged my clinic to come up with some ideas. Will continue to work on my charts. I did modify my settings on my S9 after my previous clinic was unresponsive so have learned how to get into clinical settings. The problem with my new machine is that my new clinic will know quickly when I change a setting as my info is transmitted to them daily. I want to see if they have any ideas. My sleep doc is excellent but he probably has 2000 plus patients and hasnt time to fine tune settings. Will be back to you once I digest all of your comments. Many thanks!
It is always good to involve your clinic if they are responsive to your concerns. My machine also has the "ET Call Home" wireless feature, but I am not really sure how much data is actually sent. I have a feeling only the summary data (AHI, Sleep Hours, the very basics) is sent wirelessly. If that is the case you will be seeing much more detail in SleepyHead than they will be seeing. I have come to the conclusion that is why the MyAir app that ResMed has is so limited. They really don't have much data behind them. I believe the real detailed data that SleepyHead displays is only on the SD card, and if you wanted them to look at the detail you would have to bring in the card and they would view it with the ResMed ResScan software. That does not mean you could not have a phone conversation with them to discuss the issue. It really don't think as a matter of course these clinics have the time to actually monitor individual patients results when they have 2000+ patients as you say.
I saw my sleep doc 10 days ago. Doesnt want to go the ASV route and approved purchase of an air curve 10 vauto with a new prescription autobipap max Ipap 18cm, min epap= 5 cm, delta 4. After a week back at 5000 feet, my ahi is averaging 20. My clinic does not see their role as giving advice on settings or fine tuning. I am satisfied with my readings at 500 feet so i am going to proceed with your suggesion to eliminate pressure support and if that is not enough I will try reducing epap. My centrals are 95% hp 5 % and the odd obstructives.
more info
If it were me, adjusting pressures for myself, I would start with reducing the pressure support in steps. Perhaps reduce from 4 to 2 for a couple of nights, then from 2 to 0 to see that that does. The hope would be that your overall pressure would come down. And, with the pressure lower, perhaps the CA events will be reduced. After that, if you still do not have an acceptable AHI, but it is better, then I would start to limit maximum pressure. From what I see in your charts, I don't think you are going to need a lot of pressure to control your obstructive apnea events. And when you get that pressure down, that should reduce or even stop the CA events. If you go ahead with reducing the pressure support, post some charts again when you get it down to zero.
Will do. Tks Sierra
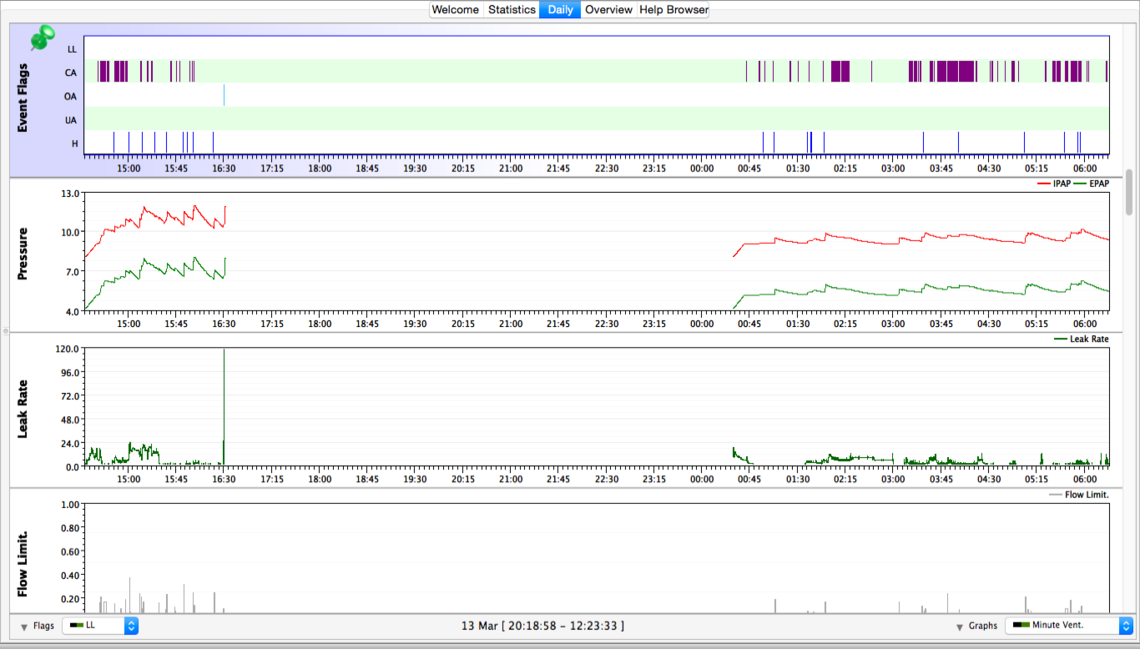
Sierra: attached are screen shots for the last 4 nights, reducing ps to 2 for 2 nights and ps 0 for 2 nights. For some reason sh did not pick up my snooze on March 14. I took 2 screen shots per day in order to capture all the info you requestedYour comments/suggestions would be appreciated.
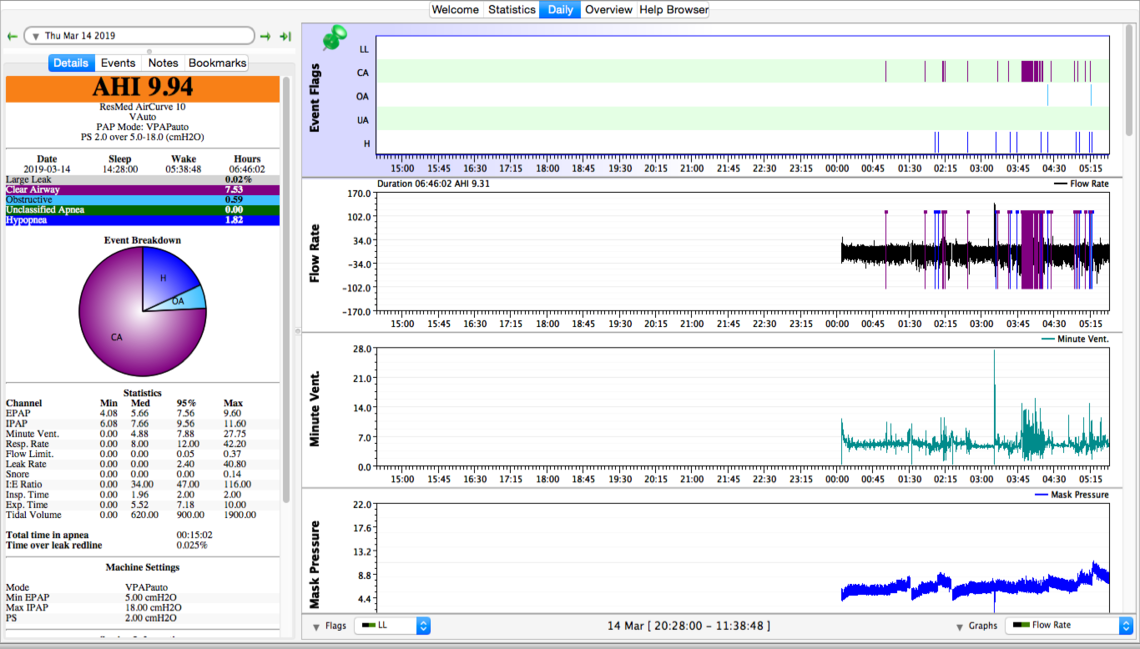
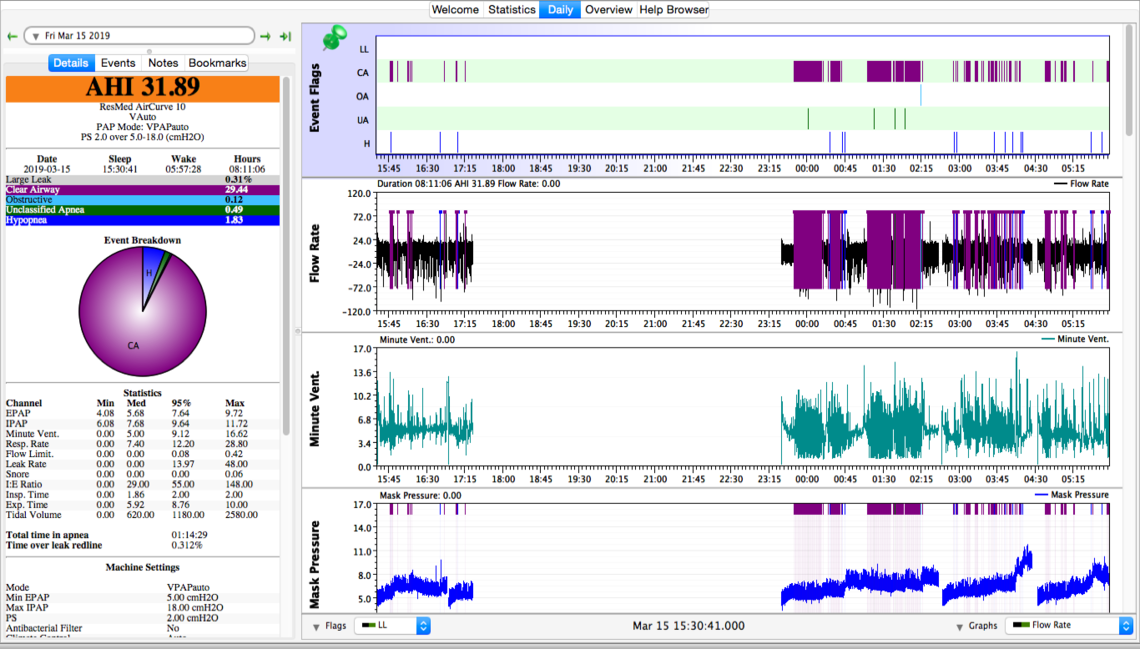
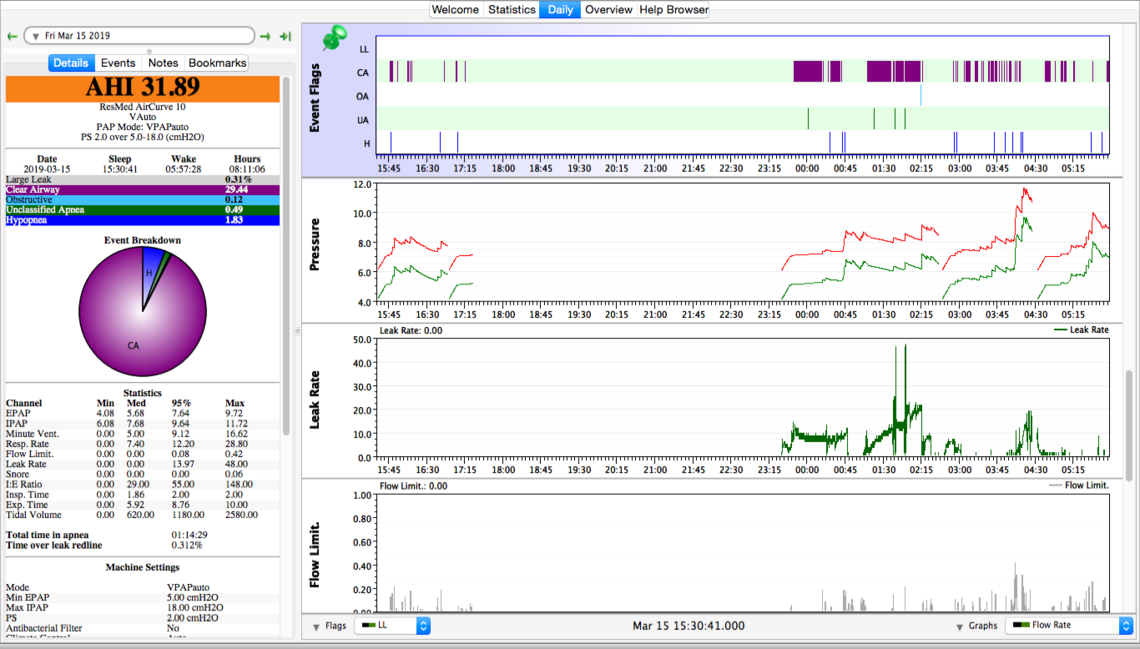

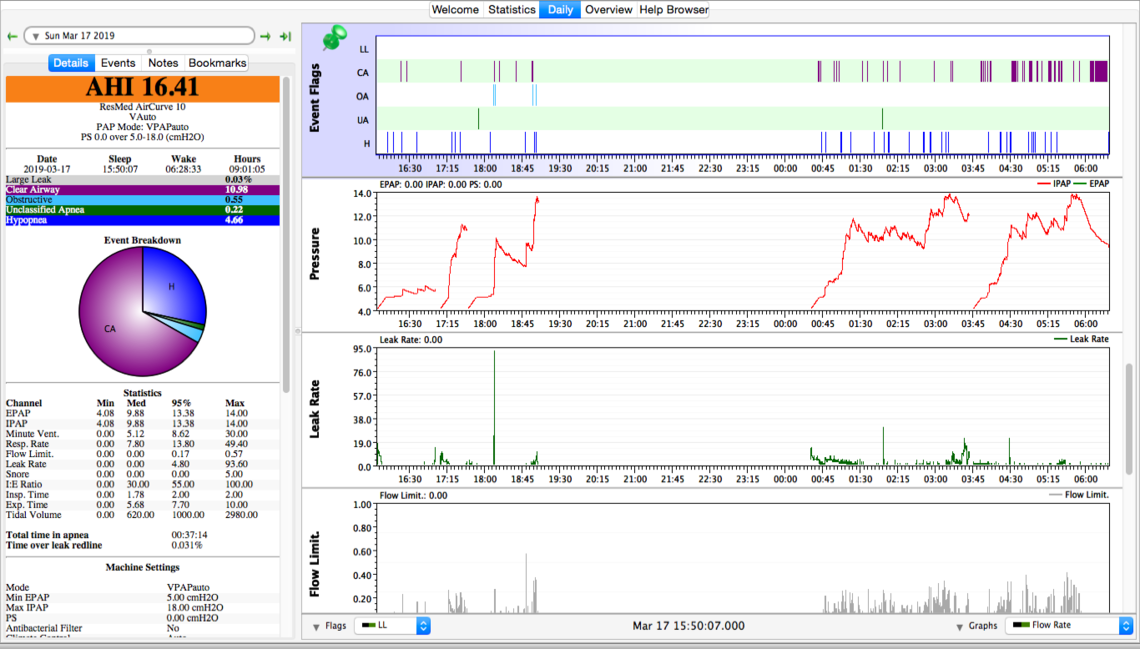
Sorry, but I have been away this week. Just got back. I am a bit surprised that reducing the pressure support did not gain you more of a reduction in the CA events. Again if it were me, my next step would be to try limiting the maximum pressure. The idea would be to try and reduce the CA without causing a significant increase in obstructive OA events. I think I would try a max pressure of 12, then 10, then 8 cm to see if progress is being made.
Tks Sierra. Hav been running at 14 pressure for 3 nites and ca % has dropped to 67% from 98%, and hyp the rest with a couple of oas. Ahi has dropped from 18 to 13. I will continue pressure drop to 8 and will send a screen shot at that time. Appreciate the help.
It sounds like things are heading in the right direction.
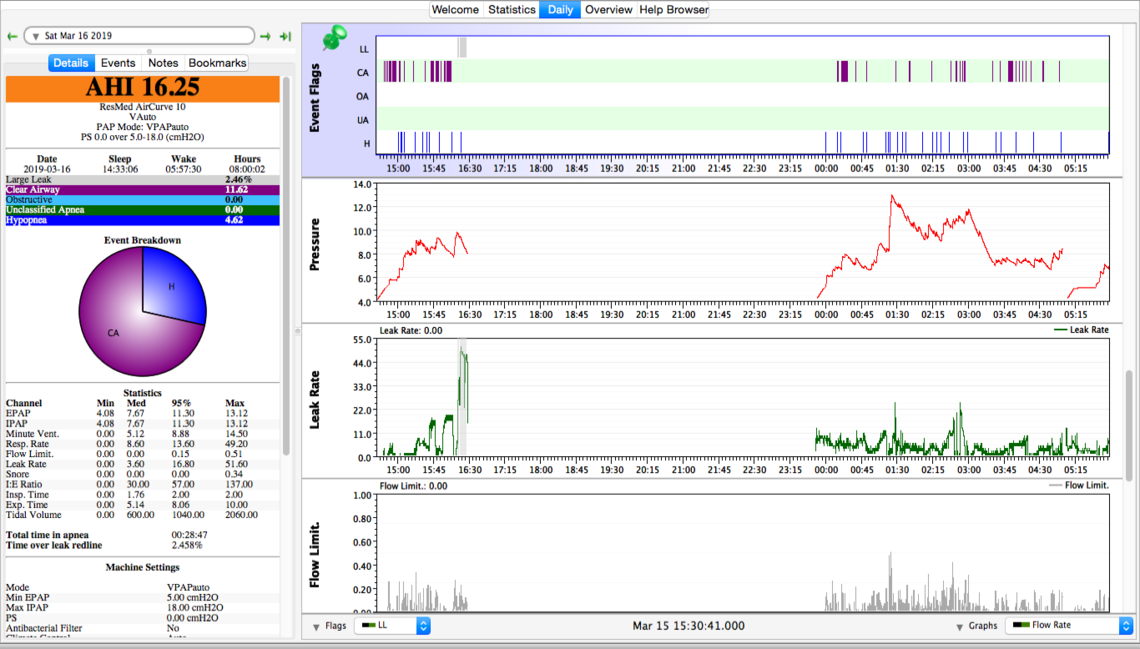
Sierra: I have sent screen shots so you can see the changes in pressure and the results. Making progress. I will be leaving 5000 feet on April 14 so still have time to try other settings. My sleep doc and yourself brought up Acetazolamide. It is a strong drug and has side effects but I have the pills and will try them perhaps 7-10 days before I leave. Meanwhile any further suggestions you may have would be appreciated.
Hope the size is now readable.
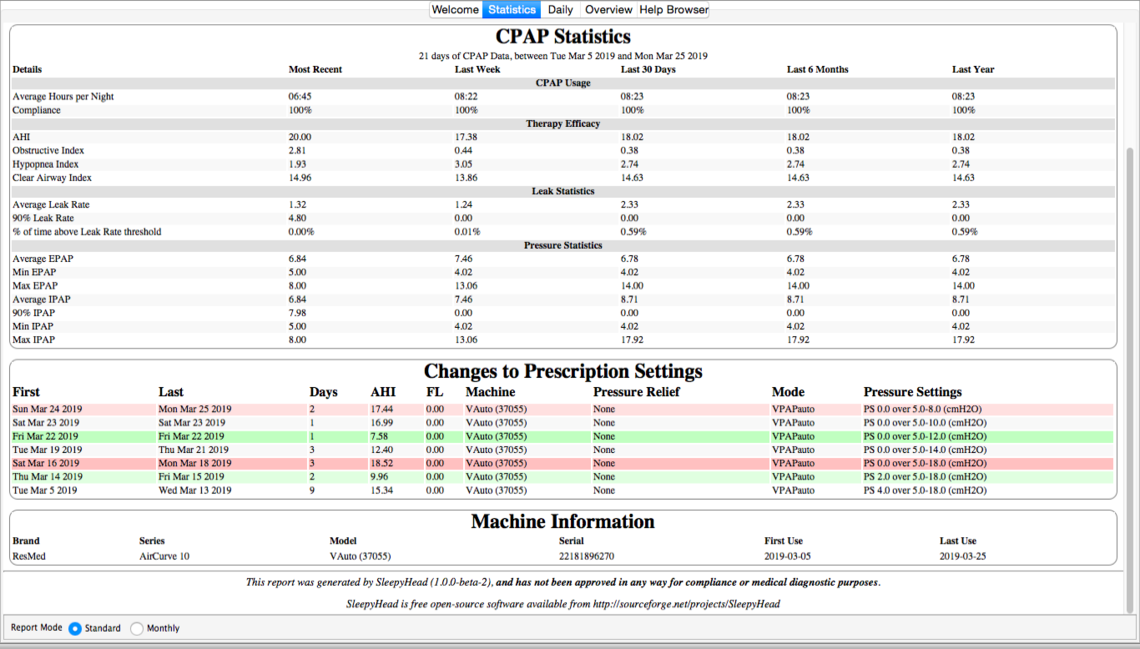
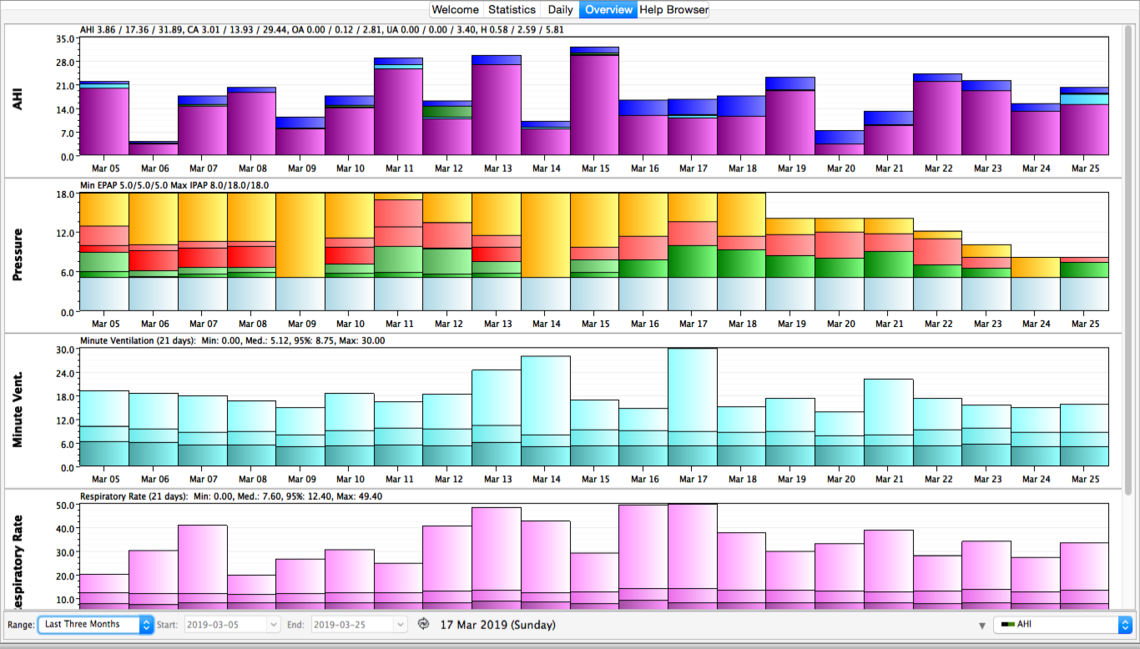
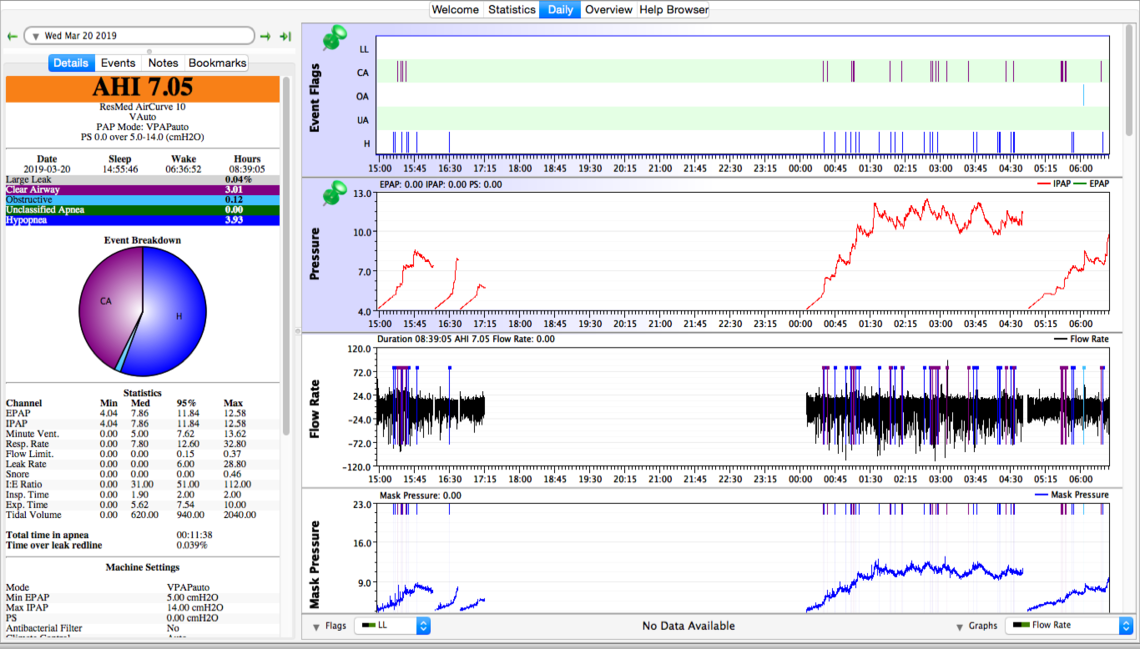
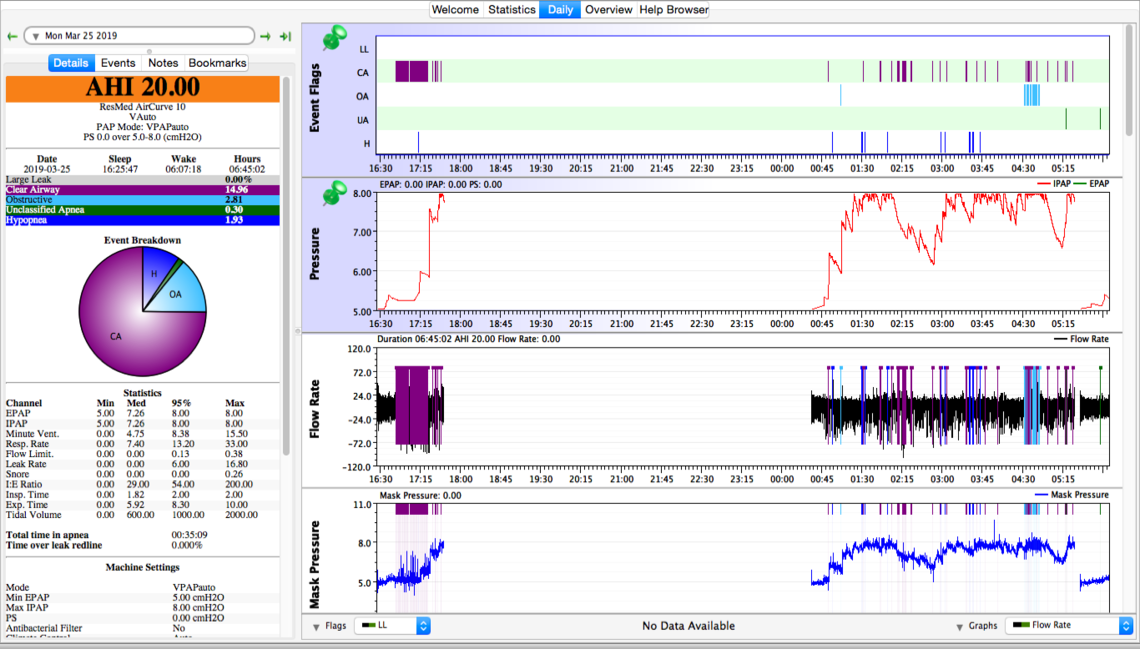
The March 20 night looks promising at 14 cm. However the Mar 23 at 8 cm does not look so good. Didn't seem to bring CA down and OA is starting to act up. About all I can suggest is trying 12 cm, 10 cm for a couple of nights each. The acetazolamide is also worth a try after that. I would try it at the pressure that has worked the best by then. I recall we talked about the ASV option already and your doctor was not willing to prescribe it.
Short of doing that, there may be some opportunity to tune your machine to provide better control of the central apnea results at altitude when in the pressure support mode. I am afraid I don't have the experience to do that. In the VAuto and S mode you can set an inspiratory time control (TiControl). In the S mode you can set the rise time. These are fairly complex settings and your best opportunity would be if your sleep clinic provided suggested settings that you could try at altitude. See pages 4-6 in the manual at the link below. These settings affect how and when the pressure switches back and forth between inspiration and expiration. They can help prevent central apnea events if properly tuned.
If none of this works, then you probably are best to revisit the AirCurve 10 ASV option with your doctor.
Thanks Sierra. I will continue to try to find the sweet spot and will talk to my dme when I get back to 500 feet about other settings however in the past he has been reluctant to give advice and I don't have the competence. I will have two weeks at 500 feet before I see my sleep doc. Do you have any suggestions as to what I should change my settings to? When I have completed my Acetazolamide trial at 5000 feet I will report my findings in a separate thread.
IMHO your at altitude chart shows the need for an ASV. That is to titrate out the Obstructive Apnea to a level of less than 5 AHI (you have) and demonstrate a remaining Central index of greater than 5 AHI ( yours is 15 ).
Your 500 ft numbers do not meet these same criteria, though they too would benefit from an ASV though you would definately have far fewer "triggered" breaths at lower altitudes. In the past I have recommended that a user maintain 2 sets of settings, one for altitude, and one for not.
I do see an ASV in your future, unfortunately, it takes the medical community some time to reach this same conclusion.